Introduction
The standard treatment for locally advanced cervical
cancer is pelvic external beam radiation therapy (EBRT) with
concurrent cisplatin chemotherapy and brachytherapy (BT) (1–3). Recently,
3D image-guided brachytherapy (IGBT), which uses computed
tomography (CT) or magnetic resonance imaging (MRI) to obtain
images of inserted applicators, has come into widespread use
(4–6).
The present study reports the use of BT in a patient with locally
advanced cervical cancer involving a complete septate uterus with
right and left uterine canals. Prior to treatment, CT images were
obtained with a tandem implant inserted alternately into the right
and left uterine canals. A treatment-planning system was used to
compare the resulting dose volumes; the uterine canal that was
associated with optimal distribution of the dose volume was chosen
for BT. There have been only a few reports of BT in patients with
uterine anomalies. To the best of our knowledge, this is the first
case in which the dose-volume difference between tandem implant
placement in the right versus left uterine canal was examined.
Case report
Patient presentation and
diagnosis
A 55-year-old woman presented with a 1-month history
of general malaise. A high creatinine level of 2.26 mg/dl (normal
range, 0.46–0.79 mg/dl) was found upon hematological examination;
CT revealed that a cervical tumor was causing bilateral
hydronephrosis involving the bilateral ureters. Therefore,
bilateral ureteral stents were inserted. Tissue biopsy of the
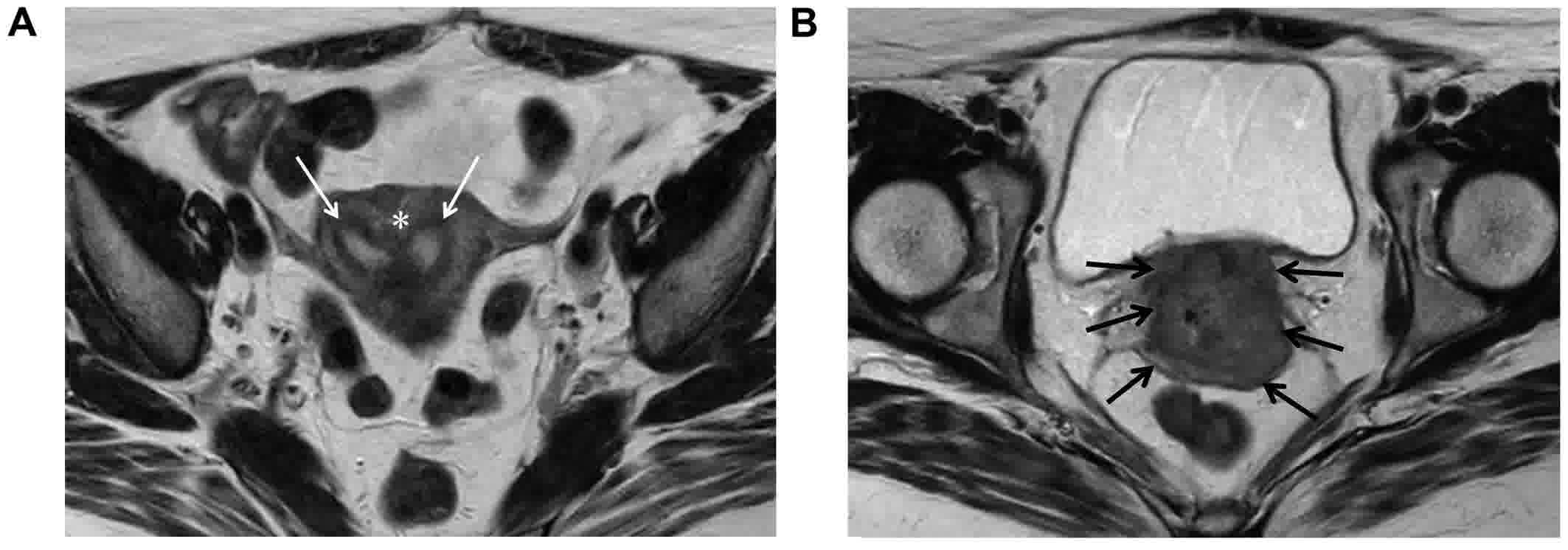
cervical tumor led to a diagnosis of squamous cell carcinoma. MRI
revealed that the endometrial cavity was separated into right and
left canals by a septum on the cranial side of the cervical tumor
(Fig. 1A and B). The septum reached
the level of the internal cervical os, indicating a complete
septate uterus corresponding to class V of the American Society of
Reproductive Medicine classification (7) and class U2 of the European Society of
Human Reproduction and Embryology/European Society for
Gynaecological Endoscopy classification (8). The patient exhibited hydronephrosis at
presentation, indicating disease stage IIIB, according to the
uterine cervical cancer staging system of the International
Federation of Gynecology and Obstetrics (FIGO) (9). CT and MRI revealed no lymph node
metastasis; endoscopy revealed no abnormalities of the mucosa in
the rectum or the bladder. Thus, combined EBRT and concurrent
chemotherapy with 5 courses of intravenously administered weekly
cisplatin (40 mg/m2) and high-dose-rate BT were planned
with hospitalization. For EBRT, whole-pelvic irradiation, covering
the cervical tumor, uterus, parametrium, vagina, and the pelvic
lymph node regions as the clinical target volume, was performed
using the box technique (6).
Irradiation was applied at 2 Gy per fraction five times per week
until 30 Gy was reached. Thereafter, a central shield (3 cm wide)
was added and irradiation was administered until a total dose of 50
Gy was reached.
Intracanal brachytherapy
A second MRI performed prior to BT revealed that the
cervical tumor had shrunk, allowing the tandem insert to be
inserted into the right and left uterine canals separately. The
right canal lumen was 7 cm long and the left was 6 cm, according to
MRI findings. In the BT room, a standard tandem implant (LAR 04-01;
Eckert & Ziegler BEBIG, Berlin, Germany) with a 15° angle was
inserted in the left uterine canal to a distance of 6 cm from the
external cervical os under X-ray fluoroscopy; ovoid implants were
inserted into the right and left vaginal fornices. Following X-ray
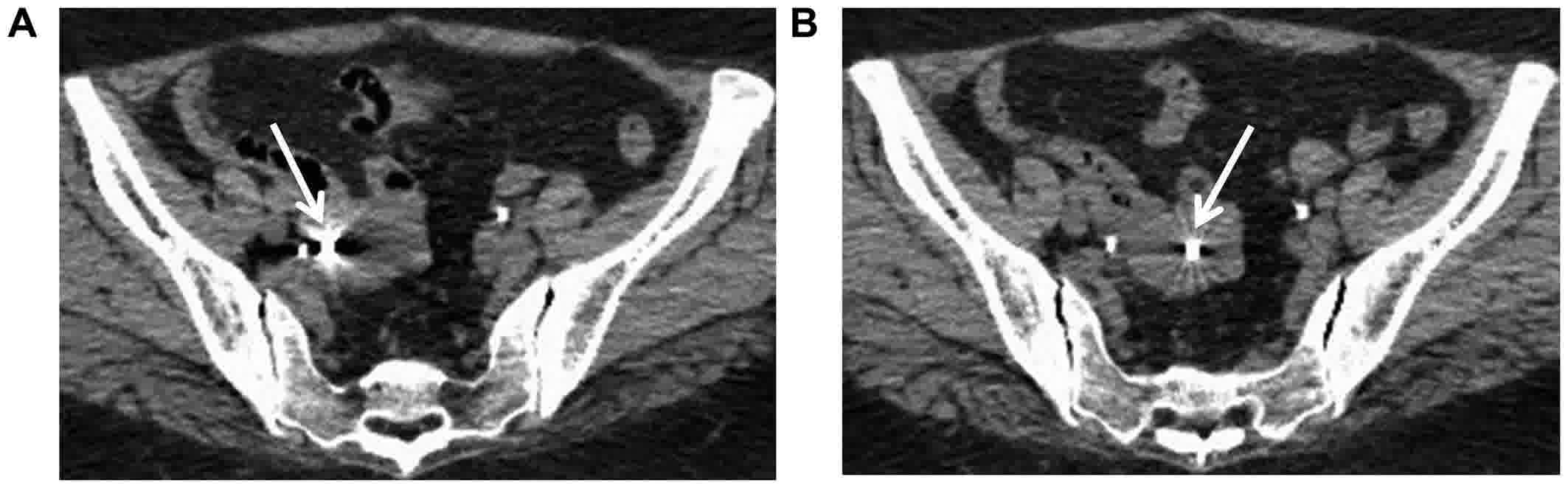
imaging, the patient was transferred to a CT room, where CT images
with a 2-mm slice thickness were obtained and tandem implant
insertion in the left uterine canal was confirmed (Fig. 2A). The patient was returned to the BT
room, where a standard tandem implant (LAR 06-01; Eckert &
Ziegler BEBIG) with a 30° angle was inserted in the right uterine
canal at a distance of 7 cm under X-ray fluoroscopy; ovoid implants
were placed into the right and left vaginal fornices. After X-ray
imaging, CT images were obtained that confirmed tandem implant
insertion in the right uterine canal (Fig. 2B). At Nihon University School of
Medicine (Tokyo, Japan), high-dose-rate BT was performed with a
60Co remote afterloading system (MultiSource; Eckert
& Ziegler BEBIG). The CT images were uploaded to the treatment
planning system (HDR plus; Eckert & Ziegler BEBIG), and the
high-risk clinical target volume (HR-CTV) and organs at risk (OARs;
the rectum and bladder) were contoured according to the Groupe
Européen de Curiethérapie and the European Society for Radiotherapy
and Oncology guidelines (10,11). The gross tumor volume was determined
using pretreatment contrast-enhanced CT images and second MRI
images prior to BT for reference. At Nihon University School of
Medicine, positional checks for BT are performed with X-ray films
alone; Manchester point A (12) was
used for treatment planning. On CT, the left and right Manchester
point A were set 2 cm superior to the line connecting the superior
aspects of the ovoid implants and 2 cm to the right and left of the
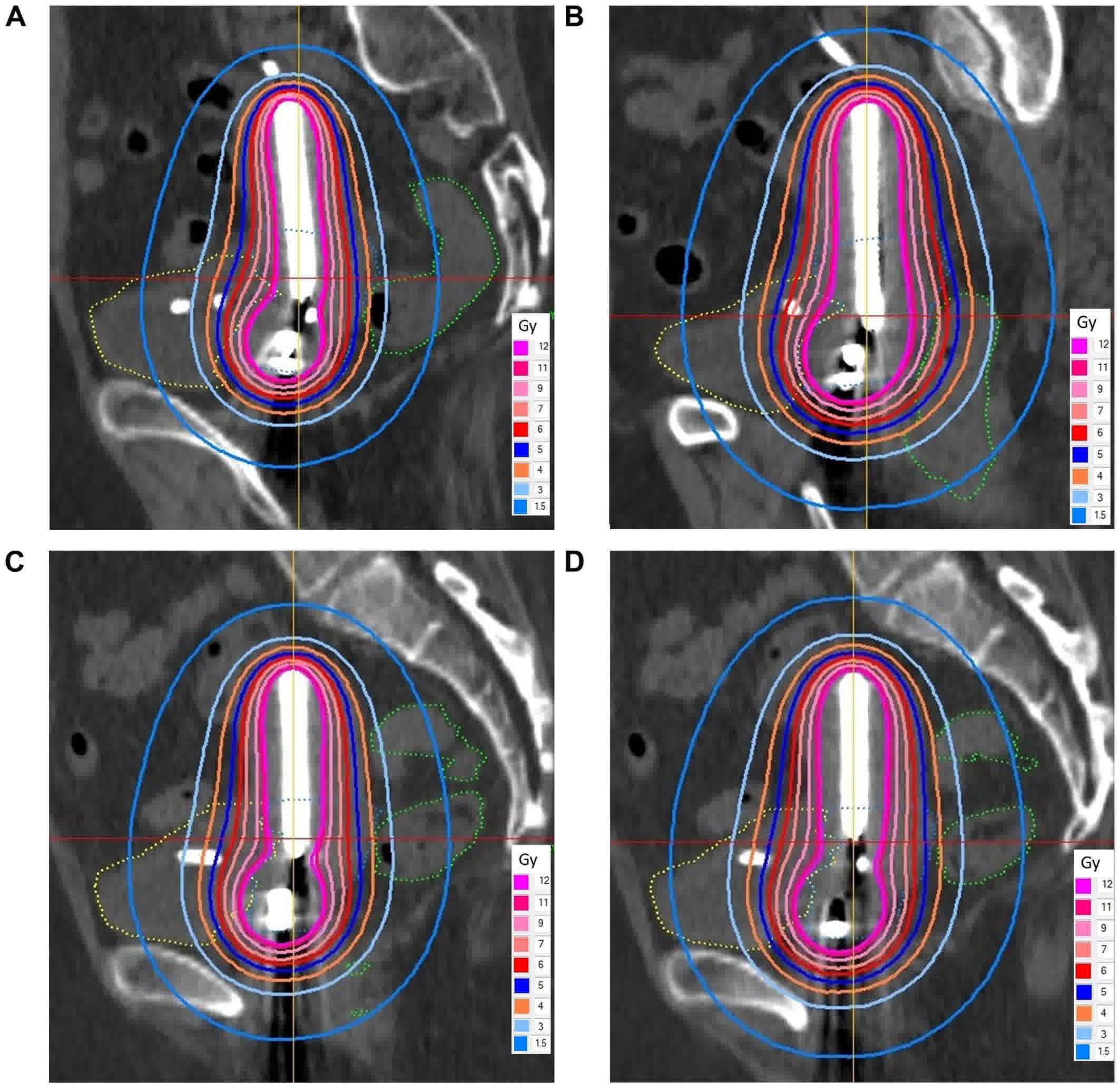
intrauterine source train. Calculation of the 90% target dose
(D90) for HR-CTV, the minimum dose delivered to the
highest irradiated 2-cm3 area (D2
cm3) for the rectum, and the D2
cm3 for the bladder per fraction at a dose of 6 Gy
to the right and left of point A with the tandem implant inserted
into the right and left uterine canals in succession revealed the
presence of wide variations in the isodose lines for the OARs
(Fig. 3). When the dose-volume
histograms of these four treatment plans were compared, there were
variations in each item; there was a particularly wide variation in
D2 cm3 for the bladder, ranging from 7.49 to
12.41 Gy per fraction (Table I). A
total of four irradiations (two irradiations based on the treatment
plan at the right point A with the tandem implant inserted into the
right uterine canal, which was associated with the lowest dose for
OARs, and two irradiations based on the treatment plan at the left
point A with the tandem implant inserted into the right uterine
canal, which was associated with the highest dose for HR-CTV) were
applied at a dose of 6 Gy per fraction. Prior to each BT session,
X-ray films were obtained and compared with X-ray images obtained
at the time of CT for positional checks, and tandem implant
insertion in the right uterine canal was confirmed. To reproduce
the treatment plan developed with CT imaging as accurately as
possible, the patients legs were extended during BT in the same
manner as during CT imaging. The total dose of EBRT and BT was
~61.76 Gy [2 Gy per fraction-equivalent dose; (EQD2)] for
D90 for HR-CTV, 61.73 Gy (EQD2) for D2
cm3 for the rectum and 115.5 Gy (EQD2) for D2
cm3 for the bladder, with α/β=10 for HR-CTV and
α/β=3 for the OARs. The cisplatin dose was reduced to 30
mg/m2 because of renal function impairment, as was
administered once a week for five courses. As acute complications,
grade 2 diarrhea and grade 2 cystitis (according to the National
Cancer Institute Common Terminology Criteria for Adverse Events
4.03 (13) were noted; which resolved
spontaneously. No local recurrence has occurred at the time of
writing, 1.5 months after the completion of radiation therapy.
 | Table I.Dose-volume histogram variations for
high-risk clinical target volume and organs at risk at a prescribed
dose of 6 Gy per fraction at point A. |
Table I.
Dose-volume histogram variations for
high-risk clinical target volume and organs at risk at a prescribed
dose of 6 Gy per fraction at point A.
| GrLocation of tandem
implant | Point A | HR-CTV
D90, Gy | Rectum D2
cm3, Gy | Bladder D2
cm3, Gy |
|---|
| Right canal | Right | 5.01 | 4.17 | 7.49 |
| Right canal | Left | 6.85 | 5.70 | 10.24 |
| Left canal | Right | 4.92 | 5.06 | 10.52 |
| Left canal | Left | 5.81 | 5.96 | 12.41 |
Discussion
The standard treatment for locally advanced uterine
cervical cancer is EBRT with concurrent cisplatin chemotherapy and
BT (14,15). For BT, a prescribed dose of
irradiation is traditionally applied to the Manchester point A.
However, in the case of a large mass, it is possible for
irradiation to this point A, administered with a uniform approach,
to result in an insufficient dose to the tumor. In recent years,
favorable disease control has been achieved with more efficient
irradiation of cervical tumors using 3D image-guided BT (IGBT) with
CT or MRI, instead of a point A prescription (4–6). However,
a 2015 nationwide Japanese survey reported that 84% of BT treatment
facilities used X-ray films during treatment (16). Until recently, position-checking and
treatment-planning at Nihon University School of Medicine were
performed using a 2D method that used X-ray film, as CT was not
available in the treatment room, and it was therefore difficult to
obtain CT images with the patient in a proper position and with the
applicators inserted properly. A standard fixed dose of 6 Gy per
fraction was prescribed to the point A, according to the Japanese
Gynecologic Oncology Group 1066 prospective study (15). However, the present patient had a
complete septate uterus with left and right uterine canals.
Therefore, it was expected that the dose distribution of the point
A prescription would vary widely depending upon whether the tandem
implant was inserted into the right or left uterine canal. To
overcome this challenge, the tandem implant was inserted into the
right and left uterine canal by turns and CT images were used to
compare the resulting dose-volume histograms. As expected, the
D90 for HR-CTV and the D2 cm3 for
the OARs varied according to the point A and the location of the
tandem implant. The variation was particularly wide in the D2
cm3 for the bladder. This finding might be
explained by changes in the intensity of bladder compression by the
uterus according to the position of the tandem implant. This
variation in the dose to OARs cannot be assessed with X-ray films
alone. The use of CT images in this case allowed us to confirm the
optimal uterine canal for tandem implant insertion and the optimal
point A.
To the best of our knowledge, there have been only
four reported cases (17–20) of BT in patients with uterine anomalies
(Table II). No dose-volume histogram
comparisons with insertion of the tandem implant into the right
versus left uterine canals were reported in any of those cases. Two
cases of BT in patients with uterus didelphys have been reported
(17,20). In one of these cases, tandem implants
were inserted into the two uterine canals simultaneously, and the
point A was defined according to the midline between the two tandem
implants and was 2 cm superior to the mean position of the os
cervix (17). In the other case, a
mold was inserted vaginally and a dose was prescribed for HR-CTV
according to IGBT (20). One reported
case involved a bicornuate uterus. In that case, a mold was
inserted vaginally, and from there a radiation source was inserted
into one uterine canal, whereas a marker was inserted into the
other uterine canal and the position of the marker of point A of
the other side was calculated; this process was repeated for the
opposite canal (18). The fourth
patient had a partial septate uterus. In that case, the Rotte Y
applicator, which includes two tandem implants, was used; tandem
implants were inserted simultaneously into the two uterine canals
and were locked together with two ovoid implants. Point A was then
defined as 2 cm superior to the line connecting the superior aspect
of the ovoid implants and 2 cm lateral to the line running between
and parallel to the two channels of the Rotte Y applicator
(19).
 | Table II.Patients with uterine anomaly treated
with brachytherapy. |
Table II.
Patients with uterine anomaly treated
with brachytherapy.
| Patient | Age, years | FIGO stage | Histology | Uterine anomaly | EBRT | BT technique and
dose | Chemotherapy | RFS, months | (Refs.) |
|---|
| 1 | 45 | IIA1 | P/D squamous cell
carcinoma | Uterus didelphys | Whole pelvis; 45
Gy | 2 tandems in the two
uterine canals; HDR; 6 Gy × 1, 6.5 Gy × 1; modified point A | Unknown | ~36 | (17) |
| 2 | 58 | IIA | M/D squamous cell
carcinoma | Bicornuate
uterus | Whole pelvis; 50
Gy | Vaginal mold and
catheter alternately in each uterine canal; LDR; 9 Gy × 2; point
A | Cisplatin | 24 | (18) |
| 3 | 34 | IIB | P/D
adenocarcinoma | Septate uterus | Whole pelvis; 45 Gy;
metastatic iliac node; additional 9 Gy | 2 tandem implants in
the two uterine canals and 2 ovoid implants; HDR; 5.5 Gy × 5; point
A | Cisplatin | 20 | (19) |
| 4 | 37 | IIIA | Adenocarcinoma | Uterus didelphys | Whole pelvis and
para-aorta; 50.4 Gy; | Vaginal mold; PDR; 20
Gy × 1; HR-CTV GTV 59.92 Gy | Cisplatin | 30 | (20) |
| 5 | 55 | IIIB | P/D squamous cell
carcinoma | Septate uterus | Whole pelvis; 50
Gy | Tandem implants in
right uterine canal and 2 ovoid implants; 6 Gy × 4; point A | Cisplatin | 1.5 | Present case |
Uterine anomalies are found in up to 7% of women. A
septate uterus is the most common of these, found in 0.9–2% of
women and accounting for 55% of all mullerian anomalies (21,22).
Detailed examination of CT and MRI images from patients with
uterine cervical cancer reveals that a septate uterus may not be
uncommon. When BT is performed in patients with a septate uterus,
the optimal dose distribution can be determined without the use of
special instruments by comparing dose-volume histograms with the
standard tandem implant inserted alternately into the right and
left uterine canals. In the present case, the approximate total
dose of EBRT and BT was 61.76 Gy (EQD2) for the D90 for
HR-CTV, 61.73 Gy (EQD2) for the D2 cm3 for
the rectum, and 115.5 Gy (EQD2) for the D2
cm3 for the bladder. According to a previous study
concerning a patient with uterine cervical cancer treated with BRT
and BT with central shielding (6),
the D90 for HR-CTV reached the necessary dose, and the
patient exhibited no local recurrence. However, the D2
cm3 for the bladder was high, necessitating
meticulous ongoing follow-up for the possible development of late
complications.
The present study shows that when cervical cancer
with uterine anomalies is treated with BT, the projected dose and
the clinical target volume may vary, putting organs at risk. Where
possible, CT based BT should be the preferred course of action.
Acknowledgements
The authors would like to thank Dr Rebecca Tollefson
for editing a draft of this manuscript.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors contributions
NI treated the patient and analyzed the patients
data, and was a major contributor in writing the manuscript. TN
biopsied the cervical tumor and performed chemotherapy. TM, TA, MS
and MO treated the patient. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent.
Consent for publication
The patient provided written informed consent.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EBRT
|
external beam radiation therapy
|
|
BT
|
brachytherapy
|
|
IGBT
|
image-guided brachytherapy
|
References
|
1
|
Eifel PJ, Winter K, Morris M, Levenback C,
Grigsby PW, Cooper J, Rotman M, Gershenson D and Mutch DG: Pelvic
irradiation with concurrent chemotherapy versus pelvic and
para-aortic irradiation for high-risk cervical cancer: An update of
radiation therapy oncology group trial (RTOG) 90–01. J Clin Oncol.
22:872–880. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rose PG, Bundy BN, Watkins EB, Thigpen JT,
Deppe G, Maiman MA, Clarke-Pearson DL and Insalaco S: Concurrent
cisplatin-based radiotherapy and chemotherapy for locally advanced
cervical cancer. N Engl J Med. 340:1144–1153. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chemoradiotherapy for Cervical Cancer
Meta-Analysis Collaboration: Reducing uncertainties about the
effects of chemoradiotherapy for cervical cancer: A systematic
review and meta-analysis of individual patient data from 18
randomized trials. J Clin Oncol. 26:5802–5812. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ribeiro I, Janssen H, De Brabandere M,
Nulens A, De Bal D, Vergote I and Van Limbergen E: Long term
experience with 3D image guided brachytherapy and clinical outcome
in cervical cancer patients. Radiother Oncol. 120:447–454. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sturdza A, Pötter R, Fokdal LU, Haie-Meder
C, Tan LT, Mazeron R, Petric P, Šegedin B, Jurgenliemk-Schulz IM,
Nomden C, et al: Image guided brachytherapy in locally advanced
cervical cancer: Improved pelvic control and survival in
RetroEMBRACE, a multicenter cohort study. Radiother Oncol.
120:428–433. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ohno T, Noda SE, Okonogi N, Murata K,
Shibuya K, Kiyohara H, Tamaki T, Ando K, Oike T, Ohkubo Y, et al:
In-room computed tomography-based brachytherapy for uterine
cervical cancer: Results of a 5-year retrospective study. J Radiat
Res. 58:543–551. 2017.PubMed/NCBI
|
|
7
|
The American Fertility Society
classifications of adnexal adhesions, distal tubal occlusion, tubal
occlusion secondary to tubal ligation, tubal pregnancies, müllerian
anomalies and intrauterine adhesions. Fertil Steril. 49:944–955.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Grimbizis GF, Gordts S, Di Spiezio Sardo
A, Brucker S, De Angelis C, Gergolet M, Li TC, Tanos V, Brölmann H,
Gianaroli L and Campo R: The ESHRE/ESGE consensus on the
classification of female genital tract congenital anomalies. Hum
Reprod. 28:2032–2044. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pecorelli S: Revised FIGO staging for
carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol
Obstet. 105:103–104. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Haie-Meder C, Pötter R, Van Limbergen E,
Briot E, De Brabandere M, Dimopoulos J, Dumas I, Hellebust TP,
Kirisits C, Lang S, et al: Gynaecological (GYN) GEC-ESTRO working
group. Recommendations from Gynaecological (GYN) GEC-ESTRO working
group (I): Concepts and terms in 3D image based 3D treatment
planning in cervix cancer brachytherapy with emphasis on MRI
assessment of GTV and CTV. Radiother Oncol. 74:235–245. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pötter R, Haie-Meder C, Van Limbergen E,
Barillot I, De Brabandere M, Dimopoulos J, Dumas I, Erickson B,
Lang S, Nulens A, et al: Recommendations from gynaecological (GYN)
GEC ESTRO working group (II): Concepts and terms in 3D image-based
treatment planning in cervix cancer brachytherapy-3D dose volume
parameters and aspects of 3D image-based anatomy, radiation
physics, radiobiology. Radiother Oncol. 78:67–77. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dean EM, Lambert GD and Dawes PJ:
Gynaecological treatments using the Selectron remote afterloading
system. Br J Radiol. 61:1053–1057. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
National cancer institute common
terminology criteria for adverse events (CTCAE). 4.03. Jun
14–2010.
|
|
14
|
Monk BJ, Tewari KS and Koh WJ:
Multimodality therapy for locally advanced cervical carcinoma:
State of the art and future directions. J Clin Oncol. 25:2952–2965.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Toita T, Kitagawa R, Hamano T, Umayahara
K, Hirashima Y, Aoki Y, Oguchi M, Mikami M and Takizawa K: Cervical
Cancer (Vulva Cancer) Committee of Japanese Gynecologic Oncology
Group (JGOG): Phase II study of concurrent chemoradiotherapy with
high-dose-rate intracavitary brachytherapy in patients with locally
advanced uterine cervical cancer: Efficacy and toxicity of a low
cumulative radiation dose schedule. Gynecol Oncol. 126:211–216.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ohno T, Toita T, Tsujino K, Uchida N,
Hatano K, Nishimura T and Ishikura S: A questionnaire-based survey
on 3D image-guided brachytherapy for cervical cancer in Japan:
Advances and obstacles. J Radiat Res. 56:897–903. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee CD, Churn M, Haddad N,
Davies-Humphries J, Kingston RK and Jones B: Bilateral radical
radiotherapy in a patient with uterus didelphys. Br J Radiol.
73:553–556. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Loo HW and Locks SM: Squamous cell
carcinoma of the cervix: Report of an unusual case of bicornuate
bicollis uterus treated with bilateral intracavity brachytherapy.
Br J Radiol. 83:e143–e146. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Platta CS, Wallace C, Gondi V, Das R,
Straub M, Al-Niaimi A, Applegate G and Bradley KA: Cervical
brachytherapy technique for locally advanced carcinoma of the
cervix in a patient with septate uterus. J Contemp Brachytherapy.
6:76–81. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cordoba A, Escande A, Comte P, Fumagalli
I, Bresson L, Mubiayi N and Lartigau E: Locally advanced
adenocarcinoma of the cervix on uterus didelphys: A case report. J
Contemp Brachytherapy. 9:71–76. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bhagavath B, Ellie G, Griffiths KM, Winter
T, Alur-Gupta S, Richardson C and Lindheim SR: Uterine
malformations: An update of diagnosis, management, and outcomes.
Obstet Gynecol Surv. 72:377–392. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Troiano RN and McCarthy SM: Mullerian duct
anomalies: Imaging and clinical issues. Radiology. 233:19–34. 2004.
View Article : Google Scholar : PubMed/NCBI
|