Introduction
Lung cancer has the highest incidence rate of all
cancer types and is the leading cause of cancer-related mortality
worldwide. Non-small cell lung cancer (NSCLC) accounts for
approximately 85% of all lung cancer (1). Advanced-stage NSCLC is mainly treated
with platinum-based combination treatment. The 5-year survival rate
for this treatment is less than 15%. Many advanced NSCLC patients
with a poor general condition often cannot tolerate chemotherapy or
are unwilling to undergo chemotherapy. Targeted therapy is a new
technique for cancer treatment, and brings hope for advanced-stage
NSCLC patients.
Breakthrough treatments using epidermal growth
factor receptor tyrosine kinase inhibitors (EGFR-TKI), including
gefitinib, are often used as a second- or third-line lung cancer
treatment. This type of drug therapy is currently being considered
as a first-line treatment option. However, results from the INTACT
and TRIBUTE trials (2–4), which combined EGFR-TKI with typical
first-line treatment regimes, did not provide evidence of any
survival benefit from EGFR-TKI treatment. Thus, studies are now
underway to identify patient populations that may benefit from this
targeted therapy as a first-line treatment.
Results from the IPASS study (5) marked gefitinib as a first-line
treatment of NSCLC and opened a new era for cancer treatment.
Compared to chemotherapeutics, gefitinib significantly elongated
the progression-free survival (PFS) of patients with mutated
EGFR genes, greatly improved safety of the treatment, and
improved the quality of the life of the patients. Therefore,
gefitinib is likely to become a new standard first-line treatment
for NSCLC patients with mutated EGFR genes. Even when the
EGFR status of patients is unknown, the demographic and clinical
characteristics of patients may be used to determine which patients
have a relatively high chance of benefiting from EGFR-TKI treatment
as the first-line treatment strategy. In 2010, gefitinib was
approved by the State Food and Drug Administration of China as a
first-line treatment for locally advanced or metastatic NSCLC in
patients with mutated EGFR-TK, as these patients are sensitive to
gefitinib treatment.
The aim of this study was to determine the efficacy
and safety of gefitinib as the first-line treatment for 68 patients
with advanced NSCLC.
Patients and methods
Patients
Between September 2007 and August 2010, a total of
68 NSCLC patients who were admitted to the Shanghai Chest Hospital,
Shanghai, China were recruited into the study. The patients had
advanced-stage (IIIB-IV, not resectable) NSCLC and had not received
any chemotherapy. Diagnoses were confirmed by bronchoscopy or
CT-guided lung biopsy. Patient clinical data were collected. Of the
68 patients, 20 were male and 48 were female, with the patient age
ranging from 40 to 88 years, with a median age of 71 years. Among
the participants, 50 patients were smokers and 18 were non-smokers.
Of the 68 patients, 60 were diagnosed with adenocarcinoma, 6 with
squamous cell carcinoma and 2 with adenosquamous carcinoma. There
were 6 patients with stage IIIB cancer and 62 with stage IV cancer.
For 13 patients, the Eastern Cooperative Oncology Group Performance
Status (ECOG PS) scores were between 0 and 1, and 55 patients had
scores ≥2. All 68 patients had at least one measurable tumor that
was regularly evaluated using CT or MRI. Blood, urine and kidney
function were regularly monitored through routine tests. The
patients received a re-evaluation every 2 months. The last
follow-up was performed on September 30, 2011.
This study was approved by the institutional review
board of the Chest Hospital and written informed consent was
obtained from every participant.
Treatment
Patients received 250 mg/day gefitinib orally
(AstraZeneca) until the disease progressed or intolerable toxicity
occurred.
Efficacy criteria and observed
parameters
Efficacy was evaluated using the Response Evaluation
Criteria in Solid Tumors (RECIST) 1.1 for solid tumors (6). Each patient experienced either a
complete response (CR), partial response (PR) or achieved stable
disease (SD) or progressive disease (PD). The response rate (RR)
was calculated using the formula: RR = CR+PR. The disease control
rate (DCR) was calculated as DCR = CR+PR+SD. Toxicity was evaluated
according to the standard for adverse reactions (grades 1–4) issued
by the National Cancer Institute of the USA (7). Efficacy evaluations were performed
every 4 weeks, beginning 4 weeks following the initiation of
treatment. Efficacy evaluations were also performed when new
symptoms developed or existing symptoms worsened. PFS was defined
as the time from the first drug administration to the time that
evidence confirmed disease progression. The overall survival (OS)
of a patient was defined as the time from the first day of oral
gefitinib administration to the day the patient succumbed to the
disease or the day of the patient’s last follow-up visit.
Performance status was scored using the ECOG PS system.
Statistical analysis
The data were analyzed with SPSS 13.0 software.
Differences between the groups were tested using the χ2
test and the survival rates were tested using the log-rank test.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Short-term efficacy
Among the 68 patients, 1 patient experienced CR
(1.5%), 23 experienced PR (33.8%), 29 achieved SD (42.6%) and 15
achieved PD (22.1%). The RR was 35.3% (24/68) and the DCR was 77.9%
(53/68). No correlation was found between gender, age, ECOG score,
pathology or smoking status and patient RR (P>0.05). However,
DCR was significantly higher for adenocarcinoma patients, females
and non-smoking patients compared to non-adenocarcinoma, males and
smoking patients (P<0.05; Table
I).
 | Table ICharacteristics and response rates of
68 NSCLC patients undergoing gefitinib therapy. |
Table I
Characteristics and response rates of
68 NSCLC patients undergoing gefitinib therapy.
| Characteristics | n | PR | SD | PD | RR (%) | P-value | DCR (%) | P-value |
|---|
| Gender |
| Male | 20 | 5 | 7 | 8 | 25.0 | 0.251 | 60.0 | 0.047 |
| Female | 48 | 19 | 22 | 7 | 39.6 | | 85.4 | |
| Age (years) |
| <70 | 33 | 11 | 17 | 5 | 33.3 | 0.742 | 84.8 | 0.182 |
| ≥70 | 35 | 13 | 12 | 10 | 37.1 | | 71.4 | |
| ECOG score |
| 0–1 | 13 | 5 | 7 | 1 | 38.5 | 0.954 | 92.3 | 0.309 |
| ≥2 | 55 | 19 | 22 | 14 | 34.5 | | 74.5 | |
| Histology |
| Adenocarcinoma | 60 | 23 | 28 | 9 | 38.3 | 0.297 | 85.0 | 0.001 |
|
Non-adenocarcinoma | 8 | 1 | 1 | 6 | 12.5 | | 25.0 | |
| Smoker |
| No | 50 | 19 | 25 | 6 | 38.0 | 0.436 | 88.0 | 0.003 |
| Yes | 18 | 5 | 4 | 9 | 27.8 | | 50.0 | |
Survival
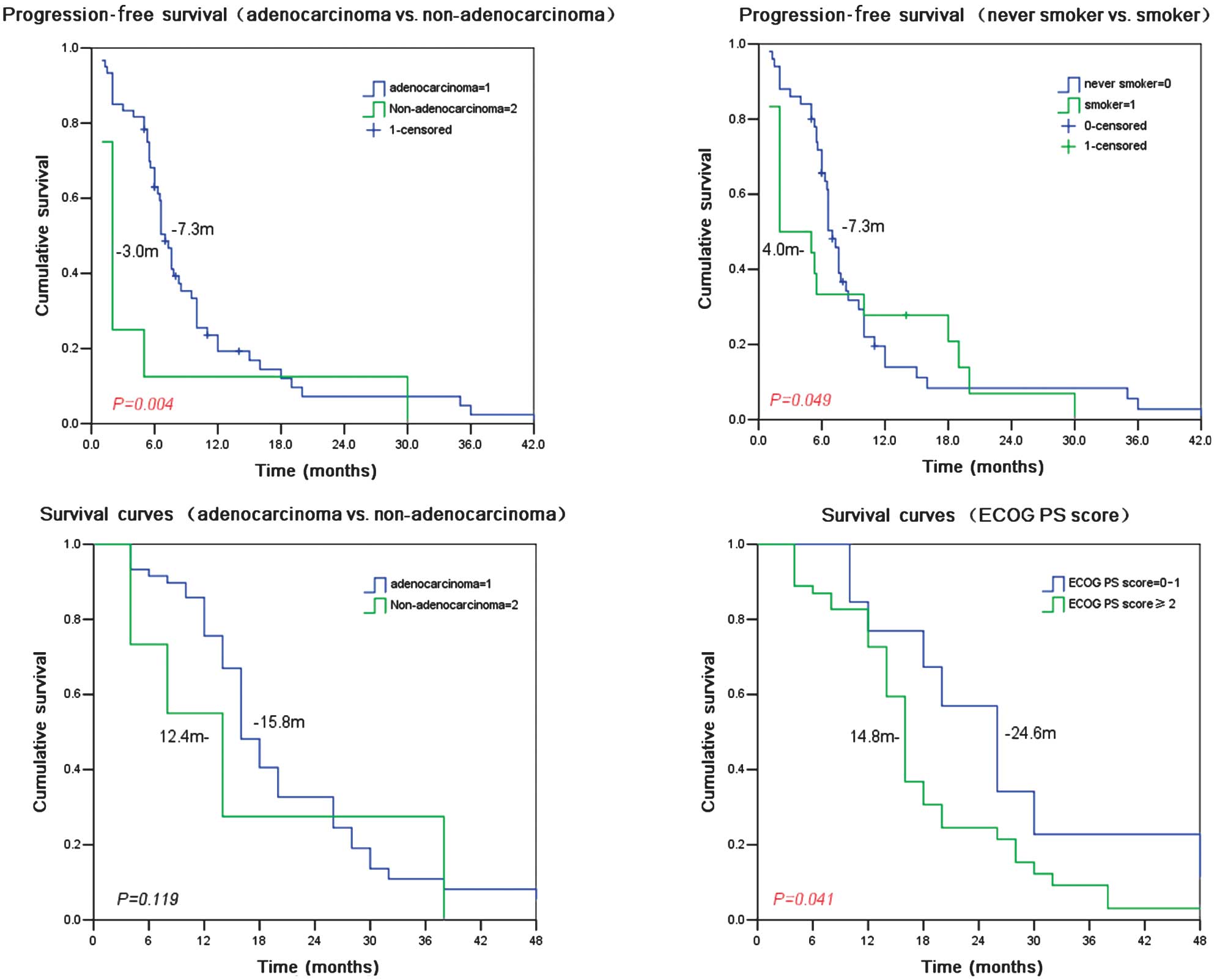
The median PFS was 6.6 months (95% CI 5.84–7.36
months), the median survival time (MST) was 15.5 months (95% CI
13.56–17.44 months), and the one-year survival rate was 55.8%.
Treatment with gefitinib resulted in a longer median PFS in the
adenocarcinoma patients compared to the non-adenocarcinoma patients
(7.3 vs. 3.0 months, P=0.004) and in the non-smokers compared to
the smokers (7.3 vs. 4.0 months, P=0.049). With gefitinib
treatment, the MST for patients with ECOG 0–1 was longer than that
for patients with ECOG ≥2 (24.6 vs. 14.8 months, P=0.041). No other
recorded parameters, including gender, age, pathology and history
of smoking were significantly correlated with patient MST (Table II and Fig. 1).
 | Table IICharacteristics and survival of 68
NSCLC patients undergoing gefitinib therapy. |
Table II
Characteristics and survival of 68
NSCLC patients undergoing gefitinib therapy.
| Characteristics | n | Mean PFS
(months) | P-value | MST (months) | P-value |
|---|
| Gender |
| Male | 20 | 5.0 | 0.102 | 15.7 | 0.722 |
| Female | 48 | 7.2 | | 15.5 | |
| Age (years) |
| <70 | 33 | 7.5 | 0.177 | 19.2 | 0.067 |
| ≥70 | 35 | 6.1 | | 14.8 | |
| ECOG PS score |
| 0–1 | 13 | 7.0 | 0.388 | 24.6 | 0.041 |
| ≥2 | 55 | 6.9 | | 14.8 | |
| Histology |
| Adenocarcinoma | 60 | 7.3 | 0.004 | 15.8 | 0.119 |
|
Non-adenocarcinoma | 8 | 3.0 | | 12.4 | |
| Smoker |
| No | 50 | 7.3 | 0.049 | 15.6 | 0.419 |
| Yes | 18 | 4.0 | | 14.7 | |
Toxicity and side effects
The most common side effect was a rash that occurred
in 47 cases (69.1%). Rashes primarily occurred on the face, chest,
back, hands and feet. The rashes were mainly red pimples or
acne-like rashes with or without itching. Few patients experienced
skin ulceration. The majority of the rashes were resolved without
treatment, but new rashes occasionally appeared. The second most
common side effect was mild diarrhea (25 cases, 36.8%), which was
alleviated by symptomatic treatment. Anorexia was encountered in 14
cases (20.6%), pruritus in 12 cases (17.6%), dry skin in 11 cases
(16.2%) and oral ulcers in 8 cases (11.2%). Abnormal liver function
developed in 4 cases (5.9%), but returned to normal following
temporary withdrawal of gefitinib therapy and administration of
liver function-protecting treatment for 1 week. A small number of
patients experienced mild nausea or anorexia that improved
following symptomatic treatment. No bone marrow suppression or
renal damage was observed. There were 2 patients who developed a
cough and chest tightness. CT scans of these patients indicated
interstitial lung disease (ILD) and the symptoms improved following
ILD treatment (Table III).
 | Table IIIAdverse events among 68 NSCLC patients
undergoing gefitinib therapy. |
Table III
Adverse events among 68 NSCLC patients
undergoing gefitinib therapy.
| Adverse event | No. of cases (%) | CTC grade 3 or 4 no.
(%) |
|---|
| Rash | 47 (69.1) | 2 (2.9) |
| Diarrhea | 25 (36.8) | 0 |
| Dry skin | 11 (16.2) | 0 |
| Anorexia | 14 (20.6) | 1 (1.5) |
| Pruritus | 12 (17.6) | 0 |
| Stomatitis | 8 (11.2) | 0 |
| Abnormal liver
function | 4 (5.9) | 0 |
| Nausea | 3 (4.4) | 0 |
| Vomiting | 2 (2.9) | 0 |
| Constipation | 2 (2.9) | 0 |
| Alopecia | 1 (1.5) | 0 |
Discussion
Recently, molecular therapy targeting the EGFR has
received a lot of attention from oncologists. One such therapy, the
EGFR-TKI gefitinib (Iressa), has been approved in a number of
countries for the treatment of advanced NSCLC (8).
A number of previous studies (9–11) have
indicated the safety and effectiveness of gefitinib for the
treatment of advanced NSCLC that did not respond to platinum-based
chemotherapy. Gefitinib is gaining popularity as a first-line
treatment for NSCLC. However, the INTACT and TRIBUTE studies
(2–4), which combined EGFR-TKI and first-line
chemotherapies, did not find any survival benefit for EGFR-TKI
therapy. Thus, the focus was on the subpopulations that may respond
well to first-line EGFR-targeting therapy. Recently, a number of
studies have indicated that EGFR mutation status is key in
determining the efficacy of EGFR-TKI (13). EGFR has a relatively high frequency
of mutations in adenocarcinoma patients, non-smokers, females and
Asians, who therefore comprise the potential target population of
first-line EGFR-TKI treatment.
Publication of data from the Iressa Pan-Asia Study
(IPASS) in 2008 (5) was a landmark
for NSCLC treatment with gefitinib. In a randomized open-label
phase III clinical trial, 1217 stage IIIB/IV Asian NSCLC patients
received either gefitinib (609 patients) or carboplatin and
paclitaxel (CP) (608 patients) as first-line treatment. Following
22 months of follow-up, gefitinib-treated patients had a
significantly higher PFS than CP-treated patients (HR=0.741,
P<0.0001). In addition, the gefitinib group showed improvement
in other factors compared to the CP group, including the objective
response rate (ORR) (43.0 vs. 32.2%, P=0.0001), treatment
tolerability and quality of life. Stratified analysis of molecular
markers revealed that CP treatment was similarly effective for
patients with wild-type and mutant EGFR, whereas gefitinib produced
an improved PFS compared to chemotherapy only in patients with
mutant EGFR. Notably, 40% of patients with wild-type EGFR who
received gefitinib treatment had a significantly higher risk of
disease progression compared to those with mutated EGFR. However,
the OS curve of the CP treatment overlapped with that of the
first-line targeting therapy, and there was no significant
difference between the median OS of the 2 groups. A similarly
designed study, FIRST-SIGNAL, confirmed the results of IPASS.
Although EGFR-TKI is more useful compared to other
types of therapy as a first-line treatment, depending on the
ethnicity, pathology and smoking history of recipients, EGFR-TKI
treatment also carries an increased risk of disease progression for
patients with wild-type EGFR. Results from the IPASS and the
FIRST-SIGNAL studies suggested that EGFR-TKI produces a total OS
comparable to that of chemotherapy when restricted to appropriate
populations. Neither of these 2 first-line strategies, however, is
clearly advantageous compared to the other (12,13).
In this study, 88.2% of the 68 advanced NSCLCs were
adenocarcinomas. In the gefitinib group, the RR was 35.3%, the DCR
was 77.9%, the median PFS was 6.6 months, the MST was 15.5 months,
and the 1-year survival rate was 55.8%. A stratified analysis
indicated that the DCRs for the adenocarcinoma patients, females
and non-smokers were significantly higher than those of the
non-adenocarcinoma patients, males and smokers (all P<0.05). The
survival analysis demonstrated that the PFS of the adenocarcinoma
patients was longer than that of the non-adenocarcinoma patients
(7.3 vs. 3.0 months, P=0.004), and that the median PFS of the
non-smokers was longer than that of the smokers (7.3 vs. 4.0
months, P=0.049). The MST of the patients with ECOG 0–1 was
improved compared to that of patients with ECOG ≥2 (24.6 months vs.
14.8 months, P=0.041). Gender, age, pathology and smoking history
were not significantly correlated with MST.
In this study, a number of the patients were elderly
(≥70 years of age), and some of them suffered from cardiovascular
or endocrine diseases. Therefore, these patients had a relatively
low tolerance to routine chemotherapy. Additionally, certain older
patients were reluctant to receive chemotherapy. Gefitinib may be a
good alternative as a first-line treatment for these patients,
producing similar outcomes to the standard platinum-based treatment
regimes. Gefitinib was, to certain extent, an effective treatment
for the brain metastasis of lung cancer. In 3 of the 8 patients
with brain metastasis, MRI indicated reduced tumor size in the
brain 3 months following a 2-month course of gefitinib treatment.
Moreover, a number of symptoms, including headache, dizziness and
limb movement disorder were markedly improved.
The main adverse reactions to gefitinib treatment
were rash and diarrhea; these were mostly reversible grade I-II
reactions. Four patients developed abnormal liver function, which
returned to normal following 1 week of liver-protecting treatment;
these patients then resumed gefitinib treatment. The most serious
toxic effect of gefitinib was interstitial lung disease (ILD). In
this study, 2 patients suffered from cough and chest tightness, and
ILD was suspected after chest CT scans were performed. These 2
patients improved following symptomatic treatment. Therefore,
withdrawal of gefitinib therapy is recommended when ILD occurs.
In conclusion, gefitinib is effective for the
treatment of advanced NSCLC patients, as it has minor adverse
effects and is well-tolerated. Patients do not require
hospitalization for this treatment. For patients who cannot
tolerate or who are reluctant to receive chemotherapy, gefitinib is
able to improve symptoms and quality of life, as well as provide a
survival benefit, particularly for female patients, patients with
adenocarcinoma and non-smokers.
Acknowledgements
This study was supported by the Shanghai Science and
Technology Research Program (10140902402).
References
|
1
|
Siegel R, Ward E, Brawley O and Jemal A:
Cancer statistics: the impact of eliminating socioeconomic and
racial disparities on premature cancer deaths. CA Cancer J Clin.
61:212–236. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Giaccone G, Herbst RS, Manegold C, et al:
Gefitinib in combination with gemcitabine and cisplatin in advanced
non-small-cell lung cancer: a phase III trial - INTACT 1. J Clin
Oncol. 22:777–784. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Herbst RS, Giaccone G, Schiller JH, et al:
Gefitinib in combination with paclitaxel and carboplatin in
advanced non-small-cell lung cancer: a phase III trial - INTACT 2.
J Clin Oncol. 22:785–794. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Herbst RS, Prager D, Hermann R, et al:
TRIBUTE: a phase III trial of erlotinib hydrochloride (OSI-774)
combined with carboplatin and paclitaxel chemotherapy in advanced
non-small-cell lung cancer. J Clin Oncol. 23:5892–5899. 2005.
View Article : Google Scholar
|
|
5
|
Mok TS, Wu YL, Thongprasert S, et al:
Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N
Engl J Med. 361:947–957. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Eisenhauer EA, Therasse P, Bogaerts J, et
al: New response evaluation criteria in solid tumours: revised
RECIST guideline (version 1.1). Eur J Cancer. 45:228–247. 2009.
View Article : Google Scholar
|
|
7
|
Wiffen P, Mitchel M, Snelling M and Stoner
N: Oxford Handbook of Clinical Pharmacy. Oxford University Press;
New York: 2007
|
|
8
|
Gaughan EM and Costa DB: Genotype-driven
therapies for non-small cell lung cancer: focus on EGFR, KRAS and
ALK gene abnormalities. Ther Adv Med Oncol. 3:113–125. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fukuoka M, Yano S, Giaccone G, et al:
Multi-institutional randomized phase II trial of gefitinib for
previously treated patients with advanced non-small-cell lung
cancer (The IDEAL 1 Trial) [corrected]. J Clin Oncol. 21:2237–2246.
2003.
|
|
10
|
Kris MG, Natale RB, Herbst RS, et al:
Efficacy of gefitinib, an inhibitor of the epidermal growth factor
receptor tyrosine kinase, in symptomatic patients with non-small
cell lung cancer: a randomized trial. JAMA. 290:2149–2158. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chang A, Parikh P, Thongprasert S, et al:
Gefitinib (IRESSA) in patients of Asian origin with refractory
advanced non-small cell lung cancer: subset analysis from the ISEL
study. J Thorac Oncol. 1:847–855. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lee J, Park K, Kim S, et al: A randomized
phase III study of gefitinib versus standard chemotherapy
(gemcitabine plus cisplatin) as a first-line treatment for
never-smokers with advanced or metastatic adenocarcinoma of the
lung. J Thorac Oncol. 4:S2832009.
|
|
13
|
Maemondo M, Inoue A, Kobayashi K, et al:
Gefitinib or chemotherapy for non-small-cell lung cancer with
mutated EGFR. N Engl J Med. 362:2380–2388. 2010. View Article : Google Scholar : PubMed/NCBI
|