Introduction
Concomitant chemo-radiation therapy (CCRT) is a
standard treatment for head and neck cancer (1,2). For
recurrent cases or residual cases following CCRT, salvage surgery
is one of the important treatment options (3). With the increasing use of CCRT in the
treatment of head and neck cancer (4), salvage surgery following failed CCRT
will be increasingly prominent. Higher rates of acute and long-term
toxicity following CCRT could result in higher rates of
postoperative morbidity and mortality (5,6).
Swallowing disorders are major complications of CCRT that can
directly affect the quality of life of the patient. Previous
studies have shown that the major complications of CCRT are
xerostomia, reduced mobility of the tongue base, reduced mobility
of the larynx, reduced pharyngeal and laryngeal sensation
(incomplete protection of the airway) and trismus (7,8). These
complications can result in the reduction of pharyngeal
construction and inadequate laryngeal closure. Pharyngeal
constriction, which presses the bolus to the esophagus, and
laryngeal closure, which prevents bolus invasion to the lungs,
serve major roles in swallowing function. In this sense, it seems
that total laryngectomy and total pharyngo-laryngo-esophagectomy
(TPLE) with free jejunal graft reconstruction cannot cause
dysphagia because the larynx is removed. However, the incidence of
dysphagia following total laryngectomy has been reported to range
between 10 and 60% (9). Similarly,
the overall reported incidence of dysphagia following
pharyngolaryngectomy with free jejunal graft reconstruction is
reported to range between 2 and 58% (10). Previous studies (9,10) have
reported a higher incidence of dysphagia at discharge and at
long-term follow-up in patients that underwent laryngectomy or
pharyngolaryngectomy. We therefore hypothesized that pharyngeal
constriction is strongly associated with swallowing function
following TPLE. Furthermore, swallowing function following salvage
TPLE is poorer than that following TPLE as an initial treatment,
because the pharyngeal membrane of the patients who received
salvage TPLE has already been affected by initial CCRT. To the best
of our knowledge, there have been no reports concerning dysphagia
following salvage surgery, particularly salvage TPLE.
The purpose of the present study was to evaluate the
influence of CCRT on pharyngeal constriction by comparing
swallowing function between the salvage TPLE group and the initial
TPLE group, and to confirm the role of pharyngeal constriction
following TPLE.
Materials and methods
Study design and patients
The present study was a retrospective study
conducted in a single institute in the National Cancer Research
Center Hospital East (Kashiwa, Japan). The present study was
approved by the Research Ethics Committee of the National Cancer
Research Center Hospital East, and the research outline is open to
the public.
Eligible patients were those who received salvage
TPLE following CCRT or received TPLE as initial treatment for
hypopharyngeal cancer, those whose clinical records were available
and those who presented for treatment between 2008 January and 2014
May in the National Cancer Research Center Hospital East. CCRT in
the current study was defined as at least one course of
chemotherapy with >60-Gy radiation.
A total of 212 patients underwent TPLE with free
jejunal reconstruction for laryngeal cancer and hypopharyngeal
cancer between 2008 January and 2014 May in the National Cancer
Research Center Hospital East, Chiba, Japan. A total of 60 patients
were eligible for the current study, with the remaining patients
excluded because they lacked videofluorography (VF) records. A
further 6 of these 60 patients with laryngeal cancer: Glottic
cancer and subglottic cancer, were excluded as the range of
radiotherapy for glottic cancer and subglottic cancer was different
from hypopharyngeal cancer and supraglottic cancer; thus, 54
patients (48 males, 6 females; median age 66.3 years; age range,
36–81 years) with hypopharyngeal cancer were included in the
present study. Overall, 14 patients received salvage TPLE following
CCRT for recurrence or residual tumor (the salvage TPLE group), and
40 patients received TPLE as initial treatment (the TPLE group)
(Table I). The TNM stage of eligible
patients was defined by Union Against Cancer and American Joint
Committee on Cancer staging system for head and neck cancer,
seventh edition (11).
 | Table I.Chemotherapy regimens. |
Table I.
Chemotherapy regimens.
| Regimen | Patients, n |
|---|
| CDDP | 11 |
| Cetuximab | 2 |
| 5-FU + CDDP | 3 |
| Total | 16 |
Chemoradiotherapy
Chemoradiotherapy was performed for all patients in
the salvage TPLE group. The chemotherapy regimens are depicted in
Table II.
 | Table II.Patient characteristics (n=60). |
Table II.
Patient characteristics (n=60).
| Characteristic | TPLE, n | Salvage TPLE, n |
|---|
| Total | 44 | 16 |
| Sex |
|
|
| Male | 40 | 14 |
|
Female | 4 | 2 |
| Tumor site |
|
|
|
Hypopharynx | 40 | 14 |
| Larynx
(supraglottic) | 4 | 2 |
| Clinical T
classification |
|
|
| T2 | 8 | 2 |
| T3 | 9 | 7 |
| T4a | 25 | 4 |
| T4b | 2 | 1 |
| Clinical N
classification |
|
|
| N0 | 11 | 6 |
| N1 | 6 | 2 |
| N2 | 24 | 8 |
| N3 | 3 | 0 |
| Combined resection of
the oropharynxa | 13 | 1 |
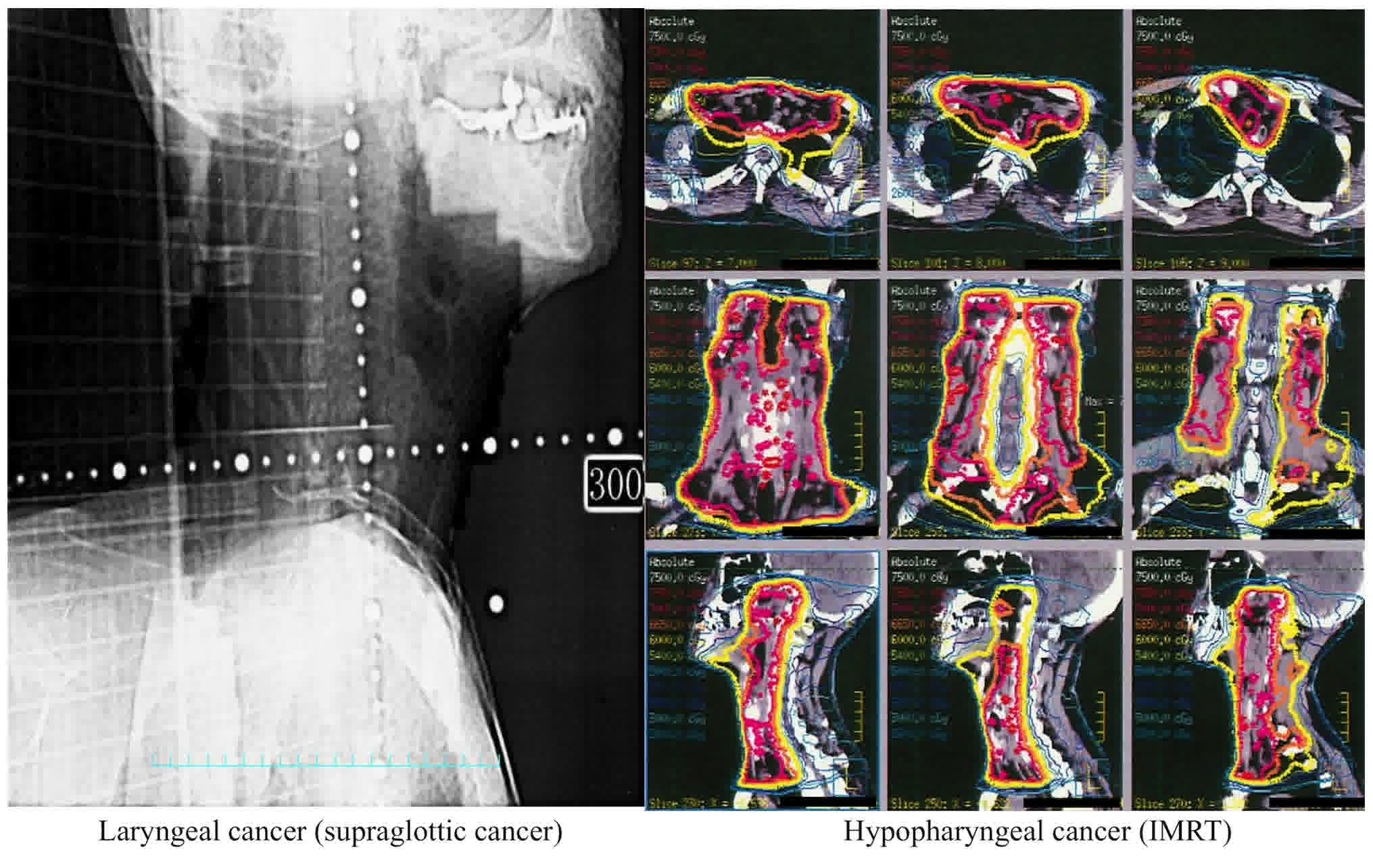
Following CT simulation in the treatment position,
the radiation dose plan was made for each individual patient. A
conventional fractionation schedule of 2 Gy/day was used. Only
patients who received a total radiation dose that was >60 Gy
were included in this study. The field of radiation is shown in
Fig. 1.
Surgery
All surgery was performed at the National Cancer
Research Center Hospital East by a single surgical team. All
patients in the present study received TPLE with free jejunal
reconstruction. With regards to primary resection, the superior
margin was set based on the degree of cancer progression. For 40
patients, the superior margin was set to over the hyoid bone, and
for the remaining 14 patients, it was set to the tonsil. The anal
side margin was also set based on cancer progression, and it was
set at the same level as tracheostomy for all patients. No patients
exhibited a tumor extension to an area lower than cervical
esophagus, and no patients required mediastinal tracheostomy.
Level 2–4 neck dissection (ND) was performed for the
bilateral neck in the TPLE group. In the salvage TPLE group, ND was
not performed. Retropharyngeal lymph node dissection was not
performed for either group.
Reconstruction surgery
Following jejunal trimming on the oral side,
pharyngojejunostomy was performed according to the Gambee technique
(12), with 4-0 absorbable
monofilament sutures. The anal side of the jejunal conduit was then
trimmed so that the jejunal graft would be pulled straight
following complete enteric anastomosis. When relaxed, the trimmed
jejunum was approximately two-thirds the length of the defect.
Jejunoesophagostomy was performed using the Gambee technique, using
4-0 absorbable monofilament sutures. Following complete enteric
anastomosis, the microscopic vascular anastomoses were established
(13).
Swallowing assessment
Swallowing was assessed by VF using a modified
barium swallow procedure (MBS). The contrast medium was 40% barium
sulfate, and a digital video recorder was used to record the images
observed from the lateral and frontal perspectives (30 frames/sec).
The MBS protocol included swallowing boluses of 5 ml of thin liquid
barium. Postoperative VF examination was performed at 7 days after
surgery in the TPLE group and at 14 days in the salvage TPLE
group.
Swallowing function was evaluated using the
pharyngeal constriction score (14),
the post-swallow pharyngeal residue rate and velopharyngeal
regurgitation on VF. Pharyngeal constriction has been proposed as a
parameter to distinguish functional from impared swallows (15–19). The
parameters for evaluation of swallowing function were then
determined, and those parameters were measured at the first swallow
in the first VF study following surgery by one investigator. The
first swallow was used to measure the parameters more easily than
the second and subsequent swallows, because there was no bolus
residue remaining from the previous examination.
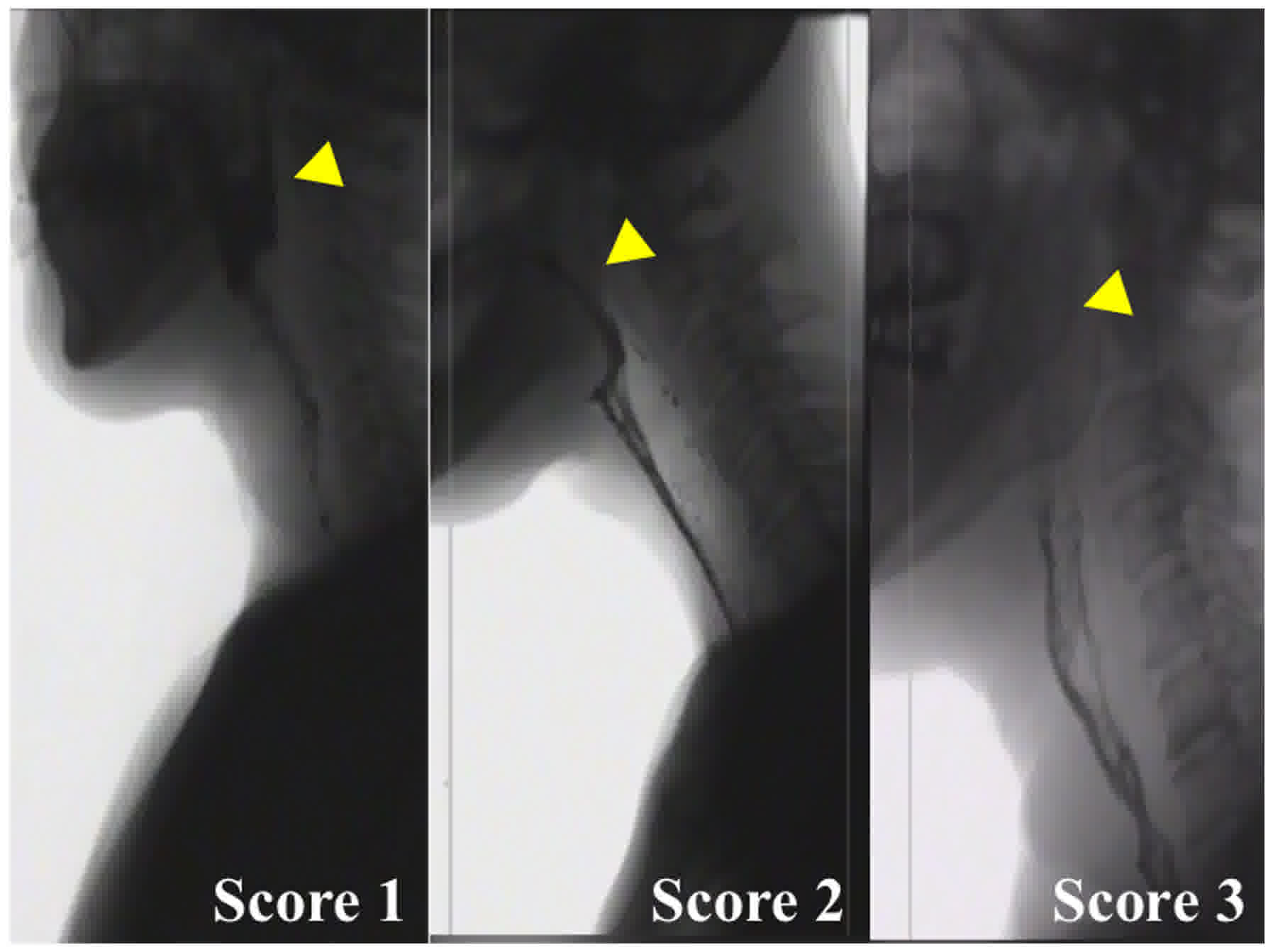
With regards to the pharyngeal constriction score,
the pharyngeal constriction ratio (PCR) is a well-established tool
for measuring and monitoring pharyngeal constriction (16). It has been validated as a surrogate
measure of strength and is associated with manometric findings
(17,20). In the present study, the pharyngeal
constriction score was determined using the VF evaluation criteria
of the Japanese Society of Dysphagia Rehabilitation (14). This score is based on the data from VF
analysis. The pharyngeal constriction score ranges from 1 to 3,
with a higher score indicating a better contact of the front and
back of the pharynx. Score 3 is normal (complete contact of the
front and back and elimination of the air space of the pharynx);
score 2 is inadequate contact of the front and back of the pharynx;
and score 1 is abnormal (no contact of the front and back of the
pharynx). In this analysis, a score of 3 was defined as normal, and
a score of 2 or 1 demonstrated that patients had constriction
disorder. VF finding criteria that are matched with the pharyngeal
constriction score are depicted in Fig.
2. The pharyngeal score was estimated based on these
criteria.
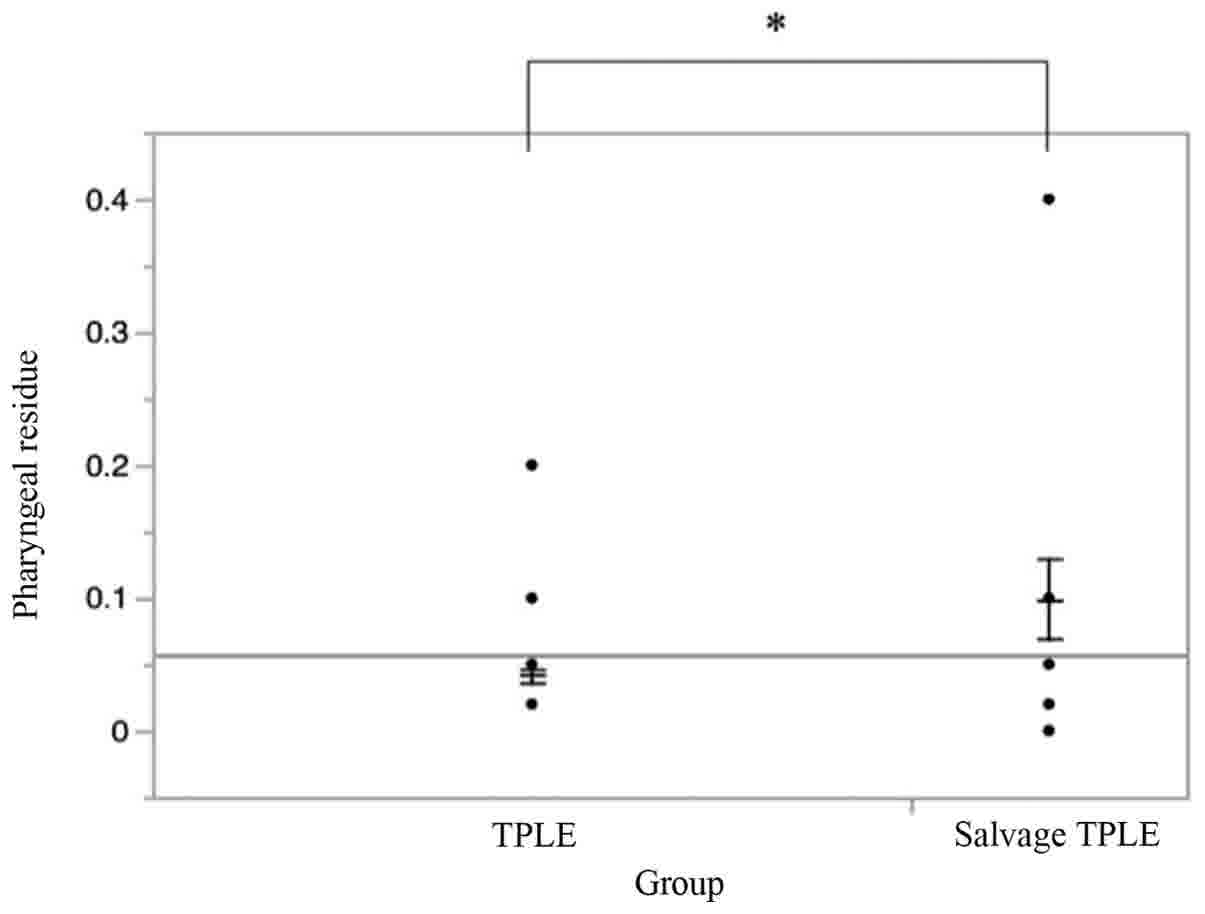
With regards to the post-swallow oropharyngeal
residue rate, the residue rate was defined as the proportion of the
oropharyngeal residue of the total bolus. The proportion of the
oropharyngeal residue was estimated by comparing the thinness of
the bolus in the oropharynx prior to and following swallowing using
the following formula: Post-swallowing oropharyngeal residue rate =
Oral-pharyngeal residue/total bolus ×100 (%) (Fig. 3). The volume of residue was measured
in the same way as the oropharyngeal swallow efficiency (OPSE).
OPSE is a global measure of swallowing function used to quantify
the interaction between the speed of bolus movement and the
safety/efficiency of the mechanism in clearing material from the
oropharynx (21).
With regards to inadequate velopharyngeal closure,
the bolus flowing backward in the velopharynx was defined as a
positive finding.
Statistical analysis
Data were analyzed to evaluate differences between
the salvage TPLE group and the TPLE group using Fisher's exact
test, Wilcoxon rank sum test and Pearson's χ test, as appropriate.
P<0.05 was considered to indicate a statistically significant
difference. All analyses were performed using JMP 11 (SAS
Institute, Inc., Cary, NC, USA).
Results
Pharyngeal constriction score
The pharyngeal constriction scores are depicted in
Table III; this score is defined in
Fig. 2, and a high score is
indicative of good constriction. In the TPLE group, 35 patients had
a score of 3 and 9 patients had a score of 2; no patients had a
score of 1. In the salvage TPLE group, 8 patients had a score of 3,
5 patients had a score of 2, and 3 patients had a score of 1.
Scores of 2 and 1 were defined as inadequate pharyngeal
constriction, and a score of 3 was defined as normal constriction.
Inadequate pharyngeal constriction was observed in 9 patients in
the TPLE group and 8 patients in the salvage TPLE group. Normal
pharyngeal constriction was observed in 35 patients in the TPLE
group and 8 patients in the salvage TPLE group. Using a Pearson's
χ2 test, the association between pharyngeal constriction
type (normal or inadequate) and surgery type (salvage or initial)
was investigated. There was a significant difference between the
TPLE group and the salvage TPLE group. The pharyngeal constriction
score was poorer in the salvage TPLE group than in the TPLE group
(P<0.05) (Table IV).
 | Table III.Pharyngeal constriction scores by
group. |
Table III.
Pharyngeal constriction scores by
group.
| Score | TPLE, n | Salvage TPLE, n |
|---|
| 3 | 35 | 8 |
| 2 | 9 | 5 |
| 1 | 0 | 3 |
 | Table IV.Comparison of pharyngeal
constriction. |
Table IV.
Comparison of pharyngeal
constriction.
| Group | Inadequate, n | Normal, n | P-value |
|---|
| TPLE | 9 | 35 | 0.0247a |
| Salvage TPLE | 8 | 8 |
|
| Total | 17 | 43 |
|
Post-swallow oropharyngeal
residue
The bolus residue rate in the oropharynx is depicted
in Fig. 4. There was a significant
difference in this rate between the TPLE group and the salvage TPLE
group using Wilcoxon rank sum test (P=0.0263). However, there were
outliers in the salvage TPLE group.
Velopharyngeal closure
The proportion of patients that experienced
inadequate velopharyngeal closure is depicted in Table V; there was no significant difference
between the TPLE group and the salvage TPLE group (P>0.99).
 | Table V.Comparison of velopharyngeal
closure. |
Table V.
Comparison of velopharyngeal
closure.
| Group | Inadequate | Normal | P-value |
|---|
| TPLE | 5 | 39 |
>0.99a |
| Salvage TPLE | 2 | 14 |
|
| Total | 7 | 53 |
|
Discussion
The present study demonstrated that pharyngeal
constriction in patients who underwent salvage TPLE was more severe
than that in patients who underwent TPLE, and that the pharyngeal
residue rate of patients who underwent salvage TPLE was higher than
that of patients who underwent TPLE.
Ward et al (22) demonstrated that there was a high
incidence of dysphagia at discharge and during long-term follow-up
in laryngectomy and pharyngolaryngectomy groups. Previous studies
have shown that the major complications of CCRT are xerostomia,
reduced mobility of the tongue base, reduced mobility of the
larynx, reduced sensitivity (incomplete protection of the airway)
and trismus (7,8). Eisbruch et al (23) demonstrated that conformal radiation
reduced the radiation dose to the pharyngeal constriction. The
present study revealed that the pharyngeal constriction scores of
the patients who underwent salvage TPLE were poorer than those of
patients who underwent TPLE. This result indicates that the adverse
effects of CCRT affect pharyngeal constriction following TPLE.
However, it is possible that the range of resection, reconstruction
method, and the scar and edema (skin and pharyngeal mucosa) from
surgery also affected swallowing function following TPLE. The
present study was retrospective, so the background characteristics
of the patients were not stratified, and other factors may also
have affected this result. Further, the current study only
evaluated the movement of the pharynx and did not evaluate
pressure. It is possible that postoperative edema also affected
this result.
With regards to pharyngeal residue, there was a
significant difference between the TPLE group and the salvage TPLE
group. The residue rate of the salvage TPLE group was higher than
that of the TPLE group. Pharyngeal constriction in the salvage TPLE
group may have been reduced by the initial CCRT treatment. However,
there were outliers in the results of the current study, which may
have affected this result. Furthermore, only the first VF
examination following surgery was evaluated. It is possible that
the residue rate may change with recovery, as the progress of
recovery may differ for each patient. Post-swallow residue should
be evaluated several times during the postoperative period.
With regards to inadequate velopharyngeal closure,
there was no significant difference between the salvage TPLE group
and the TPLE group. It was possible that the range of resection was
not suitably wide in the present study. If the upper resection
margin was over the tonsil and included soft palate resection, soft
palate movement may be limited, causing inadequate velopharyngeal
closure. In the present study, the bolus flowing backward in the
velopharynx was defined as a positive finding, so when the amount
of bolus flowing backward in the velopharynx was too small to bed
captured and objectively analyzed, the reflex may not be captured
correctly.
There were limitations to the present study. Since
the current study was retrospective, the number of patients in the
salvage TPLE group and the TPLE group may not have been adequate
for the appropriate analysis of the differences. Particularly in
the TPLE group, there were a number of ineligible patients, who
lacked VF records; thus, the present study may be biased as a
result. The quality of life of the patients was not evaluated, and
it is possible that VF findings do not associate with the
subjective perceptions of patients. Finally, the present study
measured only motor response; the pressure of constriction, and
pharyngeal and laryngeal sensation were not analyzed. In a future
study, the pressure of constriction should be evaluated directly,
and the associations between the findings of examinations and the
subjective perceptions of patients will require evaluation.
However, the results of thecurrent study indicated
the importance of pharyngeal constriction following TPLE. Stokely
et al (24) reported that
pharyngeal constriction was associated with pharyngeal residue;
however, pharyngeal constriction was not the only factor involved
in explaining pharyngeal residue. Treatments that improve
pharyngeal constriction should result in less residue. It is
possible that rehabilitation, bringing about improvements such as
reduced pharyngeal constriction, can reduce pharyngeal residue.
Thus, rehabilitation following TPLE, such as tongue-strengthening
exercises and the Masako maneuver (25) may improve swallowing function and the
patient's quality of life. Therefore, a future study should also
evaluate the effect of rehabilitation.
In conclusion, the swallowing function of patients
who underwent salvage TPLE may be affected by CCRT. Pharyngeal
constriction may be due to complications of CCRT. The results of
the current study may indicate that pharyngeal constriction has a
crucial role in swallowing ability following TPLE.
Acknowledgements
We are grateful to Dr Fujimoto (Department of
Otorhinolaryngology, Nagoya University Graduate School of Medicine)
for helpful discussions.
Funding
No funding was received.
Availability of data and materials
The datasets analyzed during the current study are
available from the corresponding author on reasonable request.
Authors' contributions
TM designed the study, and wrote the initial draft
of the manuscript. TM contributed to analysis and interpretation of
data, and assisted in the preparation of the manuscript. All other
authors contributed to data collection and interpretation, and
critically reviewed the manuscript. All authors approved the final
version of the manuscript, and agree to be accountable for all
aspects of the work in ensuring that questions related to the
accuracy or integrity of any part of the work are appropriately
investigated and resolved.
Ethics approval and consent to publish
The present study was approved by the Research
Ethics Committee of the National Cancer Research Center Hospital
East, Chiba, Japan (No. 2016-380), and the research outline is open
to the public.
Consent for publication
All patients have consented to the publication of
their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Adelstein DJ, Li Y, Adams GL, Wagner H Jr,
Kish JA, Ensley JF, Schuller DE and Forastiere AA: An intergroup
phase III comparison of standard radiation therapy and two
schedules of concurrent chemoradiotherapy in patients with
unresectable squamous cell head and neck cancer. J Clin Oncol.
21:92–98. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Forastiere AA, Goepfert H, Maor M, Pajak
TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, et
al: Concurrent chemotherapy and radiotherapy for organ preservation
in advanced laryngeal cancer. N Engl J Med. 349:2091–2098. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee SC, Shores CG and Weissler MC: Salvage
surgery after failed primary concomitant chemoradiation. Curr Opin
Otolaryngol Head Neck Surg. 16:135–140. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Esteller E, Vega MC, López M, Quer M and
León X: Salvage surgery after locoregional failure in head and neck
carcinoma patients treated with chemoradiotherapy. Eur Arch
Otorhinolaryngol. 268:295–301. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Richey LM, Shores CG, George J, Lee S,
Couch MJ, Sutton DK and Weissler MC: The effectiveness of salvage
surgery after the failure of primary concomitant chemoradiation in
head and neck cancer. Otolaryngol Head Neck Surg. 136:98–103. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Weber RS, Berkey BA, Forastiere A, Cooper
J, Maor M, Goepfert H, Morrison W, Glisson B, Trotti A, Ridge JA,
et al: Outcome of salvage total laryngectomy following organ
preservation therapy: The Radiation Therapy Oncology Group trial
91-11. Arch Otolaryngol Head Neck Surg. 129:44–49. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ozawa K, Fujimoto Y and Nakashima T:
Changes in laryngeal sensation evaluated with a new method before
and after radiotherapy. Eur Arch Otorhinolaryngol. 267:811–816.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
van der Molen L, van Rossum MA, Ackerstaff
AH, Smeele LE, Rasch CR and Hilgers FJ: Pretreatment organ function
in patients with advanced head and neck cancer: Clinical outcome
measures and patients' views. BMC Ear Nose Throat Disord. 9:102009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Crary MA and Glowasky AL: Using botulinum
toxin A to improve speech and swallowing function following total
laryngectomy. Arch Otolaryngol Head Neck Surg. 122:760–763. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Torres WE, Fibus TF, Coleman JJ III,
Clements JL Jr and Bernardino ME: Radiographic evaluation of the
free jejunal graft. Gastrointest Radiol. 12:226–230. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Edge SB, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: AJCC cancer staging manual. 7th edition.
New York, NY: Springer; 2010
|
|
12
|
Gambee LP: A single-layer open intestinal
anastomosis applicable to the small as well as the large intestine.
West J Surg Obstet Gynecol. 59:1–5. 1951.PubMed/NCBI
|
|
13
|
Sarukawa S, Sakuraba M, Kimata Y, Yasumura
T, Uchiyama K, Hishinuma S, Nakatsuka T, Hayashi R, Ebihara S and
Harii K: Standardization of free jejunum transfer after total
pharyngolaryngoesophagectomy. Laryngoscope. 116:976–981. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ueda K, Okada N, Kitazumi H, et al: VF
evaluation criteria of the Japanese Society of Dysphagia
Rehabilitation. Jap J Dysphagia Rehabil. 15:76–95. 2011.
|
|
15
|
Dejaeger E, Pelemans W, Ponette E and
Joosten E: Mechanisms involved in postdeglutition retention in the
elderly. Dysphagia. 12:63–67. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kendall KA and Leonard RJ: Pharyngeal
constriction in elderly dysphagic patients compared with young and
elderly nondysphagic controls. Dysphagia. 16:272–278. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Leonard R, Belafsky PC and Rees CJ:
Relationship between fluoroscopic and manometric measures of
pharyngeal constriction: The pharyngeal constriction ratio. Ann
Otol Rhinol Laryngol. 115:897–901. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Leonard R, Rees CJ, Belafsky P and Allen
J: Fluoroscopic surrogate for pharyngeal strength: The pharyngeal
constriction ratio (PCR). Dysphagia. 26:13–17. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yip H, Leonard R and Belafsky PC: Can a
fluoroscopic estimation of pharyngeal constriction predict
aspiration? Otolaryngol Head Neck Surg. 135:215–217. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lan Y, Xu G, Dou Z, Lin T, Yu F and Jiang
L: The correlation between manometric and videofluoroscopic
measurements of the swallowing function in brainstem stroke
patients with Dysphagia. J Clin Gastroenterol. 49:24–30. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rademaker AW, Pauloski BR, Logemann JA and
Shanahan TK: Oropharyngeal swallow efficiency as a representative
measure of swallowing function. J Speech Hear Res. 37:314–325.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ward EC, Bishop B, Frisby J and Stevens M:
Swallowing outcomes following laryngectomy and
pharyngolaryngectomy. Arch Otolaryngol Head Neck Surg. 128:181–186.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Eisbruch A, Kim HM, Feng FY, Lyden TH,
Haxer MJ, Feng M, Worden FP, Bradford CR, Prince ME, Moyer JS, et
al: Chemo-IMRT of oropharyngeal cancer aiming to reduce dysphagia:
Swallowing organs late complication probabilities and dosimetric
correlates. Int J Radiat Oncol Biol Phys. 81:e93–e99. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Stokely SL, Peladeau-Pigeon M, Leigh C,
Molfenter SM and Steele CM: The relationship between pharyngeal
constriction and Post-swallow residue. Dysphagia. 30:349–356. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Logemann JA: Treatment of oral and
pharyngeal dysphagia. Phys Med Rehabil Clin N Am. 19(803–816):
ix2008.
|