Introduction
Alzheimer's disease (AD) is a chronic, progressive
and irreversible neurodegenerative disease with clinical features
of memory loss, dementia and cognitive impairment. It is the most
common cause of dementia among the elderly, accounting for 50–70%
of all cases worldwide (1–3). AD is a multifactorial disorder,
involving several pathological mechanisms. It is
histopathologically characterized by the presence of senile
plaques, neurofibrillary tangles and neuron loss in the brain. In
particular, the senile plaques are extracellular deposits of
amyloid-β peptide (Aβ), which is cleaved from the amyloid precursor
protein. However, the exact mechanism triggering neurodegeneration
in AD remains to be fully elucidated, and there is no effective
treatment to prevent or reverse AD at present (4,5).
The inflammatory response is a beneficial host
immune response to tissue injury or infection. However, it may lead
to potentially damaging consequences and result in several
inflammatory diseases and types of cancer (6). In AD, the activation and accumulation
of microglial cells around amyloid plaques has long been described
and is considered to result in chronic neuroinflammation, which
leads to the production of proinflammatory cytokines, including
interleukin (IL)-1β and tumor necrosis factor (TNF)-α, followed by
neurodegeneration (7,8). The different functions of microglial
cells on the progression of AD have been considered to be a
double-edged sword; as Aβ is able to activate microglia and
initiate an inflammatory response, microglia may be important in
the clearance of Aβ peptides in the early stages (9,10).
However, the over stimulation of microglia cells can lead to the
excessive secretion of pro-inflammation cytokines, thus forming a
chronic neuro-inflammatory reaction in AD. Therefore, it is
critical to maintain the beneficial functions of microglial cells
and avoid neurotoxin production, which may offer useful therapeutic
strategies for AD.
Nuclear factor (NF)-κB is a transcription factor,
which is critical in regulating cellular proliferation,
inflammatory responses and cell adhesion (11). Inactive NF-κB complexes are
sequestered in the cytoplasm via binding to the inhibitory protein
(IκB). Once activated, IκB proteins are phosphorylated rapidly, and
the phosphorylated IκB proteins are targeted for ubiquitination and
degradation. The free NF-κB then translocates into the nucleus
where it regulates the production of various pro-inflammatory
mediators (12,13). It has been shown that microglia
express activated NF-κB in AD (14,15).
Mitogen-activated protein kinase (MAPK), namely, the extracellular
signal-regulated protein kinase, the c-Jun N-terminal kinase (JNK),
p38 MAPK and atypical MAPKs, is one of the signal transduction
cascades involved in the regulation of inflammatory mediators
(16). The activation of MAPK
signaling pathways has been reported to be involved in the
development of several human diseases, including AD and Parkinson's
disease (17–19). Therefore, the NF-κB and MAPK
signaling pathways serve as important molecular targets for the
development of potential anti-inflammatory drugs.
The Gengnianchun (GNC) formula has long been used in
China to treat perimenopausal syndrome (PMS) clinically, and is
particularly effective in improving learning ability and memory
(20,21). Previous studies have shown the
anti-inflammatory and neuroprotective effects of GNC (22,23).
In the present study, the anti-inflammatory properties of GNC and
its underlying molecular mechanism of action were investigated in
BV-2 microglial cells.
Materials and methods
Materials and reagents
Synthetic Aβ (1–42) was purchased from AnaSpec, Inc.
(San Jose, CA, USA). Minimum essential medium (MEM), fetal bovine
serum (FBS) and phosphate-buffered saline (PBS) were purchased from
Gibco; Thermo Fisher Scientific, Inc. (Waltham, MA, USA). Cytokine
(IL-1β and TNF-α) enzyme-linked immunosorbent assay (ELISA) kits
were purchased from R&D Systems, Inc. (Minneapolis, MN, USA). A
Cell Counting Kit-8 (CCK-8) was obtained from Dojindo Molecular
Technologies, Inc. (Kumamoto, Japan). Antibodies against
phosphorylated JNK (p-JNK) and p-p65 were purchased from Cell
Signaling Technology, Inc. (Danvers, MA, USA). All other chemicals
were purchased from common commercial suppliers.
Preparation of medicated rat
serum
A single unit of GNC formula was 138 g total weight,
composed of 12 crude herbs: 15 g Radix Rehmanniae (Shengdihuang),
12 g of Herba Epimedium brevicornum (Yinyanghuo), Radix Paeoniae
Alba (Baishao), Semen Cuscuta (Tusizi), Wolfberry fruit (Gouqizi),
Radix Morindae officinalis (Bajitian) and Herba Cistanche
(Roucongrong), 15 g of Tortoise shell (Guijia) and Rhizoma
anemarrhenae (Zhimu), 9 g of Poria (Fuling) and Cortex Phellodendri
(Huangbai), and 3 g of Rhizoma Coptidis (Huanglian). A total of 138
g of herb mixture was reduced to 25 g of concentrated powder by
Jiangyin Tianjiang Pharmaceutical Co., Ltd. (Shanghai, China). A
total of 40 female SD rats (3 months old and weighing 250±20 g)
were obtained from the Experimental Animal Center of the Chinese
Academy of Sciences [Shanghai, China, license no. SCXK (Hu)
2012–0002]. The rats were housed at 23–25°C with 55% humidity, a
12-h light/dark cycle and free access to food and tap water. All
the rats were bilaterally ovariectomized following anaesthetization
with an intraperitoneal injection with 4% chloral hydrate. After 7
days, the rats were randomly divided into two groups. One group was
intragastrically administered with GNC (25 g powder dissolved in
100 ml normal saline) at a dose of 5 g/kg. The rats in the other
group were administered with normal saline at the same volume for 5
days. At 1 h following the final administration, serum was obtained
by centrifugation (3,000 × g for 10 min at 4°C). The serum was
sterilized by vacuum filtration and stored at −20°C.
Cell culture and treatment
The murine microglia BV-2 cell line was purchased
from the China Center for Type Culture Collection (Wuhan, China)
and cultured in MEM supplemented with FBS (10%), 100 U/ml
penicillin and 100 µg/ml streptomycin at 37°C in a humidified cell
incubator in a 95/5% (v/v) mixture of air and CO2. The
BV-2 microglial cells, seeded in a 96-well plate at a density of
1×104/well, were pretreated with different
concentrations of MRS (2.5, 5, 10 and 20%) for 2 h, and were then
incubated with 5 µM Aβ (1–42) for another 12 h at 37°C. In the
preliminary experiments to determine the effect of different
concentrations of Aβ (1–42) on the secretion of IL-1β and TNF-α,
the microglial cells were seeded at a density of
1×104/well in a 96-well plate and treated with Aβ (1–42)
at different concentrations (2.5, 5, 10 and 20 µM). Subsequently,
microglial cells seeded on a 96-well plate at a density of
1×104/well were treated with 5 µM Aβ (1–42) for the
indicated periods of time. Following treatment, the supernatant was
collected and stored at −80°C for measuring the protein levels of
IL-1β and TNF-α using ELISA.
Cell viability
The cell viability was detected using a CCK-8.
Briefly, 100 µl of BV2 cell suspension (1×104
cells/well) was seeded into 96-well plates overnight, following
which the supernatant was removed and the cells were incubated in
FBS-free medium for 12 h. MRS was then added at the various
concentrations for 24 h. Following treatment, the cell viability
was assessed using the CCK-8. The optical density was measured at
450 nm.
ELISA
The protein levels of IL-1β and TNF-α in the
supernatant of the cultured BV2 microglial cells were measured
using an ELISA kit according to the manufacturer's protocol.
Western blot analysis
To confirm the effects of MRS on the Aβ
(1–42)-induced activation of NF-κB and JNK in the BV2 microglia
cells, protein extracts from the cell cultures were obtained using
a commercial extract kit (Active Motif, Carlsbad, CA, USA) and
analyzed using western blot analysis according to standard
protocols. The cells were lysed in lysis buffer (Biyuntian Biotech
Co., Ltd., Shanghai, China) following the manufacturer's protocols.
A bicinchoninic acid assay (Biyuntian Biotech Co., Ltd., Shanghai,
China) was used to determine concentration of the protein lysate.
The extracts, containing 30 µg proteins, were loaded on a 10%
SDS-PAGE gel. Following electrophoresis, the proteins were
transferred onto a polyvinylidene fluoride (PVDF) membrane
(Invitrogen; Thermo Fisher Scientific, Inc.). Following blocking
with 5% BSA for 1 h at room temperature, the PVDF membrane was
incubated with the p-p65 antibody (3033; 1:1,000; Cell Signaling
Technology, Inc., Danvers, MA, USA A), p-JNK antibody (4668;
1:1,000; Cell Signaling Technology, Inc.), and β-actin antibody
(ab8229; 1:1,000; Abcam, Cambridge, UK) at 4°C overnight.
Subsequently, the membrane was incubated with a horseradish
peroxidase-conjugated secondary antibody (SA00001-15; 1:5,000;
Proteintech Group, Inc., Chicago, IL, USA) for 1 h at room
temperature. Following three washes, the immune complexes were
detected using an electrochemiluminescence system. Images were
captured using the ImageQuant LAS 4000 mini analyzer (General
Electric Company, Fairfield, CT, USA).
Statistical analysis
Each experiment was repeated at least three times.
The data are expressed as the mean ± standard deviation. The
statistical significance was analyzed by one-way analysis of
variance followed by Fisher's LSD-t post hoc test. Statistical
analysis was performed using SPSS software (version 16.0; SPSS,
Inc., Chicago, IL, USA) to determine significant differences.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Effects of Aβ on the secretion of
pro-inflammatory cytokines in BV-2 microglial cells
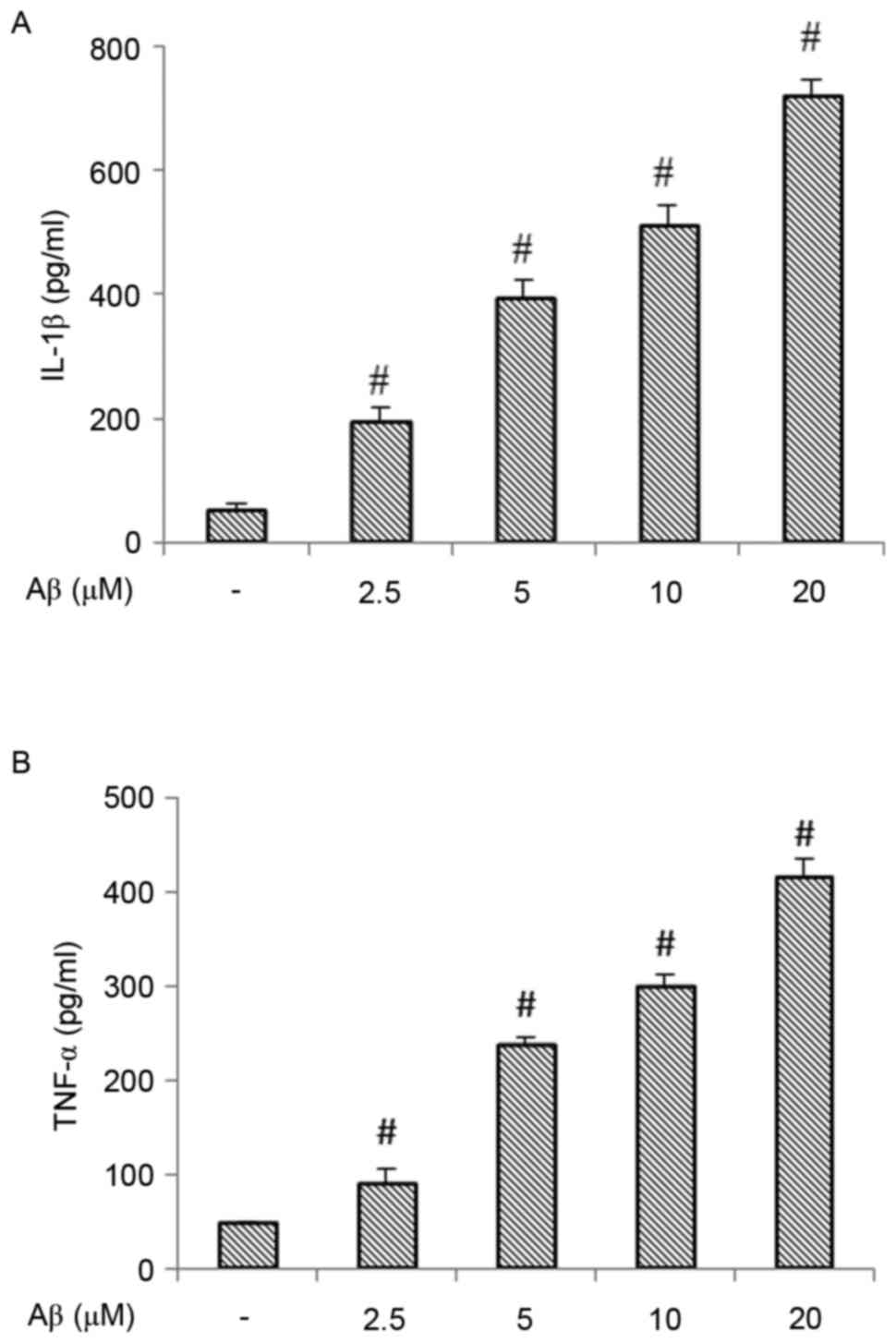
In order to assess the pro-inflammatory properties
of Aβ in BV-2 microglial cells, the present study measured the
effects of Aβ on the production of pro-inflammatory cytokines. As
shown in Fig. 1A and B, treatment
with 2.5–20 µM Aβ dose-dependently induced the release of IL-1β and
TNF-α.
MRS inhibits the release of
pro-inflammatory cytokines in β-stimulated BV-2 microglial
cells
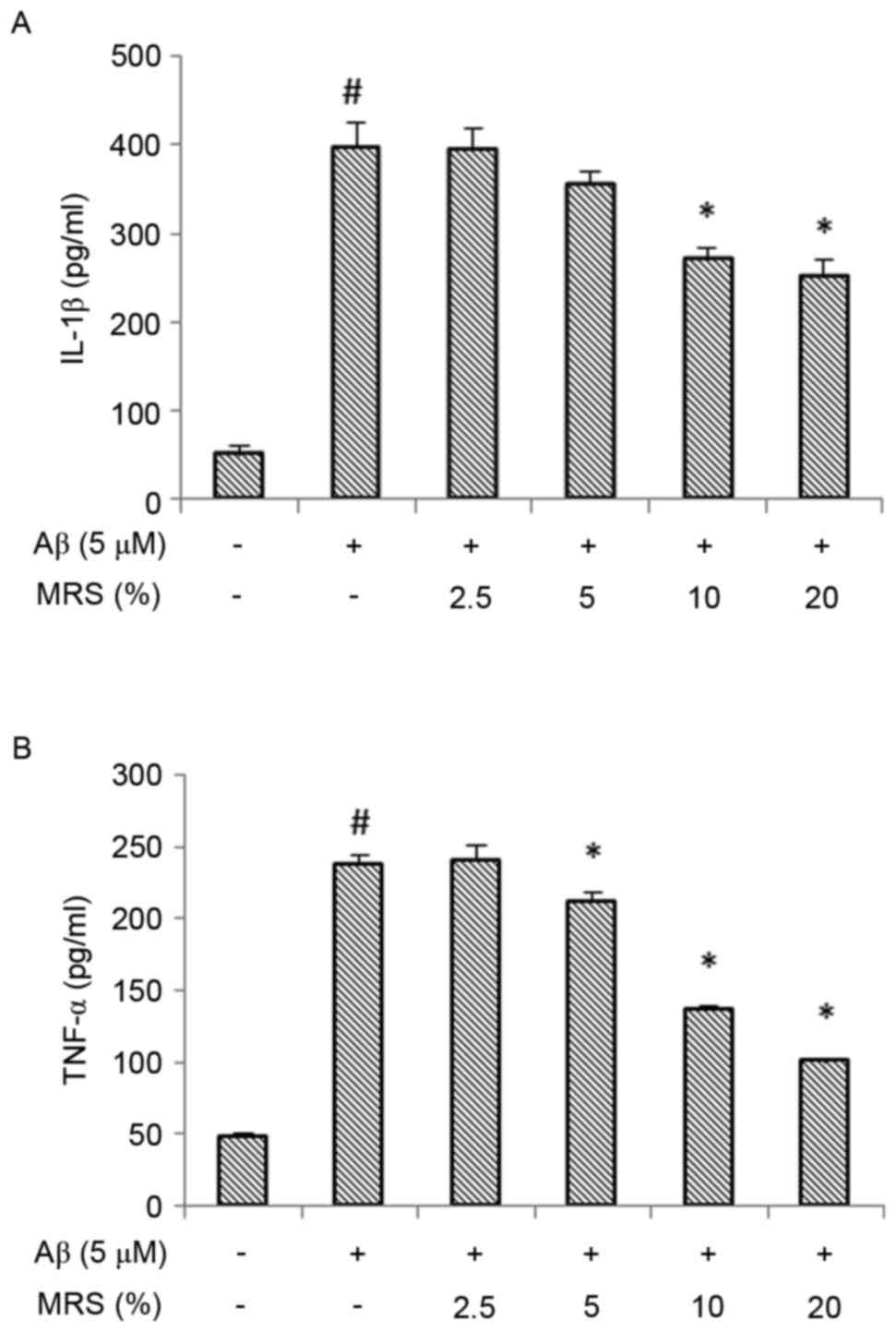
Stimulation of the BV-2 microglial cells with Aβ
increased the expression of pro-inflammatory cytokines. As shown in
Fig. 2, the protein expression
levels of IL-1β and TNF-α were significantly increased following
treatment with Aβ, compared with the levels in the normal control
group (P<0.01). However, treatment with MRS significantly
attenuated the Aβ-induced secretion of these pro-inflammatory
cytokines. At concentrations of 10–20%, MRS significantly
attenuated the Aβ-induced protein expression of IL-1β (Fig. 2A). The increase in the protein
expression of TNF-α was also reduced significantly following
treatment with MRS at concentrations of 5–20% (Fig. 2B).
Cell viability
To confirm that the anti-inflammatory property of
MRS was not due to cytotoxic effects on the BV-2 microglial cells,
a CCK-8 assay was performed. As shown in Fig. 3, the viability of the BV-2 cells
was not reduced following treatment with various concentrations of
MRS, suggesting that the inhibitory effects of the Aβ-induced
inflammatory response did not result from its cytotoxic action.
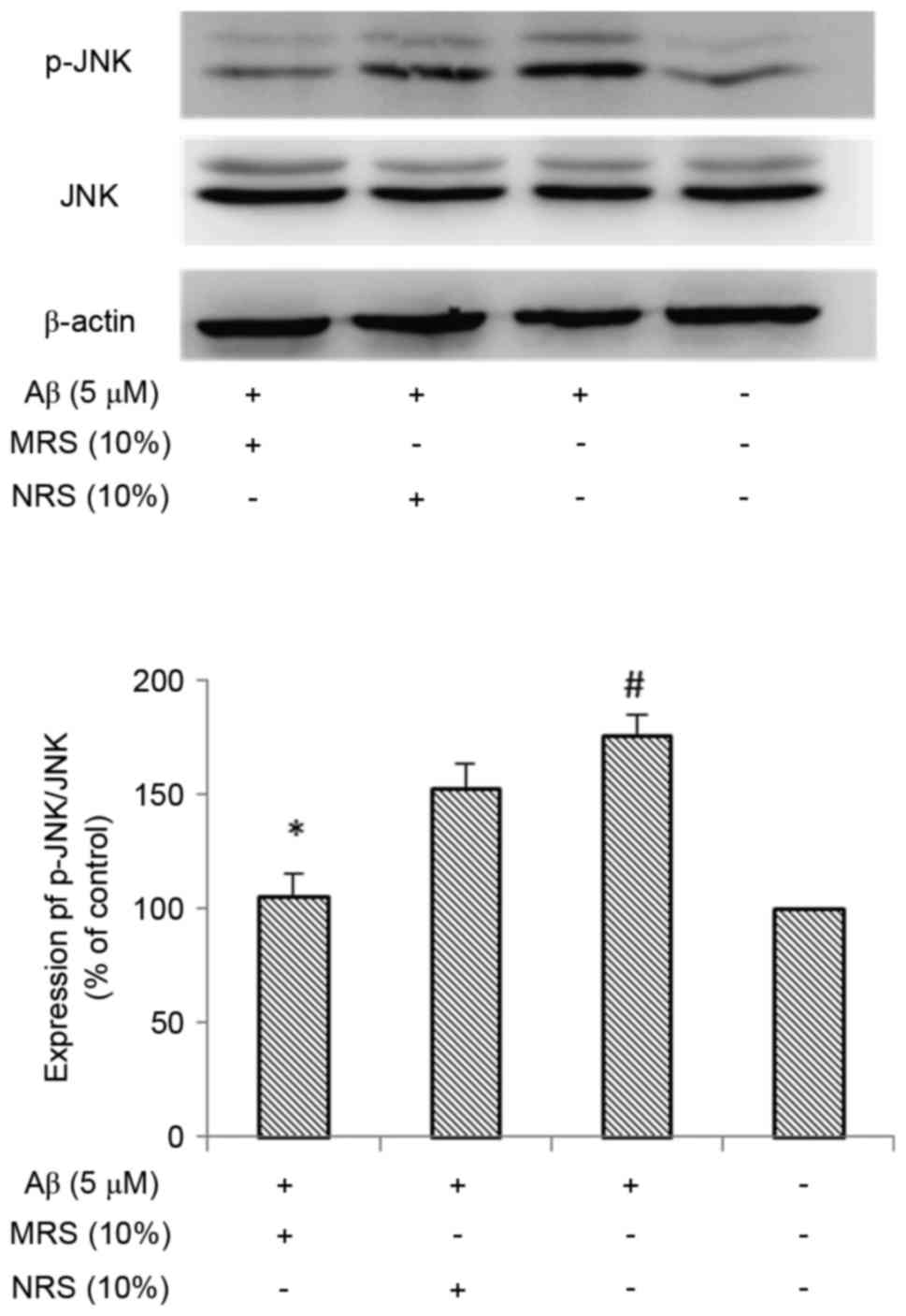
MRS inhibits the Aβ-induced activation
of NF-κB and JNK in BV-2 microglial cells
As NF-κB is known to be key in the inflammatory
response, the present study investigated whether NF-κB is involved
in suppression of the inflammatory response induced by MRS. The
effect of MRS on Aβ-induced NF-κB activation was examined using
western blot analysis. It is known that the phosphorylation of
NF-κB is considered a marker of NF-κB activation. As shown in
Fig. 4, the phosphorylation of
NF-κB was markedly increased following treatment with Aβ, compared
with that in the normal control group (P<0.01). No marked
reduction in the Aβ-induced phosphorylation of NF-κB was observed
in the non-medicated rat serum (NRS) group, however, treatment with
MRS resulted in a significant reduction in the phosphorylation of
NF-κB (P<0.05). As there is a crosstalk between NF-κB and MAPK,
and this crosstalk is important for maximal activation of genes
associated with inflammation, the present study examined the effect
of MRS on MAPK activity, which regulates the function of NF-κB. As
shown in Fig. 5, the
phosphorylation level of JNK was markedly increased following
treatment with Aβ, compared with that in the normal control group
(P<0.01), whereas treatment with MRS significantly inhibited
Aβ-induced JNK activation (P<0.05). Again, the NRS group had no
effect on reducing the Aβ-induced phosphorylation of JNK. These
data suggested that the inhibitory effect of MRS on the Aβ-induced
inflammatory response occurred through suppressing the activation
of NF-κB and JNK in the BV-2 microglial cells.
Discussion
AD is a chronic, progressive and irreversible
neurodegenerative disease, with characteristics of memory loss and
cognitive impairment. Although the exact pathophysiologic mechanism
of AD remains to be elucidated, there is accumulating evidence that
neuroinflammation is critical in the pathogenesis of AD (5). AD is characterized by senile plaques,
neurofibrillary tangles, and loss of neurons and synapses. Aβ
peptide accumulation is a major pathological hallmark of AD. In the
AD brain, microglial cells are found in close association with Aβ
deposits. It is widely accepted that inflammation in the central
nervous system is characterized by the activation of microglial
cells, and the production of pro-inflammatory cytokines and
chemokines. Furthermore, the release of neuroinflammatory cytokines
is harmful to neighboring healthy cells. Over previous years, the
process of inflammation has increased in interest in AD, not only
for its potential role in neurodegenerative disease but as a
potential therapeutic approach. Therefore, regulating
microglia-mediated neuroinflammation and neurotoxicity is
considered to be an important therapeutic target in the treatment
of neurodegenerative disorders (24). However, the exact mechanism
underlying the release of these pro-inflammatory cytokines in
activated microglial cells remains to be elucidated.
The NF-κB and MAPK signaling pathways are known to
be crucial in inflammatory gene regulation and are considered to
have an important function in the production of pro-inflammatory
cytokines induced by Aβ. Regarding the NF-κB signaling pathway,
various irritants, including Aβ, can activate it. A number of
studies have reported that NF-κB is a major signaling molecule
involved in inflammatory response (11,12).
The MAPK signaling pathway has been shown to be involved in the
Aβ-mediated production of several inflammatory genes, which are
important for the activation of NF-κB. It is known that there is
crosstalk between the NF-κB and MAPK signaling pathways, which is
important for maximum activation of genes associated with
inflammation. The present study provided definitive evidence that
the NF-κB and JNK signaling pathways were activated following Aβ
treatment in microglial cultures. It was found that Aβ treatment
significantly increased the phosphorylation of NF-κB p65 and JNK,
which are considered to be markers of NF-κB and JNK activation,
upregulating the expression of pro-inflammatory cytokines,
including IL-1β and TNF-α. Therefore, NF-κB and JNK may be
considered as targets for the molecular therapy of AD.
The GNC formula, as a traditional Chinese decoction,
has long been used in China to treat PMS clinically, and is
particularly effective in improving learning ability and memory
(20,21). Previous investigations have
demonstrated the anti-inflammatory and neuroprotective effects of
GNC (22,23). Similarly, the results of the
present study showed that serum containing GNC formula
significantly reduced the expression levels of IL-1β and TNF-α,
accompanied by the inhibition of NF-κB and JNK activation in
microglial cultures treated with Aβ. The present study also showed
that the inhibitory effect of MRS on the expression levels of IL-1β
and TNF-α was not due to its direct toxicity on microglial cells,
as the different concentrations (2.5–20%) of GNC formula in the
serum did not affect microglial cell viability.
Microglial cells are the primary immune effector
cells of the brain, with an integral role in maintaining brain
homeostasis and protecting the brain from infections. However, the
persistent stimulation of microglial cells is considered to
contribute to neurodegenerative disease through increasing the
production of pro-inflammatory cytokines, including IL-1β and
TNF-α. Several inflammatory mediators, including IL-1β and TNF-α,
are considered to be critical in the inflammatory process of AD.
There is an increase in the release of these pro-inflammatory
cytokines from microglial cells following exposure to Aβ.
Therefore, decreasing these pro-inflammatory cytokines offers an
alternative therapy for AD. However, the inflammatory mediators,
including pro-inflammatory cytokines, represent downstream
molecules only, and the NF-κB and MAPK signaling pathways are the
common pathways in the inflammatory cascade. Therefore, in order to
obtain optimal therapeutic benefits, therapies interfering with key
components of the inflammatory cascade, including NF-κB and JNK,
may be more efficient. Therefore, GNC may be a potential drug in
the treatment of AD as the therapeutic targets of GNC are critical
and multiple.
In conclusion, the present study showed that GNC
formula mediated its anti-inflammatory effects through decreasing
pro-inflammatory cytokines and by suppressing the activation of
NF-κB and JNK in Aβ-stimulated microglial cells. The treatment of
AD remains a challenge, however, these findings suggested that GNC
inhibits the release of neurotoxic products in the central nervous
system. Therefore, GNC formula may be a useful therapeutic drug to
prevent AD.
Acknowledgements
This study was supported by National Natural
Sciences Foundation of China (grant no. 81273956) and Scientific
Research Project of the Shanghai Committee of Science and
Technology, China (grant no. 15401931800) awarded to Dr Wen-Jun
Wang.
Glossary
Abbreviations
Abbreviations:
|
AD
|
Alzheimer's disease
|
|
Aβ
|
amyloid-β peptide
|
|
GNC
|
Gengnianchun formula
|
|
MRS
|
medicated rat serum containing GNC
|
|
NRS
|
non-medicated rat serum
|
|
IL-1β
|
interleukin-1β
|
|
TNF-α
|
tumor necrosis factor-α
|
|
JNK
|
c-Jun N-terminal kinase
|
|
NF-κB
|
nuclear factor-κB
|
References
|
1
|
Mattson MP: Pathways towards and away from
Alzheimer's disease. Nature. 430:631–639. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Blennow K, de Leon MJ and Zetterberg H:
Alzheimer's disease. Lancet. 368:387–403. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wortmann M: Dementia: A global health
priority-highlights from an ADI and World Health Organization
report. Alzheimers Res Ther. 4:402012.PubMed/NCBI
|
|
4
|
Huang Y and Mucke L: Alzheimer mechanisms
and therapeutic strategies. Cell. 148:1204–1222. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Iqbal K and Grundke-Iqbal I: Alzheimer's
disease, a multifactorial disorder seeking multitherapies.
Alzheimers Dement. 6:420–424. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rodriguez-Vita J and Lawrence T: The
resolution of inflammation and cancer. Cytokine Growth Factor Rev.
21:61–65. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liu L and Chan C: The role of inflammasome
in Alzheimer's disease. Ageing Res Rev. 15:6–15. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mandrekar-Colucci S and Landreth GE:
Microglia and inflammation in Alzheimer's disease. CNS Neurol
Disord Drug Targets. 9:156–167. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Solito E and Sastre M: Microglia function
in Alzheimer's disease. Front Pharmacol. 3:142012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Prokop S, Miller KR and Heppner FL:
Microglia actions in Alzheimer's disease. Acta Neuropathol.
126:461–477. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Makarov SS: NF-kappaB as a therapeutic
target in chronic inflammation: Recent advances. Mol Med Today.
6:441–448. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Roshak AK, Callahan JF and Blake SM:
Small-molecule inhibitors of NF-kappaB for the treatment of
inflammatory joint disease. Curr Opin Pharmacol. 2:316–321. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mattson MP: NF-kappaB in the survival and
plasticity of neurons. Neurochem Res. 30:883–893. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Boissiere F, Hunot S, Faucheux B,
Duyckaerts C, Hauw JJ, Agid Y and Hirsch EC: Nuclear translocation
of NF-kappaB in cholinergic neurons of patients with Alzheimer's
disease. Neuroreport. 8:2849–2852. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mattson MP and Camandola S: NF-kappaB in
neuronal plasticity and neurodegenerative disorders. J Clin Invest.
107:247–254. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Harper SJ and Wilkie N: MAPKs: New targets
for neurodegeneration. Expert Opin Ther Targets. 7:187–200. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mehan S, Meena H, Sharma D and Sankhla R:
JNK: A stress-activated protein kinase therapeutic strategies and
involvement in Alzheimer's and various neurodegenerative
abnormalities. J Mol Neurosci. 43:376–390. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Correa SA and Eales KL: The role of p38
MAPK and its substrates in neuronal plasticity and
neurodegenerative disease. J Signal Transduct. 2012:6490792012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhao H, Wang SL, Qian L, Jin JL, Li H, Xu
Y and Zhu XL: Diammonium glycyrrhizinate attenuates
Aβ(1–42)-induced neuroinflammation and regulates MAPK and NF-κB
pathways in vitro and in vivo. CNS Neurosci Ther. 19:117–124. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Suyu J and Meijuan W: Clinical observation
of ‘climacterium capsule’ in improving the memory of climacterium
women. Shanghai Zhong Yi Yao Za Zhi. 35:32–33. 2001.(In
Chinese).
|
|
21
|
Zhao FG, Wang WJ and Zhou WJ: Effect of
Gengnianchun recipe on learning memory function and hippocampal
cholinergic system in ovariectmized rats. Zhongguo Zhong Xi Yi Jie
He Za Zhi. 28:234–237. 2008.(In Chinese). PubMed/NCBI
|
|
22
|
Li J, Li B, Zhou WJ, Zhao FG, Li DJ and
Wang WJ: Medicated rat serum containing Gengnianchun decoction
reduces apoptosis of pheochromocytoma cells insulted by amyloid
beta protein. Zhong Xi Yi Jie He Xue Bao. 8:472–479. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jun L, Wenjun W, Dajin L and Wenjiang Z:
Gengnianchun recipe inhibits apoptosis of pheochromocytoma cells
from beta-amyloid 25–35 insult, better than monotherapies and their
compounds. Neur Regen Res. 6:2815–2821. 2011.
|
|
24
|
Lee JW, Lee YK, Yuk DY, Choi DY, Ban SB,
Oh KW and Hong JT: Neuro-inflammation induced by lipopolysaccharide
causes cognitive impairment through enhancement of beta-amyloid
generation. J Neuroinflammation. 5:372008. View Article : Google Scholar : PubMed/NCBI
|