Introduction
Liposarcomas are the most common soft tissue tumors,
presenting with a variety of symptoms such as bleeding, weight loss
and abdominal pain. They are usually located in the retroperitoneal
region (1). The incidence of
retroperitoneal liposarcomas vary between 0.07 and 0.2% of all
retroperitoneal tumors, while 85% of these tumors are considered
malignant (2). A rare case of a
55-year-old female patient with a giant retroperitoneal liposarcoma
presented with dyspnea is reported in the present study.
Case report
A 55-year-old female, suffering from dyspnea and
light diffuse abdominal pain was referred to our hospital. The
symptoms had begun 2 weeks prior to admission. Her past medical
history was unremarkable. The patient was stable (blood pressure,
135/950 mmHg; heart rate, 85 beats/min; saturation, 94%; and
breathing rate, 13 breaths/min) and afebrile (36.7°C). Clinical
examination revealed distended abdomen and a palpable mass
extending from the epigastrium to the right pelvic region. The
laboratory results showed hematocrit (Hct)=31.2%, and hemoglobin
(Hgb)=10,9 g/dl.
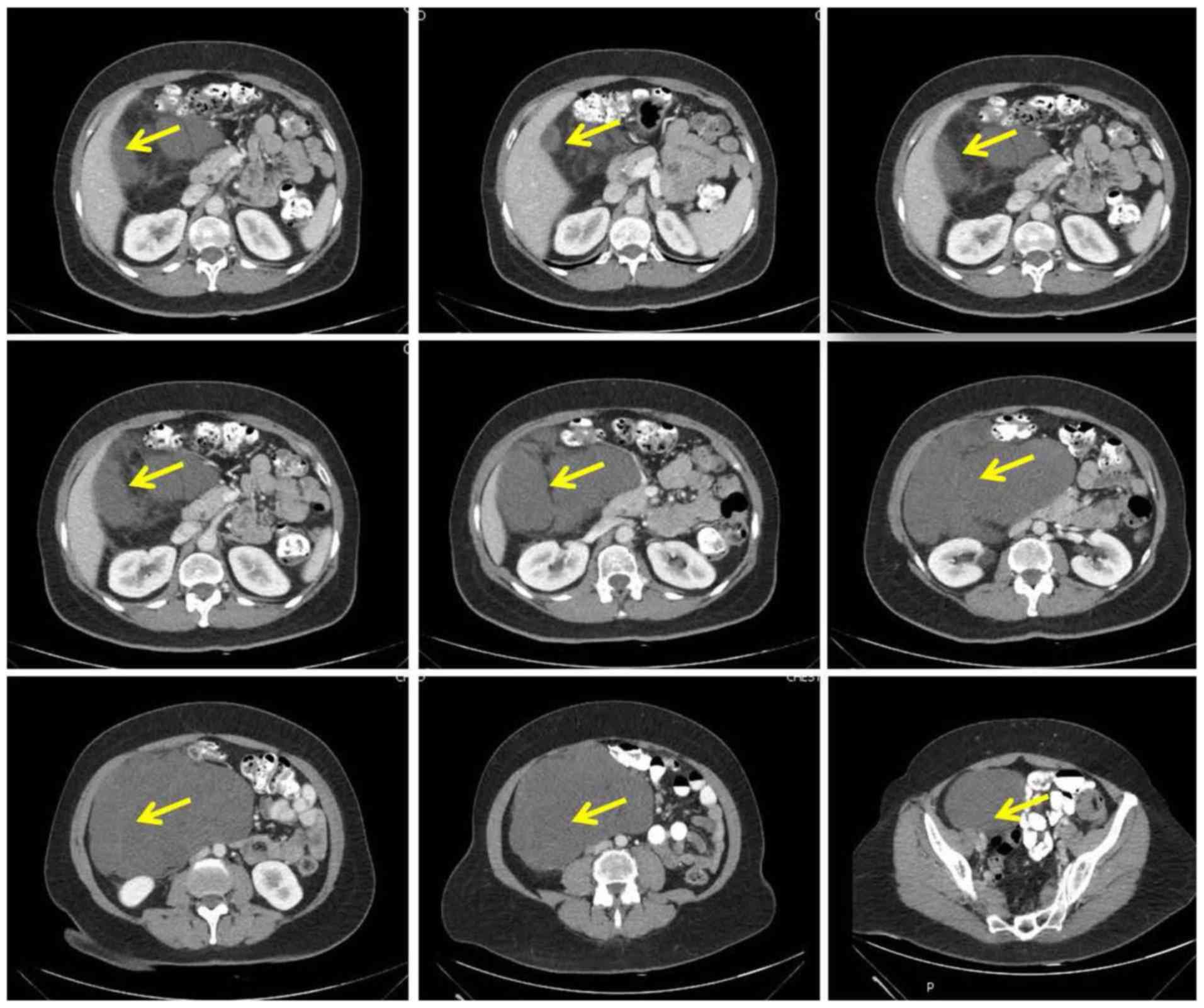
Plain X-ray views of the abdomen showed deviation of
the bowels to the left side. Further imaging with computed
tomography (CT) scan, as well as magnetic imaging resonance (MRI)
exhibited a solid mass located in the right abdomen, with its
central region not absorbing the intravenous contrast, which was
attributed to central necrosis or cystic degeneration (Fig. 1). The mass occupied the right portion
of the abdomen repulsing sections of the gastrointestinal tract,
with its upper borders to the lower edge and gate portion of the
liver and lower borders to the right ovary. The size of this mass
was calculated to be 23×19×12 cm. The position of the mass was
suppressing the anatomical structures and organs away from their
natural position. In addition, the tumor was in contact with the
right kidney, the inferior vena cava and the right renal vein
causing mild dilation of the right pelvis of the kidney. In the
pelvis, the mass was in contact with the bladder, the sigmoid
colon, as well as the right iliac vessels which were verified as
non-obstructed by the compatible intravenous contrast analysis.
There was no evidence of intra-abdominal or peritoneal
metastases.
Surgical excision of the mass was performed through
a midline incision (Fig. 2). The
patient did not suffer any postoperative complications, had an
uneventful recovery and was discharged on the 6th postoperative
day. Pathological examination revealed a well-differentiated
liposarcoma, without evidence of cellular atypia, while loose
fibrous connective tissue between the malignant cells was
observed.
The patient was followed up in the out-patient
clinic with physical examination and imaging
(chest/abdominal/pelvic CT) every 6 months for 3 years and then
annually for a total of 4 years until today.
Discussion
Retroperitoneal sarcomas are rare malignancies
accounting for approximately 15% of all sarcoma cases, while their
incidence is 0.3–0.4% per 100,000 individuals (1,2).
Liposarcomas account for approximately 40% of retroperitoneal
sarcomas making them the most common type, followed by
leiomyosarcoma and malignant fibrous histiocytoma, while it is
estimated that they comprise 0.07–0.2% of all neoplasms (3–5).
Retroperitoneal liposarcomas have a higher incidence
in the sixth and seventh decade, while the influence of sex remains
unclear (3,5). The present case was a 55-year-old
female. About 50% of cases are diagnosed when their size is over 20
cm. The reported case sought medical assistance 2 weeks after the
onset of symptoms, while the mass was already 23×19×12 cm. This is
due to the fact that the retroperitoneal region offers large spaces
for expansion and the symptomatology may present in the late stages
(3,5).
Additionally, symptoms are usually non-specific, such as flank or
abdominal pain, lower extremity swelling or pain, constipation or
urinary symptoms (3,5). The reported case suffered mainly from
dyspnea, a symptom very rarely associated with these tumors. Of
note, most retroperitoneal liposarcomas remain asymptomatic.
Liposarcomas have 5 types: Well-differentiated
liposarcoma, dedifferentiated liposarcoma, myxoid/round cell
liposarcoma, pleomorphic liposarcoma and mixed liposarcoma.
Well-differentiated and dedifferentiated liposarcomas are the most
commonly observed retroperitoneal ones, while well-differentiated
liposarcoma has 3 subtypes: Lipomatous, sclerotic and inflammatory
liposarcoma (3,6–8). The
reported case is a well-differentiated liposarcoma, which is
usually a slow-growing mass with minimum metastatic behavior.
Dedifferentiated liposarcomas are either primary or develop from a
well-differentiated one, while myxoid/round cell liposarcomas have
a high metastatic potential and are aggressive. Mixed liposarcoma
are the rarest and have a poor prognosis (3,7).
In patients suspected with retroperitoneal sarcoma a
pre-treatment biopsy is not usually performed. Retroperitoneal
masses are more likely to be liposarcomas than lipomas and
therefore it is best to surgically excise them. In patients unfit
for surgery or those who are candidates for preoperative
radiotherapy and/or chemotherapy or those with metastases a
fine-needle aspiration or core-needle biopsy should be performed.
In cases that the management would change with a definite diagnosis
and percutaneous biopsies have failed, open biopsy should be
considered (3,4).
Regarding management of these tumors, surgical
excision represents the definite treatment, while surgical
resection with negative microscopic margins is the most consistent
prognostic factor (3,9–16).
Surgical treatment of these cases is challenging, since many
structures and organs are usually involved and adipocyte
differentiation makes it difficult to distinguish the tumor from
retroperitoneal fat tissue (17).
Additionally, some cases involve unresectable vital structures or
resection could lead to increased morbidity (18). In these cases, a biopsy should be
considered and preoperative radiotherapy and/or chemotherapy should
be performed to preoperatively downstage the tumor (3). Studies evaluating the aggressive
surgical resection have reported good results with 5-year local
recurrence-free and disease-specific survival rates of 55 and 75%,
respectively (12). Due to the
potential high difficulty of these operations the open approach is
usually preferred. In the reported patient an open approach with
midline incision was performed and the tumor was resected with
negative microscopic margins (19).
Recurrence of these tumors usually occurs within 6
months to 2 years following surgical excision with local recurrence
being much more common than distant metastases. Five-year local
recurrence rates following complete macroscopic resection are
approximately 50% for well-differentiated retroperitoneal
liposarcomas. Early diagnosed and operated recurrences have
complete excision rates in approximately 90% of cases (20). Therefore, it is crucial to regularly
follow up these patients with imaging, such as CT scan and/or MRI
(21). It is recommended that
patients with low-grade retroperitoneal soft-tissue sarcomas,
successfully treated with surgical resection, should have a
follow-up physical examination with imaging (chest/abdominal/pelvic
CT) every 3 to 6 months for 2 to 3 years, then annually, while for
those with high-grade sarcoma, successfully treated with surgical
resection, a follow-up physical examination with imaging
(chest/abdominal/pelvic CT) every 3 to 6 months for 2 to 3 years,
then every 6 months for the next 2 years, and then annually is
recommended. The present patient has been followed up (4 years
now), according to this protocol, without any signs of recurrence
up-to-date (22).
In conclusion, retroperitoneal sarcomas are
relatively rare tumors that represent a surgical challenge.
Surgical resection with negative microscopic margins is the
definite treatment. It is of note that the symptomatology is
non-specific. The reported patient presented with dyspnea,
something extremely rare and not usually reported in the
literature. It is therefore crucial for the physician to perform a
thorough physical examination and to keep a keen eye for cases such
as this.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AI and CK were involved in the conception of the
study. AI, MK and SA performed the review. AI, NM and KK analyzed
and interpreted the data. AI, MK and KK wrote the manuscript. NM
and KK critically revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Consent for publication
The patient provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mettlin C, Priore R, Rao U, Gamble D, Lane
W and Murphy P: Results of the national soft-tissue sarcoma
registry. J Surg Oncol. 19:224–227. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Herrera-Gómez A, Ortega-Gutiérrez C,
Betancourt AM and Luna-Ortiz K: Giant retroperitoneal liposarcoma.
World J Surg Oncol. 6:1152008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vijay A and Ram L: Retroperitoneal
liposarcoma: A comprehensive review. Am J Clin Oncol. 38:213–219.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Das Gupta TK: Tumors and tumor-like
conditions of the adipose tissue. Curr Probl Surg. 7:1–60. 1970.
View Article : Google Scholar
|
|
5
|
Chouairy CJ, Abdul-Karim FW and MacLennan
GT: Retroperitoneal liposarcoma. J Urol. 177:11452007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hosaka A, Masaki Y, Yamasaki K, Aoki F,
Sugizaki K and Ito E: Retroperitoneal mixed-type liposarcoma
showing features of four different subtypes. Am Surg. 74:1202–1205.
2008.PubMed/NCBI
|
|
7
|
Sheffield BS and Nielsen TO: Myxoid
liposarcoma in a 91-year-old patient. Mol Cytogenet. 6:502013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fritz B, Schubert F, Wrobel G, Schwaenen
C, Wessendorf S, Nessling M, Korz C, Rieker RJ, Montgomery K,
Kucherlapati R, et al: Microarray-based copy number and expression
profiling in dedifferentiated and pleomorphic liposarcoma. Cancer
Res. 62:2993–2998. 2002.PubMed/NCBI
|
|
9
|
Lewis JJ, Leung D, Woodruff JM and Brennan
MF: Retroperitoneal soft-tissue sarcoma: Analysis of 500 patients
treated and followed at a single institution. Ann Surg.
228:355–365. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee SY, Goh BK, Teo MC, Chew MH, Chow PK,
Wong WK, Ooi LL and Soo KC: Retroperitoneal liposarcomas: The
experience of a tertiary Asian center. World J Surg Oncol. 9:12–17.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bonvalot S, Rivoire M, Castaing M,
Stoeckle E, Le Cesne A, Blay JY and Laplanche A: Primary
retroperitoneal sarcomas: A multivariate analysis of surgical
factors associated with local control. J Clin Oncol. 27:31–37.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Strauss DC, Hayes AJ, Thway K, Moskovic
EC, Fisher C and Thomas JM: Surgical management of primary
retroperitoneal sarcoma. Br J Surg. 97:698–706. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
van Dalen T, Plooij JM, van Coevorden F,
van Geel AN, Hoekstra HJ, Albus-Lutter Ch, Slootweg PJ and
Hennipman A: Dutch Soft Tissue Sarcoma Group: Long-term prognosis
of primary retroperitoneal soft tissue sarcoma. Eur J Surg Oncol.
33:234–238. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Alldinger I, Yang Q, Pilarsky C, Saeger
HD, Knoefel WT and Peiper M: Retroperitoneal soft tissue sarcomas:
Prognosis and treatment of primary and recurrent disease in 117
patients. Anticancer Res. 26(2B): 1577–1581. 2006.PubMed/NCBI
|
|
15
|
Erzen D, Sencar M and Novak J:
Retroperitoneal sarcoma: 25 years of experience with aggressive
surgical treatment at the Institute of Oncology, Ljubljana. J Surg
Oncol. 91:1–9. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Singer S, Corson JM, Demetri GD, Healey
EA, Marcus K and Eberlein TJ: Prognostic factors predictive of
survival for truncal and retroperitoneal soft-tissue sarcoma. Ann
Surg. 221:185–195. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Elias A, Ryan L, Sulkes A, Collins J,
Aisner J and Antman KH: Response to mesna, doxorubicin, ifosfamide,
and dacarbazine in 108 patients with metastatic or unresectable
sarcoma and no prior chemotherapy. J Clin Oncol. 7:1208–1216. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shibata D, Lewis JJ, Leung DH and Brennan
MF: Is there a role for incomplete resection in the management of
retroperitoneal liposarcomas? J Am Coll Surg. 193:373–379. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shalhav AL, Chan SW, Bercowsky E,
Elbahnassy AM, McDougall EM and Clayman RV: Laparoscopic
exploration in the management of retroperitoneal masses. JSLS.
3:209–214. 1999.PubMed/NCBI
|
|
20
|
Kim EY, Kim SJ, Choi D, Lee SJ, Kim SH,
Lim HK and Song SY: Recurrence of retroperitoneal liposarcoma:
Imaging findings and growth rates at follow-up CT. AJR Am J
Roentgenol. 191:1841–1846. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Song T, Shen J, Liang BL, Mai WW, Li Y and
Guo HC: Retroperitoneal liposarcoma: MR characteristics and
pathological correlative analysis. Abdom Imaging. 32:668–674. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
NCCN: Clinical Practice Guidelines in
Oncology. http://www.nccn.org/professionals/physician_gls/PDF/sarcoma.pdfApril
8–2018
|