Introduction
Lipomas of the colon are extremely uncommon benign
tumors, with a frequency of 0.035–4.4% worldwide (1). Approximately 90% of cases originate from
the submucosa, while 10% arise from the subserosa (1). Lipomas have a benign clinical course
with a low recurrence rate following surgical excision and the
survival rate is ~99% 10 years subsequent to surgical excision
(2). Bauer was the first to describe
this entity in 1757 (3). Lipomas are
the third most prevalent benign tumor of the large bowel, after
hyperplastic and adenomatous polyps, and the incidence rate ranges
from 0.2–4.5% worldwide (1,4). These lesions are typically asymptomatic
and are discovered incidentally during colonoscopy, surgery or
autopsy (5). Gastroenterologists or
radiologists are able to distinguish the benign nature of such
tumors and characterize them as a lipoma; however,
histopathological examination is required to reach a final
diagnosis (6). In a small number of
cases, lipomas may cause symptoms such as pseudo-obstruction, blunt
abdominal pain, changes in daily defecation habits, rectal bleeding
and constipation (6). In extremely
rare cases, these lesions may also cause massive hemorrhage, full
obstruction of the colon's lumen, intussusceptions and perforation,
which results in acute abdomen and prolapse (5,6). The size
of lipomas may range from millimeters to centimeters in diameters,
but symptoms occur only when their diameter exceeds 2 cm (7). The term ‘giant lipoma’ is used when its
maximum diameter exceeds 5 cm (5).
The current case describes a young Caucasian woman who presented to
the Emergency Department of the University Hospital of Heraklion
(Crete, Greece) due to a 1-month history of blunt pain in the lower
abdomen and the presence of a solid mass, which prolapsed out of
the anus following defecation. The present study described this
rare case and reviewed the relevant literature in order to
standardize the necessary procedures required for the diagnosis and
treatment of these lesions.
Case report
In May 2013, a 27-year-old Caucasian woman was
admitted to the Emergency Department of the University Hospital of
Heraklion (Crete, Greece). The patient presented with difficulty
when defecating due to the presence of a solid mass, which
prolapsed out of the anus following defecation for the previous
month. The relevant medical history of the patient was unremarkable
without disease, and clinical examination of the abdomen was
unremarkable. Visual inspection of the anus and digital examination
of the rectum did not identify any notable pathological findings.
Therefore, the patient was asked to simulate the conditions of
normal defecation with prolonged extrusion, and a solid, yellow
mass protruding from the anal ring was observed.
The patient underwent an urgent colonoscopy, which
revealed a suspicious polypoid lesion measuring 2.5 cm in diameter,
which was located in the middle of the sigmoid colon ~12 cm above
the anal ring, with a smooth surface and tissue fragility. Tissue
samples were obtained and sent for histopathological analysis.
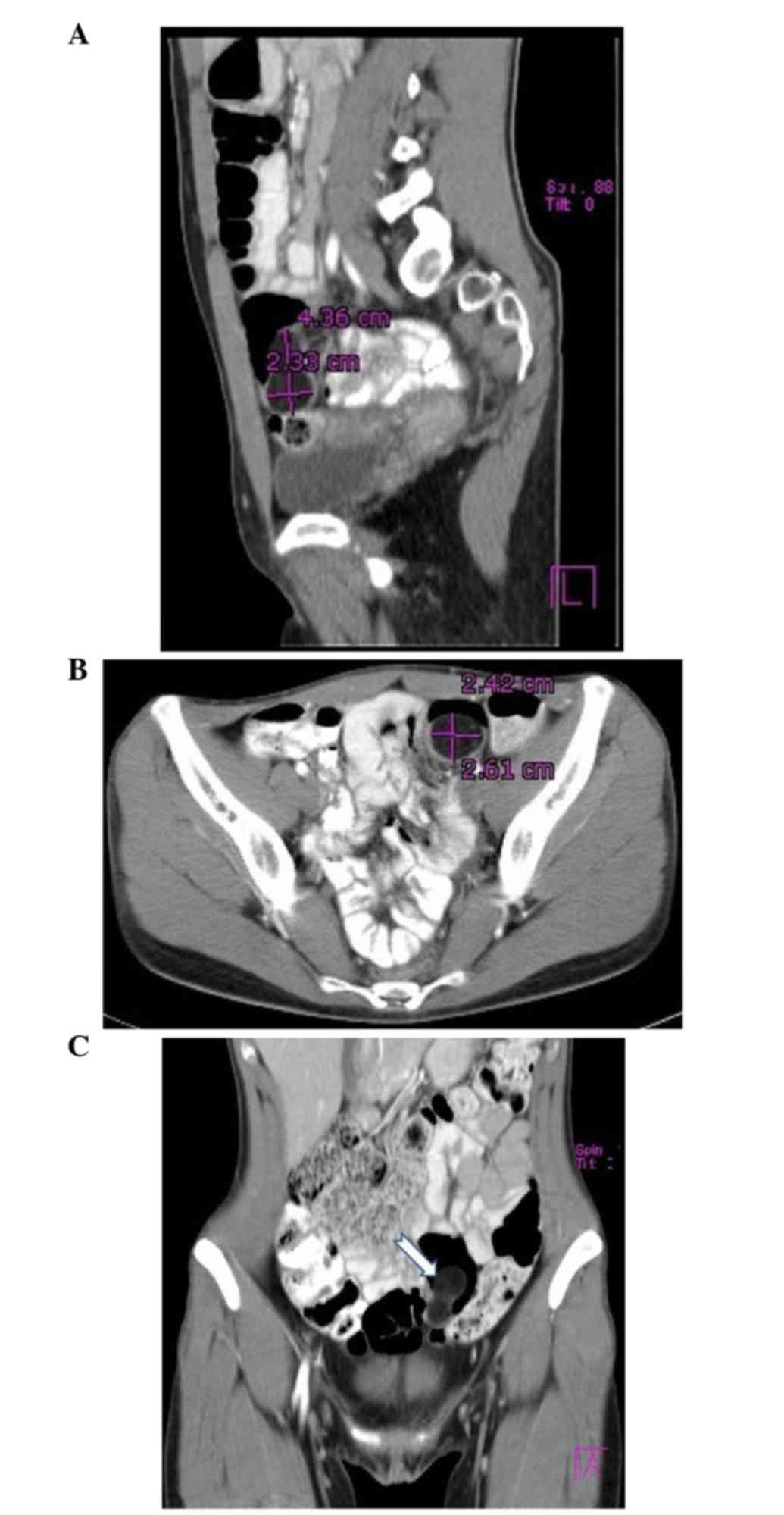
Contrast-enhanced computed tomography (CT) of the abdomen was
performed urgently and revealed the presence of a solid mass in the
sigmoid colon (Fig. 1). Regional
lymph nodes were not enlarged. Preoperative tests were completed,
including blood tests, and cancer biomarkers [including
carcinoembryonic antigen, α-fetoprotein, carbohydrate antigen
(CA)19-9, CA15-3 and CA125] were negative.
Following adequate intestinal preparation with
laxatives, the patient underwent a laparoscopic segmental
sigmoidectomy. The patient was placed in a traditional Lloyd-Davis
position, with the left arm abduced and the right arm positioned
along the body. During the procedure, the operating table was
tilted towards the right and ranged between Trendelenburg and
reverse Trendelenburg positions depending on the various operative
steps.
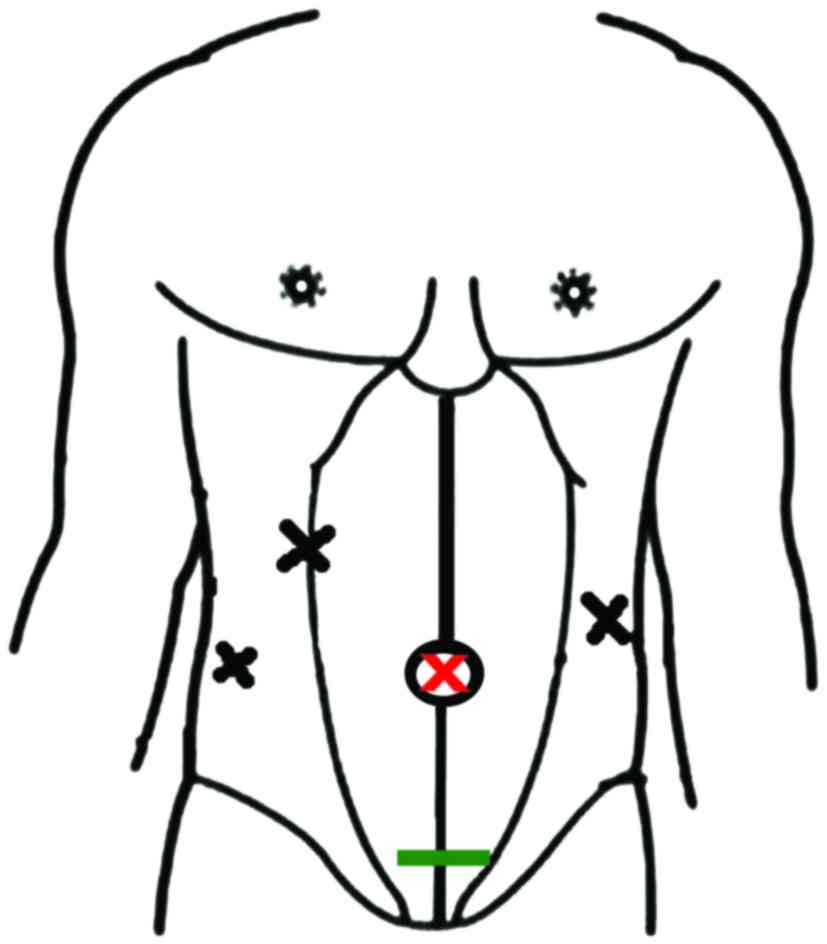
Initially, a 3-mm incision was made under the
umbilicus and a 12-mm trocar was inserted using the ‘Hasson
technique’. Insufflating carbon dioxide, pneumoperitoneum was
established to an abdominal pressure of 12–14 mmHg. Under direct
vision with laparoscopic assistance, one 12-mm trocar was inserted
into the right-middle subcostal area and two 11-mm trocars were
inserted into the frontal axillary line in the bilateral regions of
the abdomen (Fig. 2). Once the
abdominal cavity was full of carbon dioxide at a preset
intra-abdominal pressure, the sigmoid colon containing the lipoma
was identified. This segment of the sigmoid colon was dissected
with laparoscopic instruments (Ligasure® Dissector and
Endo-GIA™ 30 mm) using upward traction and a dissection from the
medial to lateral side. Subsequently, a small horizontal incision
of 4 cm was made in the midline of the lower abdomen, from which
the surgical specimen was removed (Figs.
3 and 4). The small abdominal
incision was sutured and pneumoperitoneum in the preset
intra-abdominal pressure was re-established. Finally, an
intracorporeal termino-terminal colorectal anastomosis was
performed, with the use of a 28 mm circular stapler, without the
use of a drain.
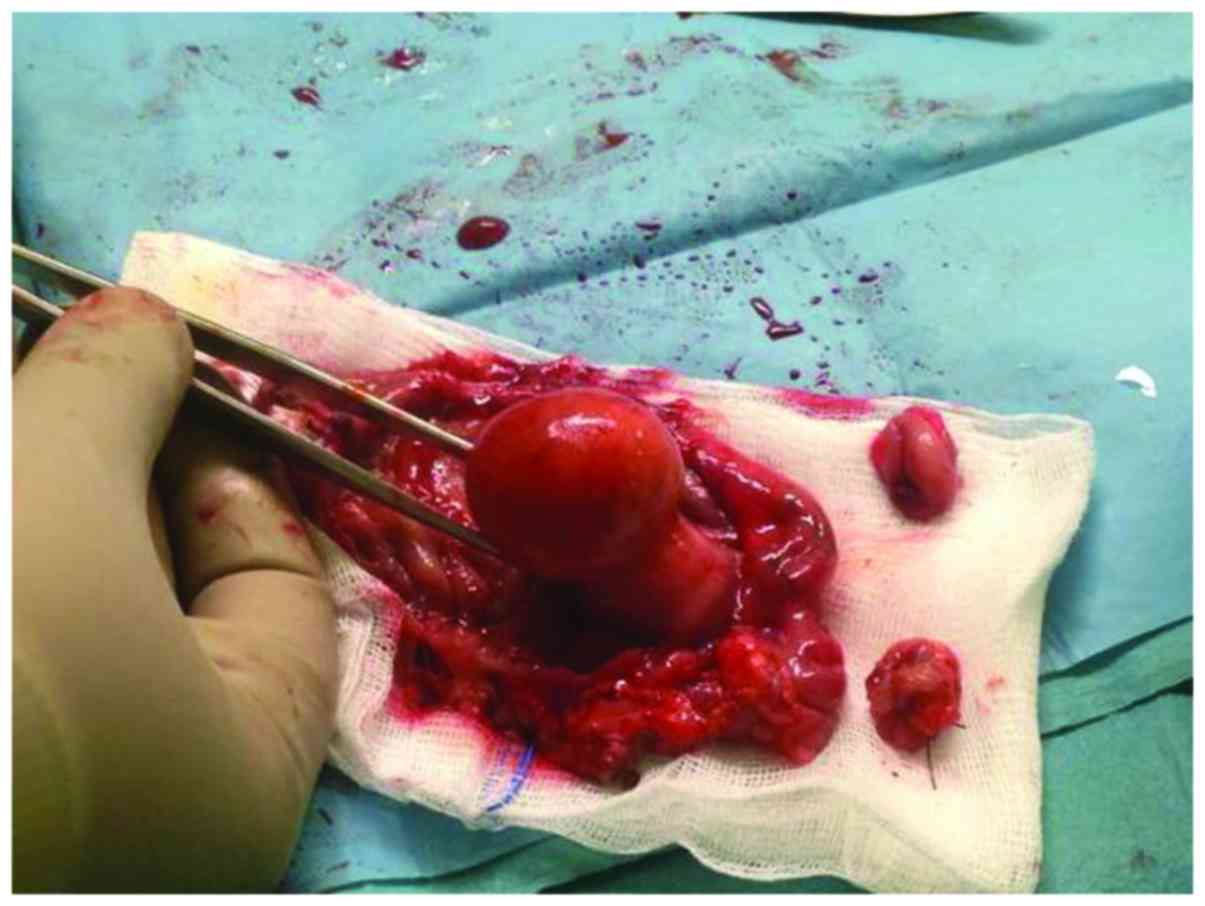
An intraoperative frozen section of the surgical
specimen was not performed. Macroscopic inspection of the resected
sigmoid colon confirmed the initial preoperative diagnosis
(Fig. 5). The surgical specimen
presented as a pedunculated lipoma that was shaped like a
‘champagne bottle cork’, and was covered in normal intestinal
mucosa, with well-shaped, bright yellow parenchyma. The patient had
a positive post-operative outcome without complications and was
discharged on day 4 post-surgery in an optimal condition.
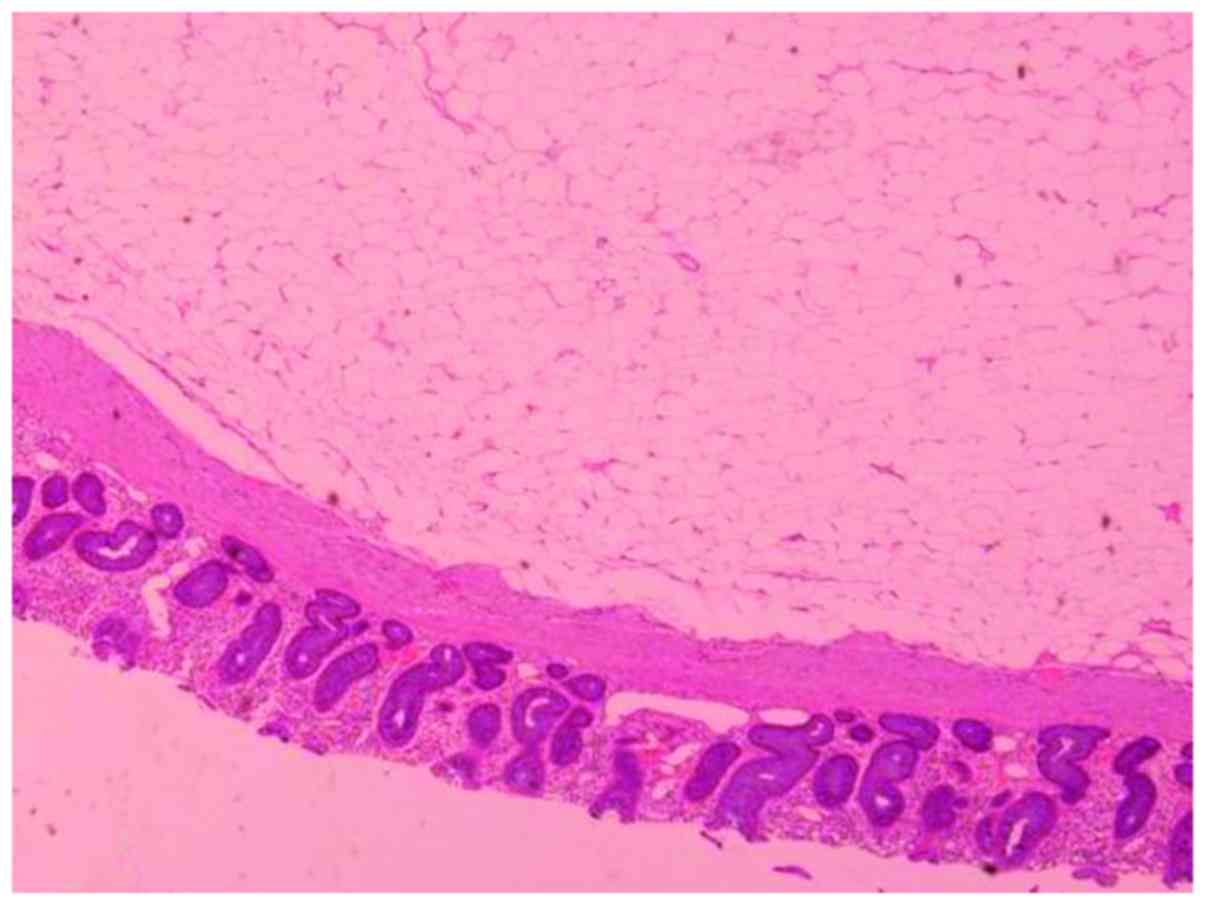
Histopathological examination of the formalin-fixed surgical
specimen revealed that the tumor was composed of mature adipose
tissue compatible with a lipoma, and also exhibited regions of
inflammatory changes in the colonic mucosa (Fig. 6). The overlying colonic mucosa showed
hyperplastic crypts with regenerative changes. In the lamina
propria mild inflammatory infiltration was observed. Serial
sections were obtained an embedded in paraffin. Hematoxylin and
eosin staining was performed on 3-µm sections, and the samples were
observed under a light microscope (Nikon Eclipse E400; Nikon
Corporation, Tokyo, Japan; magnification, ×100. At 3 years
post-surgery, the patient remains asymptomatic without any clinical
evidence of recurrence. The patient undergoes planned follow-up
appointments every 6 months, with blood tests (including cancer
biomarkers) and CT scanning of the abdomen and chest once a
year.
Written informed consent was obtained from the
patient for publication of the present study and any accompanying
images.
Discussion
Lipomas of the gastrointestinal tract are extremely
rare (4). Esophageal lipomas are
uncommon and account for 0.4% of all benign digestive tract
neoplasms (8). Gastric lipomas are
remarkably rare, benign tumors and are commonly located
submucosally in the gastric antrum; these lesions represent <5%
of all lipomas of the gastrointestinal tract (9). Additionally, lipomas may also be
identified accidentally within the small bowel due to
intussusception and gastrointestinal bleeding (10).
Lipomas of the large intestine are uncommon, benign,
adipose tumors that are typically asymptomatic and diagnosed
accidentally during colonoscopy (3).
Despite their rarity, they may occasionally induce symptoms such as
lower abdominal pain, pseudo-obstruction of the colon,
intussusceptions, hemorrhage and perforation (7). If they are localized to the sigmoid
colon, the lipoma may prolapse out of the anus ring, as observed in
the present case.
It may be challenging to obtain an accurate
preoperative diagnosis of a colon lipoma. Nowadays, a wide range of
imaging techniques are available that are able to help achieve a
reliable diagnosis (11). Abdominal
ultrasonography and abdominal radiography performed when the
patient is in an upright and decubitus position do not typically
aid the diagnosis of colon lipomas, due to their small size, the
adipose consistency and the low distinctive ability of these
imaging techniques (12). Abdominal
double-contrast (intravenous and peros) CT may aid a reliable
diagnosis, and are able to determine the size, position, morphology
and proximity of the lipoma to adjacent organs and tissues
(13). In addition, magnetic
resonance imaging of the abdomen may help lipoma diagnosis, but
does not appear to have superior diagnostic value compared with CT
(14).
Endoscopic examination of the large colon serves an
important role not only to achieve accurate diagnosis, but also
when forming the final therapeutic plan for the patient. According
to the literature, there is a theory that pedunculated lipomas with
a diameter of <2 cm may be removed by endoscopy without major
complications (15).
Preoperative tests may include blood cell counts,
hepatic and renal biochemical functional profiling, and evaluation
of cancer markers (11). The adequate
preoperative preparation of the patient is crucial for a positive
surgical outcome. Solid preparation of the bowel with laxatives,
and preoperative administration of antibiotics and prophylactic
low-molecular-weight heparin for the prevention of deep vein
thrombosis, are routine practices.
Once preoperative tests and preparation are
completed, the surgeon must then decide whether to perform open
surgery or use laparoscopic techniques.
With regards to open surgery, it is less likely that
the surgeon may encounter intraoperative complications compared
with laparoscopic techniques (16).
However, there is an increase in the duration of intraoperative
surgery and post-operative hospitalization time, and therefore,
daily hospital charges are greater. Post-operative complications,
including intra-abdominal abscesses, post-operative ileus, wound
infection and respiratory failure, occur more often following open
procedures. Post-operative chronic pain is less likely to occur in
patients who undergo laparoscopic resection vs. those who undergo
open laparotomy (16,17). In the present case, the patient
underwent a laparoscopic procedure and had an uneventful
post-operative hospitalization.
It has been suggested that intraoperative frozen
section of surgical specimens may provide an accurate diagnosis to
guide the selection of surgical procedures (18). In the current case, histopathological
examination of the surgical specimen was performed postoperatively,
therefore further strategic planning of the surgical operation and
intraoperative management of the patient was straightforward.
In conclusion, the present case highlights an
extremely rare surgical entity and describes the process from
diagnosis to surgical treatment (11). Colonoscopy and laparoscopy are
considered as the best options for diagnosis and treatment,
respectively, for patients with lipomas (15–17). The
surgical excision of a sigmoid colon lipoma is a great challenge
for surgeons. The correct pre-operative management, the appropriate
radiological examinations and the right surgical method chosen by
the surgeon can all lead to a successful result. Surgical therapy,
though challenging and demanding, may be the only mode of treatment
that can offer these patients a return to a satisfactory level of
function and quality of life. Informed consent is always necessary
and ensures that the patient is fully aware of all the pros and
cons. In conclusion, the present scientific report may assist
surgeons worldwide with the correct decision making in similar
cases.
References
|
1
|
Yaman İ, Derici H and Demirpolat G: Giant
colon lipoma. Ulus Cerrahi Derg. 31:102–104. 2013.PubMed/NCBI
|
|
2
|
Mnif L, Amouri A, Masmoudi MA, Mezghanni
A, Gouiaa N, Boudawara T and Tahri N: Giant lipoma of the
transverse colon: A case report and review of the literature. Tunis
Med. 87:398–402. 2009.PubMed/NCBI
|
|
3
|
Ryan J, Martin JE and Pollock DJ: Fatty
tumours of the large intestine: A clinicopathological review of 13
cases. Br J Surg. 76:793–796. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vecchio R, Ferrara M, Mosca F, Ignoto A
and Latteri F: Lipomas of the large bowel. Eur J Surg. 162:915–919.
1996.PubMed/NCBI
|
|
5
|
Târcoveanu E, Chifan M, Veisa E, Epure O
and Florea N: Colonic lipoma. Chirurgia (Bucur). 95:353–357.
2000.(In Romanian). PubMed/NCBI
|
|
6
|
Begos DG, Sandor A and Modlin IM: The
diagnosis and management of adult intussusceptions. Am J Surg.
173:88–94. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Atmatzidis S, Chatzimavroudis G, Patsas A,
Papaziogas B, Kapoulas S, Kalaitzis S, Ananiadis A, Makris J and
Atmatzidis K: Pedunculated cecal lipoma causing colo-colonic
intussusception: A rare case report. Case Rep Surg.
2012:2792132012.PubMed/NCBI
|
|
8
|
Tsalis K, Antoniou N, Kalfadis S, Dimoulas
A, Dagdilelis AK and Lazaridis C: Laparoscopic enucleation of a
giant submucosal esophageal lipoma. Case report and literature
review. Am J Case Rep. 14:179–183. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ramdass MJ, Mathur S, Seetahal-Maraj P and
Barrow S: Gastric lipoma presenting with massive upper
gastrointestinal bleeding. Case Rep Emerg Med.
2013:5061012013.PubMed/NCBI
|
|
10
|
Lucas LC, Fass R and Krouse RS:
Laparoscopic resection of a small bowel lipoma with incidental
intussusception. JSLS. 14:615–618. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sourrouille I, Vilcot L, Honoré C, Coppola
S, Terrier P, le Cesne A, Le Péchoux C and Bonvalot S: Algorithm
for the surgical management of mesenchymal tumors of the perineum
in adults. Dis Colon Rectum. 58:304–313. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kuzmich S, Harvey CJ, Kuzmich T and Tan
KL: Ultrasound detection of colonic polyps: Perspective. Br J
Radiol. 85:e1155–e1164. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Moussa OM, Tee M, Khan AU and Selvasekar
CR: Computerized tomography providing definitive diagnosis of
colonic lipoma: A case series. Surg Laparosc Endosc Percutan Tech.
23:e232–e243. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Leufkens AM, Kwee TC, van den Bosch MA,
Mali WP, Takahara T and Siersema PD: Diffusion-weighted MRI for the
detection of colorectal polyps: Feasibility study. Magn Reson
Imaging. 31:28–35. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mummadi R and Raju GS: New endoscopic
approaches to removing colonic lipomas. Gastroenterol Hepatol.
3:882–883. 2007.
|
|
16
|
Onder A, Benlice C, Church J, Kessler H
and Gorgun E: Short-term outcomes of laparoscopic versus open total
colectomy with ileorectal anastomosis: a case-matched analysis from
a nationwide database. Tech Coloproctol. 20:767–773. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Stormark K, Søreide K, Søreide JA, Kvaløy
JT, Pfeffer F, Eriksen MT, Nedrebø BS and Kørner H: Nationwide
implementation of laparoscopic surgery for colon cancer: Short-term
outcomes and long-term survival in a population-based cohort. Surg
Endosc. 30:4853–4864. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Khoury W, Abboud W, Hershkovitz D and Duek
SD: Frozen section examination may facilitate reconstructive
surgery for mid and low rectal cancer. J Surg Oncol. 110:997–1001.
2014. View Article : Google Scholar : PubMed/NCBI
|