Introduction
Bladder carcinoma is the fourth (7%) most frequently
newly diagnosed malignancy in men in USA, with an estimated
incidence of 60,490 new cases and 12,240 deaths in 2017 (1). In recent decades, the incidence of
bladder cancer in China has been increasing rapidly according to
the 2014 Chinese Diagnosis and Treatment of Urological Diseases
Guide. Neuroendocrine carcinoma, which includes carcinoid tumors,
large-cell neuroendocrine carcinomas and small-cell carcinomas,
commonly occurs in the respiratory and gastrointestinal systems
(2,3). Primary small-cell neuroendocrine
carcinoma (SCNEC) of the bladder is rare, accounting for <1% of
all bladder carcinomas (4,5). To the best of our knowledge, only ~150
cases of primary SCNEC of the urinary bladder have been reported to
date (2,5). SCNEC of the urinary bladder is
characterized by poor differentiation and high aggressiveness, and
is frequently at an advanced stage when initially diagnosed,
resulting in high metastatic potential and poor prognosis. The mean
survival is only a few months and the mean 5-year survival rate is
~8% (2,6). We herein report a case of primary SCNEC
arising within the urinary bladder, along with a review of the
relevant literature and a discussion of the clinical presentation,
pathological characteristics, behavior, management and outcome of
this disease. The study was approved by the Ethics Committee of
Peking University Shenzhen Hospital (Shenzhen, China) and written
informed consent was obtained from the patient for publication of
the case details.
Case report
An 87-year-old male patient presented with gross
hematuria for 15 days and was admitted to the local hospital. The
patient had a smoking history of 40 pack-years, Ultrasonography
revealed a 35×31-mm mass in the urinary bladder. The patient was
diagnosed with bladder cancer and referred to the Peking University
Shenzhen Hospital (Shenzhen, China) for further treatment.
Laboratory tests were performed and the results were as follows:
White blood cell (WBC) count, 11.59×109/l (normal range,
3.5-9.5×109/l); neutrophilic granulocytes, 75.7% (normal
range, 40-75%); hemoglobin level, 128 g/l (normal range, 130-175
g/l); urine sediment analysis: Red blood cell count, 1,061.9/µl
(normal range, 0-13.1/µl), WBC 1,151.2/µl (normal range, 0-9.2/µl).
Plasma electrolytes, liver and kidney function tests were within
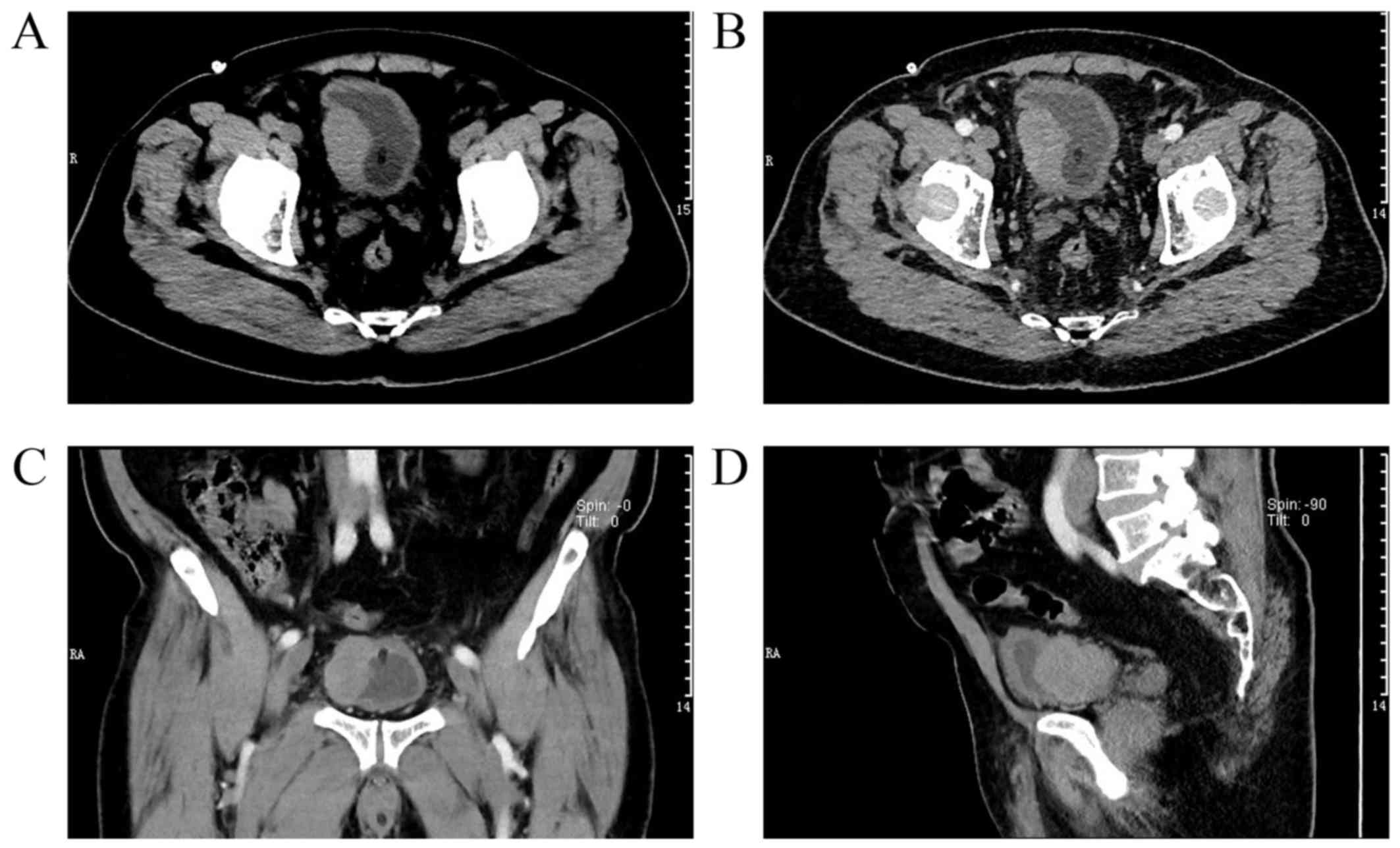
the normal range. The computed tomography (CT) scans revealed a
51×31-mm ill-defined mass involving the right wall of the urinary
bladder and the CT number was 47 HU (Fig. 1A). In addition, heterogeneous
enhancement was observed in the arterial phase (CT number: 60 HU;
Fig. 1B). Of note, the right bladder
wall was thickened locally, and it was considered likely that the
bladder cancer invaded the outer wall. Images at the coronal and
sagittal planes are shown in Fig. 1C and
D, respectively. Cystoscopic examination revealed a 4×3-cm
sessile tumor mass in the right wall of the urinary bladder. Some
of tumor tissues were clamped and removed for a biopsy. As shown in
Fig. 2, pathological examination
with hematoxylin and eosin staining demonstrated that the mucosa of
the bladder wall was extensively infiltrated by neuroendocrine
carcinoma, consistent with SCNEC. The results of
immunohistochemistry revealed that the tumor cells were
CD56+, synaptophysin (Syn)+ and epithelial
membrane antigen−. The patient refused further surgical
treatment after being informed on the associated morbidity risk,
and eventually succumbed to the disease 2 months after the
diagnosis.
Discussion
Primary SCNEC of the urinary bladder, first reported
by Cramer in 1981 (7), is a rare
aggressive malignant neoplasm with a high incidence of local
recurrence and metastasis (8,9). This
malignancy commonly affects male patients aged 50-80 years
(10,11), although it may be observed in
patients aged 35-87 years based on the current literature (12). SCNECs of the urinary bladder may be
associated with longstanding cystitis, bladder lithiasis and
smoking (6,13), as was the case in our patient. Of
note, this type of cancer more often involves the right lateral
wall of the urinary bladder. The most common clinical presentation
is hematuria, which may be accompanied by pain, dysuria,
hypertension and muscle weakness due to hypokalemia (11,14–16). The
differential diagnosis includes small-cell carcinoma of the urinary
bladder, high-grade urothelial carcinoma (lymphoma-like variant),
lymphoma, non-Hodgkin lymphoma, and metastatic malignant round-cell
neoplasms, particularly from pulmonary tissue.
There is no consensus regarding the origin and
histogenesis of SCNEC of the urinary bladder. Some researchers
hypothesized an origin from totipotent stem cells in the submucosa
of the urinary bladder. Metaplastic differentiation from
transitional cell carcinoma has also been suggested. Both
hypotheses may account for the coexistence of other histological
types of tumors occasionally seen in primary SCNECs of the urinary
bladder (11,17,18),
while malignant transformation of neuroendocrine cells is
considered to be closely associated with tumorigenesis (17,19). The
cytomorphological characteristics of primary SCNEC of the bladder
are indistinguishable from metastatic SCNEC. Ali et al
conducted a clinicopathological study with 23 patients, and
reported that isolated single cells with near-naked nuclei and
scant cytoplasm were always detected; hypercellularity and
anisonucleosis were present in 90% of the cases; other
cytomorphological characteristics included nuclear molding (75%),
hyperchromatic nuclei (75%), high mitotic karyorrhectic index (45%)
and inflammatory background (40%) (17). Diagnosis of primary SCNEC of the
bladder mainly depends on histopathology, immunohistochemistry and
cytomorphological characteristics, which is similar to SCNEC in the
lung and other tissues. An analysis of clinicopathological
characteristics revealed that 12 cases of SCNEC of the bladder
expressed CD56 (12/12), Syn (11/12), chromogranin Α (CgA; 8/12) and
thyroid transcription factor-1 (9/12) (20). Chen et al also verified that
CD56, Syn, neuron-specific enolase and CgA are positive and
sensitive markers for small-cell carcinoma of the bladder (21), which was consistent with the
immunohistochemical findings in the present case. There is no
general consensus or guideline for the management of this
malignancy. A multimodal approach is recommended by the Canadian
Association of Genitourinary Medical Oncologists (22,23).
Transurethral resection of bladder tumor and radical cystectomy are
considered as surgical treatment options based on each individual
patient (23). Adjuvant chemotherapy
has been well-documented to increase long-term survival rates.
Siefker-Radtke et al have confirmed that the
5-year survival of patients treated with radical cystectomy after
preoperative chemotherapy increased by 42% compared with patients
treated with radical cystectomy alone (24). Radiation therapy is also recommended
for SCNEC of the bladder with skull or bone metastasis (21).
The number of reports on the biological behavior and
prognosis of SCNEC of the bladder to date is insufficient. Chen
et al reported that the 1-, 2-, 3- and 4-year survival rates
were 57.78, 36.94, 16.61 and 2.97%, respectively, with a mean
survival time of 20.54 months (21).
Choong et al reported that the 5-year survival rate of
small-cell carcinoma of the bladder was 25% (4). Zhou et al demonstrated that
overall survival was associated with factors such as patient age,
size and shape of the tumor, perineuronal invasion, vascular
invasion, distant organ metastasis and pathological type (20).
In conclusion, SCNEC of the urinary bladder is a
rare aggressive malignant neoplasm with a high incidence of local
recurrence and metastasis. The diagnosis of this malignancy mainly
depends on histopathology, immunohistochemistry and
cytomorphological characteristics. Multimodal approach to treatment
is recommended, although the prognosis is poor. Long-term follow-up
is warranted due to the risk of local recurrence and distant
metastasis.
Acknowledgements
Not applicable.
Funding
This study was supported by Science and Technology
Development Fund Project of Shenzhen (grant no.
JCYJ20170307111334308), Clinical Research Project of Shenzhen
Health Commission (grant no. SZLY2018023) and the Fund of
‘San-ming’ Project of Medicine in Shenzhen (grant no.
SZSM201612066).
Availability of data and materials
Not applicable.
Authors' contributions
ZL and CL performed data collection and data
interpretation as well as drafting the manuscript. DW, CZ and JX
contributed to the study design and acquisition of data. PC, YY,
SS, JP and SY participated in the study design, data collection,
data analysis and follow-up analysis of the patient. YL contributed
to study design, as well as the analysis and interpretation of
data. All the authors have read and approved the final version of
this manuscript.
Ethics approval and consent for
publication
The study was approved by the Ethics Committee of
Peking University Shenzhen Hospital (Shenzhen, China).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the case details.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
Statistics. 2017: CA Cancer J Clin. 67:1–30. 2017.
|
|
2
|
Hussein MR, Al-Assiri M, Eid RA and
Musalam AO: Primary small cell neuroendocrine carcinoma of the
urinary bladder: A clinicopathologic, immunohistochemical and
ultrastructural evaluation. Ultrastruct Pathol. 34:232–235. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zakaria A, Al Share B, Kollepara S and
Vakhariya C: External beam radiation and brachytherapy for prostate
cancer: Is it a possible trigger of large cell neuroendocrine
carcinoma of the urinary bladder? Case Rep Oncol Med 2017.
18539852017.
|
|
4
|
Choong NW, Quevedo JF and Kaur JS: Small
cell carcinoma of the urinary bladder. The mayo clinic experience.
Cancer. 103:1172–1178. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang X, Zhang S, MacLennan GT, Eble JN,
Lopez-Beltran A, Yang XJ, Pan CX, Zhou H, Montironi R and Cheng L:
Epidermal growth factor receptor protein expression and gene
amplification in small cell carcinoma of the urinary bladder. Clin
Cancer Res. 13:953–957. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ahsaini M, Riyach O, Tazi MF, El Fassi MJ,
Farih MH, Elfatmi H and Amarti A: Small cell neuroendocrine
carcinoma of the urinary tract successfully managed with
neoadjuvant chemotherapy. Case Rep Urol. 2013:5983252013.PubMed/NCBI
|
|
7
|
Cramer SF, Aikawa M and Cebelin M:
Neurosecretory granules in small cell invasive carcinoma of the
urinary bladder. Cancer. 47:724–730. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
McClellan T, DeBord J, Franklin G and
Tierney J: Small cell neuroendocrine carcinoma of the urinary
bladder: Case report of a rare primary tumor. W V Med J.
97:151–152. 2001.PubMed/NCBI
|
|
9
|
Kickuth R, Laufer U, Pannek J, Adamietz
IA, Liermann D and Adams S: Magnetic resonance imaging of bone
marrow metastasis with fluid-fluid levels from small cell
neuroendocrine carcinoma of the urinary bladder. Magn Reson
Imaging. 20:691–694. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Holmang S, Borghede G and Johansson SL:
Primary small cell carcinoma of the bladder: A report of 25 cases.
J Urol. 153:1820–1822. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lau SK and Zhang Y: Pathologic quiz case.
A 73-year-old man with a bladder mass. Combined primary small cell
neuroendocrine carcinoma and high-grade papillary urothelial
carcinoma of the urinary bladder. Arch Pathol Lab Me.
128:1055–1056. 2004.
|
|
12
|
Nabi G, Singh I, Ansari MS, Sharma MC and
Dogra PN: Primary small cell neuroendocrine carcinoma of urinary
bladder: An uncommon entity to be recognized. Int Urol Nephrol.
33:637–640. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Alijo Serrano F, Sanchez-Mora N, Angel
Arranz J, Hernandez C and Alvarez-Fernandez E: Large cell and small
cell neuroendocrine bladder carcinoma: Immunohistochemical and
outcome study in a single institution. Am J Clin Pathol.
128:733–739. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Blomjous CE, Vos W, De Voogt HJ, Van der
Valk P and Meijer CJ: Small cell carcinoma of the urinary bladder.
A clinicopathologic, morphometric, immunohistochemical and
ultrastructural study of 18 cases. Cancer. 64:1347–1357. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Akamatsu S, Takenawa J, Kanamaru S and
Soeda A: Ectopic adrenocorticotropic hormone syndrome in a case of
small cell carcinoma of the bladder manifesting as severe muscle
weakness. Urology. 68:1122.e5–e8. 2006. View Article : Google Scholar
|
|
16
|
Partanen S and Asikainen U: Oat cell
carcinoma of the urinary bladder with ectopic adrenocorticotropic
hormone production. Hum Pathol. 16:313–315. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ali SZ, Reuter VE and Zakowski MF: Small
cell neuroendocrine carcinoma of the urinary bladder. A
clinicopathologic study with emphasis on cytologic features.
Cancer. 79:356–361. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shahab N: Extrapulmonary small cell
carcinoma of the bladder. Semin Oncol. 34:15–21. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Young RH and Parkhurst EC: Mucinous
adenocarcinoma of bladder. Case associated with extensive
intestinal metaplasia of urothelium in patient with nonfunctioning
bladder for twelve years. Urology. 24:192–195. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhou HH, Liu LY, Yu GH, Qu GM, Gong PY, Yu
X and Yang P: Analysis of clinicopathological features and
prognostic factors in 39 cases of bladder neuroendocrine carcinoma.
Anticancer Res. 37:4529–4537. 2017.PubMed/NCBI
|
|
21
|
Chen Z, Liu Q, Chen R, Liu Z, Li M, Ling
Q, Wu L, Yang J, Liu X, Wang T, et al: Clinical analysis of small
cell carcinoma of the bladder in Chinese: Nine case reports and
literature reviews. World J Surg Oncol. 15:332017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Moretto P, Wood L, Emmenegger U, Blais N,
Mukherjee SD, Winquist E, Belanger EC, Macrae R, Balogh A,
Cagiannos I, et al: Management of small cell carcinoma of the
bladder: Consensus guidelines from the Canadian Association of
Genitourinary Medical Oncologists (CAGMO). Cana Urol Assoc J.
7:E44–E56. 2013. View
Article : Google Scholar
|
|
23
|
Celik O, Ekin G, Ipekci T, Budak S and
Ilbey YO: Diagnosis and treatment in primary bladder small cell
carcinoma: Literature review. Arch Ital Androl. 88:52–55. 2016.
View Article : Google Scholar
|
|
24
|
Siefker-Radtke AO, Dinney CP, Abrahams NA,
Moran C, Shen Y, Pisters LL, Grossman HB, Swanson DA and Millikan
RE: Evidence supporting preoperative chemotherapy for small cell
carcinoma of the bladder: A retrospective review of the M. D.
Anderson cancer experience. J Urol. 172:481–484. 2004. View Article : Google Scholar : PubMed/NCBI
|