Introduction
Osteolytic lesions of long bones are typical
occurring pathological fracture. The most common bone disease
pathological fracturse are metastatic tumors. About 10% of patients
with primary malignant tumor will develop metastasis of the
proximal femur. Common bone metastases are derived from breast,
kidney, thyroid, prostate cancer, or myeloma (1,2).
Several studies have documented that patients with
rheumatoid arthritis (RA) have an increased risk of developing a
lymphoproliferative disorder (LPD). Patients with RA have a high
risk of developing LPDs about two to four times compared to the
general population (3). Methotrexate
(MTX) is currently a widely used disease-modifying anti-rheumatic
drug. MTX-associated LPD (MTX-LPD) is a lymphoid proliferation or
lymphoma that occurs in patients immunosuppressed with MTX and
classified as a part of the ‘other iatrogenic
immunodeficiency-associated LPDs’ category by the World Health
Organization (WHO) in 2001 (4).
MTX-LPD have characteristics of elderly patients, more females,
more Diffuse large B cell lymphoma (DLBCL), more EBV positivity,
and poor prognosis (5).
Case report
A 46-year-old woman was admitted to our hospital
complaining of right thigh pain and fatigue. She had a medical
history of RA for 5 years and 2 months. She had been receiving MTX
(8-10 mg/week) for 4 years and 11 months and etanercept (25
mg/week) for 3 years and 5 months. Her RA activity had been well
controlled with these drugs. The laboratory data showed the
following elevated values: Leukocyte, 8,200/µl (normal range:
4,300-8,000/µl); C-reactive protein (CRP), 10.07 mg/dl (normal
range: 0-0.40 mg/dl); calcium, 11.5 mg/dl (normal range: 7.0-10.0
mg/dl); inorganic phosphorus, 6.0 mg/dl (normal range: 2.9-4.3
mg/dl); alkaline phosphatase, 442 U/l (normal range: 115-359 U/l);
lactate dehydrogenase (LD), 466 U/l (normal range: 119-229 U/l);
and soluble interleukin-2 receptor (sIL-2R), 2,900 U/ml (normal
range: 124-466 U/ml). On examination for infection, serological
tests revealed that the Epstein-Barr virus (EBV) viral capsid
antigen immunoglobulin G titer was high, which indicated a current
infection.
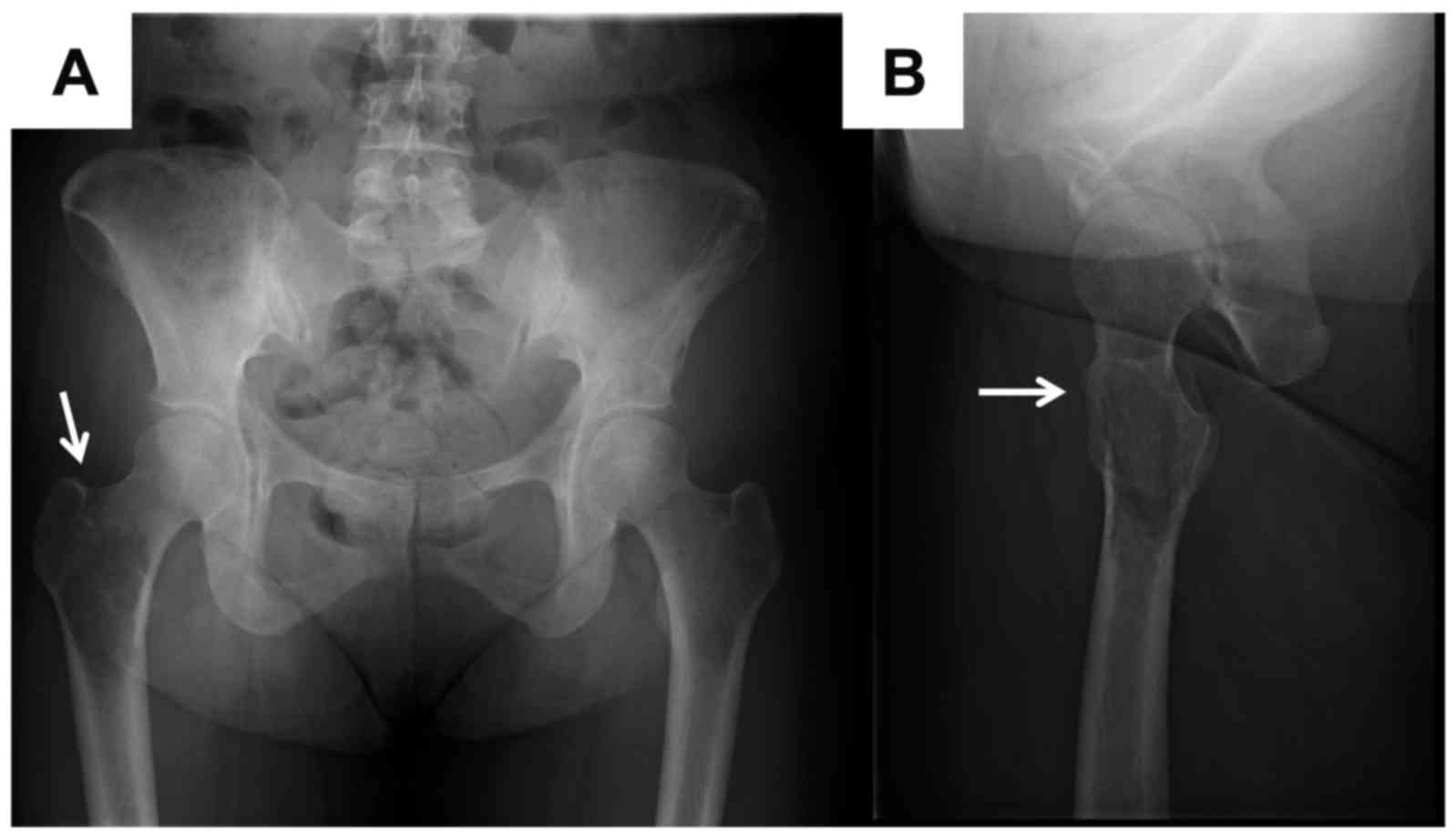
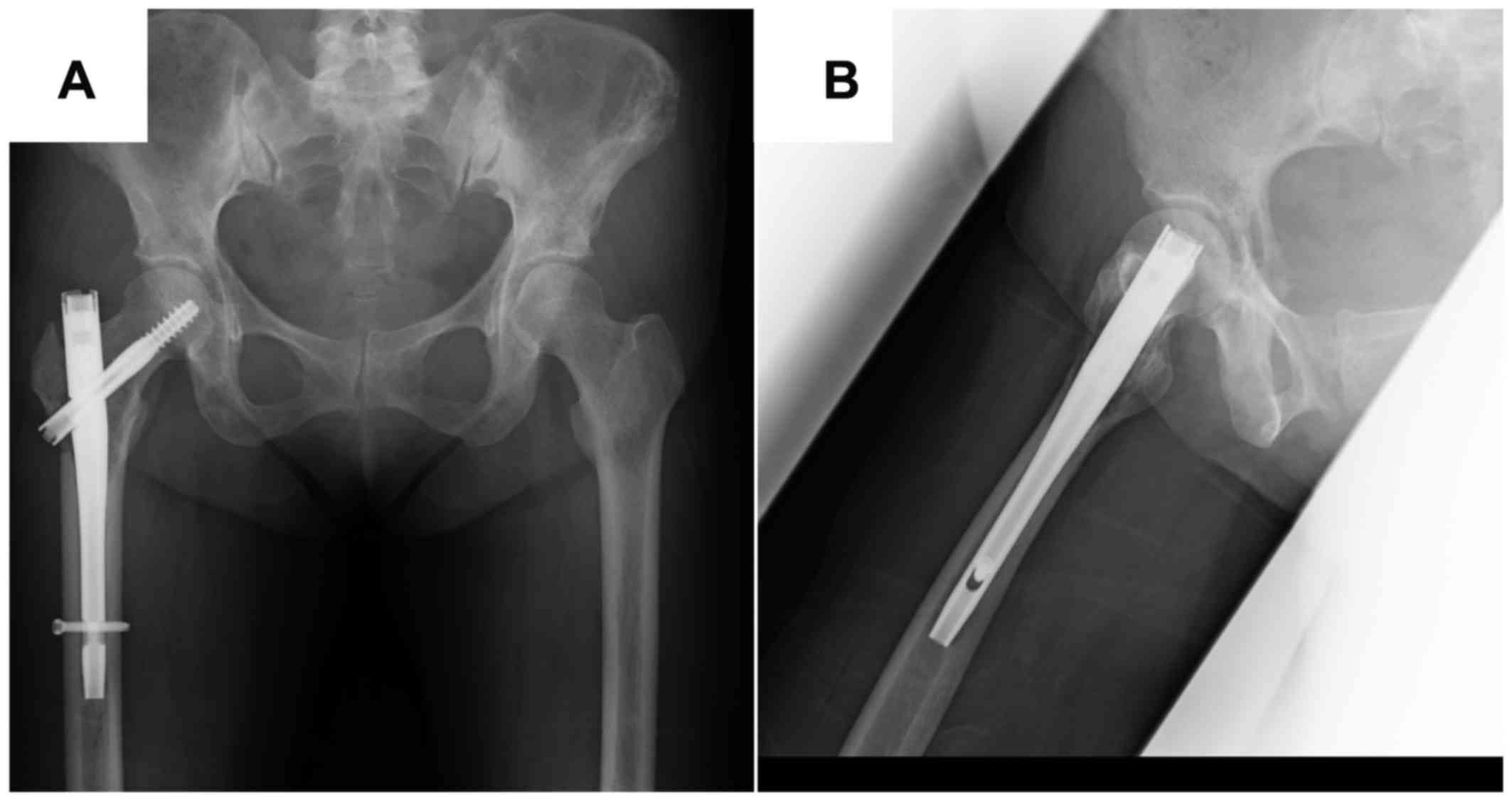
Hip X-ray image showed an ill-defined osteolytic
lesion and pathological fracture of the right femoral trochanter
(Fig. 1A and B, white arrows).
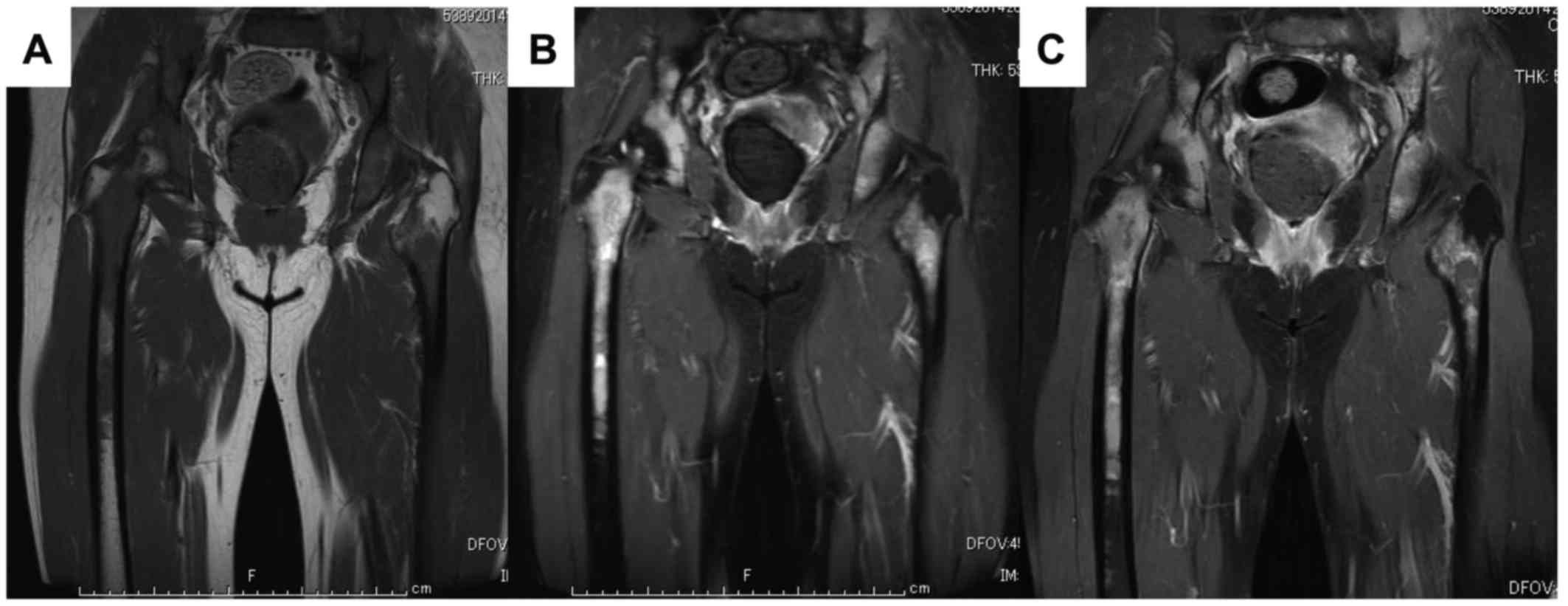
Magnetic resonance imaging (MRI) showed that the masses in the
bilateral femur and iliac had a low intensity on the T1-weighted
image (T1WI) and high intensity on the T2-weighted image and were
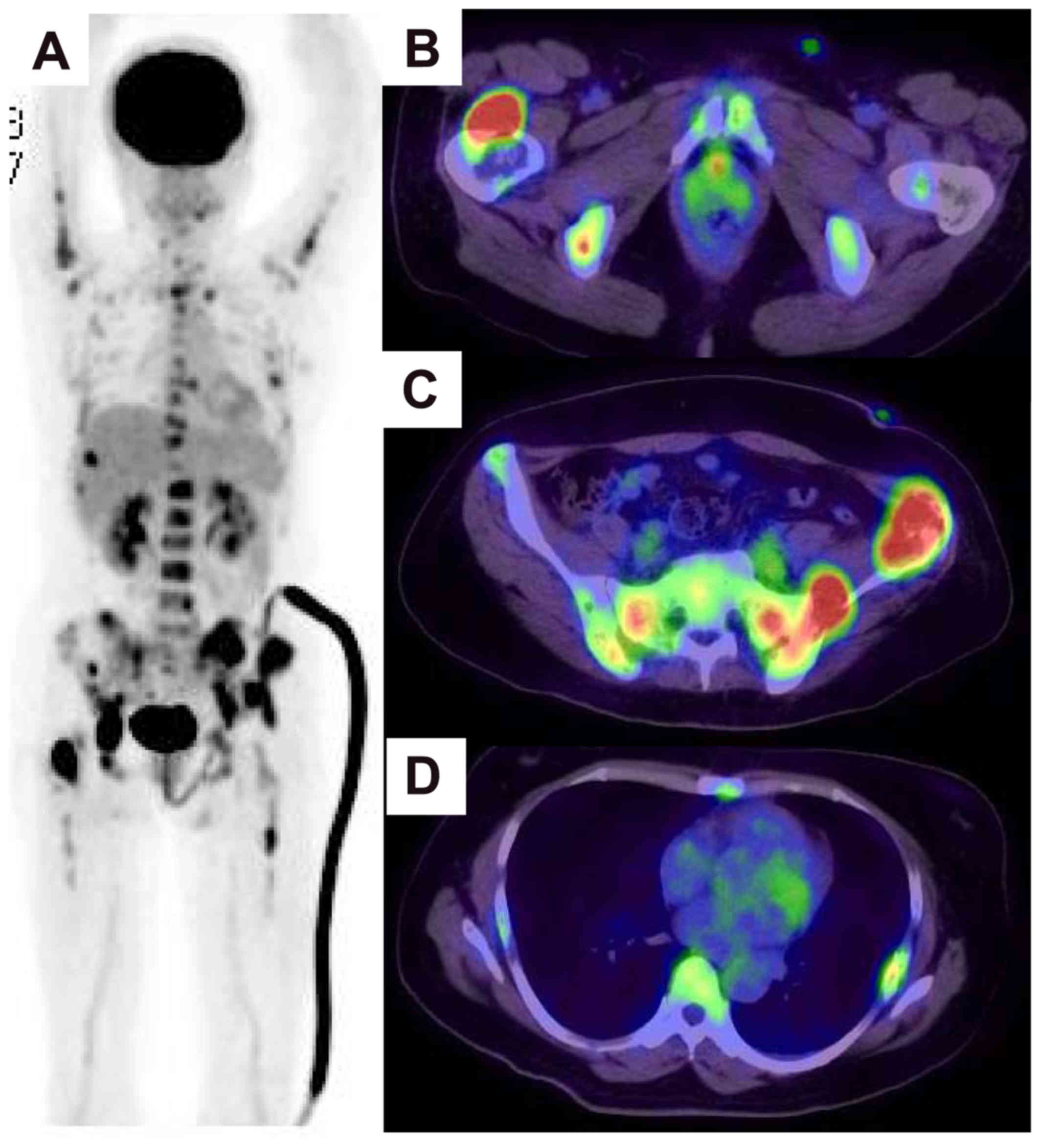
enhanced on gadolinium enhanced-T1WI (Fig. 2A-C). Whole-body computed tomography
demonstrated axillary, mediastinal, and external iliac
lymphadenopathies. Further, 18F-fluoro-deoxy-glucose
positron emission tomography (18F-FDG-PET) showed some
abnormal uptakes in the ribs, pelvis, femur, and lymph nodes
(Fig. 3A-D).
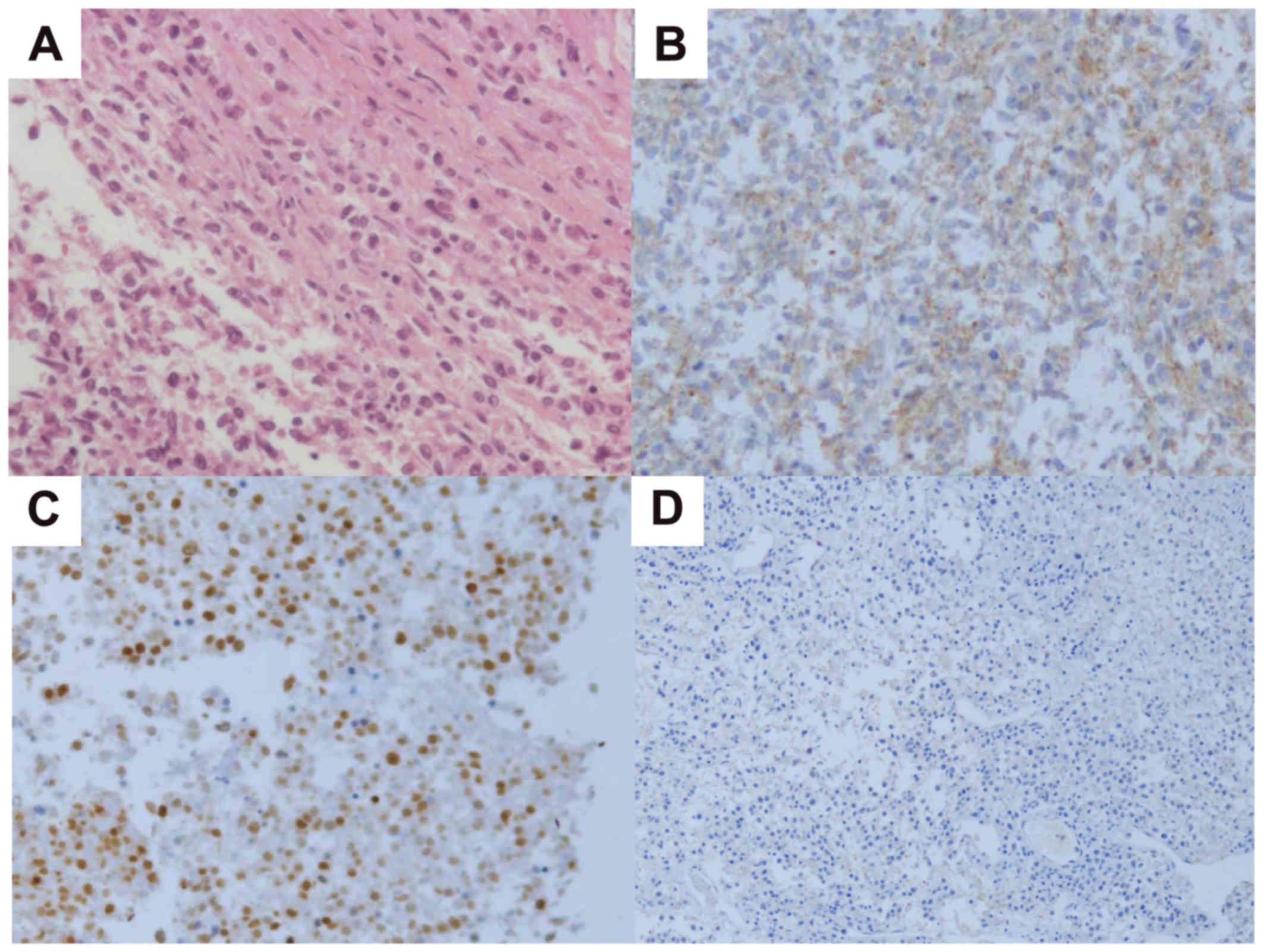
We performed open biopsy and palliative surgery
using an intramedullary nail, because we considered that
complete resection was impossible. The specimen showed diffuse
infiltration of monotonous lymphoid cells (Fig. 4A). Immunohistochemical studies
demonstrated that the infiltrating mononuclear cells were
predominantly positive for CD79a, CD20 and MUM-1. CD10 and B-cell
lymphoma 6 were not detected (Fig.
4B-D). The histological diagnosis was diffuse large B-cell
lymphoma (DLBCL) of non-germinal center B type (non-GCB type).
We referred the patient to a hematologist. Following
withdrawal of MTX, her LD and sIL-2R levels decreased gradually at
4 weeks. Furthermore, osteoblastic change in the iliac bone was
observed on an X-ray image. Based on the overall clinical data, the
multiple bone tumors were diagnosed as MTX-LPD.
However, her LD and sIL-2R levels increased rapidly
after 2 months. Further, 18F-FDG-PET revealed
progressive disease. She received a total of five cycles of R-CHOP
(rituximab, 375 mg/m2; cyclophosphamide, 750
mg/m2; doxorubicin, 50 mg/m2; vincristine,
1.4 mg/m2; and oral prednisolone, 225 mg) on days 1-5 on
a 21-day schedule. After chemotherapy, she experienced nausea and
headache. Thus, she underwent MRI of the head, and intracranial
dissemination of the DLBCL was observed. Then, she also underwent
cranial irradiation, one cycle of mini MEAM (ranimustine, 50
mg/day; etoposide, 100 mg/day; cytarabine, 200 mg/day; and
melphalan, 20 mg/day) on days 1-3, and two cycles of IT triple
(MTX, 15 mg; cytarabine, 40 mg; and prednisolone, 10 mg). After the
three cycles of chemotherapy, she received haplo-peripheral blood
stem cell transplantation (haplo-PBSCT). After haplo-PBSCT, her
intracranial lesion disappeared, and her symptoms improved.
At the final follow-up, tumor condition was
no evidence of disease. She had no pain of her lower legs, and
walking alone. X-ray showed sclerotic change of bilateral proximal
femurs were observed (Fig.
5).
Discussion
The prevalence of RA is slightly different among
countries worldwide; however, the prevalence is ~0.5%, and the
estimated number of affected patients is 800,000 in Japan (6). RA is a systemic inflammatory disease
characterized by the destruction of the articular structures and
synovitis in multiple joints. MTX is an anti-rheumatic drug that is
expected to have an excellent suppressive effect on articular
destruction (7). For this reason,
MTX is currently a widely used key drug for the treatment of
patients with RA. However, patients with RA have a high risk of
developing LPDs (3). Furthermore,
LPD in patients with RA treated with MTX is defined as MTX-LPD in
the 2001 WHO classification of tumors of hematopoietic and lymphoid
tissues (4). Although the detailed
mechanism of the occurrence of MTX-LPD is unknown, it is considered
that MTX is involved as an etiology because there are cases where
LPD had a complete regression after withdrawal of MTX alone
(8). Furthermore, patients with RA
treated with high-dose MTX (over 8 mg/week) are at a high risk of
developing LPDs (9).
The clinical findings of MTX-LPD include fever,
weight loss, and swelling of superficial lymph nodes. In the blood
sampling data, high levels of CRP, LD, and sIL-2R are observed. In
MTX-LPD, lymphomas occur in half of the lymph nodes and half of the
extranodal lesions, such as the skin, gastrointestinal tract,
salivary gland, thyroid, and nasal cavity (4,10). As in
this case, multiple bone lesions accompanying a pathological
fracture were not detected. The percentage of the pathological
diagnosis of lymphomas in patients with RA is 35 to 60% for DLBCL
and 12 to 25% for Hodgkin's lymphoma (5). In our case, the pathological diagnosis
was DLBCL.
EBV is a known oncogenic virus involved in
lymphomagenesis. An immunodeficiency status is considered to
provide the basis for the onset of malignant lymphomas through the
activation of EBV. The EBV-positive rate in MTX-LPD is 27.6 to 95%,
which is significantly higher than that in sporadic LPD (9.9%)
(3,11,12).
Kamel et al (13) reported
that MTX-LPD was associated with EBV because some cases of
EBV-positive MTX-LPD spontaneously regressed after the withdrawal
of MTX. Further, Feng et al (14) showed that MTX directly releases
infectious virions and induces reactivation of EBV infection. No
case of non-MTX-LPD showed spontaneous regression. In our case, the
EBV result was positive; thus, she stopped using MTX. However, her
condition did not improve, and the LD and sIL-2R levels in her
blood sampling data increased rapidly after 2 months. Miyazaki
et al (8) reported that the
complete remission rate of MTX-LPD was ~30% with MTX withdrawal;
however, the complete remission rate was as high as 60% in their
EBV-positive cases. Therefore, many cases resulted in complete
remission within 2 weeks. In this case, temporary improvement was
obtained after MTX withdrawal; however, complete remission was not
achieved within 2 weeks. Therefore, the patient was determined to
have progressive disease after 2 months. For cases wherein complete
remission cannot be obtained within 2 weeks, we should consult with
hematologists and need to introduce chemotherapy.
Since DLBCL of a non-GCB type diagnosed on
immunohistochemistry usually has a poor prognosis (15), we need to consider introducing
chemotherapy. In summary, we experienced an MTX-LPD case with a
pathological fracture. We need to consider MTX-LPD when
pathological fractures occur in patients with RA treated with
MTX.
Acknowledgements
The authors would like to thank Dr Yuko Kuwae of the
Department of Diagnostic Pathology, Osaka City University Graduate
School of Medicine (Osaka, Japan) for their assistance with
pathological examinations and interpretations.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Author's contributions
NO designed the study and wrote the initial draft of
the manuscript. MH contributed to analysis and interpretation of
data and assisted in the preparation of the manuscript. MI, TI, ST,
MO and HN contributed to data collection and interpretation, and
critically reviewed the manuscript. All authors approved the final
version of the manuscript.
Ethics approval and consent to
participate
The patient provided consent.
Patient consent for publication
The patient and her family were informed that the
data from her case would be submitted for publication and provided
consent.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
RA
|
rheumatoid arthritis
|
|
LPD
|
lymphoproliferative disorder
|
|
MTX
|
methotrexate
|
|
MTX-LPD
|
methotrexate-associated
lymphoproliferative disorder
|
|
WHO
|
World Health Organization
|
|
CRP
|
C-reactive protein
|
|
LD
|
lactate dehydrogenase
|
|
sIL-2R
|
soluble interleukin-2 receptor
|
|
EBV
|
Epstein-Barr virus
|
|
MRI
|
magnetic resonance imaging
|
|
T1W1
|
T1-weighted image
|
|
18F-FDG-PET
|
18F-fluoro-deoxy-glucose
positron emission tomography
|
|
DLBCL
|
diffuse large B-cell lymphoma
|
|
non-GCB
|
non-germinal center B
|
|
haplo-PBSCT
|
haplo-peripheral blood stem cell
transplantation
|
References
|
1
|
Hage WD, Aboulafia AJ and Aboulafia DM:
Incidence, location, and diagnostic evaluation of metastatic bone
disease. Orthop Clin North Am. 31:515–528. vii2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ricci AI, Wodajo FM and Malawer M:
Metastatic carcinoma of the long bones. Am Fam Physician.
76:1489–1494. 2007.PubMed/NCBI
|
|
3
|
Ekström K, Hjalgrim H, Brandt L, Baecklund
E, Klareskog L, Ekbom A and Askling J: Risk of malignant lymphomas
in patients with rheumatoid arthritis and in their first-degree
relatives. Arthritis Rheum. 48:963–970. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harris NL and Swerdlow SH:
Methotrexate-associated lymphoproliferative disorders. Jaffe ES,
Harris NL, Stein H and Vardiman JW: Pathology and genetics, tumours
of haematopoietic and lymphoid tissues, World Health Organization
classification of tumours Lyon: IARC Press; pp. pp270–271. 2001
|
|
5
|
Hoshida Y, Xu JX, Fujita S, Nakamichi I,
Ikeda J, Tomita Y, Nakatsuka S, Tamaru J, Iizuka A, Takeuchi T and
Aozasa K: Lymphoproliferative disorders in rheumatoid arthritis:
Clinicopathological analysis of 76 cases in relation to
methotrexate medication. J Rheumatol. 34:322–331. 2007.PubMed/NCBI
|
|
6
|
Ministry of Health Labour Welfare
Rheumatoid arthritis and allergy information. 6:123–154. 2010.
|
|
7
|
Heldmann F and Braun J: Perioperative use
of methotrexate. Clin Exp Rheumatol. 28 5 Suppl 61:S110–S113.
2010.PubMed/NCBI
|
|
8
|
Miyazaki T, Fujimaki K, Shirasugi Y,
Yoshiba F, Ohsaka M, Miyazaki K, Yamazaki E, Sakai R, Tamaru J,
Kishi K, et al: Remission of lymphoma after withdrawal of
methotrexate in rheumatoid arthritis: Relationship with type of
latent Epstein-Barr virus infection. Am J Hematol. 82:1106–1109.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kameda T, Dobashi H, Miyatake N, Inoo M,
Onishi I, Kurata N, Mitsunaka H, Kawakami K, Fukumoto T, Susaki K,
et al: Association of higher methotrexate dose with
lymphoproliferative disease onset in rheumatoid arthritis patients.
Arthritis Care Res (Hoboken). 66:1302–1309. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mariette X, Cazals-Hatem D, Warszawki J,
Liote F, Balandraud N and Sibilia J: Investigators of the Club
Rhumatismes et Inflammation; Lymphomas in rheumatoid arthritis
patients treated with methotrexate: A 3-year prospective study in
France. Blood. 99:3909–3915. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hoshida Y and Aozasa K: Malignancies in
organ transplant recipients. Pathol Int. 54:649–658. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nalesnik MA, Jaffe R, Starzl TE, Demetris
AJ, Porter K, Burnham JA, Makowka L, Ho M and Locker J: The
pathology of posttransplant lymphoproliferative disorders occurring
in the setting of cyclosporine A-prednisone immunosuppression. Am J
Pathol. 133:173–192. 1988.PubMed/NCBI
|
|
13
|
Kamel OW, Van de Rijin M, Weiss LM, Del
Zoppo GJ, Hench PK, Robbins BA, Montgomery PG, Warnke RA and
Dorfman RF: Brief report: Reversible lymphomas associated with
Epstein-Barr virus occurring during methotrexate therapy for
rheumatoid arthritis and dermatomyositis. N Engl J Med.
328:1317–1321. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Feng WH, Cohen JI, Fischer S, Li L,
Sneller M, Goldbach-Mansky R, Raab-Traub N, Delecluse HJ and Kenney
SC: Reactivation of latent Epstein-Barr virus by methotrexate: A
potential contributor to methotrexate-associated lymphomas. J Natl
Cancer Inst. 96:1691–1702. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hans CP, Weisenburger OD, Greiner TC,
Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E,
Braziel RM, Jaffe ES, et al: Confirmation of the molecular
classification of diffuse large B-cell lymphoma by
immunohistochemistry using a tissue microarray. Blood. 103:275–282.
2004. View Article : Google Scholar : PubMed/NCBI
|