Introduction
Myositis ossificans (MO) is a benign condition
characterized by abnormal heterotopic bone formation, typically
involving striated muscle and soft tissue (1). In 1924, Noble (2) classified MO into myositis (fibrous)
ossificans progressiva, traumatic MO circumscripta, and atraumatic
MO circumscripta. The latter includes the more descriptive
pseudomalignant as well as idiopathic forms (2). MO is most commonly found in muscle
tissue as a solitary lesion (3).
Myositis ossificans can be categorized into nonhereditary and
hereditary types, with the latter being a distinct entity with a
separate pathophysiology and treatment approach (4). The pathophysiology of MO formation is
incompletely understood. Kan et al (5) demonstrated that the cellular mechanism
of heterotopic bone formation is the result of local stem cell
dysregulation in response to tissue injury and subsequent
inflammation. Recent studies have demonstrated that extra-skeletal
bone formation may be dependent on a process known as
endothelial-mesenchymal transition (4,5). The
clinical presentation of MO is variable. MO has been reported to
occur in all ages, including the very young (as young as 1 year of
age) and in atypical locations, including the hands, feet, ribs,
head, and neck (6). Patients may
present atypically, especially when the history is not clear. This
atypical clinical presentation, combined with nonspecific imaging
findings, often raises concerns of malignancy (4–6). MO
often starts as a non-specific painful soft tissue mass that could
be mistaken for an infection or a soft tissue tumor. Therefore,
some authors have suggested using the more descriptive term
‘pseudomalignant’ MO (7,8). We report on an unusual pseudomalignant
form of myositis ossificans in the breast.
Case report
A 31-year-old Caucasian woman with no significant
previous medical history was referred to the Breast Unit of the 2nd
Department of OB/GYN, University Hospital of Bratislava, Slovakia,
for assessment of a growing lump in her right breast. The prominent
lump was in the upper, inner quadrant of the breast, near the
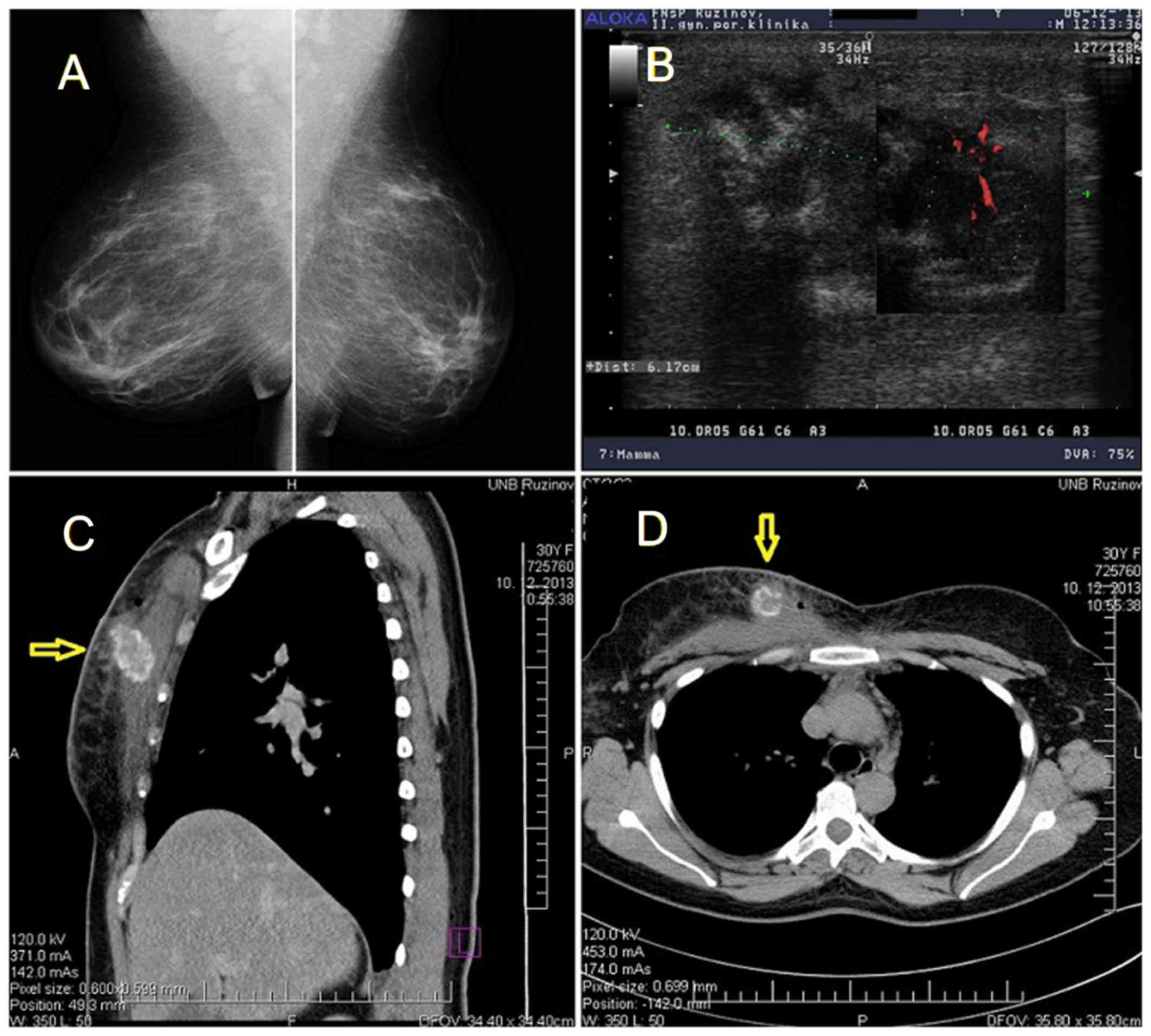
infraclavicular region, and fixed to the chest wall. Mammography
was ineffective at visualizing the lesion because of its location,
however, the remaining breast parenchyma was tumor free (Fig. 1A). Breast ultrasonography revealed an
oval-shaped, low-echoic tumor of unclear etiology with a
pathological pattern of blood flow, as seen on Power-Doppler
imaging (Fig. 1B). Infiltrating
ductal carcinoma could not be excluded. Because the tumor was fixed
to the chest wall, a computed tomography scan of the chest was
ordered. CT showed a tumor mass with ossification signs on the
upper chest wall that appeared to be continuous with the right
pectoralis major muscle (Fig. 1C and
D). A core biopsy was performed on the palpable mass. A
malignant form of a spindle cell tumor was suspected.
The patient underwent breast surgery, with
anticipated en bloc resection of the underlying parts of thoracic
wall, at the Department of Thoracic Surgery, University Hospital of
Bratislava, Slovakia. Surgery was performed under general
anesthesia and consisted of an quadrantectomy with en bloc
resection of the underlying musculature (superior medial part of
the right pectoralis major muscle).
The surgically removed specimen was lobulated and
measured 5.5×4.5×4.0 cm in size, containing a 4.5×3.2×3.0 cm
grossly circumscribed, capsulated firm tumor, which had infiltrated
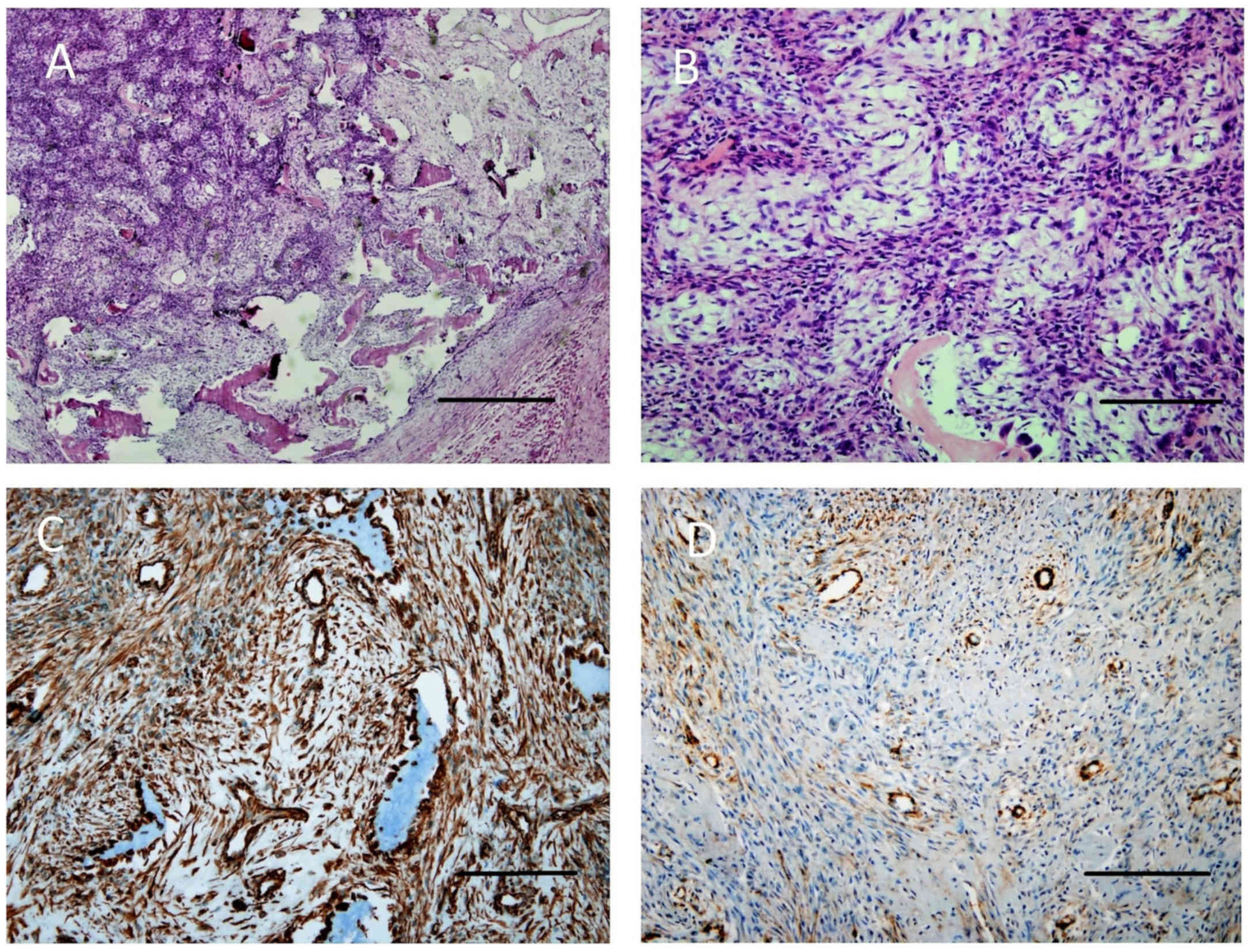
the surrounding fat and musculature. Histologic evaluation of the
surgical specimens revealed nodular proliferation of spindle cells
with characteristic centripetal zonation of ossification and giant
osteoclasts-like cells. Osteoblastic activity with marginally
mature lamellar bone was present, without atypical mitoses
(Fig. 2A and B). A definitive
diagnosis of a tumorous form of myositis ossificans was established
from serial paraffin sectioning and immunohistochemistry (IHC).
Immunostaining with anti-vimentin and anti-alpha smooth muscle
actin (SMA) antibodies was positive (Fig. 2C and D), while IHC analysis with
anti-cytokeratins, anti-EMA, and anti-desmin antibodies was
negative. Tests for diffuse steroid receptors (estrogen and
progesterone receptor) were also negative. The index of Ki67
proliferative activity was positive in 10% of cells. The patient's
post-operative course was uneventful; she was discharged to home on
post-operative day seven. The patient is now 48 months
post-procedure and remains disease free.
Discussion
MO is essentially metaplasia of the intramuscular
connective tissue resulting in extraosseous bone formation
(8,9). Histologically, the lesions exhibit a
wide range of histologic features with different amounts of
immature fibroblastic cells, osteoid, cartilage, and young or
mature bone accompanied by fibrous connective tissue (4,10,11).
Sumiyoshi et al (1), in their
clinicopathologic study of 21 cases, classified MO into three types
according to the predominant or most striking histologic features.
Type I (6 cases) was characterized by highly cellular areas with
islands of osteoid, which can occasionally be confused with
extra-skeletal osteogenic sarcoma. Type II lesions (8 cases)
consisted mainly of osteoid and young bone rimmed by osteoblasts,
with the occasional presence of cellular areas. Type III lesions (7
cases) were made up, almost wholly, of mature bone and cartilage
surrounded invariably by dense fibrous connective tissue. The
prognosis was excellent in the 17 patients for whom follow-up
information was available (1).
A biopsy is necessary to confirm the diagnosis of
indeterminate lesions (1,4,12,13). Due
to the presence of bone formation as well as a similar
epidemiology, osteosarcoma needs to be excluded. An important
feature is the characteristic zonation in myositis ossificans,
which is in contrast to the lace-like disorderly growth of osteoid
bone formations in osteosarcomas (5,14). Small
biopsies can be difficult to interpret since zonation is usually
not present (14).
Surgical excision is generally reserved for
symptomatic MO lesions (15).
However, since recurrence has been reported, excision with clear
resection margins is recommended (10,15).
Because of the infiltration of the MO tumor into the chest wall in
our patient, a thoracic surgeon (M.J.) was part of our surgical
team.
Tumorous forms of MO in the breast are very rare.
Salomonowitz et al (16)
reported the first case in a healthy 21-year-old female who
developed a rapidly growing mass in her left breast, which proved
to be a non-progressive form of MO that had originated in fat
tissue. Clinically, the tumor measured more than 6 cm in length and
showed all the signs of carcinoma. In 2004, Alonso Calderón et
al (17) described a 15-year-old
girl with atraumatic MO circumscripta in the axillary region. A
case of MO in the pectoralis muscle, associated with an
extracapsular silicone implant rupture has also been described
(18).
Brown and Carty (19)
described a case of nodular fasciitis of the breast (a benign
pseudosarcomatous proliferative lesion of the soft tissue) in a
65-year-old previously healthy woman who was referred to their
breast clinic with a one-month history of a lump in her left breast
lying against the pectoral muscle. A similar case was also recently
reported by Choi et al (20).
Fasciitis ossificans of the breast, a rare subtype of nodular
fasciitis, was described by Sato et al (21) and Su et al (22). Simple excision, not radical
resection, was recommended and was sufficient for a definite
histological diagnosis and therapy because neither fasciitis
ossificans nor nodular fasciitis generally recur and no
transformations to sarcoma have been reported (20–22).
In the differential diagnosis of heterotopic bone
forms in soft tissues, fibrodysplasia ossificans progressiva (FOP)
comes into consideration. The disease is an ultra-rare genetic
disorder (23). Classic FOP is
caused by a recurrent activating mutation (617G>A; R206H) in the
ACVR1/ALK2 gene encoding activin A receptor type I/activin-like
kinase 2, which is a bone morphogenetic protein (BMP) type I
receptor. Atypical FOP patients also have heterozygous ACVR1
missense mutations in conserved amino acids (24). A diagnosis of FOP is made through
clinical evaluation. Suspicion of FOP early in life, on the basis
of malformed great toes, can lead to an early clinical diagnosis.
During the first decade of life, sporadic episodes of painful soft
tissue swellings occur and are commonly mistaken for tumors;
confirmatory genetic testing is now available (23,24).
In conclusion, MO in the breast region is rare.
Since it is so rare, the present case study stands out as a
noteworthy case with unique clinical features and histological
findings.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KP performed the patient's examination, breast
imaging, interventional breast procedures, breast surgery, and
analyzed and interpreted the patient data regarding the disease. KP
was a major contributor in writing the manuscript. MJ performed the
final breast surgery. IM performed the histological examination of
the core needle biopsy, surgical specimens, and analyzed and
interpreted the patient data regarding the histology. FO assisted
with the histological findings of the surgical specimens.
Ethics approval and consent to
participate
Written informed consent was obtained for patient
participation.
Consent for publication
Written informed consent was obtained from patients
for the publication of all associated data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sumiyoshi K, Tsuneyoshi M and Enjoji M:
Myositis ossificans. A clinicopathologic study of 21 cases. Acta
Pathol Jpn. 35:1109–1122. 1985.PubMed/NCBI
|
|
2
|
Noble TP: Myositis ossificans: A clinical
and radiological study. Surg Gynecol Obstet. 39:7951924.
|
|
3
|
Kransdorf MJ, Meis JM and Jelinek JS:
Myositis ossificans: MR appearance with radiologic-pathologic
correlation. AJR Am J Roentgenol. 157:1243–1248. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Walczak BE, Johnson CN and Howe BM:
Myositis Ossificans. J Am Acad Orthop Surg. 23:612–622. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kan L and Kessler JA: Evaluation of the
cellular origins of heterotopic ossification. Orthopedics.
37:329–340. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ogilvie-Harris DJ and Fornasier VL:
Pseudomalignant myositis ossificans: Heterotopic new-bone formation
without a history of trauma. J Bone Joint Surg Am. 62:1274–1283.
1980. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rööser B, Herrlin K, Rydholm A and Akerman
M: Pseudomalignant myositis ossificans. Clinical, radiologic, and
cytologic diagnosis in 5 cases. Acta Orthop Scand. 60:457–460.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nuovo MA, Norman A, Chumas J and Ackerman
LV: Myositis ossificans with atypical clinical, radiographic, or
pathologic findings: A review of 23 cases. Skeletal Radiol.
21:87–101. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tyler P and Saifuddin A: The imaging of
myositis ossificans. Semin Musculoskelet Radiol. 14:201–216. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mavrogenis AF, Soucacos PN and
Papagelopoulos PJ: Heterotopic ossification revisited. Orthopedics.
34:1772011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Micheli A, Trapani S, Brizzi I, Campanacci
D, Resti M and de Martino M: Myositis ossificans circumscripta: A
paediatric case and review of the literature. Eur J Pediatr.
168:523–529. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wakely PE Jr, Almeida M and Frable WJ:
Fine-needle aspiration biopsy cytology of myositis ossificans. Mod
Pathol. 7:23–25. 1994.PubMed/NCBI
|
|
13
|
Klapsinou E, Despoina P and Dimitra D:
Cytologic findings and potential pitfalls in proliferative myositis
and myositis ossificans diagnosed by fine needle aspiration
cytology: Report of four cases and review of the literature. Diagn
Cytopathol. 40:239–244. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ng VWL: Pseudosarcomatous soft tissue
lesions: A review. Proc Singap Healthc. 19:220–228. 2010.
View Article : Google Scholar
|
|
15
|
Adebayo ET, Ayuba GI, Ajike SO and Fomete
B: Myositis ossificans of the platysma mimicking a malignancy: A
case report with review of the literature. J Korean Assoc Oral
Maxillofac Surg. 42:55–59. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Salomonowitz E, Youssefzadeh S, Reiner A,
Heilbron EA and Zollikofer CL: Nontraumatic myositis ossificans in
the breast. Eur J Radiol. 12:130–131. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Calderón Alonso JL, Valdueza Delgado J and
Vicente Deprada I: Myositis ossificans circumscripta in the axilla.
An Pediatr (Barc). 60:373–375. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mugea TT and Schiffman MA: Aesthetic
Surgery of the Breast. Springer Verlag; Berlin, Heidelberg:
2015
|
|
19
|
Brown V and Carty NJ: A case of nodular
fascitis of the breast and review of the literature. Breast.
14:384–387. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Choi HY, Kim SM, Jang M, Yun BL, Ahn HS,
Park SY, Kim SW and Kang EY: Nodular fasciitis of the breast: A
case and literature review. Ultraschall Med. 36:290–291.
2015.PubMed/NCBI
|
|
21
|
Sato K, Oda Y, Ueda Y and Katsuda S:
Fasciitis ossificans of the breast. Pathol Res Pract. 203:737–739.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Su TF and Chen A: Fasciitis ossificans of
the breast. Breast J. 20:429–430. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pignolo RJ, Shore EM and Kaplan FS:
Fibrodysplasia ossificans progressiva: Clinical and genetic
aspects. Orphanet J Rare Dis. 6:802011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wentworth KL, Bigay K, Chan TV, Ho JP,
Morales BM, Connor J, Brooks E, Salamat Shahriar M, Sanchez HC,
Wool G, et al: Clinical-pathological correlations in three patients
with fibrodysplasia ossificans progressiva. Bone. 17:S8756–3282.
2017.
|