Introduction
High-grade non-Hodgkin lymphoma (NHL) is considered
to represent one of three acquired immune deficiency syndrome
(AIDS)-defining malignancies (1),
among which diffuse large B-cell lymphoma (DLBCL) is the most
common, accounting for 31% of all NHL cases (2,3).
However, primary non-Hodgkin lymphoma of the lung is uncommon and
accounts for only 0.4% of all malignant lymphomas (4). The majority of primary pulmonary
lymphomas (PPL) are of low grade, of the mucosa-associated lymphoid
tissue type, and primary pulmonary DLBCL is extremely rare
(5). Primary central nervous system
lymphoma (PCNSL) is a rare tumor of the brain that accounts for 4%
of newly diagnosed patients with CNS malignancies (6,7);
however, the majority of patients with PCNSL have the highly
aggressive diffuse large B-cell subtype. In the present study, the
case of a patient suffering from DLBCL with concurrent pulmonary
and cerebral involvement is reported. This is rare in clinical
practice and, considering that its clinical symptoms are
non-specific, prompt diagnosis often proves difficult (8).
Case report
A 42-year-old man presented with a 2-week history of
dry cough and thoracalgia accompanied by intermittent mild fever
and headaches; however, no night sweats or weight loss were
reported. The patient had a history of sexual contact with men. A
total of 18 months prior to the presentation, the patient was
diagnosed with pulmonary tuberculosis (TB) in a specialized
hospital in China following the development of fever and cough. The
results of acid-fast staining on sputum smear analysis and a chest
X-ray showing infiltrates in both lungs were consistent with
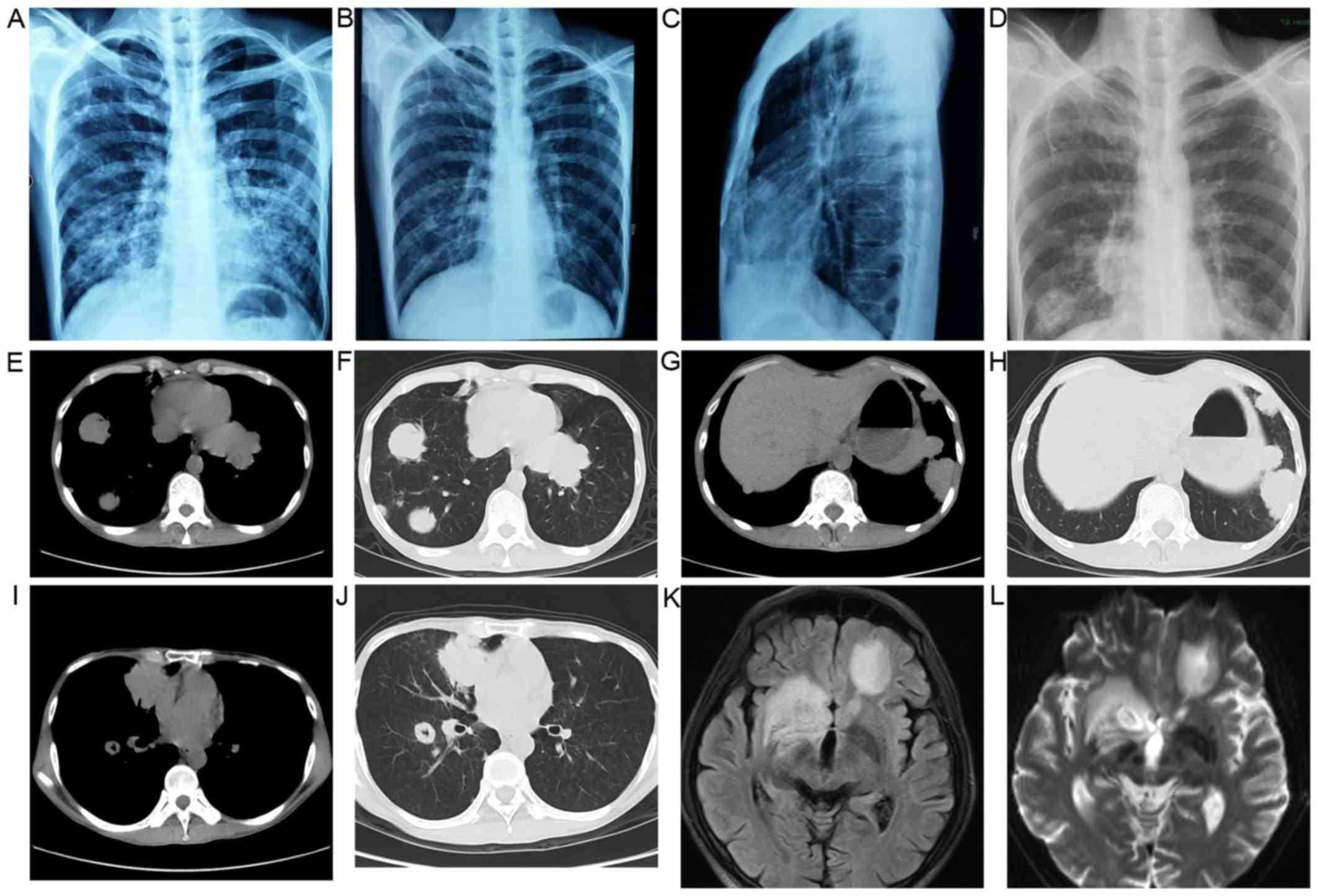
typical TB manifestations (Fig. 1A).
Simultaneously, the patient was diagnosed with human
immunodeficiency virus (HIV) infection. According to the guideline
for adult HIV/AIDS patients with opportunistic infections
recommended by the Center for Disease Control and Prevention,
Infectious Diseases Society of America and National Institutes of
Health (http://aidsinfo.nih.gov/guidelines), the specialist
consultant at the TB specialized hospital empirically prescribed
first-line anti-TB treatment for this patient with 2 months of
isoniazid, rifampicin, ethambutol and pyrazinamide, followed by 4
months of isoniazid and rifampicin. As a result, the fever and
cough were eliminated, and the pulmonary infiltrate was also
absorbed (Fig. 1B and C). Thus,
according to the guideline, further testing for anti-TB drug
sensitivity was not deemed necessary. One month after the
aforementioned treatments, lamivudine, tenofovir and efavirenz were
administered to the patient as an additional anti-HIV treatment
strategy; however, the medication was not taken regularly and
follow-up appointments were also irregular. A physical examination
was performed following admittance to the hospital, which revealed
bilateral oral leukoplakia and tenderness in the left lower chest.
Sputum acid-fast staining analysis did not reveal any signs of TB
infection, and no anaerobic bacteria, aerobic bacteria, fungi or
Mycobacterium tuberculosis were present in blood culture.
The results of the laboratory tests performed on admission are
presented in Table I. Lumbar
puncture was performed due to the patient suffering from headaches;
however, no pathogens were found in the cerebrospinal fluid (CSF).
The results of CSF examinations are presented in Table I. A chest X-ray revealed multiple
masses in both lungs (Fig. 1D) and a
subsequent thoracic computerized tomography (CT) scan confirmed
this result (Fig. 1E-J). Brain
magnetic resonance imaging (MRI) revealed nodules in the left
frontal cortex and the bilateral basal ganglia. (Fig. 1K and L). The patient was initially
suspected to be suffering from a pulmonary and CNS infection;
however, the X-ray and laboratory findings did not support this
suspected diagnosis. To determine the composition of the lung and
brain masses, a percutaneous lung needle biopsy was performed,
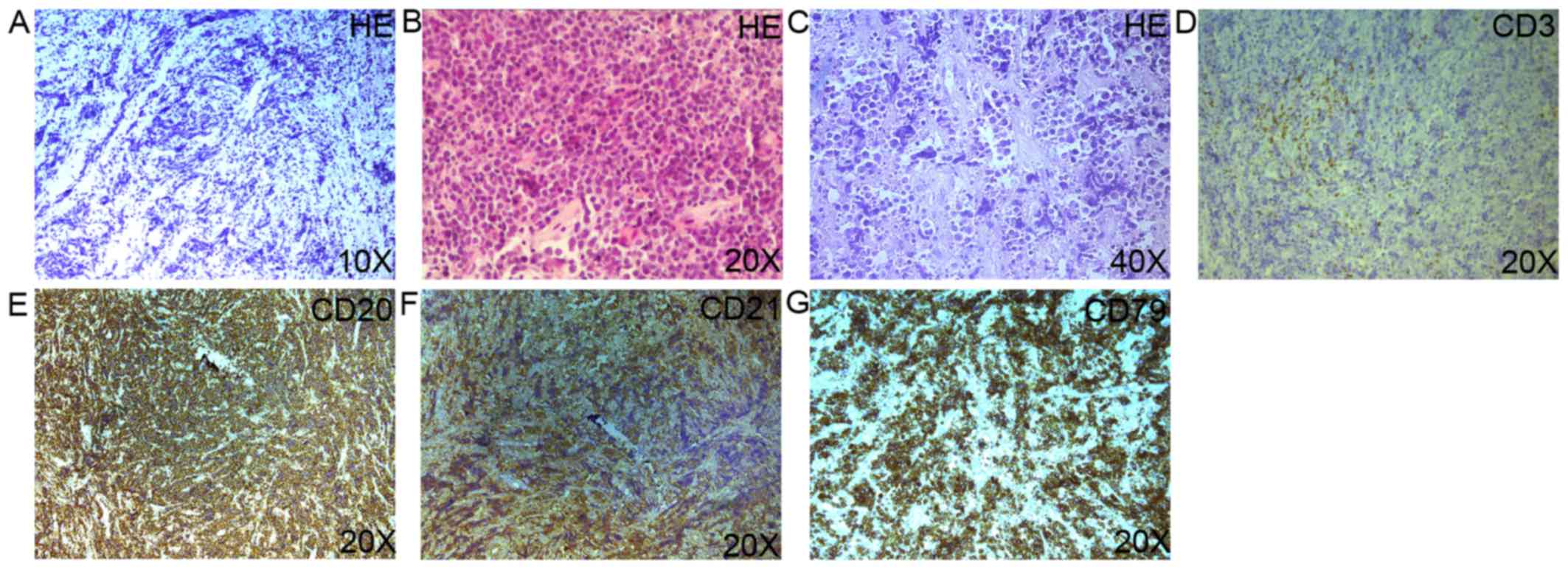
revealing large numbers of lymphocytes ranging in size from medium
to large, with oval or round nuclei containing fine chromatin and
scanty cytoplasm (Fig. 2A-C).
Furthermore, immunohistochemistry staining analysis revealed that
these results were consistent with a diagnosis of germinal center
B-cell-like (GCB) DLBCL (Fig. 2D-G).
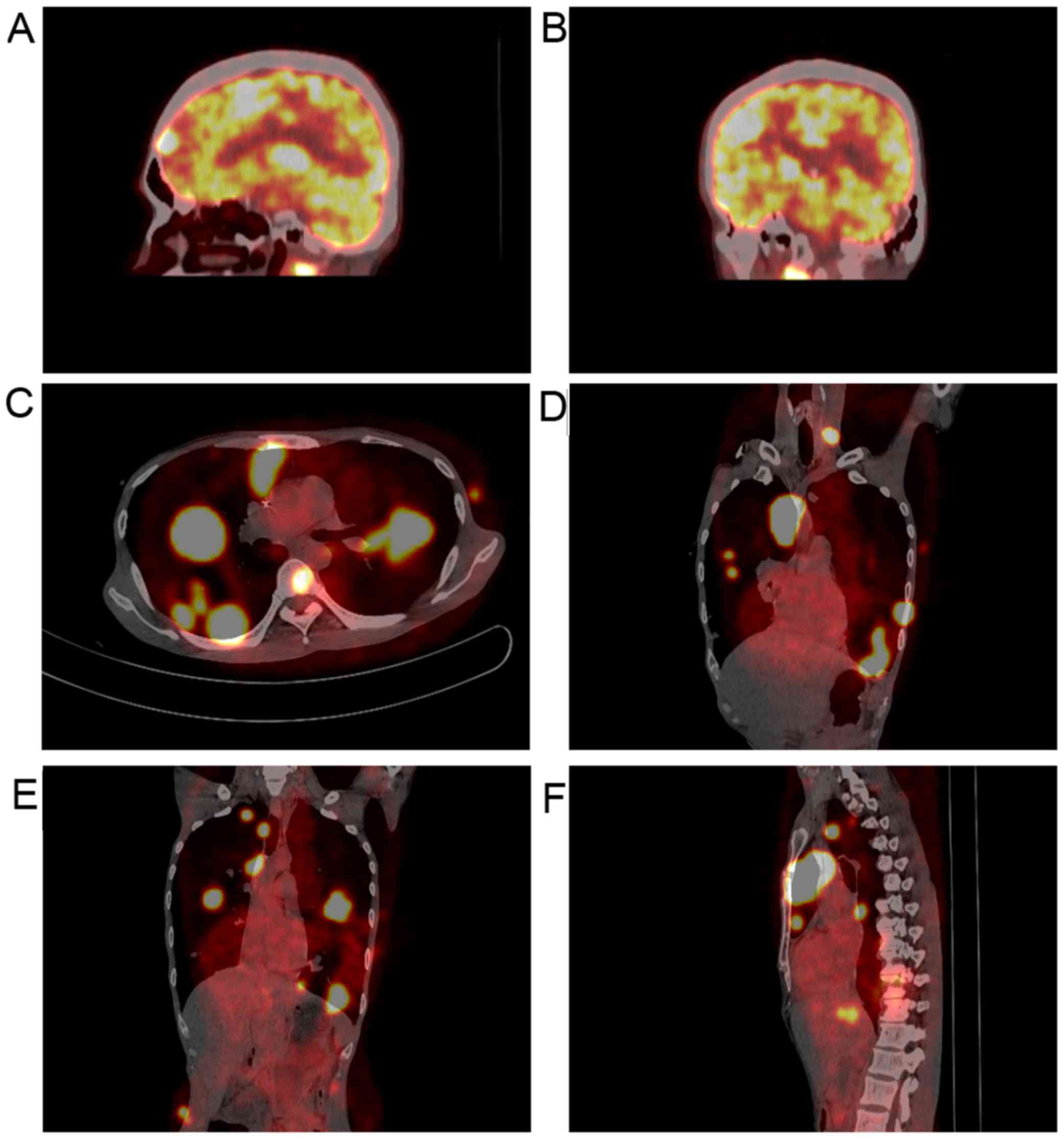
18F-labelled fluorodeoxyglucose (FDG) positron emission
tomography (PET) revealed that FDG uptake was high in the brain,
mediastinum, lungs, right adrenal gland, thoracic vertebrae and
ribs (Fig. 3). Based on these
results, experienced radiologists suggested a diagnosis of systemic
lymphoma with CNS involvement. Then, bone marrow aspiration was
performed, and cytological examination revealed normal bone marrow
hyperplasia, without the presence of lymphosarcoma cells.
Therefore, the patient was diagnosed with stage IV NHL according to
the Ann Arbor staging system for lymphoma (9), B group as he displayed one of the
systemic B symptoms, including fevers (>38.5°C), drenching night
sweats and/or weight loss (>10% of body weight over 6 months
prior to diagnosis). The patient had a poor prognosis due to his
high-intermediate risk (score 3) according to international
prognostic index: Stage IV, high serum lactate dehydrogenase level,
>1 extranodal sites (10) and CD4
cell count <100 cells/µl (11).
Unfortunately, the patient refused chemotherapy or radiotherapy for
the treatment of lymphoma due to his poor economic status and poor
prognosis, and discharged himself from the hospital.
 | Table I.Laboratory test results on
admission. |
Table I.
Laboratory test results on
admission.
| Test item | Test value | Normal range |
|---|
| White blood cell
count (109/l) | 2.94 | 3.5-9.5 |
| Neutrophils (%) | 73.5 | 40-75 |
| Lymphocytes (%) | 15.0 | 20-50 |
| Hemoglobin (g/l) | 95.0 | 130-175 |
| Platelets
(109/l) | 202 | 125-350 |
| Blood urea nitrogen
(mmol/l) | 4.19 | 2.29-7.0 |
| Creatinine
(µmol/l) | 47.6 | 53-106 |
| Alanine transaminase
(U/l) | 34.9 | 9-50 |
| Glutamic-oxaloacetic
transaminase (U/l) | 39.8 | 15-40 |
| Total bilirubin
(µmol/l) | 4.0 | 5-20 |
| Direct bilirubin
(µmol/l) | 2.6 | 1.7-10 |
| Albumin (g/l) | 28.6 | 40-55 |
| β٢-microglobulin
(mg/l) | 6.08 | 1.09-2.53 |
| Lactate dehydrogenase
(U/l) | 526 | 135-225 |
| CD4 cell count
(cells/µl) | 42 | 600-800 |
| Erythrocyte
sedimentation rate (mm/h) | 50 | <15 |
| High-sensitivity
C-reactive protein (mg/l) | 35 | 0-3 |
| Procalcitonin
(ng/ml) | 1.76 | <1.0 |
| Plasma (1,3)
β-D-glucan (pg/ml) | 10 | <60 |
| Serum galactomannan
antigen | Negative | Negative |
| Cryptococcal
antigen | Negative | Negative |
| Anti-EBV-EA IgM
antibody | Negative | Negative |
| Anti-EBV-VCA IgM
antibody | Negative | Negative |
| Anti-CMV IgM
antibody | Negative | Negative |
| Anti-mycoplasma IgM
antibody | Negative | Negative |
| Anti-chlamydia IgM
antibody | Negative | Negative |
| EBV DNA
(copies/ml) | <500 | <500 |
| CMV DNA
(copies/ml) | <500 | <500 |
| HIV RNA loads
(copies/ml) | 10×106 | <500 |
| CSF pressure
(mmH2O) | 85 | 80-180 |
| CSF total cell count
(106/l) | 0 | 0-8 |
| CSF protein
(g/l) | 0.22 | 0.15-0.45 |
| CSF glucose
(mmol/l) | 2.59 | 2.8-4.5 |
| CSF chloride
(mmol/l) | 120.9 | 120-132 |
| CSF TOX-IgM | Negative | Negative |
| CSF TOX-IgG | Negative | Negative |
Discussion
The majority of risk factors for the development of
lymphoma are associated with altered immune function (12), including infection with HIV, the
administration of immunosuppressants for the prevention of organ
transplant rejection and severe autoimmune conditions (13). DLBCL is the most common type of NHL
in HIV-infected as well as non-HIV infected patients (3). The majority of patients with PPL suffer
from marginal zone lymphomas of the mucosa-associated lymphoid
tissue type (14,15). DLBCL directly arising from lung
tissue is extremely rare, and accounts for 0.4% of all lymphomas
(16). Primary pulmonary DLBCL is
frequently misdiagnosed as pneumonia, TB or lung cancer due to its
non-specific clinical symptoms, and definitive diagnosis most often
requires invasive lung biopsy (5,17). There
has been a report of a patient suffering from pulmonary
lymphomatoid granulomatosis who was misdiagnosed as suffering from
pulmonary aspergillosis and TB (18).
PCNSL is a rare type of extranodal NHL (19), and congenital or acquired
immunodeficiency is the only risk factor for this tumor that has
been established to date. Patients with PCNSL have lymphosarcoma
cells present in the CNS, which may induce lymphoma relapse
(20). Unlike peripheral tumors,
cerebral lymphoma is difficult to diagnose by histopathology.
Therefore, MRI and PET-CT examinations can assist in the diagnosis
of most CNS lymphomas. The typical findings of PCNSL on MRI are
considered to be single lesions (60-70% of the cases) or multiple
lesions (30-40% of the cases) without necrosis and with a
relatively small oedema, which are usually localized in the
periventricular space (21). FDG-PET
has been shown to provide high accuracy in the differentiation
between cerebral lymphomas and infectious lesions in patients with
AIDS. Malignant processes tend to exhibit higher uptake compared
with infections (22). In the
present case, the brain MRI revealed nodules in the left frontal
cortex and bilateral basal ganglia, and the FDG-PET revealed high
signal in the brain, which were considered to be consistent with
the MRI and PET characteristics of CNS lymphoma by experienced
radiologists based on the NCCN Clinical Practice Guideline in
Oncology (www.NCCN.org). Furthermore, other CNS
malignancies were excluded, as the simultaneous presence of a
systemic lymphoma and another carcinoma in the same patient is
extremely rare. The most common pathogenic infections in the brain
parenchyma of HIV/AIDS patients are toxoplasma, TB and
cryptococcosis. The clinical presentation and laboratory tests for
the presence of pathogenic microorganisms in the blood and CSF did
not confirm the diagnosis of cerebral parenchymal pathogen
infection in the present case. Furthermore, the radiographic
appearance of the CNS lesions did not support this diagnosis.
Therefore, infectious lesions of the brain were not considered in
this case.
In conclusion, patients suffering from both
pulmonary and nervous system lymphoma are extremely rare. This case
study was reported with the aim to increase awareness among
physicians regarding the presence of DLBCL with concurrent
pulmonary and CNS involvement.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81571178).
Availability of data and materials
Not applicable.
Authors' contributions
JZ and XZ selected clinical information; WH, CG and
HW, provided clinical diagnostic support; RJ and YZ prepared the
manuscript. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
This case report was approved by the Human Subjects
Protection Committees of Beijing You An Hospital, Capital Medical
University.
Patient consent for publication
Written informed consent was obtained from the
patient regarding the publication of the case details.
Competing interests
The authors declare that they have no competing
interests to disclose.
References
|
1
|
Bower M, Palfreeman A, Alfa-Wali M, Bunker
C, Burns F, Churchill D, Collins S, Cwynarski K, Edwards S, Fields
P, et al: British HIV association guidelines for HIV-associated
malignancies 2014. HIV Med. 15 Suppl 2:S1–S92. 2014. View Article : Google Scholar
|
|
2
|
Martelli M, Ferreri A, Agostinelli C, Di
Rocco A, Pfreundschuh M and Pileri S: Diffuse large B-cell
lymphoma. Crit Rev Oncol Hematol. 87:146–171. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Birendra KC, Afzal MZ, Wentland KA, Hashmi
H, Singh S, Ivan E and Lakhani N: Spontaneous regression of
refractory diffuse large B-cell lymphoma with improvement in immune
status with ART in a patient with HIV: A case report and literature
review. Am J Case Rep. 16:347–352. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Majid N, Kamal el B, Oncology B, Rachid A
and Hassan IH: Primary pulmonary lymphoma: About five cases and
literature review. Lung India. 31:53–55. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jiang AG, Gao XY and Lu HY: Diagnosis and
management of a patient with primary pulmonary diffuse large B-cell
lymphoma: A case report and review of the literature. Exp Ther Med.
8:797–800. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Montesinos-Rongen M, Purschke FG, Brunn A,
May C, Nordhoff E, Marcus K and Deckert M: Primary central nervous
system (CNS) lymphoma B cell receptors recognize CNS proteins. J
Immunol. 195:1312–1319. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Villano JL, Koshy M, Shaikh H, Dolecek TA
and McCarthy BJ: Age, gender, and racial differences in incidence
and survival in primary CNS lymphoma. Br J Cancer. 105:1414–1418.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ferraro P, Trastek VF, Adlakha H,
Deschamps C, Allen MS and Pairolero PC: Primary non-Hodgkin's
lymphoma of the lung. Ann Thorac Surg. 69:993–997. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lister TA, Crowther D, Sutcliffe SB,
Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA and
Tubiana M: Report of a committee convened to discuss the evaluation
and staging of patients with Hodgkin's disease: Cotswolds meeting.
J Clin Oncol. 7:1630–1636. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ribera JM, Oriol A, Morgades M,
González-Barca E, Miralles P, López-Guillermo A, Gardella S, López
A, Abella E and García M; PETHEMA, GELTAMO, GELCAB and GESIDA
Groups, : Safety and efficacy of cyclophosphamide, adriamycin,
vincristine, prednisone and rituximab in patients with human
immunodeficiency virus-associated diffuse large B-cell lymphoma:
results of a phase II trial. Br J Haematol Haematol Haematol.
140:411–419. 2008. View Article : Google Scholar
|
|
11
|
Straus DJ, Huang J, Testa MA, Levine AM
and Kaplan LD: Prognostic factors in the treatment of human
immunodeficiency virus-associated non-Hodgkin's lymphoma: Analysis
of AIDS clinical trials group protocol 142-low-dose versus
standard-dose m-BACOD plus granulocyte-macrophage
colony-stimulating factor. National institute of allergy and
infectious diseases. J Clin Oncol. 16:3601–3606. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lin Y, Gustafson MP, Bulur PA, Gastineau
DA, Witzig TE and Dietz AB: Immunosuppressive CD14+HLA-DR(low)/-
monocytes in B-cell non-Hodgkin lymphoma. Blood. 117:872–881. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Saitoh Y, Ohnishi-Amemiya A, Asano M,
Tanaka Y, Yoshizawa S, Fujimoto H, Itoh Y, Nakamura N and Ohyashiki
K: Unique radiological features of two cases of primary pulmonary
diffuse large B-cell lymphoma. Thorax. 72:859–860. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zucca E, Gregorini A and Cavalli F:
Management of non-Hodgkin lymphomas arising at extranodal sites.
Ther Umsch. 67:517–525. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xu H, Xu K, Wang R and Liu X: Primary
pulmonary diffuse large B-cell lymphoma on FDG PET/CT-MRI and DWI.
Medicine (Baltimore). 94:e12102015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cardenas-Garcia J, Talwar A, Shah R and
Fein A: Update in primary pulmonary lymphomas. Curr Opin Pulm Med.
21:333–337. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xu B, Liu H, Wang B, Zhang H, Wu H, Jin R
and Zhang Y: Fever, dry cough and exertional dyspnea: Pulmonary
lymphomatoid granulomatosis masquerading as pneumonia,
granulomatosis with polyangiitis and infectious mononucleosis.
Intern Med. 54:3045–3049. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Batchelor T and Loeffler JS: Primary CNS
lymphoma. J Clin Oncol. 24:1281–1288. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Uni M, Kagoya Y, Nannya Y, Nakamura F and
Kurokawa M: Central nervous system relapse in patients with diffuse
large B-cell lymphoma: Analysis of incidence and prognostic
factors. Leuk Lymphoma. 56:1869–1871. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Korfel A and Schlegel U: Diagnosis and
treatment of primary CNS lymphoma. Nat Rev Neurol. 9:317–327. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Maza S, Buchert R, Brenner W, Munz DL,
Thiel E, Korfel A and Kiewe P: Brain and whole-body FDG-PET in
diagnosis, treatment monitoring and long-term follow-up of primary
CNS lymphoma. Radiol Oncol. 47:103–110. 2013. View Article : Google Scholar : PubMed/NCBI
|