Introduction
Although there is a general declining trend in the
incidence of peptic ulcers, the disease remains common.
Approximately 500,000 people develop peptic ulcers per year in the
USA (1). They are mainly caused by
infection of Helicobacter pylori, gastric acid, nonsteroidal
anti-inflammatory drugs (NSAIDs) and protective factors (2). Peptic ulcers are diagnosed by endoscopy
and can be treated with proton pump inhibitors, H. pylori
therapy (according to the results of H. pylori testing),
endoscopy or surgery according to the severity of the disease. At
the same time, non-variceal upper gastrointestinal (GI) bleeding
and other accompanying complications of peptic ulcers remain a
major prevalent and clinically significant condition worldwide
(3,4).
If affected patients neglect the warning symptoms (e.g. epigastric
discomfort, abdominal pain associated with eating, pain that causes
awakening at night, weight loss, loss of appetite and melena) and
receive no effective treatment for the peptic ulcer, then one or
more complications will develop. These complications will make the
disease much more complicated, and more difficult to diagnose and
treat. The present study reports the case of such a patient who was
diagnosed with peptic ulcers accompanied with upper GI bleeding,
pylorus obstruction and choledochoduodenal fistula (CDF), and was
successfully treated.
Case report
On December 12, 2010, a 67-year-old man was admitted
to The First Affiliated Hospital of Zhejiang University (Hangzhou,
Zhejiang, China) due to recurrent abdominal pain, fever and melena.
The patient had a 1-year history of recurrent upper abdominal pain
without any treatment, and no history of non-steroidal
anti-inflammatory drugs. At 3 months prior to the admission,
besides the abdominal pain, the patient experienced a fever, which
was controlled by antibiotic treatment, without any abdominal
distention or vomiting. At 1 month prior to admission, the patient
was admitted into a local hospital due to persistent melena.
However, the attempt to find the etiology and relieve the symptoms
was unsuccessful. The patient was subsequently admitted to The
First Affiliated Hospital of Zhejiang University for further
diagnosis and treatment.
The patient's abdomen was soft, with slight
tenderness in the upper region. The laboratory results showed
anemia (hemoglobin, 62 g/l; normal range, 120–160 g/l) and
hypoproteinemia (albumine 23 g/l; normal range, 35–55 g/l), with
total bilirubin (normal range, 0–21µmol/l), alanine
aminotransferase (normal range, 5–35 U/l) and aspartate
transaminase (normal range, 8–40 U/l) levels that were all within
the normal ranges. Anti-hemorrhagic (hemocoagulase atrox for
injection, 4 units/day, intravenous injection) and antibiotic
treatments (Cefodizime Sodium, 2 g/day, intravenously guttae) were
commenced. Abdominal ultrasound and magnetic resonance
cholangiopancreatography showed multiple low-echo occupations and a
stripe echo in the common bile duct, with dilatation of the
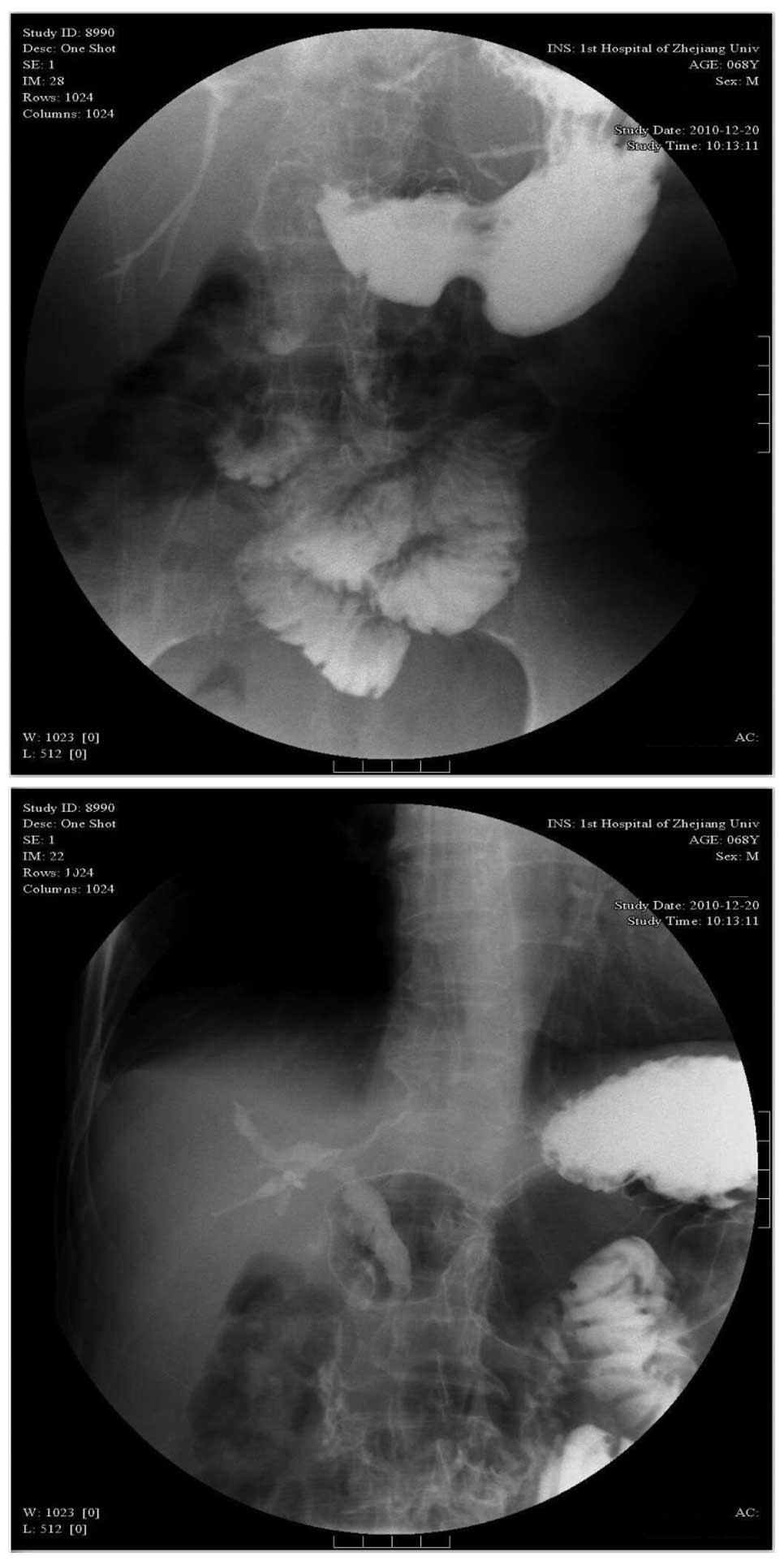
intrahepatic and extrahepatic bile ducts. Abdominal computed
tomography revealed stones in gallbladder and right liver with air
in dilated intrahepatic and extrahepatic bile duct (Fig. 1). Suspecting that the bleeding was
associated with the inflammation of the bile duct, endoscopic
retrograde cholangiopancreatography (ERCP) was performed to find
the position and the etiology of the bleeding. However, during the
examination, the scope could not be passed through the obstructed
section of deformed pylorus, and no significant abnormality of
tract was found above the pylorus. Therefore, gastroduodenography
was performed, which showed contrast medium entering into the bile
tract (Fig. 2). Accordingly, upper GI
bleeding and pyloric obstruction, with cholangitis secondary to a
CDF was considered. Following anti-hemorrhagic and antibiotic
treatments, the symptoms of fever and abdominal pain were
relieved.
However, the patient received emergency surgery due
to shock, which occurred 2 days later as a result of a massive
hemorrhage of the GI tract. The hemoglobin level decreased to 40
g/l. During the surgery, the bleeding was located to a branch of
the gastroduodenal artery, which was eroded by an ulcer (~1.0 cm in
diameter), in the pyloric canal. Furthermore, the scar of this
ulcer was also believed to be responsible for the pyloric
deformity. Additionally, another ulcer (~1.5 cm in diameter) was
found around the area of the duodenal papilla, which was suspected
to be the etiology for the disappearance of the papilla. No stones
were found in the gallbladder or common bile duct during the
procedure. So multiple surgeries, including a
pancreatoduodenectomy, a pancreaticojejunostomy, a
gastrojejunostomy and a choledochojejunostomy, were performed to
fulfill the following three objectives: i) Control of the
hemorrhage; ii) removal of the ulcers and the deformed pylorus; and
iii) repair of the CDF. Finally, the post-operative pathology
confirmed that the chronic ulcers in the pyloric canal and duodenum
were benign. Following the surgery, the patient responded well and
was discharged without any serious complications. The patient felt
no discomfort associated with the former diseases and gastroscope
found no ulcer recurrence during the following 3 years after the
surgery.
Discussion
Bleeding is the most frequent of the multiple
complications of peptic ulcers, occurring when an ulcer erodes a
blood vessel. Therefore, it must be managed promptly and
appropriately to prevent adverse outcomes. The guidelines for the
management of patients with non-variceal upper GI bleeding
recommend that endoscopy should generally be performed within 24 h
in order to diagnose, assess and treat the bleeding lesion
(3–5).
Even when endoscopic therapy fails, certain useful information can
be obtained for the subsequent transcatheter arterial embolization
(TAE) or surgery. Where available, percutaneous or TAE has been
investigated as an alternative to surgery in those individuals in
whom endoscopic therapy has failed, particularly those patients who
are high-risk candidates for surgery (4,6–9). A retrospective, single-center study
(6) demonstrated that there were no
significant differences between embolization therapy and surgery
with regard to the rates of rebleeding, surgery or mortality, even
though the patients in the embolization group were older with a
higher prevalence of heart disease. In other studies, TAE was
approved to associate with a high rate (93%) of technical success,
minimal complications (9%), a decreased surgery rate and overall
complications (6,10,11). The
indication for surgery is limited among cases where hemostasis
cannot be performed due to the position of the ulcer or the type of
bleeding. In the present patient, besides the GI bleeding, the
pyloric obstruction and CDF also had to be taken into account.
Therefore, endoscopic therapy and TAE were not suitable choices to
solve all these problems.
Pyloric and duodenal obstructions always develop in
patients with recurrent peptic ulcers as a result of acute
inflammation, spasm, edema, or scarring and fibrosis. The patients
suffer the associated symptoms of recurrent episodes of emesis,
persistent abdominal distention or fullness after eating, early
satiety and weight loss. Chronic peptic ulcer obstruction can be
relieved by endoscopic pyloric balloon dilatation or surgery
(vagotomy and pyloroplasty, antrectomy or gastroenterostomy)
(12). However, former experience in
our hospital showed that endoscopic balloon dilatation in pyloric
obstruction does not achieve long-term remission, and the majority
of patients require surgery.
CDF is a biliary abnormality that always occurs as a
consequence of long-lasting and poorly-treated chronic duodenal
ulcers (13,14). Patients with this abnormality are
believed to be prone to ascending biliary infection (15). The diagnosis of CDF is always
incidentally made by radiography, with the signs of air in the
biliary tree and barium reflux into the biliary tract following a
barium meal (16). Demonstration of
ostium discharging bile during ERCP is always regarded as the gold
standard for the diagnosis of CDF. Possible treatments for this
disease include conservative treatment with drugs, endoscopic
sphincterotomy and surgical therapy. The choice is based on the
etiology, the severity of the disease and the patient's general
condition. It has been reported that recurrent bile tract
infections and gallstone ileuses caused by CDF are considered as a
definitive indication for surgical management (17). Presently, biliary enteric anastomosis
is regarded as the primary method of treatment, with common bile
duct exploration, T-tube drainage and endoscopic sphincterotomy
also being effective (15,18).
To the best of our knowledge, peptic ulcers
accompanied with GI bleeding, pylorus obstruction and CDF have not
previously been reported. In the present case, considering the
coexisting complications of GI bleeding, pyloric obstruction and
CDF, simple surgical intervention was insufficient. Therefore, a
pancreatoduodenectomy was chosen for the purpose of simultaneously
treating the bleeding artery, reconstructing the GI tract and
resecting the CDF. The patient recovered well without any
complications or remaining symptoms. Since peptic ulcers are
extremely common, we hope this case will offer useful experience
with regard to the diagnosis and treatment strategy for peptic
ulcers that are accompanied by a group of complications.
Acknowledgements
The present study was supported by the Ministry of
Health of Special Fund Industry (grant no. 201002015). The authors
wish to thank all the doctors in the Division of Hepatobiliary and
Pancreatic Surgery, Department of Surgery in The First Affiliated
Hospital of Zhejiang University.
References
|
1
|
University of Michigan Health System.
Peptic ulcer disease. simplewww.cme.med.umich.edu/pdf/guideline/PUD05.pdfAccessed.
May 04–2007
|
|
2
|
Malfertheiner P, Chan FK and McColl KE:
Peptic ulcer disease. Lancet. 374:1449–1461. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sung JJ, Chan FK, Chen M, Ching JY, Ho KY,
Kachintorn U, Kim N, Lau JY, Menon J, Rani AA, et al: Asia-Pacific
Working Group: Asia-Pacific Working Group consensus on non-variceal
upper gastrointestinal bleeding. Gut. 60:1170–1177. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Barkun AN, Bardou M, Kuipers EJ, Sung J,
Hunt RH, Martel M and Sinclair P: International Consensus Upper
Gastrointestinal Bleeding Conference Group: International consensus
recommendations on the management of patients with nonvariceal
upper gastrointestinal bleeding. Ann Intern Med. 152:101–113. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Laursen SB, Jørgensen HS and de Muckadell
Schaffalitzky OB: Danish Society of Gastroenterology and
Hepatology: Management of bleeding gastroduodenal ulcers. Dan Med
J. 59:C44732012.PubMed/NCBI
|
|
6
|
Ripoll C, Bañares R, Beceiro I, Menchén P,
Catalina MV, Echenagusia A and Turegano F: Comparison of
transcatheter arterial embolization and surgery for treatment of
bleeding peptic ulcer after endoscopic treatment failure. J Vasc
Interv Radiol. 15:447–450. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Larssen L, Moger T, Bjørnbeth BA, Lygren I
and Kløw NE: Transcatheter arterial embolization in the management
of bleeding duodenal ulcers: A 5.5-year retrospective study of
treatment and outcome. Scand J Gastroenterol. 43:217–222. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Eriksson LG, Ljungdahl M, Sundbom M and
Nyman R: Transcatheter arterial embolization versus surgery in the
treatment of upper gastrointestinal bleeding after therapeutic
endoscopy failure. J Vasc Interv Radiol. 19:1413–1418. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Venclauskas L, Bratlie SO, Zachrisson K,
Maleckas A, Pundzius J and Jönson C: Is transcatheter arterial
embolization a safer alternative than surgery when endoscopic
therapy fails in bleeding duodenal ulcer? Scand J Gastroenterol.
45:299–304. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Loffroy R, Rao P, Ota S, De Lin M, Kwak BK
and Geschwind JF: Embolization of acute nonvariceal upper
gastrointestinal hemorrhage resistant to endoscopic treatment:
Results and predictors of recurrent bleeding. Cardiovasc Intervent
Radiol. 33:1088–1100. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wong TC, Wong KT, Chiu PW, Teoh AY, Yu SC,
Au KW and Lau JY: A comparison of angiographic embolization with
surgery after failed endoscopic hemostasis to bleeding peptic
ulcers. Gastrointest Endosc. 73:900–908. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Behrman SW: Management of complicated
peptic ulcer disease. Arch Surg. 140:201–208. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jorge A, Diaz M, Lorenzo J and Jorge O:
Choledochoduodenal fistulas. Endoscopy. 23:76–78. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Colović R, Grubor N, Perisic M, Micev M,
Latincić S and Colović N: Choledochoduodenal fistula of ulcer
etiology. Srp Arh Celok Lek. 138:347–350. 2010.(In Serbian).
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Choi D, Lim HK, Kim MJ, Kim SJ, Kim SH,
Lee WJ, Lim JH, Paik SW, Yoo BC, Choi MS, et al: Liver abscess
after percutaneous radiofrequency ablation for hepatocellular
carcinomas: Frequency and risk factors. AJR Am J Roentgenol.
184:1860–1867. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zong KC, You HB, Gong JP and Tu B:
Diagnosis and management of choledochoduodenal fistula. Am Surg.
77:348–350. 2011.PubMed/NCBI
|
|
17
|
Vagefi PA, Ferguson CM and Hall JF: The
occurrence of gallstone ileus. Arch Surg. 143:l118–l120. 2008.
|
|
18
|
Agarwal N, Sharma BC, Garg S, Kumar R and
Sarin SK: Endoscopic management of postoperative bile leaks.
Hepatobiliary Pancreat Dis Int. 5:273–277. 2006.PubMed/NCBI
|