Introduction
Colorectal cancer (CRC) is one of the leading causes
of cancer mortalities worldwide, and is the third most common
cancer type and the fifth leading cause of mortality in China
(1–3). The majority of CRCs develop
sporadically (70–80%), and the somatic loss of tumor suppressor
gene, adenomatous polyposis coli (APC), was revealed to be
present in 85% of patients with CRC and familial adenomatous
polyposis (4–6). It has previously been demonstrated to
have significant pro-apoptosis and anti-proliferative effects in
several different types of cancers in vivo and in
vitro (1–3). Recently, Riccardin D, a novel
macrocyclicbis (bibenzyl) compound isolated from the Chinese
liverwort plant Dumortiera hirsuta, has been observed to
prevent the growth of intestinal polyps in adenomatous polyposis
coli (APC)Min/+ mice, an animal model of human
familial adenomatous polyposis, which spontaneously develops
numerous polyps in the intestinal tract due to a mutation in the
APC gene (6). This indicates that
Riccardin D may serve an important role in the inhibition of
CRC.
APC serves a critical role in regulating gene
transcription through the Wnt signaling pathway (7). The APC gene mutation is the
most common cause of colon cancer associated with the Wnt/β-catenin
signaling pathway, which serves a critical role in the development
of colon cancer (6–8). By contrast, the nuclear factor
(NF)-κB-cyclooxygenase (COX)-2 signaling pathway has also been
shown to affect the APC gene mutation in the human intestine
and colon cells (9,10). In the APCMin/+
mouse, a higher expression of inflammation-associated cytokines has
been reported (11,12). These results have suggested that
there may be a connection between inflammation and tumor
development. Our previous report also demonstrated that Riccardin D
downregulated inflammatory factors, particularly those associated
with the NF-κB signaling pathway, in the mouse model (6). NF-κB is hypothesized to promote
tumorigenesis via pro-inflammatory transcription factors, which can
be activated by bacterial products, such as lipopolysaccharides
(LPS), and inflammatory cytokines. The transcriptional targets of
NF-κB include genes encoding COX-2, intercellular adhesion
molecule-1, vascular endothelial growth factor, and the
inflammatory cytokines, interleukin (IL)-1β and tumor necrosis
factor α (TNFα) (13,14).
Previous reports have indicated that regular use of
nonsteroidal anti-inflammatory drugs lowers the mortality
associated with sporadic colon cancer and results in the regression
of adenomas in patients with familial adenomatous polyposis, who
have inherited a mutation in the APC gene (15,16).
Pro-inflammatory cytokines, including TNFα, IL-6 and IL-1β, or
transcription factors that are required by these cytokines for
signaling, such as NF-κB and signal transducer and activator of
transcription, have been identified as potential targets for
anticancer therapy (17). In the
present study, the mechanism underlying the anti-inflammation
effects of Riccardin D in vitro were investigated. The
results indicated that Riccardin D may exert its modulatory effects
by blocking NF-κB activity in colon cancer cells. To the best of
our knowledge, these results show, for the first time, the
evaluation of macrocyclicbis (bibenzyls) against CRC associated
with the inflammation pathway, suggesting its potential in the
therapeutic intervention of intestinal cancers as a novel NF-κB
inhibitor.
Materials and methods
Drugs
Riccardin D, a novel macrocyclicbis (bibenzyl)
compound, was extracted from the Chinese liverwort plant
Dumortiera hirsuta (previously collected from the Guizhou
region, China), and its structure was identified as reported
previously (18). The purity of
Riccardin D, as measured by high performance liquid chromatography
(18), was 98.6%. The compound was
dissolved in dimethyl sulfoxide (DMSO; Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany) at 20 mM as stock solution for the in
vitro study (18).
Cell lines and cell culture
The human colon cancer cell line HT-29 with a mutant
APC gene, expressed as two C-terminal-truncated APC proteins of 100
and 200 kDa, was purchased from American Type Cell Culture
Collection (Manassas, VA, USA) (12). The HCT-8 cell line expressing
normal APC proteins was also obtained from American Type Cell
Culture Collection. Cancer cells were grown in Dulbecco's modified
Eagle's medium supplemented with 10% (v/v) heat-inactivated fetal
bovine serum (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA,
USA), penicillin (100 IU/ml), streptomycin (100 µg/ml) and 10 mM
HEPES buffer at 37°C in a humid atmosphere (5% CO2, 95%
air).
Cell Counting kit (CCK)-8 assay
HCT-8 and HT-29 cells were seeded in 96-well plates
(5×103 cells/well) and incubated with increasing
concentrations (2.5, 5, 10, 20, 40 and 60 µM) of Riccardin D for
24, 48 and 72 h at 37°C, respectively. The control cells were
treated with an equal volume of the drug's vehicle DMSO. The cell
viability was then detected using a CCK-8 kit (Dojindo Molecular
Technologies, Inc., Kumamoto, Japan).
Hoechst 33258 staining
HT-29 cells were seeded in 6-well plates
(3×105 cells/well) and treated with 0, 5, 10 and 20 µM
of Riccardin D for 24 h at 37°C; whereas control cells were treated
with DMSO only. Cells were then fixed with 4% formaldehyde in
phosphate-buffered saline (PBS) for 10 min, stained with Hoechst
33258 (10 mg/l) for 1 h at 37°C, and then subjected to fluorescence
microscopy (Nikon TE2000; Nikon Corporation, Tokyo, Japan). These
data were obtained by eye via counting the number of apoptotic
cells in five different fields of view for each group.
Mitochondrial membrane permeability
assay
The mitochondria membrane potential (MMP) was
investigated using JC-1 dye (Beyotime Institute of Biotechnology,
Shanghai, China) according to the manufacturer's protocol. The
ratio of green to red fluorescence provides an estimate of the
changes in MMP. Briefly, HT-29 cells seeded in 6-well plates
(3×105 cells/well) were exposed to 0, 5, 10 and 20 µM
Riccardin D for 24 h at 37°C; whereas control cells were treated
with DMSO only. Cells were then incubated with an equal volume of
JC-1 staining solution (5 µg/ml) at 37°C for 20 min and rinsed
twice with PBS. MMPs were monitored by determining the relative
quantity of dual emissions from mitochondrial JC-1 monomers or
aggregates using an Olympus fluorescent microscope under Argon-ion
488 nm laser excitation. Mitochondrial depolarization is indicated
by an increase in the green/red fluorescence intensity ratio.
Experiments were performed at least three times.
Western blotting analysis
Western blotting analysis was employed to evaluate
the protein expression associated with tumor growth in human colon
cancer cells. HT-29 cells (3×105 cells/well) cultured in
6-well plates were incubated with 20 µM of Riccardin D for 48 h at
37°C. The cells were collected and washed thrice using PBS
(Beyotime Institute of Biotechnology) to produce lysates using
radioimmunoprecipitation assay lysis buffer (Beyotime Institute of
Biotechnology), and concentrations of proteins were determined
using a bicinchoninic acid assay kit purchased from Beyotime
Institute of Biotechnology. Protein samples (30 µg/lane) were
separated by 10% SDS-PAGE and then transferred to polyvinylidene
fluoride (PVDF) membranes. Non-specific binding was blocked via
incubation with 5% non-fat milk for 2 h at room temperature, and
membranes were then incubated for 1 h at room temperature using the
following primary antibodies: Anti-NF-κB (1:800; cat. no. sc-8008;
Santa Cruz Biotechnology, Inc., Dallas, TX, USA), anti-phosho
(p)-NF-κB Ser536 (1:800; cat. no. sc-33020; Santa Cruz
Biotechnology, Inc.), anti-caspase-3 (1:1,000; cat. no. 9662; Cell
Signaling Technology, Inc., Danvers, MA, USA), anti-caspase-9
(1:1,000; cat. no. 9502; Cell Signaling Technology, Inc.),
anti-cleaved poly(adenosine diphosphate-ribose) polymerase (PARP;
1:1,000; cat. no. 9541; Cell Signaling Technology, Inc.),
anti-B-cell lymphoma (Bcl)-2 (1:1,000; cat. no. 2872; Cell
Signaling Technology, Inc.), anti-Bcl-2-associated X protein
(1:1,000; Bax; cat. no. 2772; Cell Signaling Technology, Inc.),
TNFα (1:1,000; cat. no. 6945; Cell Signaling Technology, Inc.) and
anti-β-actin (1:5,000; cat. no. ab6276; Abcam, Cambridge, MA, USA).
The PVDF membranes were then washed with TBS containing 0.05%
Tween-20 prior to incubation with horseradish peroxidase-conjugated
secondary antibodies (1:1,000; cat. nos. ZDR-5306 and ZDR-5307;
OriGene Technologies, Inc., Beijing, China) at room temperature for
1 h. The bound antibodies were detected using an enhanced
chemiluminescence reagent (EMD Millipore, Billerica, MA, USA).
Densitometry analysis was performed using an electrophoresis image
analysis system (cat. no. FR980; Shanghai FuriScience &
Technology Co., Ltd., Shanghai, China). Experiments were performed
at least three times.
Reverse
transcription-semi-quantitative polymerase chain reaction
(RT-sqPCR)
A RT-sqPCR assay was performed to analyze the
expression of COX-2 in colon cancer cells. HT-29 cells
(3×105 cells/well) cultured in 6-well plates were
administrated 0, 10 and 20 µM Riccardin D for 24 h at 37°C. Total
RNA was extracted using an RNAeasy kit (Sangon Biotech Co., Ltd.,
Shanghai, China) according to the manufacturer's instructions. cDNA
was synthesized from RNA using the First Strand cDNA Synthesis kit
(Toyobo Life Science, Osaka, Japan). The following primers (Gene
Core Biotech Co., Ltd., Shanghai, China) were used for
amplification: COX-2 forward, 5′-TTCAAATGAGATTGTGGGAAAATTGCT-3′ and
reverse, 5′-AGATCATCTCTGCCTGAGTATCTT-3′; and β-actin forward,
5′-GGGTCAGAAGGATTCCTATG-3′ and reverse, 5′-GGTCTCAAACATGATCTGGG-3′.
The reverse transcription reaction was performed at 37°C for 15 min
and 98°C for 5 min; and PCR was performed for 40 cycles at 92°C for
30 sec, 56°C for 30 sec and 68°C for 1 min. PCR products were run
on 2% agarose gels containing 0.51 g/ml of ethidium bromide and
then photographed using an ultraviolet transilluminator (cat. no.
FR980; Shanghai FuriScience & Technology Co., Ltd.). β-actin
was used as the internal control and experiments were performed at
least three times. Alpha Ease FC software was used to analyze
relative light intensities (version 4.0.0.34; Protein Simple, San
Jose, CA, USA).
Luciferase reporter gene assay
The effect of Riccardin D on NF-κB-dependent
reporter gene transcription induced by LPS was analyzed by
NF-κB-luciferase assay using a Firefly Luciferase Reporter Gene
Assay kit (Beyotime Institute of Biotechnology). Briefly, HT-29
cells (3×105 cells/well) were plated in 6-well plates
and transiently transfected using Lipofectamine® 2000
(Thermo Fisher Scientific, Inc.) method with the pNF-κB-luc plasmid
reporter gene (1 µg; Beyotime Institute of Biotechnology)
containing four NF-κB binding motifs (5′-GGGAATTTCC-3′) and
β-galactosidase (90 ng; BioVector NTCC Inc., Beijing, China).
Following 24 h post-transfection, cells were treated with Riccardin
D and 10 µg/ml LPS for a further 20 h. Cells were then harvested in
order to measure β-galactosidase and luciferase activity. Relative
luciferase activity was normalized to the value of β-galactosidase
to correct the transfection efficacy (β-galactosidase Assay kit;
Beyotime Institute of Biotechnology). Triplicate experiments with
triplicate samples were performed.
Molecular modeling analysis
Auto Dock Vina (version 4.0; Molecular Graphics
Laboratory, The Scripps Research Institute, La Jolla, CA, USA) has
previously been demonstrated to locate docking modes that are
consistent with X-ray crystal structures (19). Auto Dock simulates interactions
between substrates or drug candidates as ligands, and their
macromolecular receptors with known three dimensional structures,
allowing ligand flexibility described to a full extent. In order to
investigate the binding mode of Riccardin D, a molecular model of
Riccardin D docked into NF-κB was produced using SYBYL-X Suite by
Certara USA, Inc. (Princeton, NJ, USA). The X-ray crystal structure
of NF-κB was taken from the Protein Data Bank (1K3Z) and was used
for docking studies. Computer software was used in the present
study to mimic the structure of Riccardin D and NF-κB, in order to
identify the main binding sites between Riccardin D and NF-κB
through docking simulation. The default parameters as described in
the Sybyl manual were used.
Statistical analysis
Statistical analysis was performed using PASW
Statistics Windows 18 download (version 15.0; SPSS, Inc., Chicago,
IL, USA). Data were presented as the mean ± standard deviation and
were analyzed by Student's t-test or one-way analysis of variance
followed by a Student-Newman-Keuls post hoc test for multiple
comparisons. P<0.05 was considered to indicate a statistically
significant difference. Triplicate experiments were performed using
triplicate samples.
Results
Inhibition of colon cancer cell growth
by Riccardin D
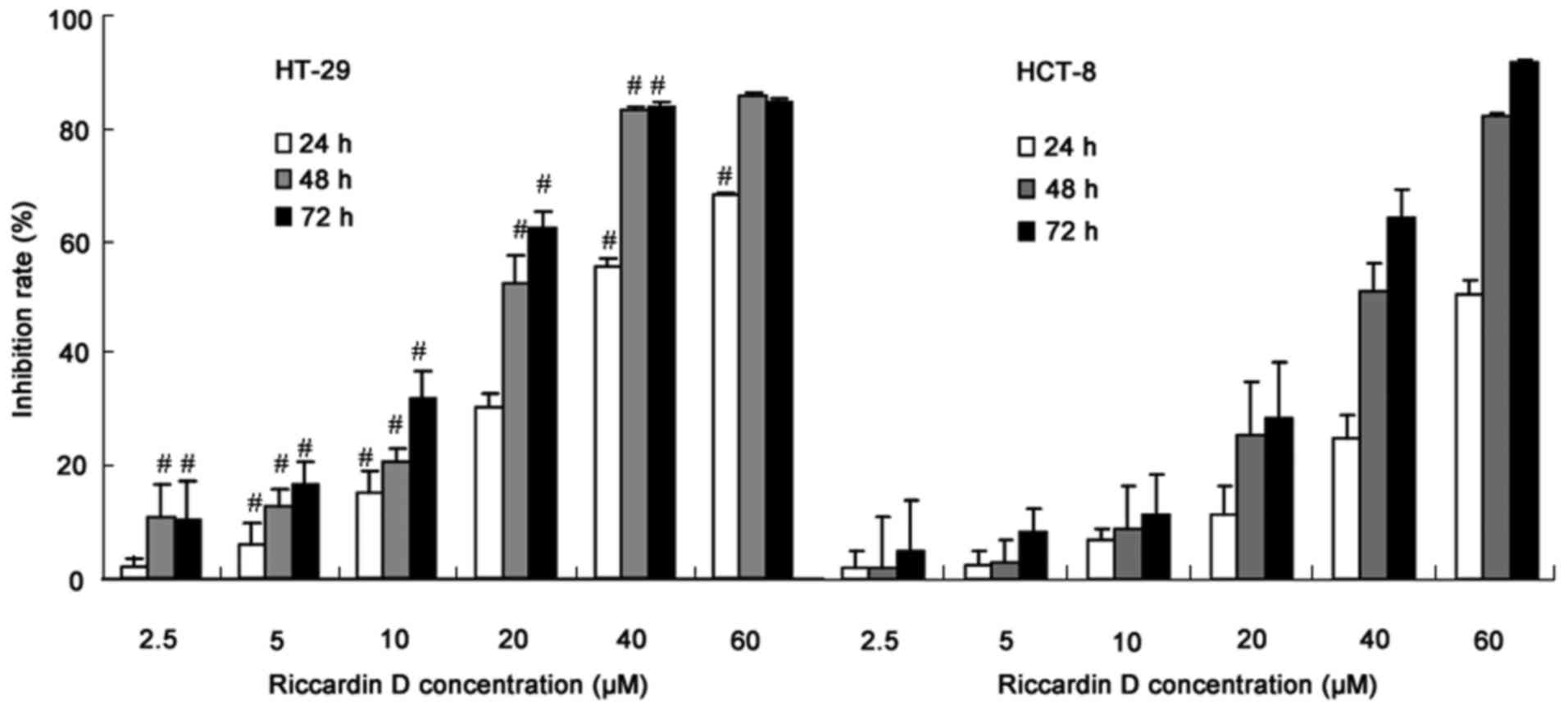
Human colon cancer HT-29 and HCT-8 cells were
exposed to Riccardin D for 24, 48 and 72 h, and were then subjected
to a proliferation assay. The inhibition rate (%) was calculated as
(OD450 value of control group-OD450 value of
drug treated group)/OD450 value of control group ×100.
As shown in Fig. 1, Riccardin D,
in a concentration range of 2.5–40 µM, inhibited HT-29 and HCT-8
cell growth in a dose-dependent manner. Notably, the
anti-proliferation effects of Riccardin D on human colon cancer
cells was more significant in HT-29 cells with the APC mutation
(HT-29 vs. HCT-8: at 2.5 µM for 24 h, and at 60 µM for 48 and 72 h;
P>0.05). These experiments also indirectly revealed the
chemopreventative effects of Riccardin D on intestinal adenoma
formation in APCMin/+ mice; thus, the subsequent
experiments were carried out using HT-29 cells only.
Riccardin D induces HT-29 cell
apoptosis
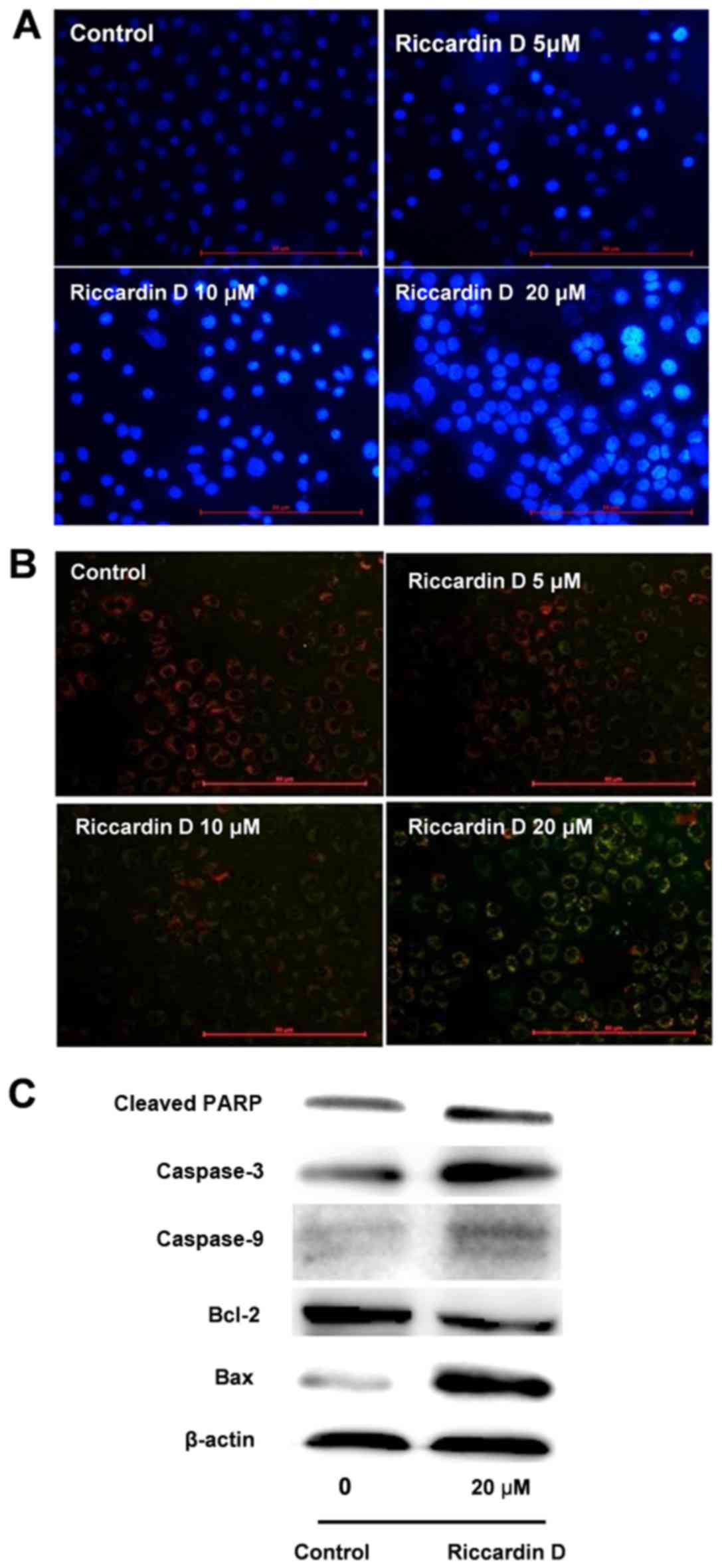
The induction of apoptosis was detected to evaluate
the inhibitory effect of Riccardin D via a number of different
assays. As indicated by Hochest 33258 analysis in Fig. 2A, the number of apoptotic cells
increased following 24 h incubation with 20 µM of Riccardin D.
Treatment with Riccardin D, also revealed morphological changes
using Hochest 33258 staining, including decreased cell size and
nuclear chromatin condensation.
The JC-1 fluorescence probe demonstrated that the
MMP in HT-29 cells was markedly reduced following treatment with
Riccardin D. As shown in Fig. 2B,
the red fluorescence of JC-1 gradually decreased and the green
fluorescence was correspondingly increased following Riccardin D
administration. In the range of 5–20 µM, the ratio of green to red
fluorescence increased in a dose-dependent manner. The results
revealed that treatment with Riccardin D in HT-29 cells reduced the
MMP.
Further studies of the apoptotic proteins in HT-29
cells were also undertaken. Riccardin D treatment activated the
caspase cascade pathway, in agreement with in vivo data from
our previous research in the APCMin/+ mouse (6). As shown in Fig. 2C, the levels of cleaved caspase-3,
caspase-9 and PARP were markedly increased in Riccardin D treated
cells. Riccardin D also increased the Bax:Bcl-2 ratio, as the
protein level of Bax was markedly increased, which was accompanied
by a notable decrease in Bcl-2 in HT-29 cells treated with 20 µM
Riccardin D.
Suppression of inflammation via a
decrease in COX-2 and NF-κB expression
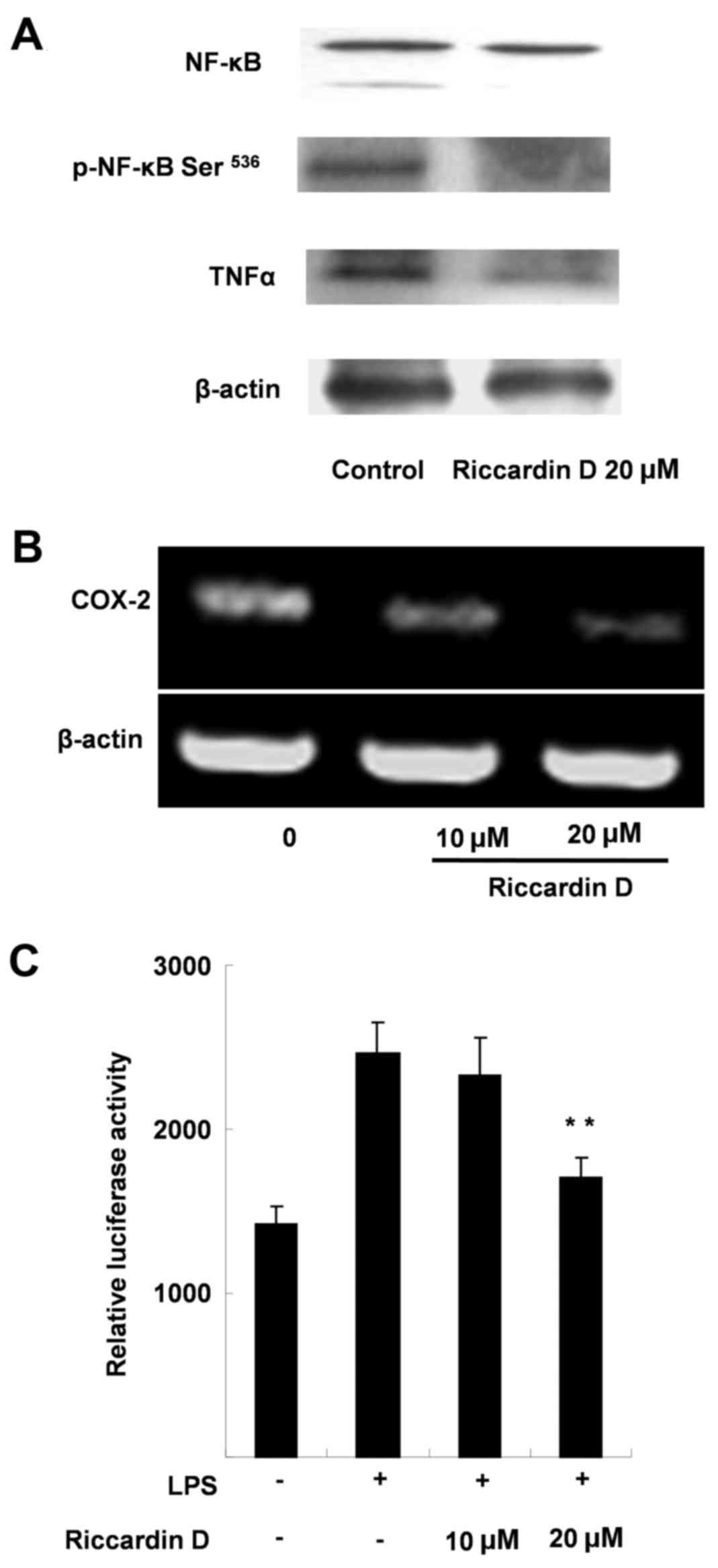
The results revealed that Riccardin D decreased the
protein expression of NF-κB. Fig.
3A indicated that the level of total NF-κB p65 protein in HT-29
cells was markedly decreased by 53.4% (P<0.01) when compared
with control. Further analysis of p-NF-κB Ser536
demonstrated that the active form of NF-κB, was markedly decreased
by 47.2% (P<0.01; Fig. 3A)
compared with the control.
The inhibitory effect of Riccardin D on COX-2 cDNA
expression was also shown in HT-29 cells by RT-PCR analysis. As
shown in Fig. 3B, following 24 h
exposure with 10 and 20 µM Riccardin D, the levels of COX-2 mRNA
were decreased by 35.0 and 66.7%, respectively (Fig. 3B). These results suggested that
Riccardin D treatment reduced COX-2 expression at the DNA
level.
To further substantiate the finding that Riccardin D
may target NF-κB, the present study also investigated the effects
of Riccardin D on NF-κB-mediated transcriptional activity using
HT-29 cells, wherein 20 µM of Riccardin D reduced luciferase
activity by 45.2% (P<0.01) compared with control cells, which
were treated with LPS and 0 µM Riccardin D (Fig. 3C). These results provided
additional insight into the suppression of intestinal tumorigenesis
by Riccardin D.
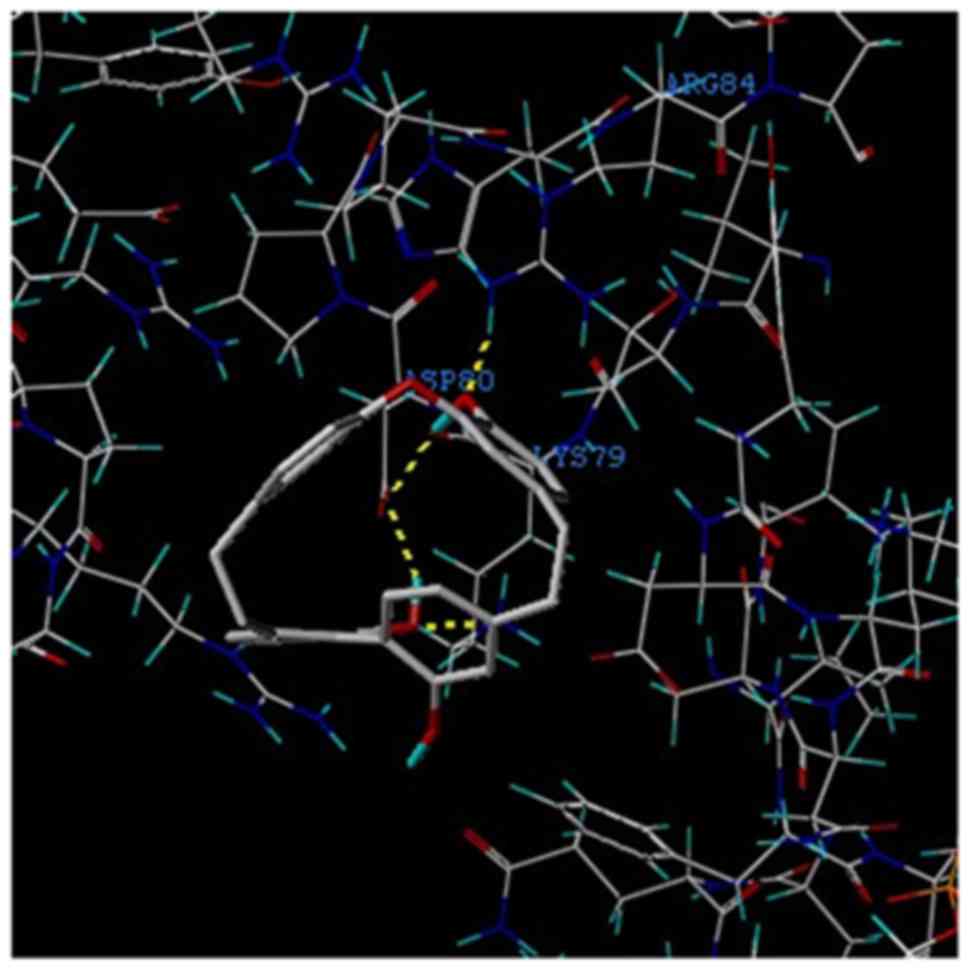
In addition, the theoretical binding mode of
Riccardin D to NF-κB-p65 is presented in Fig. 4. Two binding sites were identified
between Riccardin D and NF-κB-p65 protein.
Discussion
Patients with chronic inflammatory bowel disease are
more susceptible to developing CRC, and a number of studies have
indicated that chronic inflammation may affect intestinal
tumorigenesis (20–22). It is also believed that aberrant
Wnt/β-catenin signaling following the loss of APC function may
initiate colon adenoma formation (21,23).
The APC gene mutation mouse model
(APCMin/+) has been considered to be the standard
experimental model for research into intestinal carcinogenesis as
tumors grow spontaneously in the intestinal tract (4). Our previous study demonstrated that
the administration of Riccardin D caused the inhibition of polyps
in the intestine of APCMin/+ mice through its
anti-proliferative, apoptotic and anti-inflammatory effects
(6). Therefore, the present study
investigated the anti-cancer effects of Riccardin D using human
colon cancer cell lines in vitro and aimed to further
understand the underlying mechanisms involved in the NF-κB
signaling pathway in HT-29 cells with the APC mutation. The
results revealed that Riccardin D markedly inhibited the
proliferation of the human colon cancer cell line HT-29 with a
mutant car boxy-truncated APC gene.
The NF-κB transcription factor pathway is a crucial
regulator of a number of normal cellular functions. Under
physiological conditions, NF-κB may coordinate the transcription of
cytokines including COX-2 (24),
cyclin D1 (25) and numerous other
factors (26). The constitutive
activation of NF-κB contributes to multiple cellular outcomes and
pathophysiological conditions, including rheumatoid arthritis,
asthma, inflammatory bowel disease, acquired immunodeficiency
syndrome and cancer, through interactions with multiple pathways
including the cell cycle, apoptosis and proliferation (27,28).
Aberrant NF-κB signaling has been identified in a number of
different types of cancer; NF-κB regulates the transcription of
target genes that promote cell survival and proliferation, inhibit
apoptosis, and mediate invasion and metastasis (29). Loss of APC function can lead to the
activation of β-catenin signaling, which is the first step in the
oncogenic pathway leading to CRC development (30). It has been reported that TNF
receptor superfamily member 19 (TNFRSF19) is a β-catenin target
gene and TNFRSF19 receptor molecule-associated activation of NF-κB
signaling has demonstrated that β-catenin may regulate NF-κB
activity via TNFRSF19; activation of NF-κB activity has also been
observed in the APCMin+ mice model, which was inhibited
by Riccardin D as shown in our previous study (4). NF-κB inhibition is also considered to
be an important therapeutic target in CRC (14,31).
Thus, it may be hypothesized that the inhibition of NF-κB by
Riccardin D maybe a pivotal mechanism of its effects in
chemotherapy for CRC with the APC mutation. The present
study then detected the expression and activity of NF-κB, revealing
that Riccardin D markedly reduced NF-κB protein expression in HT-29
cells; the active form of NF-κB, p-NF-κBSer536, was also
markedly suppressed.
The NF-κB signaling pathway is a complex network
that regulates cellular pathways involved in a myriad of
physiological and pathological conditions. In addition, the
accumulation of nuclear NF-κB increases the aberrant activation of
the COX-2 gene (14). In the
present study, Riccardin D inhibited the expression of NF-κB, COX-2
and TNFα, as well as the transcriptional activity of NF-κB induced
by LPS. Riccardin D may also be directly associated with the
transcriptional activity of NF-κB. One potential mode of this
action is that Riccardin D may serve as a NF-κB activation
suppressor, which is supported by Auto Dock molecular analysis;
however, further confirmation via X-ray crystal structure analysis
is required.
It is also believed that the NF-κB signaling pathway
may be a critical regulator of apoptosis, as NF-κB can block
apoptosis by regulating anti-apoptosis proteins, and apoptotic
signals can be activated following NF-κB inhibition during the
cancer treatment (32,33). Suppression of NF-κB is also thought
to limit the proliferation of cancer cells (34). NF-κB regulates a number of
anti-apoptotic genes, particularly the TNF receptor-associated
factors (TRAFs), TRAF1 and TRAF2 (35,36).
The present study revealed that Riccardin D induced HT-29 cell
apoptosis as indicated by the reduction in MMP, the activation of
cleaved caspase-3, caspase-9 and PARP, and the increase in the
Bax/Bcl-2 ratio of Riccardin D-treated cells; this indicated that
the intrinsic pathway may have been triggered by Riccardin D
treatment. Therefore, these results suggested that Riccardin D,
following NF-κB inhibition, may induce colon cell apoptosis by
modulating the mitochondria-mediated intrinsic apoptosis signaling
pathway.
The results of the present study demonstrated that
Riccardin D inhibits cell proliferation and induces apoptosis in
HT-29 cells, which may be associated with inhibiting the NF-κB
signaling pathway. Previous studies have revealed that Riccardin D
inhibits breast cancer growth through the suppression of telomerase
(37). However, some telomeric
proteins, such as Ras-related protein RAP1, have been shown to
serve a role as a modulator of the NF-κB-mediated signaling pathway
(38). Therefore, Riccardin D may
have inhibitory effects on the NF-κB pathway through the
suppression of telomerase. However, the underlying mechanisms
require further investigation.
In conclusion, the results of the present study
indicated that human colon cancer cell death induced by Riccardin D
may be associated with the inhibition of NF-κB signaling and that
Riccardin D may be a novel NF-κB inhibitor, inhibiting colon cancer
cell proliferation and inducing cell apoptosis. The critical role
of regulating the NF-κB signaling pathway in apoptosis, tumor
promotion and tumor maintenance, suggests that Riccardin D maybe a
promising candidate in cancer therapy. Further studies
investigating the mechanism of Riccardin D and its therapeutic
effects on clinical tumors are still required. However, based on
these results, Riccardin D may be an effective NF-κB inhibitor in
cancer therapy.
Acknowledgements
The authors are grateful to the staff at the Central
Research Laboratory, the Second Hospital of Shandong University
(Shandong, China) for their technical assistance and support.
Funding
The present study was supported by the Natural
Science Foundation of China (grant no. 81402962).
Availability of data and materials
All of the materials used in the present study are
commercially available and all data included in the present study
were obtained by the co-authors.
Authors' contributions
HL, DS, BZ, FK and RW designed the study. HL, XX, JW
and FC performed the experiments. HL, GL, XX, YL and WJ analyzed
the data. HL, GL and XX wrote the manuscript.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wu Y, Yang L, Zhao J, Li C, Nie J, Liu F,
Zhuo C, Zheng Y, Li B, Wang Z and Xu Y: Nuclear-enriched abundant
transcript 1 as a diagnostic and prognostic biomarker in colorectal
cancer. Mol Cancer. 14:1912015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen W, Zheng R, Zhang S, Zhao P, Li G, Wu
L and He J: Report of incidence and mortality in China cancer
registries, 2009. Chin J Cancer Res. 25:10–21. 2013.PubMed/NCBI
|
|
3
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nishisho I, Nakamura Y, Miyoshi Y, Miki Y,
Ando H, Horii A, Koyama K, Utsunomiya J, Baba S and Hedge P:
Mutations of chromosome 5q21 genes in FAP and colorectal cancer
patients. Science. 253:665–669. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Binefa G, Rodríguez-Moranta F, Teule A and
Medina-Hayas M: Colorectal cancer: From prevention to personalized
medicine. World J Gastroenterol. 20:6786–6808. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu HP, Gao ZH, Cui SX, Sun DF, Wang Y,
Zhao CR, Lou HX and Qu XJ: Inhibition of intestinal adenoma
formation in APC mice by riccardin d, a natural product derived
from liverwort plant Dumortiera hirsuta. PLoS One. 7:e332432012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chiurillo MA: Role of the Wnt/β-catenin
pathway in gastric cancer: An in-depth literature review. World J
Exp Med. 5:84–102. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Larriba MJ, Ordóñez-Morán P, Chicote I,
Martín-Fernández G, Puig I, Muñoz A and Pálmer HG: Vitamin D
receptor deficiency enhances Wnt/β-catenin signaling and tumor
burden in colon cancer. PLoS One. 6:e235242011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Carothers AM, Davids JS, Damas BC and
Bertagnolli MM: Persistent cyclooxygenase-2 inhibition
downregulates NF-{kappa}B, resulting in chronic intestinal
inflammation in the min/+ mouse model of colon
tumorigenesis. Cancer Res. 70:4433–4442. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McClellan JL, Davis JM, Steiner JL, Day
SD, Steck SE, Carmichael MD and Murphy EA: Intestinal inflammatory
cytokine response in relation to tumorigenesis in the Apc (Min/+)
mouse. Cytokine. 57:113–119. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Murphy EA, Davis JM, McClellan JL, Gordon
BT and Carmichael MD: Curcumin's effect on intestinal inflammation
and tumorigenesis in the ApcMin/+ mouse. J Interferon Cytokine Res.
31:219–226. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Coghill AE, Newcomb PA, Campbell PT,
Burnett-Hartman AN, Adams SV, Poole EM, Potter JD and Ulrich CM:
Prediagnostic non-steroidal anti-inflammatory drug use and survival
after diagnosis of colorectal cancer. Gut. 60:491–498. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Robbins D and Zhao Y: Imaging NF-κB
signaling in mice for screening anticancer drugs. Methods Mol Biol.
716:169–177. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang S, Liu Z, Wang L and Zhang X:
NF-kappaB signaling pathway, inflammation and colorectal cancer.
Cell Mol Immunol. 6:327–334. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Qiu W, Wang X, Leibowitz B, Liu H, Barker
N, Okada H, Oue N, Yasui W, Clevers H and Schoen RE:
Chemoprevention by nonsteroidal anti-inflammatory drugs eliminates
oncogenic intestinal stem cells via SMAC-dependent apoptosis. Proc
Natl Acad Sci USA. 107:pp. 20027–20032. 2010; View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hansen-Petrik MB, McEntee MF, Jull B, Shi
H, Zemel MB and Whelan J: Prostaglandin E(2) protects intestinal
tumors from nonsteroidal anti-inflammatory drug-induced regression
in Apc(Min/+) mice. Cancer Res. 62:403–408. 2002.PubMed/NCBI
|
|
17
|
Klampfer L: Cytokines, inflammation and
colon cancer. Curr Cancer Drug Targets. 11:451–464. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lu ZQ, Fan PH, Ji M and Lou HX: Terpenoids
and bisbibenzyls from Chinese liverworts conocephalum conicum and
Dumortiera hirsute. J Asian Nat Prod Res. 8:187–192. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rosenfeld RJ, Goodsell DS, Musah RA,
Morris GM, Goodin DB and Olson AJ: Automated docking of ligands to
an artificial active site: Augmenting crystallographic analysis
with computer modeling. J Comput Aided Mol Des. 17:525–536. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mariani F, Sena P and Roncucci L:
Inflammatory pathways in the early steps of colorectal cancer
development. World J Gastroenterol. 20:9716–9731. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Samowitz WS, Slattery ML, Sweeney C,
Herrick J, Wolff RK and Albertsen H: APC mutations and other
genetic and epigenetic changes in colon cancer. Mol Cancer Res.
5:165–170. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Abdullah M, Rani AA, Sudoyo AW, Makmun D,
Handjari DR and Hernowo BS: Expression of NF-kB and COX2 in
colorectal cancer among native Indonesians: The role of
inflammation in colorectal carcinogenesis. Acta Med Indones.
45:187–192. 2013.PubMed/NCBI
|
|
23
|
Phelps RA, Broadbent TJ, Stafforini DM and
Jones DA: New perspectives on APC control of cell fate and
proliferation in colorectal cancer. Cell Cycle. 8:2549–2556. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yamamoto K, Arakawa T, Ueda N and Yamamoto
S: Transcriptional roles of nuclear factor kappa B and nuclear
factor-interleukin-6 in the tumor necrosis factor alpha-dependent
induction of cyclooxygenase-2 in MC3T3-E1 cells. J Biol Chem.
270:31315–31320. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hinz M, Krappmann D, Eichten A, Heder A,
Scheidereit C and Strauss M: NF-kappaB function in growth control:
Regulation of cyclin D1 expression and G0/G1-to-S-phase transition.
Mol Cell Biol. 19:2690–2698. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Esteve PO, Chicoine E, Robledo O, Aoudjit
F, Descoteaux A, Potworowski EF and St-Pierre Y: Protein kinase
C-zeta regulates transcription of the matrix metalloproteinase-9
gene induced by IL-1 and TNF-alpha in glioma cells via NF-kappa B.
J Biol Chem. 277:35150–35155. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vaiopoulos AG, Athanasoula KCh and
Papavassiliou AG: NF-κB in colorectal cancer. J Mol Med (Berl).
91:1029–1037. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sakamoto K, Maeda S, Hikiba Y, Nakagawa H,
Hayakawa Y, Shibata W, Yanai A, Ogura K and Omata M: Constitutive
NF-kappaB activation in colorectal carcinoma plays a key role in
angiogenesis, promoting tumor growth. Clin Cancer Res.
15:2248–2258. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Morin PJ, Sparks AB, Korinek V, Barker N,
Clevers H, Vogelstein B and Kinzler KW: Activation of
beta-catenin-Tcf signaling in colon cancer by mutations in
beta-catenin or APC. Science. 275:1787–1790. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shaked H, Hofseth LJ, Chumanevich A,
Chumanevich AA, Wang J, Wang Y, Taniguchi K, Guma M, Shenouda S,
Clevers H, et al: Chronic epithelial NF-κB activation accelerates
APC loss and intestinal tumor initiation through iNOS
up-regulation. Proc Natl Acad Sci. 109:pp. 14007–14012. 2012;
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Temraz S, Mukherji D and Shamseddine A:
Potential targets for colorectal cancer prevention. Int J Mol Sci.
14:17279–17303. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kucharczak J, Simmons MJ, Fan Y and
Gelinas C: To be, or not to be: NF-κB is the answer-role of
Rel/NF-κB in the regulation of apoptosis. Oncogene. 22:8961–8982.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yamamoto Y and Gaynor RB: Therapeutic
potential of inhibition of the NF-kappaB pathway in the treatment
of inflammation and cancer. J Clin Invest. 107:135–142. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kim SM, Lee SY, Yuk DY, Moon DC, Choi SS,
Kim Y, Han SB, Oh KW and Hong JT: Inhibition of NF-kappaB by
ginsenoside Rg3 enhances the susceptibility of colon cancer cells
to docetaxel. Arch Pharm Res. 32:755–765. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Takada Y, Kobayashi Y and Aggarwal BB:
Evodiamine abolishes constitutive and inducible NF-kappaB
activation by inhibiting IkappaBalpha kinase activation, there by
suppressing NF-kappaB-regulated antiapoptoticand metastatic gene
expression, up-regulating apoptosis and inhibiting invasion. J Biol
Chem. 280:17203–17212. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Elbaz M, Yanay N, Laban S, Rabie M,
Mitrani-Rosenbaum S and Nevo Y: Life or death by NF-κB, Losartan
promotes survival in dy2J/dy2J mouse of MDC1A. Cell Death Dis.
6:e16902015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sun CC, Xu HM, Yuan Y, Gao ZH, Lou HX and
Qu XJ: Riccardin D, a macrocyclicbisbibenzy, inhibits human breast
cancer growth through the suppression of telomerase activity. Basic
Clin Pharmacol Toxicol. 115:488–498. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Teo H, Ghosh S, Luesch H, Ghosh A, Wong
ET, Malik N, Orth A, de Jesus P, Perry AS, Oliver JD, et al:
Telomere-independent Rap1 is an IKK adaptor and regulates
NF-kappaB-dependent gene expression. Nat Cell Biol. 12:758–767.
2010. View Article : Google Scholar : PubMed/NCBI
|