Introduction
Prostate cancer is the second most common cancer in
men following lung cancer, and the fourth most common cancer type
worldwide (1). Prostate cancer
frequently metastasizes to bone and can present as osteolytic or
osteoblastic lesions (2). Monoclonal
gammopathy of undetermined significance (MGUS) is a condition where
an abnormal protein is produced by plasma cells. The diagnostic
criteria for MGUS is M protein <3 g/dl, clonal plasma cell
population in bone marrow >10% and no end organ damage (3). MGUS has been documented to transform
into multiple myeloma (MM) or similar lymphoproliferative disorders
at a rate of 1-3% per year, or 17, 34 and 39% at 10, 20 and 25
years, respectively (4,5). In a prospective study performed in
2009, all or nearly all cases of MM were preceded by MGUS (6). The 5 year survival rate for individuals
with MM is ~45%. Therefore, it is essential that any condition,
which increases the risk of developing MM be addressed. The present
study reported two cases where it is hypothesized that metastatic
prostate cancer may have led to the condition of MGUS.
Case 1
This case study was approved by the Bioethics
Committee of the Raritan Bay Medical Center (Perth Amboy, NJ, USA).
A 76-year-old Caucasian male without significant past medical
history presented to the emergency department of the Raritan Bay
Medical Center with intractable lower back pain. The patient
started developing back pain with increasing severity, which was
aggravated by movements and decreased with rest, 2 weeks prior to
admission. The patient complained of obstructive urinary symptoms,
including hesitancy and urgency, which started 6 months previously.
Physical examination findings were normal, other than the patient
resisting movements of his lower extremities for fear of
aggravating his back pain, and his vital signs were: Blood pressure
129/88 mmHg, respiratory rate of 19/min and a temperature of
98.6°F. Laboratory examination revealed hemoglobin (Hb) levels of
12.6 g/dl, hematocrit (hct) 37.3%, white blood cells (WBC) 9.1 K/µl
and platelets 263 K/µl. A lumbar spine computed tomography (CT)
scan, without contrast, revealed a mild compression fracture,
superior endplate L2 without soft tissue involvement. Heterogeneous
appearance of osseous elements and a lytic lesion involving the
cortex of the visualized portion of the right iliac bone raised
suspicion of osseous metastases or myeloma. Additionally, the
levels of prostate-specific antigen (PSA) were determined to be
681.4 ng/ml. Based on imaging, a serum protein electrophoresis
(SPE) was performed to rule out MM. The results revealed: Serum
albumin, 2.70 l, α 1 globulin, 0.3, α 2 globulin, 0.8, β globulin,
0.7, γ globulin, 1.0 and M-spike, 0.5 (Fig. 1). A bone marrow aspirate revealed
<10% plasma cells. These results failed to meet the criteria for
MM. The patient was subsequently diagnosed with MGUS and metastatic
prostate cancer. The patient was started on bicalutamide treatment
and referred to a cancer center for further management.
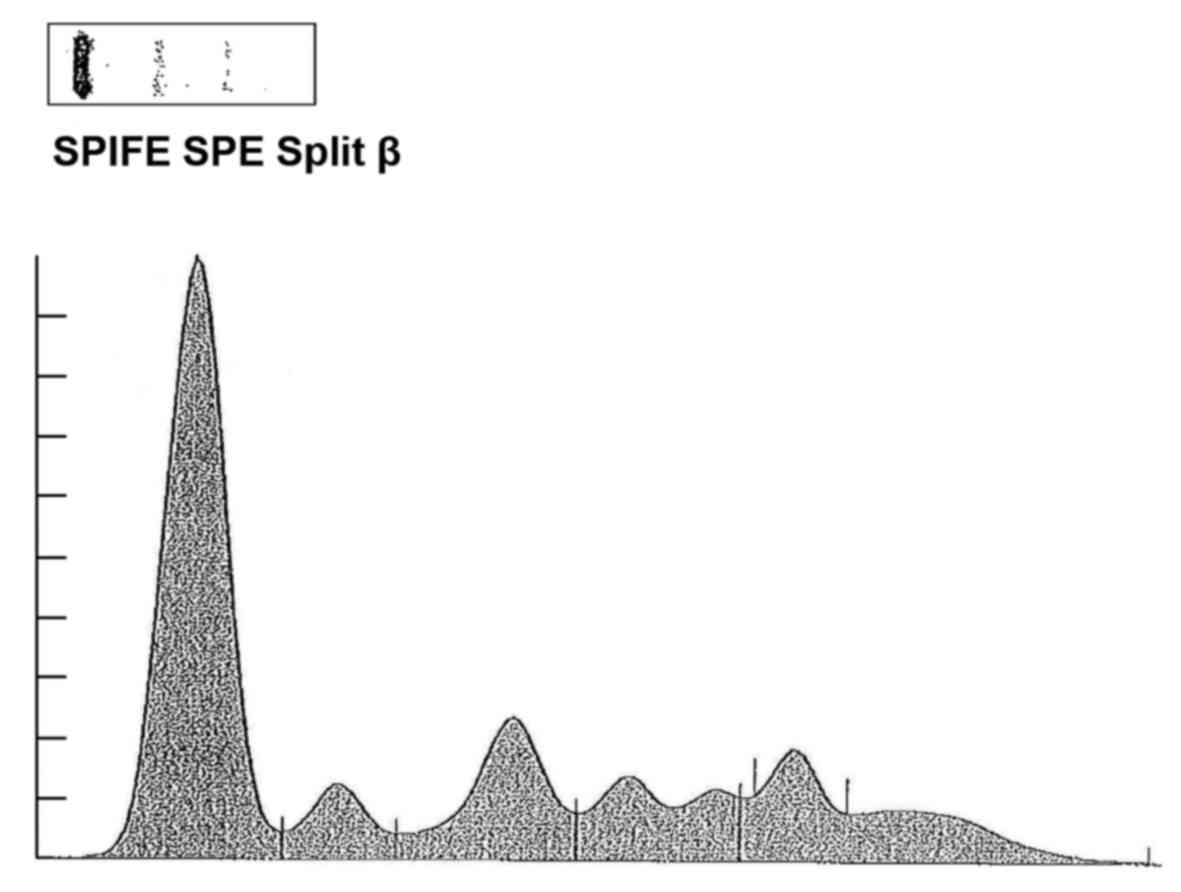
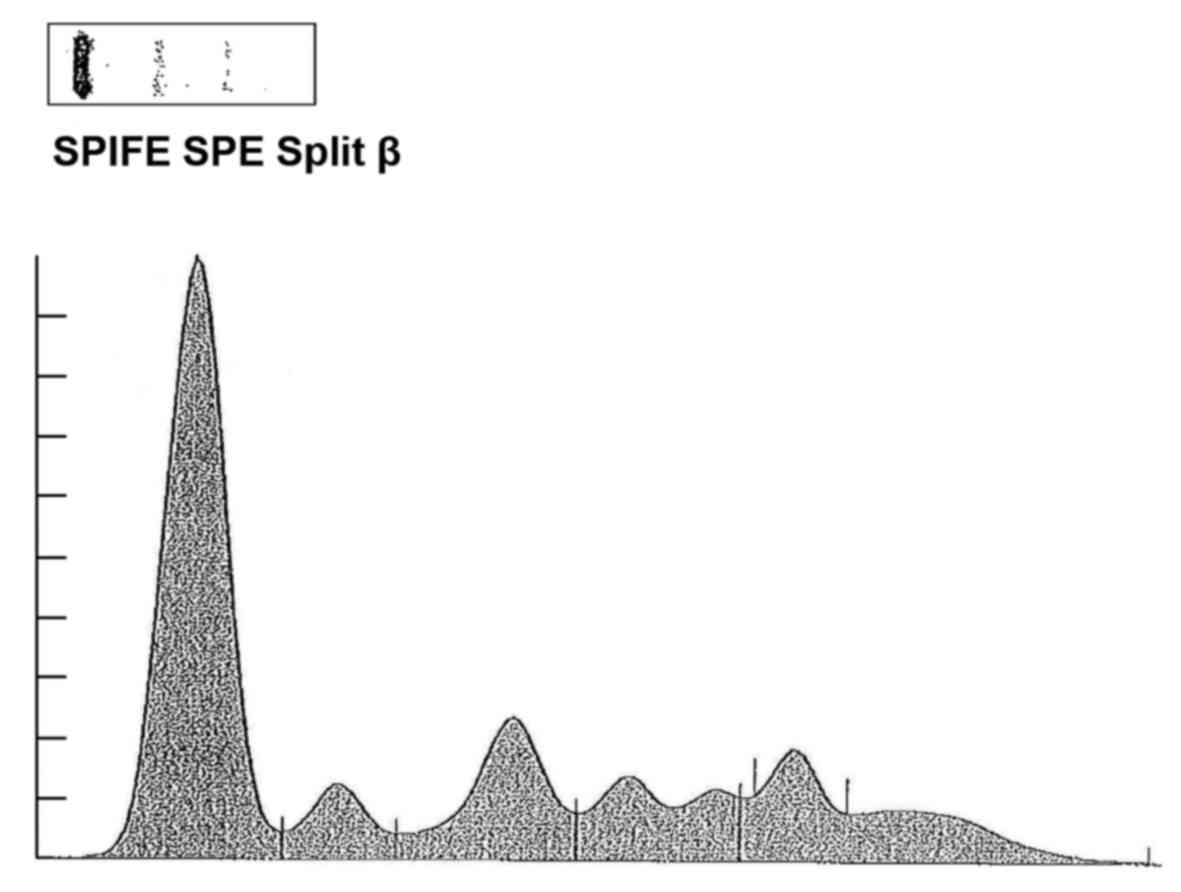 | Figure 1.SPE was performed to detect the levels
of serum albumin, 2.70 g/dl (normal, 3.2-5.6 g/dl); α 1, 0.3 g/dl
(normal, 0.1-0.4 g/dl); α 2, 0.8 g/dl (Normal 0.4-1.2 g/dl); β, 0.7
g/dl (Normal 0.6-1.3 g/dl); γ, 1.0 g/dl (normal, 0.5-1.6 g/dl);
M-spike, 0.5 g/dl. SPE, serum protein electrophoresis. |
Case 2
An 83-year-old Hispanic male, with a past medical
history significant for prostatic adenocarcinoma, presented with
altered mental status. The patient began to look very weak and
lethargic 2 days prior to admission. The family stated that the
patient had difficulty passing urine and appeared disoriented. Upon
physical examination, vital signs were a pulse rate of 101
beats/minute, blood pressure of 158/96 mmHg, temperature of 98.3°F,
respiratory rate was 18/min and the remainder of the physical exam
was unremarkable, with the exception that the patient was
lethargic. Laboratory analysis revealed: Hb 10.1 g/dl, Hct 30%, WBC
13.4 K/µl, platelets 119,000 K/µl, sodium 131 mmol/l, potassium 6.5
mmol/l, chloride 95 mmol/l, blood urea nitrogen 76 mg/dl,
creatinine 8.4 mg/dl and glucose 41 mg/dl. An electrocardiogram
revealed sinus tachycardia. A chest x-ray was within the normal
limits and a CT scan of the head revealed no acute intracranial
hemorrhage or significant mass effect. The patient was admitted to
the intensive care unit for altered mental status, secondary to
uremia, acute kidney injury and hyperkalemia. A CT urogram revealed
an enlarged and lobulated prostate gland, measuring 4.2×6.3 cm,
with consequent bilateral hydronephrosis along with small sclerotic
lesions scattered throughout the lower thoracic spine, lower
lumbosacral spine, iliac bones, left superior pubic ramus,
bilateral inferior pubic rami and left proximal femur. recom
bilateral nephrostomy tube was placed and the patient underwent
dialysis, which improved his renal function. A whole body bone scan
confirmed the findings of the CT urogram and demonstrated focal
areas of radioisotope uptake within the upper right ribs
peripherally and mid right ribs posteriorly. SPE revealed an M
spike of 0.3 (Fig. 2). Based on the
M spike and findings on imaging, the patient was diagnosed with
MGUS and metastatic prostatic adenocar cinoma upon biopsy. The
patient was started on bicalutamide and Leuprolide treatment for
metastatic prostate cancer, and was referred to a cancer center for
further management.
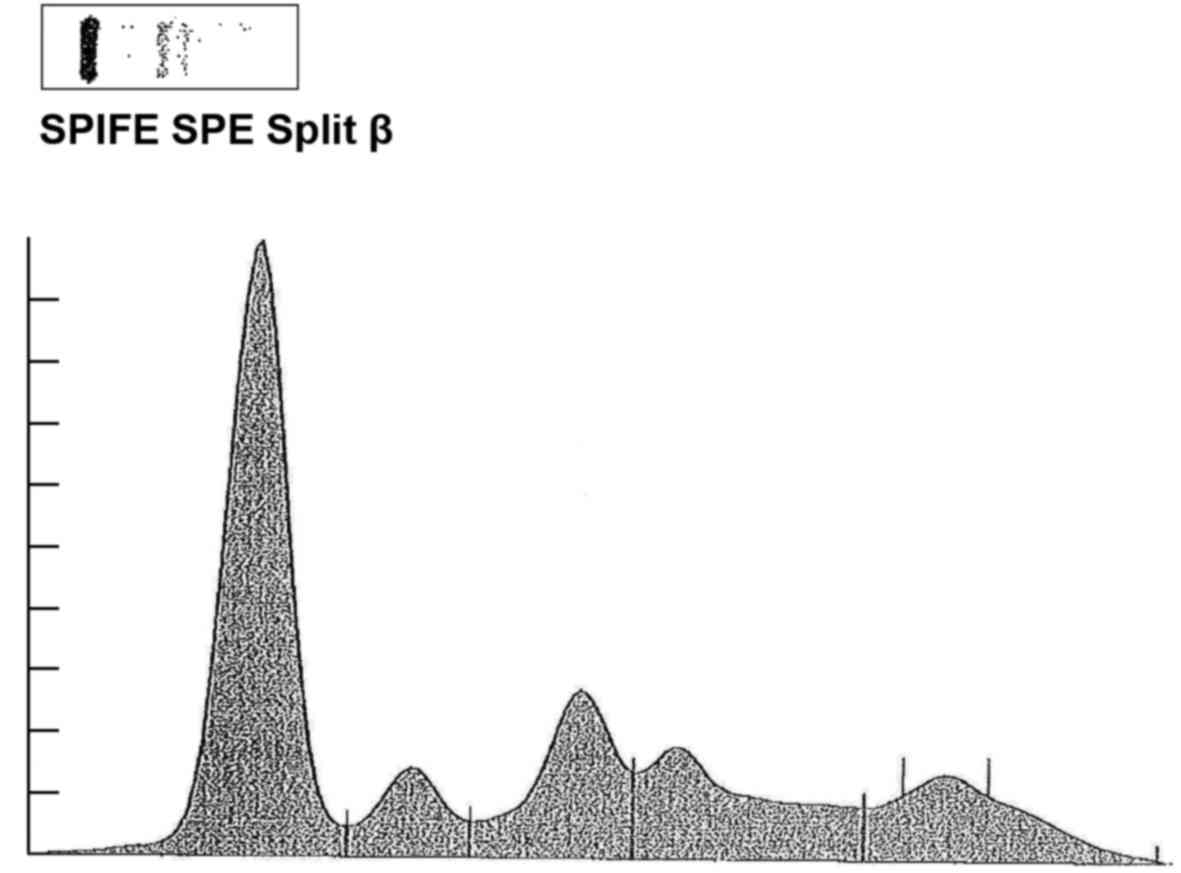
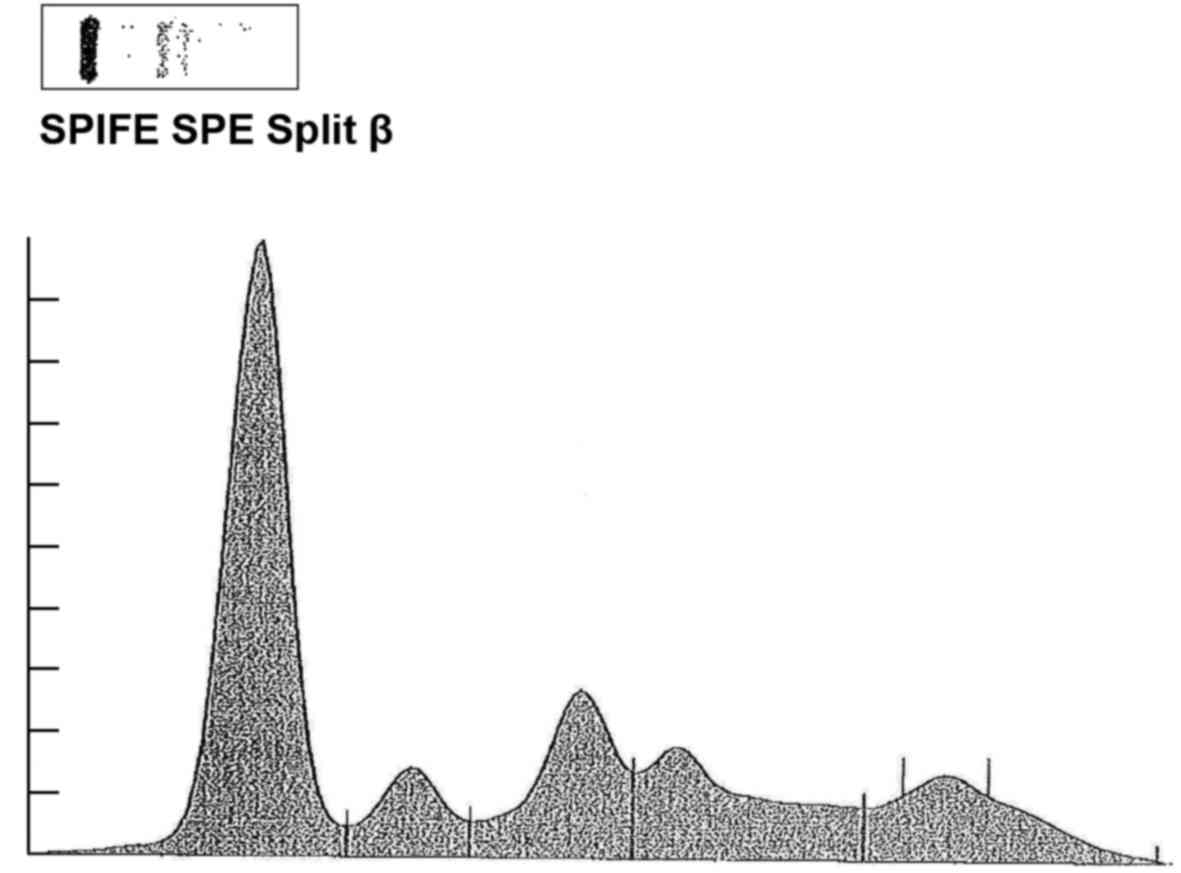 | Figure 2.SPE was performed to detect the levels
of serum albumin, 2.6 g/dl (normal 3.2-5.6 g/dl); α 1, 0.4 g/dl
(normal, 0.1-0.4 g/dl); α 2, 0.9 g/dl (normal, 0.4-1.2 g/dl); β,
0.9 g/dl (normal, 0.6-1.3 g/dl); γ, 0.7 g/dl (normal, 0.5-1.6
g/dl); M spike of 0.3 g/dl. SPE, serum protein electrophoresis. |
Discussion
In 2012, >1 million cases of prostate cancer were
diagnosed worldwide and >2/3 of those occurred in developed
nations (1). According to the
American Cancer Society, in the United States alone, 233,000 novel
cases of prostate cancer were predicted in 2014 and ~30,000 men are
expected to succumb to prostate cancer. Although the risk factors
remain to be completely understood, diet, ethnicity, age and
genetics are important. A diet consisting of red meat and large
quantities of dairy puts an individual at a greater risk of
developing prostate cancer (2). In
addition, African American men are at an increased risk of
developing prostate cancer (2,7).
Patients with prostate cancer often present with
obstructive symptoms, pain/discomfort in the lower back, hips or
thighs, and bone pain. In the majority of cases, prostate cancer
metastasizes to the bone causing osteoblastic legions, though
rarely, osteolytic lesions can be observed (2,8,9). However, since there are a large number
of prostate cancer cases, it is easy to identify a case, which may
present itself differently.
Patients with MGUS have been previously shown to
have a higher risk of developing MM, as well as Waldenstrom
macroglobulinemia, light-chain amyloidosis, or associated disorders
(10).
In the initial case in the present study, the
patient was observed to exhibit prostate cancer from the classical
signs of difficulty voiding, back pain and a high levels of PSA.
However, since the predominant complaint was the lower back pain,
the patient was initially hypothesized to exhibit metastatic spread
to the lumbar spine. The lumbar CT revealed osteolytic lesions,
which are classical for multiple myeloma, however, further studies,
including protein electrophoresis and bone marrow aspirate ruled
out MM. This raised a question about the possible scenario of
prostate cancer leading to MGUS.
A few cases have been documented in the past two
decades noting MGUS presenting with prostate cancer (3). Other cases of prostate cancer
presenting with MM have been previously observed (11). However, the present study noted that
no sufficient studies suggesting the possibility for MGUS forming
from prostate cancer existed. Although the mechanism remains to be
elucidated, chronic inflammation, in this case from cancer, is
believed to stimulate excessive growth of a single clone of a
plasma cell (3). This may lead to
MGUS and quite possibly other hematologic cancer types.
Since the patient in case 1 exhibited a high PSA
level and had trouble voiding for the past 6 months, it was
hypothesized that the prostate cancer may have been present for at
least 6-7 months. During that 6-7 months, the constant inflammation
and proliferation of the plasma cells may have resulted in MGUS.
Furthermore, it is likely that the osteolytic lesions are from
prostate cancer since the patient does not fit into any other
characteristics of MM.
The patient in case 2 presented with a history of
prostate cancer, diagnosed 13 years previously, which has now
recurred along with being newly diagnosed with MGUS. Based on the
levels of M protein and the exponential increase in the risk of
MGUS turning into MM or other lymphoproliferative disorders, the
present study hypothesized that his MGUS is in fact a novel
development likely to be caused by his prostate cancer.
Currently, recommendations for evaluating patients
with high risk MGUS are using baseline bone marrow examination with
cytogenetics and fluorescence in situ hybridization
(12). Additionally it is
recommended that these patients undergo bone imaging studies, and
SPE every 6 months for the first year, followed by an annual SPE
(13). Although MGUS is generally a
benign condition, the possibility of MGUS becoming MM warrants the
requirement for careful observation and annual studies. The present
study recommend that patients with prostate cancer have more
frequent clinical examinations, as well as using SPE, in order to
diagnose lymphoproliferative disorders at an earlier stage.
Glossary
Abbreviations
Abbreviations:
|
CT
|
computed tomography
|
|
MGUS
|
monoclonal gammopathy of undetermined
significance
|
|
MM
|
multiple myeloma
|
|
SPE
|
serum protein electrophoresis
|
References
|
1
|
Mandair D, Rossi RE, Pericleous M, Whyand
T and Caplin ME: Prostate cancer and the influence of dietary
factors and supplements: A systematic review. NutrMetab (Lond).
11:302014. View Article : Google Scholar
|
|
2
|
Rajendiran G, Green L and Chhabra G: A
rare presentation of prostate cancer with diffuse osteolytic
metastases and PSA of 7242 ng/ml. International Journal of Case
Reports and Images. 2:16–20. 2011. View Article : Google Scholar
|
|
3
|
Tsutsumi M, Hara T, Fukasawa R and Koiso
K: Prostatic cancer presenting monoclonal gammopathy: Report of two
cases. Hinyokika Kiyo. 39:569–571. 1993.PubMed/NCBI
|
|
4
|
Bladé J: Clinical practice. Monoclonal
gammopathy of undetermined significance. N Engl J Med.
355:2765–2770. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kyle RA, Therneau TM, Rajkumar SV, Offord
JR, Larson DR, Plevak MF and Melton LJ: A long-term study of
prognosis in monoclonal gammopathy of undetermined significance. N
Engl J Med. 346:564–569. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Landgren O, Kyle RA, Pfeiffer RM, Katzmann
JA, Caporaso NE, Hayes RB, Dispenzieri A, Kumar S, Clark RJ, Baris
D, et al: Monoclonal gammopathy of undetermined significance (MGUS)
consistently precedes multiple myeloma: A prospective study. Blood.
113:5412–5417. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Roberts R: From bench to bedside: The
realities of reducingglobalprostatecancerdisparity in black men.
Ecancermedicalscience. 28:4582014.
|
|
8
|
Vinjamoori AH, Jagannathan JP, Shinagare
AB, Taplin ME, Oh WK, Van den Abbeele AD and Ramaiya NH: Atypical
metastases from prostate cancer: 10-year experience at a single
institution. AJR AM J Roentgenology. 199:367–372. 2012. View Article : Google Scholar
|
|
9
|
Migita T, Maeda K and Ogata N: A case of
prostate cancer associated with osteolytic bone metastases.
Hinyokika Kiyo. 45:371–374. 1999.(In Japanese). PubMed/NCBI
|
|
10
|
Kyle RA: Monoclonal gammopathy of
undetermined significance: Natural history in 241 cases. Am J Med.
64:814–826. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pérez López ME, Garcia Mata, Garcia Gómez
J, Salgado Fernández M and Fírvida Pérez JL: Prostate
adenocarcinoma and synchronous multiple myeloma: A case report.
ActasUrol Esp. 31:157–159. 2007.(In Spanish). View Article : Google Scholar
|
|
12
|
Kyle RA, Buadi F and Rajkumar SV:
Management of monoclonal gammopathy of undetermined significance
(MGUS) and smoldering multiple myeloma (SMM). Oncology (Williston
Park). 7:578–586. 2011.
|
|
13
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: GLOBOCAN 2008 v2.0, Cancer incidence and
mortality worldwide: IARC CancerBase No. 10. Int Agency Res Canc.
2010.
|