Introduction
Adrenal collision tumors (ACTs) are uncommon masses
consisting of two biologically distinct tumor types in the same
adrenal gland (1–3). In general, collision tumors are
difficult to diagnose by imaging studies, such as B-type
ultrasonography, computed tomography (CT) (4) and magnetic resonance imaging (MRI)
(5,6). Therefore, postoperative
histopathological examination is considered the gold standard for
the diagnosis of collision tumors. Ganglioneuromas, mostly
originating from primordial neural crest cells, are rare benign
tumors, while parachordomas are rare slow-growing tumors with low
invasive potential, which mainly develop in the limbs, chest,
abdomen and back (7). Furthermore,
parachordoma as well as ganglioneuroma mainly appear as single
space-occupying lesions. Therefore, both tumors in the same adrenal
gland is a rare occurrence and, thus far, there have been no
published reports of parachordoma and ganglioneuroma as components
of an ACT.
Case report
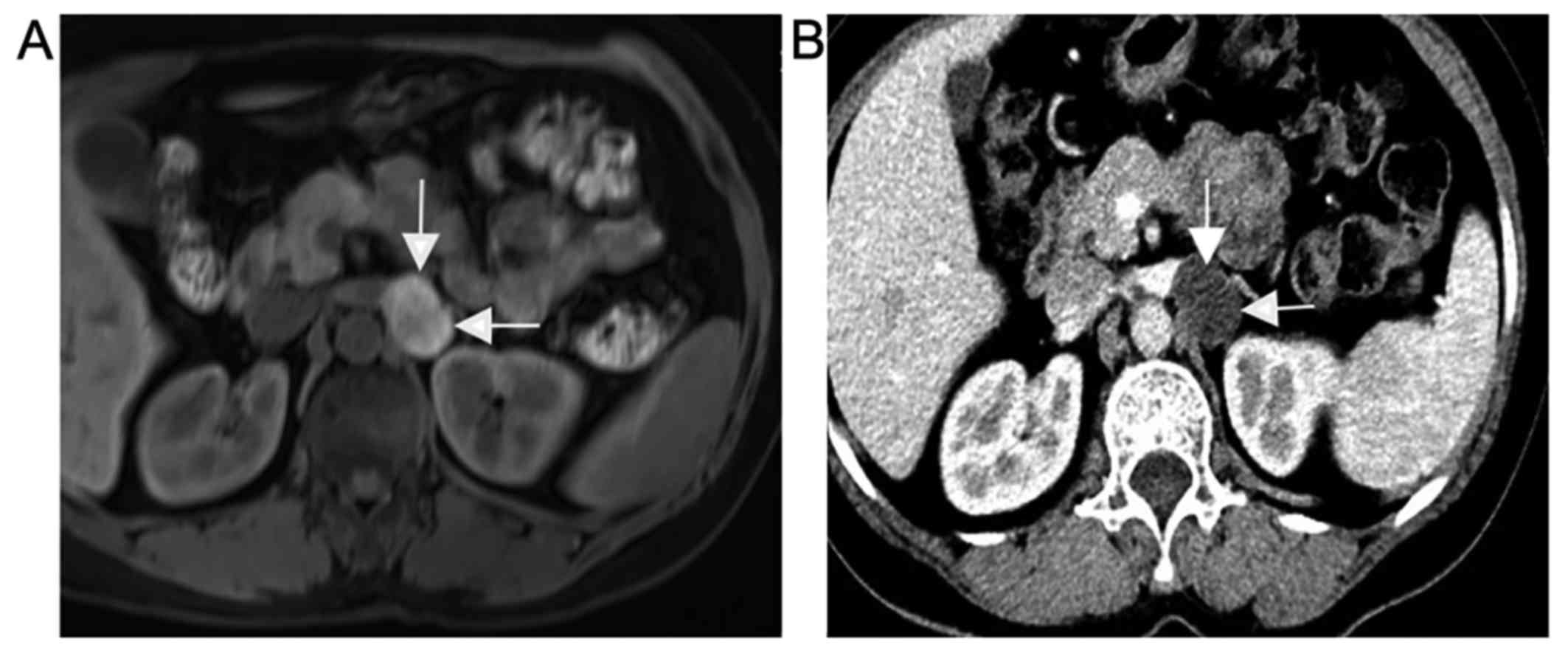
In April 2017, a 56-year-old woman was found to have
a left adrenal space-occupying lesion on an MRI examination,
without any associated discomfort. The MRI revealed a 25×19-mm
nodular, irregular mass, appearing as a long T1 and long T2 signal
shadow in the inferior margin of the left adrenal gland, with
slight enhancement on contrast-enhanced imaging, which indicated a
neurogenic tumor. This tumor was considered to originate from the
adrenal gland (Fig. 1A). The patient
was in good health and had no symptoms indicating hormonal
imbalance. Moreover, there were no abnormalities on systematic
review and physical examination. The laboratory examination
revealed no major abnormalities in the blood cell counts, liver and
kidney function tests, or serum electrolytes. The plasma
adrenocorticotropic hormone level was 18.5, 36.8 and 19.5 pg/ml at
0, 8 and 16 h, respectively (normal range 0–20, 6.0–40 and 3.0–30
pg/ml, respectively), and the serum cortisol level was 0.80, 7.2
and 1.6 μg/dl at 0, 8 and 16 h, respectively (normal range 0–9.7,
3.7–19.4, 2.9–17.3 µg/dl, respectively). The B-ultrasound
examination revealed a 24×16-mm solid and hypoechoic lesion without
an obvious blood flow signal in the left adrenal gland.
Furthermore, an adrenal CT scan revealed a space-occupying lesion
(sized ~28×20×33 mm) in the inferior margin of the left adrenal
gland (Fig. 1B), and the CT value of
the plain scan only differed by 2 HU from that of arterial phase
CT. Therefore, the possibility of a ganglioneuroma was first
considered. After excluding surgical contraindications,
laparoscopic surgery for adrenal tumor resection was successfully
performed.
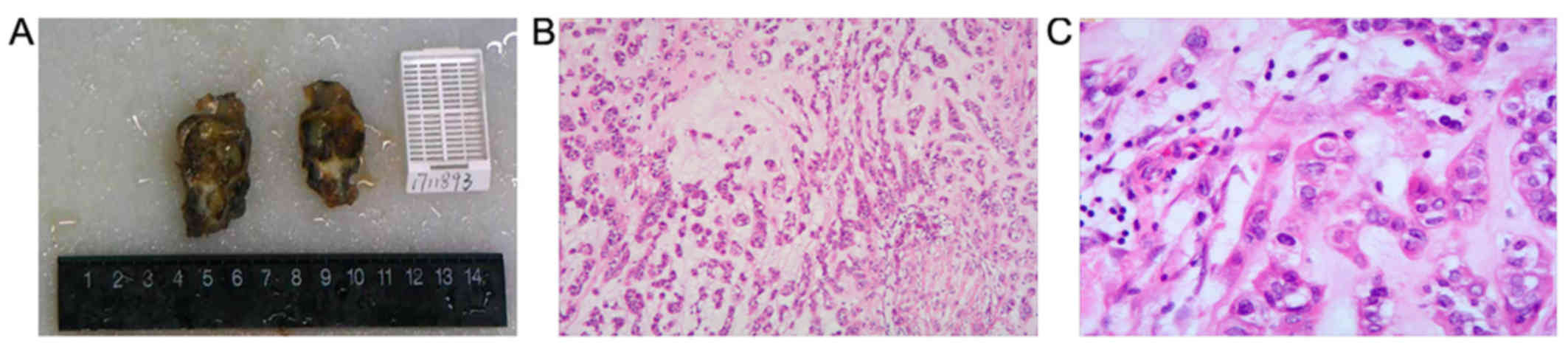
On gross examination, the lesion was composed of two
masses with a fibrous capsule (Fig.
2A). Microscopically, the postoperative histological
examination confirmed the mass as an ACT, consisting of a
parachordoma coexisting with a ganglioneuroma. The larger mass was
composed of fibrocartilaginous matrix and tumor cells arranged in a
funicular or adenoid duct pattern, with pale red cytoplasm, without
mitotic figures (Fig. 2B). The
smaller mass was mainly composed of ganglion cells and
spindle-shaped nerve fibers, and the tumor cells did not exhibit
any heteromorphism (Fig. 2C).
Immunohistochemical staining revealed that S-100, cytokeratin,
synaptophysin (Syn), calponin and chromogranin A (CgA) were
positive in the parachordoma, whereas S-100, Syn, calponin and CgA
were positive in the ganglioneuroma. The postoperative recovery was
uneventful, and there were no abnormalities on the 3-month
postoperative radiographic follow-up examination.
Discussion
ACTs are defined as two or more biologically
distinct tumor types occurring simultaneously without admixture in
the adrenal gland (8). Thus far,
nearly 100 cases of ACTs have been reported (1); however, to the best of our knowledge,
this is the first report of an ACT consisting of a parachordoma
coexisting with a ganglioneuroma. However, the actual prevalence of
ACTs remains unclear (2). Although
some hypotheses have been suggested, the pathogenesis of ACTs is
currently under investigation (2,4,9).
Parachordoma is a rare soft tissue tumor, and its
origin remains unknown (10).
Parachordoma was initially described as ‘chordoma periphericum’ by
Lawskowski in 1951 (11). According
to reports in the literature, the clinical manifestations of
parachordoma mainly include a painless mass of varying size and the
imaging findings are non-specific. Thus, parachordoma is difficult
to diagnose by preoperative imaging alone (7). According to the WHO International
Classification of Diseases for Oncology, parachordoma is an
intermediate tumor with local invasive potential (7). At present, the main treatment for
parachordoma is surgical resection. Due to the possibility of local
recurrence and metastasis after surgical resection (12), regular postoperative follow-up should
be performed. Overall, the prognosis is good following surgical
resection.
Similarly, the prevalence of adrenal ganglioneuroma
is also unclear (9,13). Ganglioneuromas are infrequent benign
tumors, which often manifest as a well-demarcated masses, and are
composed of mature Schwann cells, nerve fibers and ganglion cells
(14). Thus, they seldom develop
local recurrence or distant metastasis (15).
In conclusion, parachordoma and ganglioneuroma are
infrequent components of ACTs. Histopathological examination is the
gold standard for diagnosis. Although parachordoma and
ganglioneuroma are usually benign, they have malignant
transformation potential. Thus, a detailed evaluation of the
patient to detect tumor spread is necessary, including laboratory,
endocrine and imaging studies. After excluding surgical
contraindications, surgical treatment is the preferred option for
patients with a mass of ≥4 cm in size, or if there is a suspicion
of malignant transformation, such as newly emerging hormonal
symptoms or abnormal endocrine function results. Moreover,
postoperative follow-up is crucial for detecting any local
recurrence and distant metastasis at an early stage. In general,
the prognosis of ACTs with coexisting benign tumors is good, and
the focus should be placed on excluding the possibility of
malignant transformation. Malignant tumors, such as kidney cancer
and metastatic tumors, must also be included in the differential
diagnosis. The coexistence of parachordoma and ganglioneuroma in
the left adrenal gland as an ACT is unprecedented. Clinically, two
different types of tumors, which coexist, may be encountered, which
may complicate the diagnosis, and may even lead to misdiagnosis.
Therefore, it is important to distinguish ACTs from other types of
adrenal masses.
Acknowledgements
Not appicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no.81101922), the
Science and Technology Development Fund Project of Shenzhen (grant
nos. JCYJ20150403091443329 and JCYJ20170307111334308), the fund of
‘San-ming’ Project of Medicine in Shenzhen and the fund of
Guangdong Key Medical Subject.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LN and YL conceived and designed the study. JH, WL
and LC collected literature data and clinical information. YL and
LZ drafted and edited the manuscript. All the authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent
preoperatively.
Consent for publication
The reported case has been approved by the patient
for academic exchange only.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee HS, Choi YJ, Kim C and Kim BH: Adrenal
collision tumor: coexistence of pigmented adrenal cortical
oncocytoma and ganglioneuroma. Case Rep Surg.
2016:57906452016.PubMed/NCBI
|
|
2
|
Schwartz LH, Macari M, Huvos AG and
Panicek DM: Collision tumors of the adrenal gland: Demonstration
and characterization at MR imaging. Radiology. 201:757–760. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sung CT, Shetty A, Menias CO, Houshyar R,
Chatterjee S, Lee TK, Tung P, Helmy M and Lall C: Collision and
composite tumors; radiologic and pathologic correlation. Abdom
Radiol (NY). 42:2909–2926. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Siddiqi AJ, Miller FH, Kasuganti D and
Nikolaidis P: Adrenal hemangioma-adenoma: An exceedingly rare
adrenal collision tumor. J Magn Reson Imaging. 29:949–952. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Herr K, Muglia VF, Koff WJ and Westphalen
AC: Imaging of the adrenal gland lesions. Radiol Bras. 47:228–239.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Elsayes KM, Mukundan G, Narra VR, Lewis JS
Jr, Shirkhoda A, Farooki A and Brown JJ: Adrenal masses: Mr imaging
features with pathologic correlation. Radiographics. 24 Suppl
1:S73–S86. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ghanta RK, Uppin MS, Koti K, Hui M, Uppin
SG and Mukherjee KK: Primary intracranial Parachordoma: An unusual
tumor in brain. Surg Neurol Int. 5 Suppl 14:S506–S511. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Untch BR, Shia J, Downey RJ, Carrasquillo
JA, Panicek DM and Strong VE: Imaging and management of a small
cell lung cancer metastasis/adrenal adenoma collision tumor: A case
report and review of the literature. World J Surg Oncol. 12:452014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Katabathina VS, Flaherty E, Kaza R, Ojili
V, Chintapalli KN and Prasad SR: Adrenal collision tumors and their
mimics: Multimodality imaging findings. Cancer Imaging. 13:602–610.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Clabeaux J, Hojnowski L, Valente A and
Damron TA: Case report: Parachordoma of soft tissues of the arm.
Clin Orthop Relat Res. 466:1251–1256. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dabska M: Parachordoma: A new
clinicopathologic entity. Cancer. 40:1586–1592. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Samaka RM and Kandil MA: Huge pelvic
parachordoma: Fine needle aspiration cytology and histological
differential diagnosis. Rare Tumors. 4:e532012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Qing Y, Bin X, Jian W, Li G, Linhui W,
Bing L, Huiqing W and Yinghao S: Adrenal ganglioneuromas: A 10-year
experience in a Chinese population. Surgery. 147:854–860. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou Y, Liang Q, Ou WT, Li ZY and Liu QL:
Laparoscopic resection of primary adrenal ganglioneuroma: A case
report and review of the literature. Oncol Lett. 9:2167–2170. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Srinivasan R, Koliyadan KS, Krishnand G
and Bhat SS: Retroperitoneal ganglioneuroma with lymphnode
metastasis: A case report. Indian J Pathol Microbiol. 50:32–35.
2007.PubMed/NCBI
|