Introduction
Extraskeletal osteosarcoma (ESOS) is a rare subtype
of osteosarcoma, with which patients affected have distinct
clinical features but similar prognostic factors and poor outcome
compared to primary skeletal osteosarcoma (1), and its' management principles are not
well defined and even conflicting, multimodality treatment remains
standard (2–4). ESOS originating in the subcutaneous
tissue is a rare occurrence, accounting for <10% of all ESOS
cases (5,6). We present a case of ESOS primary in
subcutaneous tissue of the right neck with which treated by both
local resection and radiotherapy being relapsed several times (a
brief summary of therapy on the patient see Table I).
 | Table I.Summary of the therapy received by the
patient with extraskeletal osteosarcoma in right-hand neck
subcutaneous tissue. |
Table I.
Summary of the therapy received by the
patient with extraskeletal osteosarcoma in right-hand neck
subcutaneous tissue.
| Therapy details | First surgery | Second surgery | Radiotherapy | Third surgery | Fourth surgery |
|---|
| Date of therapy | June 4, 2014 | July 3, 2015 | From August 3 to | February 20,
2017 | July 7, 2017 |
| Therapeutic
method | Local widely
resection | Partial
resection | September 22, 2015
SMART | Partial
resection | Partial
resection |
|
|
|
| CTV1:
60.16Gy/1.88Gy/32f |
|
|
|
|
|
| CTV2:
70.08Gy/2.19Gy/32f |
|
|
| Pretreatment
diagnosis | Primary subcutaneous
ESOS in right neck | Postoperative
recurrence | Postoperative
recurrence | Local recurrence | Local recurrence |
| Tumor size (CT or
INOPF) | INOPF: 4.0×3.0×3.0
cm | CT: 2.9×1.9×1.7
cm | CT: 2.6×1.6×1.4 cm
(Following radiotherapy) | CT: 8.8×6.0×5.4 cm
Excisions contains of multiple tissue fragments | CT: 9.2×6.6×5.3 cm
INOPF: 10.0×6.0×6.0 cm |
| Therapeutic
effect | Incompletely
removed | Partial resected | RECIST: SD. Acute
radioactive skin injury | Following 3 months,
the mass enlarged with trachea compression | Partial removed (the
resected mass: 6.0×3.0×3.0 cm), with trachea compression
relieved |
Case report
Patient case
An 81-year-old man admitted to our hospital on May
26, 2014, presented with two weeks history of a mass founded on the
right side of the neck, suffering with dull pain and swallowing;
the patient provided written informed consent for participation in
the present study. There was no history of any surgical procedure,
trauma, local radiation exposure in head and neck, any long-term
medication or addictions. There was no clinical evidence of
metastatic disease. His family history and general physical
examination was unremarkable. On physical examination, a
hard-mobile subcutaneous mass approximately 4.0×3.0 cm was palpable
on the right side of the neck which moved with a slight tenderness.
bilateral neck swollen lymph nodes were not touched. Karnofsky
performance score (KPS) was 90. Blood count, serum alkaline
phosphatase and tumor markers such as CEA and AFP were normal. CT
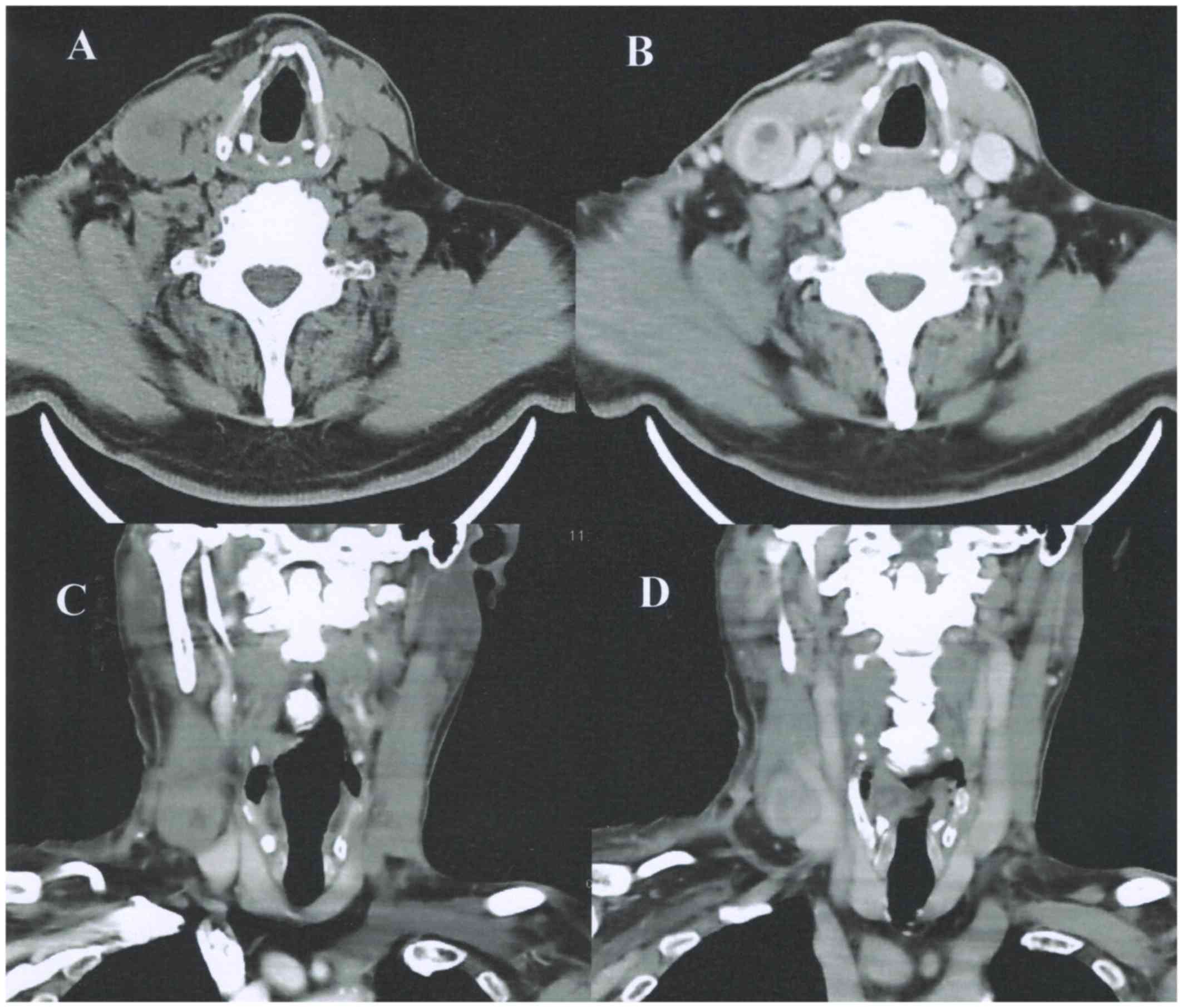
(Fig. 1) scan revealed an uneven
density soft tissue masses is of about 4.1×3.0×2.8 cm size in the
rear of sternocleidomastoid on the right neck (Fig. 1A and C), contrast-enhanced CT (CECT)
shows the mass peripherally enhanced with the necrosis in the
center area, adjacent sternocleidomastoid and the right internal
jugular vein were showed displaced (Fig.
1B and D).
First operation
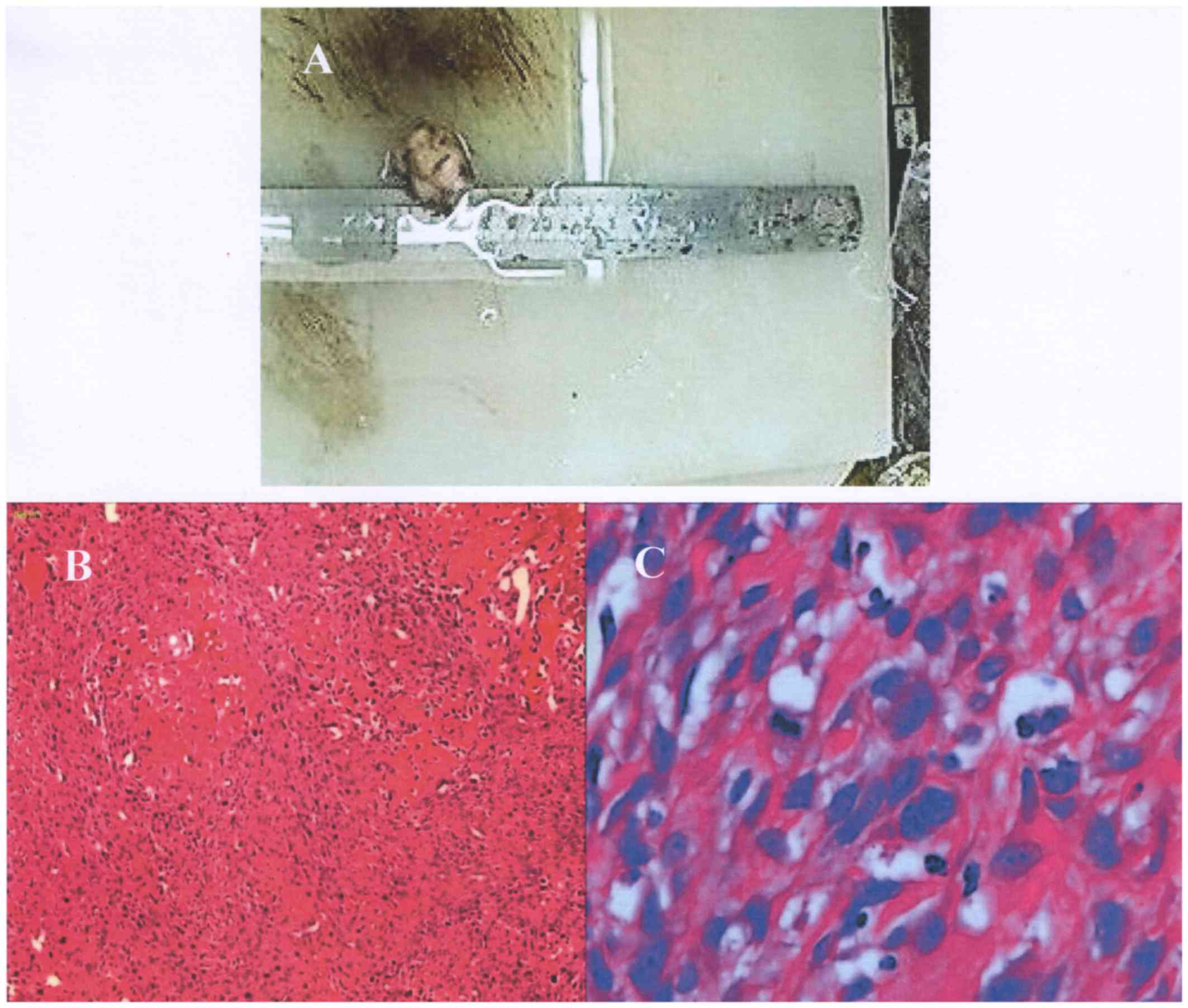
A local widely resection was done on this patient in
June 4, 2014. The operative procedure was performed under general
anaesthesia, a subcutaneous mass with the size of about 4.0×3.0×3.0
cm was visible in the operation (Fig.
2A), and the tumour was incompletely removed as it closely
related to the right jugular vein. On microscopy shows the resected
mass consists of spindle, small round cells, with the nuclei
hyperchromatic and pleomorphism, and neoplastic cartilage formation
is seen (Fig. 2B and C),
postoperative pathological diagnosis was as ESOS. The patient was
unwilling to undergo chemotherapy or local radiotherapy after the
operation.
Second operation and radiotherapy
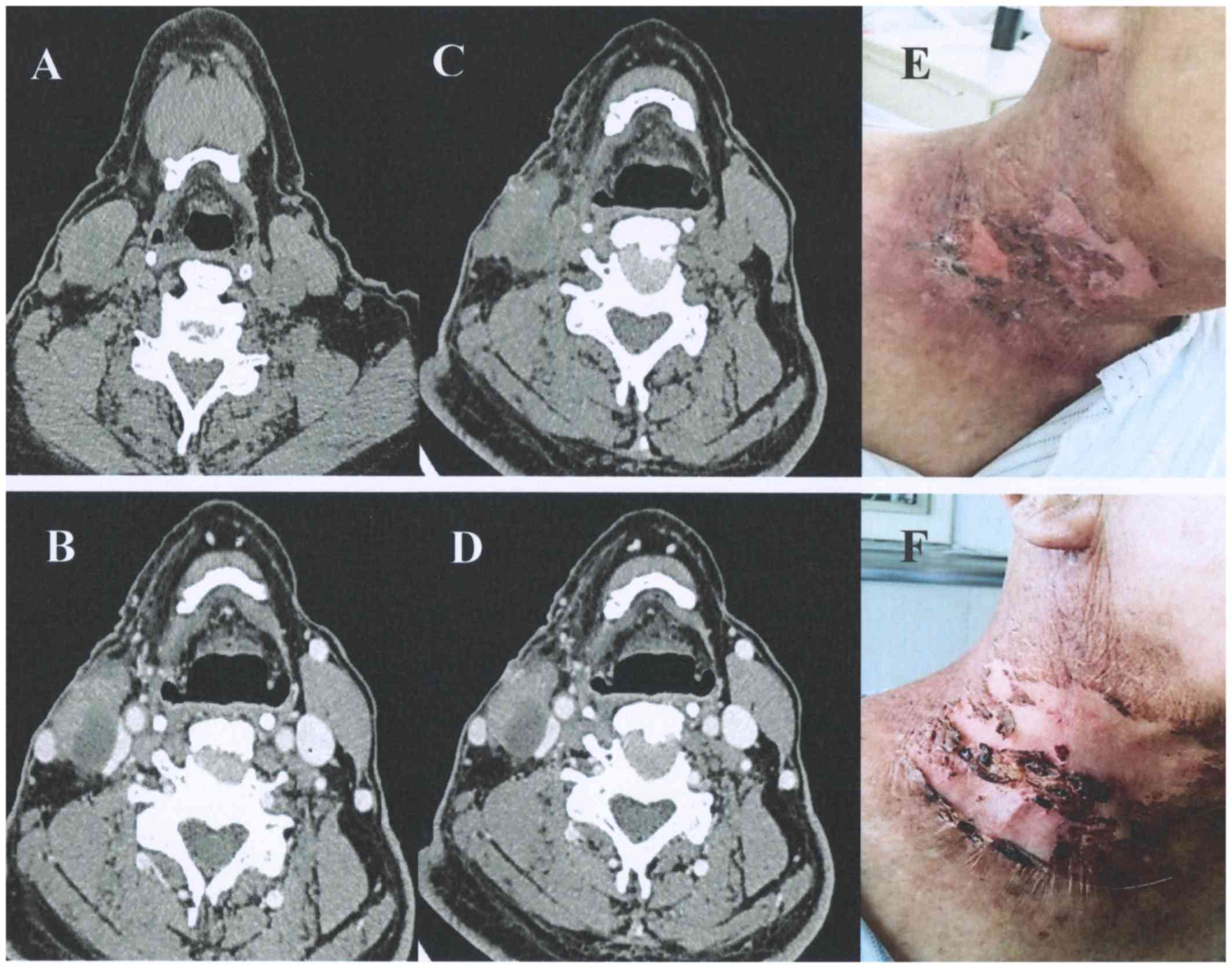
Ten months later, On June 29, 2015, the patient was
admitted to hospital again for ‘postoperative and recurrence’ of
the right cervical osteosarcoma (Fig. 3A
and B). A partial resection of the right neck mass was
performed on July 3, 2015 (the second operation), and the
postoperative pathology report indicated that the osteosarcoma of
the right neck was recurred. Four weeks later, the patient
underwent postoperative simultaneous modulated accelerated
radiotherapy (SMART). The prescribed dose of CTV1 and CTV2 was
60.16 Gy/32 fractions and 70.08 Gy/32 fractions respectively, both
once daily. 6 weeks after the radiotherapy, CT were performed to
assess RT effects (Fig. 3C and D)
was as stable disease (SD) according to the RECIST 1.1 criteria.
During the period of RT, acute radioactive skin injury (level 2)
occurred in the right neck skin (Fig. 3E
and F) according to RTOG acute radiation injury classification
criteria.
Third operation
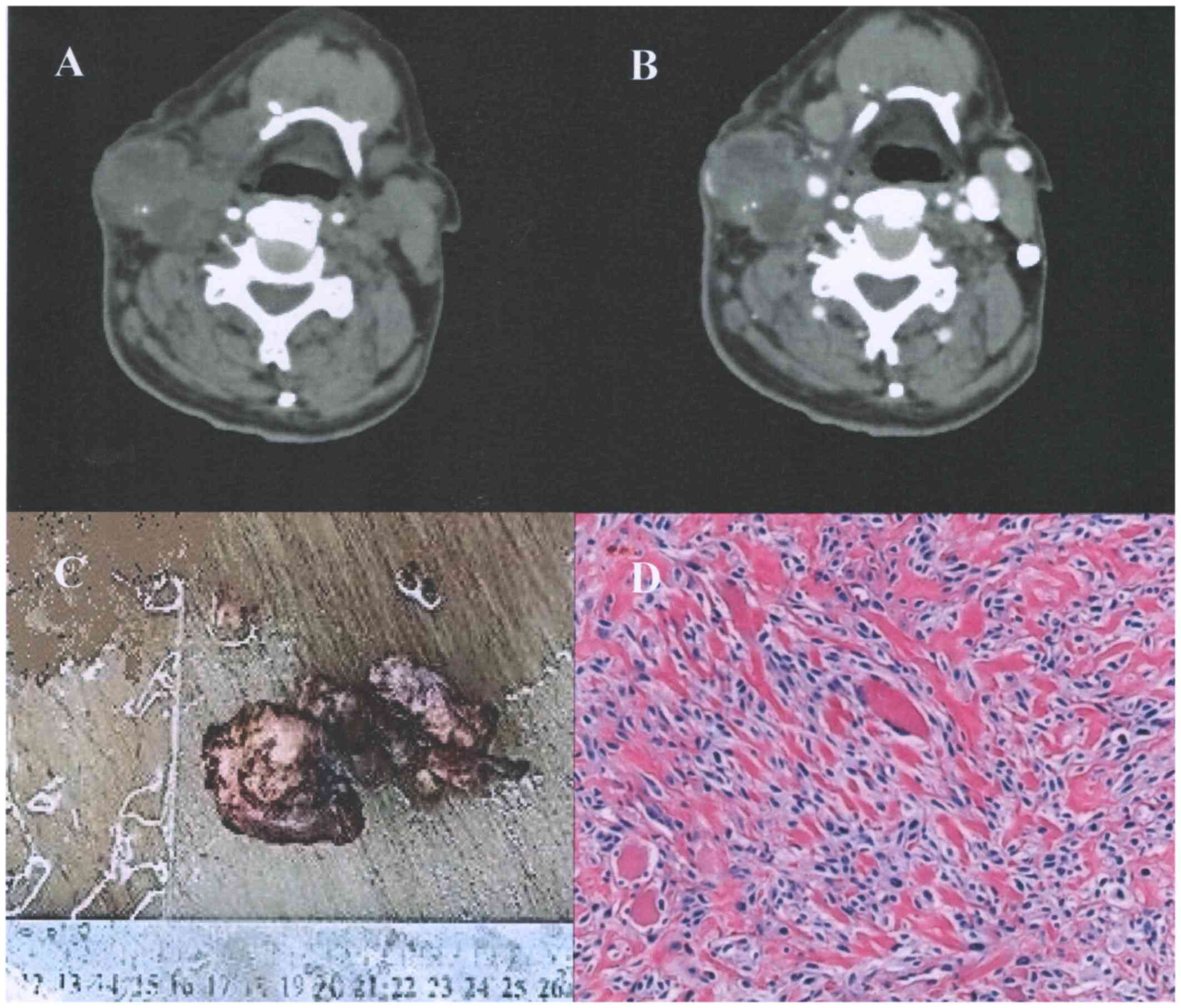
The neck neoplasm to be founded increasing again
from January 2017, with painful and obvious when swallowing, a mass
was touched in the right neck, with mild tenderness and activity,
CT showed recurrence (Fig. 4A and
B). On February 20, 2017, the patient underwent the right neck
neoplasm resection in condition of the resting compound anesthesia
(the third operation). Postoperative pathological biopsy results
showing (Fig. 4C and D): Neoplasm
composed of spindle cells with nuclear atypia, nucleolus is clear,
and multinucleated giant cells could be seen, nuclear fission is
obvious, osteoid matrix is not obvious, and infringement of
striated muscle tissue around them.
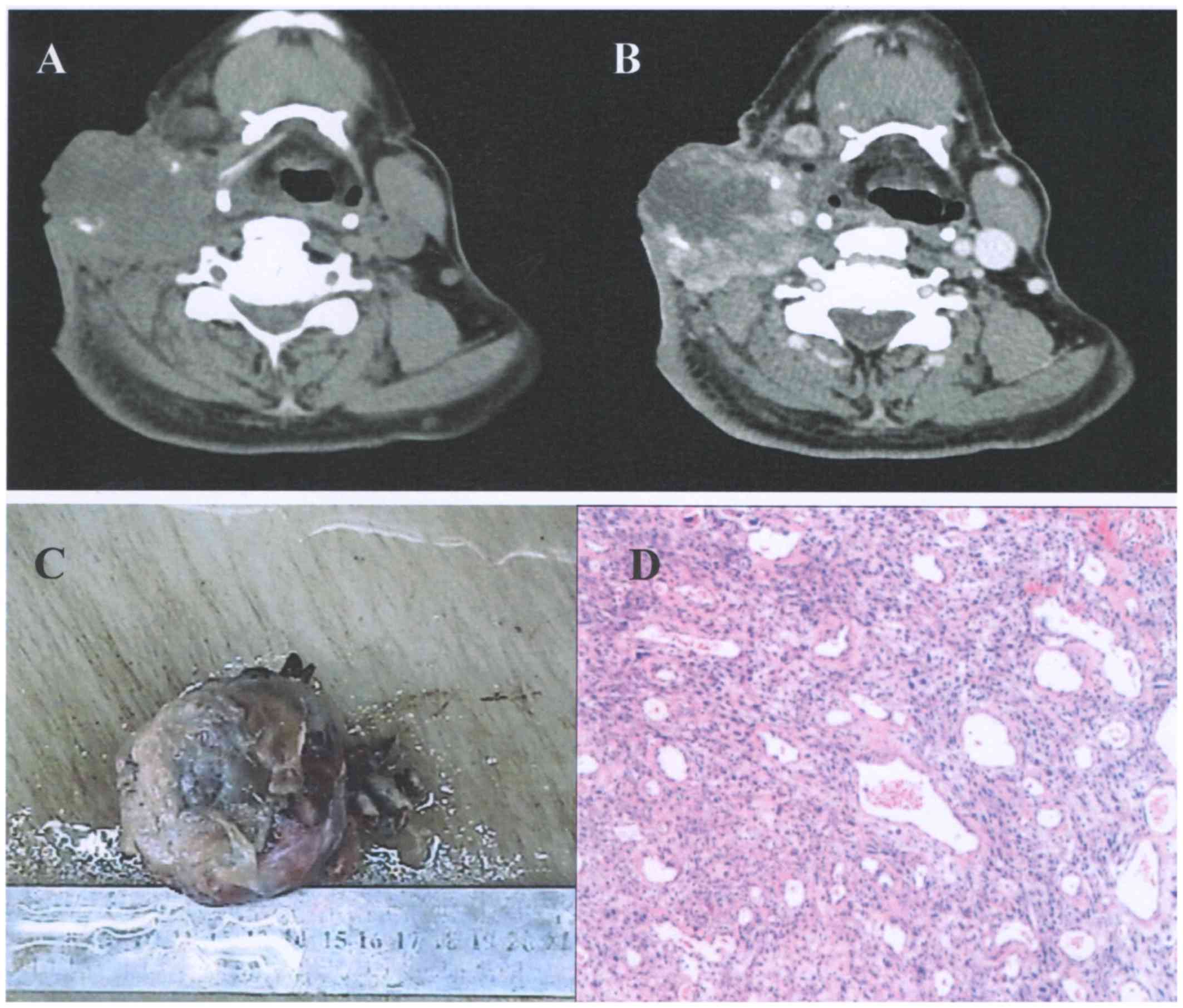
 | Figure 4.(A) CT scan showing an enlarged mass
of ~8.8×6.0×5.4 cm, with n increased density on the right-hand side
of the neck. (B) Contrast-enhanced CT revealed the mass was
enhanced in homogeneity, with a fuzzy surrounding fat gap, adjacent
skin thickening and a moderately enhanced nature. (C) Surgical
excision contains multiple tissue fragments. (D) Hematoxylin and
eosin staining (magnification, ×200). The tumor was composed of
spindle cells, nuclear heteromorphism, nucleolus clarity, multiple
nuclear giant cells, nuclear fission, the osteoid matrix was not
obvious, and the surrounding rhabdomyosis was infringed. CT,
computed tomography. |
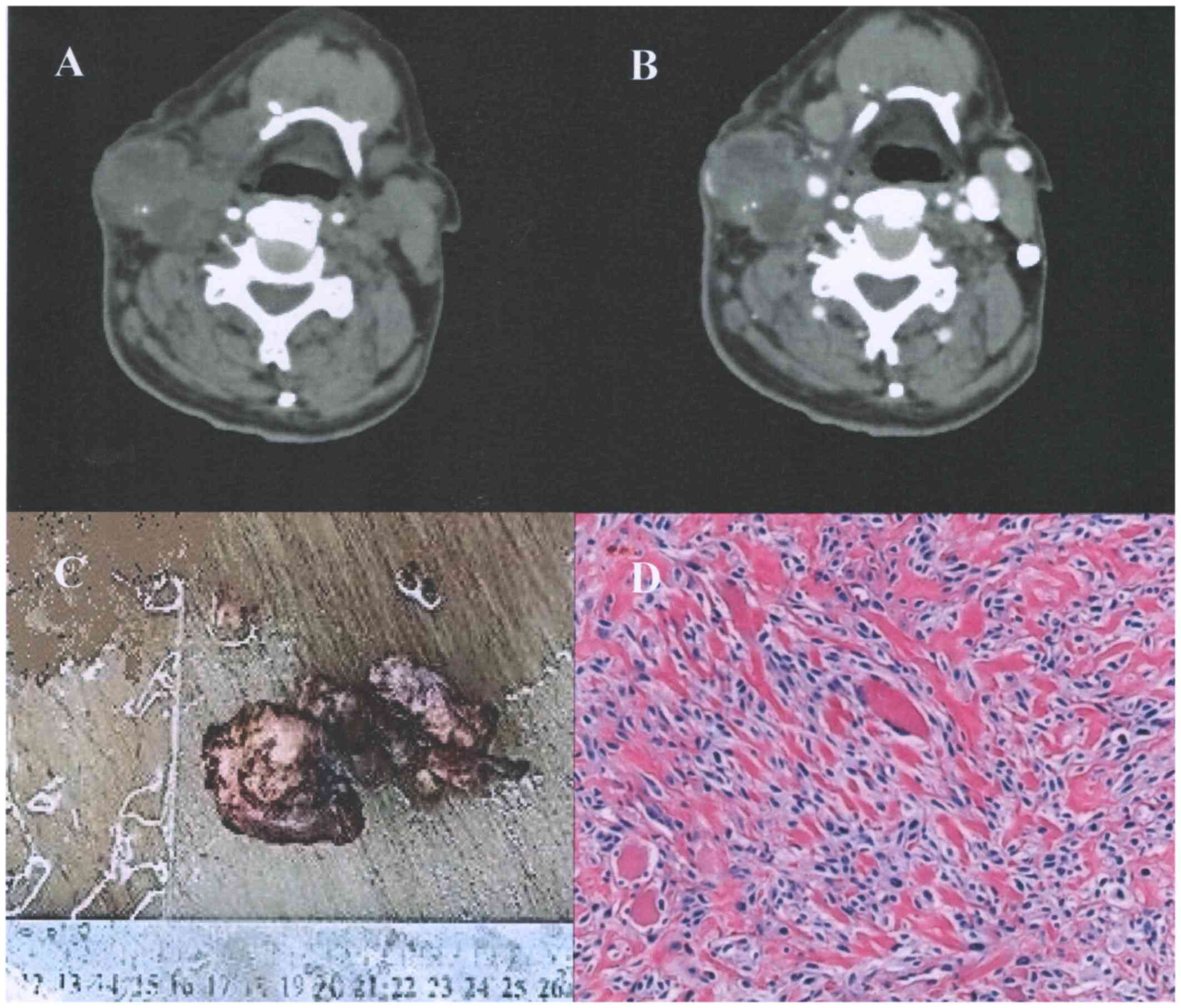
Fourth Operation and the
follow-up
July 7, 2017, the patient underwent the partial
resection for the mass enlarged once more with trachea compression,
and damaged the skin. Partial mass with the range of about
6.0×3.0×3.0 cm was resected (Fig.
5). The patient is alive till now.
Discussion
Skeletal osteosarcoma (ESOS), also named as soft
tissue osteosarcoma, is a rare malignant soft tissue sarcoma with
histologic similarities to primary bone osteosarcoma but without
attachment to the bone or periosteum, with malignant osteoid or
bone (or both) formation and a uniform morphological sarcomatous
tissue patterns (1). ESOS is a rare
malignancy that the morbidity accounts for about 1 to 2% of all
soft tissue sarcomas (1,7), and less than 4% of all osteosarcomas
(7,8). Most of the ESOS occur in the upper and
lower extremity, with the proportion of ~40.0–67.5 (1,9) to ~85.7
−88.7% (4,10), but very few occur in the head and
neck, with the constituent ratio is ~2.5-3% (9,11) to
~5-7.3% (1,3). These tumors generally arise with a high
incidence of the median age is ~57-60.7 years (1,10), which
usually located in the deep soft tissues without attachment to
skeletal bones but were firmly attached to the fascia (12). This case of primary ESOS occurs in
subcutaneous on the right side of the neck is exceedingly rare,
which underwent four times of the operation, followed by once
postoperative radiotherapy, but relapse for several times.
ESOS patients starting symptoms tend to be
progressive enlargement of tumors and rarely causing pain or
tenderness, the preoperative duration of symptoms ranged from 2
weeks to 25 years (median, 6 months) (12). But ESOS could firstly manifest as
spontaneous tumor lysis syndrome which represents an oncological
emergency must be treated as soon as possible (13). ESOS is a rare mesenchymal malignancy
of soft tissue, histologically indistinguishable from primary
osteosarcoma of bone. However, there are distinct differences in
demographics, imaging features, prognosis, and management compared
with osteogenic osteosarcoma (8),
its correct diagnosis may depend on a combination of clinical,
radiographic, and pathologic findings (8,12,14–16).
There are several treatment methods for ESOS,
including surgery, radiation therapy, and chemotherapy (2–4,10,11),
surgical resection is dominated, 85 to 98% (10,11),
even all patients with localized disease were managed with surgical
resection of the primary tumor (4),
radical resections are effective for local control and have the
best chance of cure for ESOS (8),
5-year OS and 5-year disease-free survival (DFS) was 51.4 and 43%
respectively (10), but the
proportion of patients treated alone with surgery was low (21.8%)
(10), and its effect on distant
metastasis is not so clear, multiagent chemotherapy may be help to
reduce distant metastasis, a trend towards increased length of
survival was found in patients who received chemotherapy compared
to those who did not (16.4 months vs. 9.3 months) (2), the gemcitabine-docetaxel chemotherapy
regimen was considered as well-tolerated and induced a long lasting
partial response for ~14 months in the treatment of ESOS (17). Higher survival was observed in
patients who received perioperative chemotherapy with a trend in
favour of multiagent osteosarcoma-type regimen which included
doxorubicin, ifosfamide and cisplatin (10), and postoperative adjuvant external
beam radiotherapy being considered to improve local control rate
and preserve organ function (18,19), and
especially the patients who with tumour >5 cm and R0 margins
seems to benefit more from RT (10),
and there is a tendency to extend 5-y DFS in patients who underwent
postoperative adjuvant RT compared with surgery alone (66 vs. 42%,
P=0.38) (11), though RT was not
associated with a lower disease-related mortality rate or a longer
event-free survival (4). However,
the available data are contradictory with regard to the use of
chemotherapy and radiotherapy regimens in the management of ESOS,
radiographic response rates and pathologic complete response rates
to doxorubicin-based systemic therapy are low (3), no significant association of
disease-specific or event-free survival was found with the addition
of radiation, chemotherapy, or both to surgery, radiation and
chemotherapeutic treatment were not associated with a lower
incidence of death due to disease or a longer event-free survival
(4). Currently, a multimodality
approach is used to treat extra skeletal osteosarcoma, which
entails incorporation of multidrug chemotherapy and /or
radiotherapy along with the surgery to get the best outcome in
terms of disease specific survival and local relapse free survival
(10). In fact, there are many
factors influence the treatment effects and clinical outcomes of
ESOS, including tumor size, tumor location, pathology
classification and grade, clinical stage, surgical margin, choice
of chemotherapy drugs, age (1,4,7,1),
expression of oncogenes (21,22), and
so on.
In this case of ESOS, lesion located in subcutaneous
on the right side of the neck, in the posterior of the
sternocleidomastoid, with the adjacent sternocleidomastoid and the
right internal jugular vein were displaced, thus, the tumour was
incompletely removed. The postoperative chemotherapy and local
radiotherapy seem to be necessary (2,10,11,2),
but the patient refused the postoperative radiation and
chemotherapy, with the result of the local recurrence after about
nine months of the first operation. In the case, the patient
voluntarily received local radiotherapy after the second operation,
and DFS is about 15 months. Third resection performed when relapsed
again, second course of radiotherapy was not considered for having
had a history of local radiotherapy and an obvious skin injury, but
the patients still refused to chemotherapy, 5 months later, the
patient underwent another operation for relapsed once more.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JSZ participated in the conception and design of the
case report and wrote the manuscript. GW and YL evaluated the
patient, participated in the radiotherapy procedures and were major
contributors in writing the manuscript. ZHW performed the surgical
management procedures and reviewed the manuscript. GDC conducted
the surgical management procedures. HW participated in radiotherapy
and wrote the manuscript. TCZ assisted with the treatment of
radiotherapy and reviewed the manuscript. All authors have read and
approved the final draft.
Ethics approval and consent to
participate
The patient provided written informed consent for
participation in the present study.
Consent for publication
The patient provided written informed consent for
the publication of any associated data and images in this case
report.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ESOS
|
extraskeletal osteosarcoma
|
|
CT
|
computed tomography
|
|
CECT
|
contrast-enhanced CT
|
|
SMART
|
simultaneous modulated accelerated
radiotherapy
|
|
RT
|
radiotherapy
|
|
RECIST 1.1
|
Response Evaluation Criteria In Solid
Tumours version 1.1
|
|
SD
|
Stable disease
|
|
RTOG
|
Radiation Therapy Oncology Group
|
|
CEA
|
carcinoembryonic antigen
|
|
AFP
|
α-fetoprotein
|
|
CTV
|
clinical target volume
|
References
|
1
|
Thampi S, Matthay KK, Boscardin WJ,
Goldsby R and DuBois SG: Clinical features and outcomes differ
between skeletal and extraskeletal osteosarcoma. Sarcoma.
2014:9026202014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nystrom LM, Reimer NB, Reith JD,
Scarborough MT and Gibbs CP Jr: The treatment and outcomes of
extraskeletal osteosarcoma: Institutional experience and review of
the literature. Iowa Orthop J. 36:98–103. 2016.PubMed/NCBI
|
|
3
|
Ahmad SA, Patel SR, Ballo MT, Baker TP,
Yasko AW, Wang X, Feig BW, Hunt KK, Lin PP, Weber KL, et al:
Extrasseous osteosarcoma: Response to treatment and long-term
outcome. J Clin Oncol. 20:521–527. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Choi LE, Healey JH, Kuk D and Bennan MF:
Analysis of outcomes in extraskeletal osteosarcoma: A review of
fifty-three cases. J Bone Joint Surg Am. 96:e22014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Healy C, Kahn BL and Kenan S: Subcutaneous
extraskeletal osteosarcoma of the forearm: A case report and review
of the literature. Skeletal Radiol. 45:1307–1311. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nakamura T, Matsumine A, Nishimura K,
Yokoyama H, Murata T, Uchida A and Sudo A: Extraskeletal
subcutaneous osteosarcoma of the upper arm: A case report. Oncol
Lett. 2:75–77. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bane BL, Evans HL, Ro JY, Carrasco CH,
Grignon DJ, Benjamin RS and Ayala AG: Extraskeletal osteosarcoma: A
clinicopathologic review of 26 cases. Cancer. 65:2762–2770. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mc Auley G, Jagannathan J, O'Regan K,
Krajewski KM, Hornick JL, Butrynski J and Ramaiya N: Extraskeletal
osteosarcoma: Spectrum of imaging findings. AJR Am J Roentgenol.
198:W31–W37. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee JY, Fefsch JF, Wasdhal DA, Lee BP,
Pritchard DJ and Nascimento AG: A review of 40 patients With
extraskeletal osteosarcom. Cancer. 76:2253–2259. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Longhi A, Bielack SS, Grimer R, Whelan J,
Windhager R, Leithner A, Gronchi A, Biau D, Jutte P, Krieg AH, et
al: Extraskeletal osteosarcoma: A European musculoskeletal oncology
society study on 266 patients. Eur J Cancer. 74:9–16. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sio TT, Vu CC, Sohawon S, Van Houtte P,
Thariat J, Novotny PJ, Miller RC and Bar-Sela G: Extraskeletal
osteosarcoma: An international rare cancer network study. Am J Clin
Oncol. 39:32–36. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chung EB and Enzinger FM: Extraskeletal
osteosarcoma. Cancer. 60:1132–1142. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Catania VE, Vecchio M, Malaguarnera M,
Madeddu R, Malaguarnera G and Latteri S: Tumor lysis syndrome in an
extraskeletal osteosarcoma: A case report and review of the
literature. J Med Case Rep. 11:792017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Fanburg-Smith JC, Bratthauer GL and
Miettinen M: Osteocalcin and osteonectin immunoreactivity in
extraskeletal osteosarcoma: A study of 28 cases. Hum Pathol.
30:32–38. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Secil M, Mungan U, Yorukoglu K and Dicle
O: Case 89: Retroperitoneal extraskeletal osteosarcoma. Radiology.
237:880–883. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hu B, Liu Y, Cheng L, Li W and Cao X:
SPECT/CT imaging of retroperitoneal extraskeletal osteosarcoma.
Clin Nucl Med. 39:200–202. 2014.PubMed/NCBI
|
|
17
|
Strippoli S, Traversa M, Cramarossa A,
Popescu O, Lorusso V and Guida M: Long-term response of gemcitabine
plus docetaxel chemotherapy regimen for extraskeletal osteosarcoma:
A case report. Oncol Lett. 9:2567–2571. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bhatt NR, Kakked GA, Merchant R and Bhatt
R: Extraskeletal osteosarcoma of the larynx: An extremely unusual
tumour. BMJ Case Rep. 2014:pii: bcr2014206759. 2014. View Article : Google Scholar
|
|
19
|
Casey DL, van de Rijn M, Riley G, Tung KW,
Mohler DG and Donaldson SS: Extraskeletal osteosarcoma of the hand:
The role of marginal excision and adjuvant radiation therapy. Hand
(NY). 10:602–606. 2015. View Article : Google Scholar
|
|
20
|
Abramovici LC, Hytiroglou P, Klein RM,
Karkavelas G, Drevelegas A, Panousi E and Steiner GC:
Well-differentiated extraskeletal osteosarcoma: report of 2 cases,
1 with dedifferentiation. Hum Pathol. 36:439–443. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jour G, Wang L, Middha S, Zehir A, Chen W,
Sadowska J, Healey J, Agaram NP, Choi L, Nafa K and Hameed M: The
molecular landscape of extraskeletal osteosarcoma: A
clinicopathological and molecular biomarker study. J Pathol Clin
Res. 2:9–20. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yamashita K, Kohashi K, Yamada Y, Nishida
Y, Urakawa H, Oda Y and Toyokuni S: Primary extraskeletal
osteosarcoma: A clinicopathological study of 18 cases focusing on
MDM2 amplification status. Hum Pathol. 63:63–69. 2017. View Article : Google Scholar : PubMed/NCBI
|