Introduction
Osteosarcoma (OS) is the most prevalent form of
aggressive primary malignant bone tumor with a high tendency to
metastasize to the lung and occurs mainly in children and
adolescents (1). Current optimal
treatment consists of systemic multi-agent chemotherapy and
surgical resection. The prognosis of OS patients has been markedly
improved with the current optimal treatment. However, cases with
metastases or an unresectable tumor have a poor prognosis.
Therefore, there is a strong demand for early diagnosis and an
improved therapeutic approach, which requires a comprehensive
understanding of the molecular and cellular mechanisms of the
disease. Human fibroblast activation protein (FAP, or seprase) is a
170-kDa homodimeric glycoprotein consisting of two 97-kDa subunits.
FAP is an integral transmembrane protein belonging to the prolyl
peptidase family with gelatinase and collagenase activity (2,3). Human
FAP gene is located on chromosome 2q23 and the 760-aa FAP protein
shows 48% sequence identity with dipeptidyl peptidase 4 (DPP-IV).
FAP is expressed by reactive stromal fibroblasts in >90% of
common types of human epithelial cancer, in the granulation tissue
of healing wounds and in bone and soft tissue sarcomas (4–6). FAP
and DPP-IV are known to form a hetero-oligomer in a proteolytic
complex, which is involved in the invasion of tumor cells in
collagenous matrices (7).
Increasing evidence has suggested that the expression of the
membrane-bound FAP in various solid tumors is associated with tumor
growth and invasion and poor prognosis (2,8–12).
This makes FAP an attractive subject when seeking a tumor biomarker
or a potential therapeutic target for the disease (13). To date, the function of FAP in OS
cells and implication in the disease progression remain
unknown.
The current study sought to investigate the
expression of FAP in OS cell lines and examine the association of
this molecule with OS cell function. A FAP-knockdown cell model
using hammerhead ribozymes was used to study the function of FAP
in vitro.
Materials and methods
Immunohistochemical staining of FAP
Immunohistochemistry staining method of
avidin-biotin complex (ABC) was used to test the protein expression
of FAP in tissue sections. Paraffin samples of OS bone tissues
(n=13) were sectioned (6-μm thick) and dewaxed using a series of
gradient alcohol washes. Endogenous peroxidase activity was blocked
with 0.3% hydrogen peroxide for 15 min prior to washes. Sections
were then boiled, in a microwave, in antigen retrieval solution (pH
6.0) to retrieve antigen. Following washing in Tris-buffered saline
(TBS) three times, the horse serum (Vector Laboratories, Ltd.,
Peterborough, UK) was added and the sections were incubated at room
temperature for 30 min. The primary antibody (mouse anti-human FAP;
1:100; Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA),
secondary antibody (multilink swine anti-mouse immunoglobulin) and
ABC (Vector Laboratories, Ltd.) were added successively with 30, 30
and 45 min of incubation, respectively, and three TBS washes were
performed in between. Absence of the primary antibody was used as a
negative control. Diaminobenzidine chromogen (Vector Laboratories,
Ltd.) was added to the sections and incubated in the dark for 5
min. Sections were then counterstained in Gill’s hematoxylin and
dehydrated in ascending grades of methanol prior to clearing in
xylene and mounting under a cover slip. Monoclonal mouse FAPα
(ss-13; sc-100528) and anti-GAPDH (sc-32233) were obtained from
Santa Cruz Biotechnology, Inc. Peroxidase-conjugated anti-mouse was
purchased from Sigma-Aldrich (Poole, UK).
Cell culture
OS cell lines, HOS and MG-63, were purchased from
the European Collection of Animal Cell Cultures (Salisbury, UK).
The cells were routinely cultured in Dulbecco’s modified Eagle’s
medium/Ham’s F12 with L-Glutamine medium (PAA Laboratories, Yeovil,
UK), supplemented with the antibiotics, penicillin and streptomycin
and 10% fetal calf serum (PAA Laboratories) and incubated at
37.0°C, 5% CO2 and 95% humidity.
Generation of FAP knockdown in OS cell
lines
Anti-human FAP hammerhead ribozymes were designed
based on the structure of FAP mRNA, generated using the Zuker RNA
mFold program (14). The ribozymes
were synthesized and cloned into a pEF6/V5-His-TOPO plasmid vector
(Invitrogen Life Technologies, Paisley, UK). Ribozyme transgenes
and empty pEF6 control plasmids were transfected into HOS and MG-63
cells individually, according to a previously reported procedure
(15,16). Following transfection and
blasticidin (5 μg/ml) selection, cells were subsequently cultured
in medium with blastidin (0.5 μg/ml) to maintain the transfectants.
The ribozyme transgene plasmids containing cells were routinely
tested to confirm the knockdown of FAP expression at cDNA or
protein level. Cells transfected with anti-FAP ribozyme and empty
plasmid vector were respectively labeled as HOSFAPRIB
and HOSpEF6 for HOS cells and MG-63FAPRIB and
MG-63pEF6 for the transfected MG-63 cells.
RNA extraction and reverse
transcription-polymerase chain reaction (RT-PCR)
RNA was extracted from cells using the TRI reagent
(Sigma-Aldrich). RT was performed using the iScript™ cDNA synthesis
kit (Bio-Rad, Hercules, CA, USA). The following PCR conditions were
used: Denaturing at 94°C for 40 sec; annealing at 55°C for 40 sec;
and extension at 72°C for 60 sec. PCR was conducted over 30 cycles
with an initial 5 min denaturing step (94°C) and a final 10 min
extension step (72°C). PCR products were separated on a 2% agarose
gel stained with ethidium bromide. The primer sequences used are
provided in Table I.
 | Table IPrimers used for polymerase chain
reaction. |
Table I
Primers used for polymerase chain
reaction.
| Primer | Primer sequence,
5′-3′ | Optimal annealing
temperature, °C |
|---|
| FAP ribozyme |
| 2F |
CTGCAGGTGGATCTCCTGGTCTTTGTTTCAATACTGATGAGTCCGTGAGGA | 55 |
| 2R |
ACTAGTAAATTAGCATATGTCTATCAAAACAATATTTCGTCCTCAGGACT | 55 |
| FAP |
| F1 |
TCCCTTGCTAATTCAAGTGT | 55 |
| R1 |
AGAGCTTTAGCAATCTGTGC | 55 |
| F2 |
TGGAAAATGATTTGAAAAAT | 55 |
| R2 |
CTGTGTAGACAGACGCGTAA | 55 |
| GAPDH |
| F8 |
GGCTGCTTTTAACTCTGGTA | 55 |
| R8 |
GACTGTGGTCATGAGTCCTT | 55 |
SDS-PAGE and western blotting
Proteins of each control or transfected cells were
obtained following lysis. Equal amounts of each sample were
separated on a 10% acrylamide gel. Following transfer from the gel
onto a nitrocellulose membrane (Santa Cruz Biotechnology, Inc.),
proteins were probed using the respective primary antibodies (FAP
and GAPDH) at a concentration of 1:300, and specific
peroxidase-conjugated secondary antibodies at a concentration of
1:1,000. Protein bands were documented using a gel documentation
system (UVITech Ltd., Cambridge, UK).
In vitro growth assay
Briefly, 2,000 cells were seeded into each well
using three 96-well plates labeled as Day 1, 3 and 5. Following
incubation for 1, 3 and 5 days, cells were fixed in 4% (v/v)
formaldehyde and stained with 0.5% (w/v) crystal violet. The
crystal violet stain was then extracted using 10% (v/v) acetic acid
and cell density was determined by measuring the absorbance at a
wavelength of 540 nm using an ELx800 spectrophotometer (BioTek
Instruments, Inc., Winooski, VT, USA).
In vitro Matrigel invasion assay
In the in vitro Matrigel invasion assay
(17), a 24-well plate with
Transwell inserts containing 8.0-μm pores (Becton-Dickinson,
Franklin Lakes, NJ, USA) was first coated with 50 μg/insert of
Matrigel matrix basement membrane (BD Biosciences, Oxford, UK). In
total, 15,000 cells were seeded into Transwell inserts, followed by
72 h of incubation. After three days of incubation, cells which had
invaded through the artificial basement membrane to the outside of
the Transwell insert were fixed, stained and counted.
In vitro Matrigel adhesion assay
In the in vitro Matrigel adhesion assay
(18), a 96-well plate was
precoated with 5 μg Matrigel per well. Briefly, 45,000 cells were
seeded into each well. Following 45 min of incubation, non-adherent
cells were removed by vigorous washing using TBS. Adherent cells
were then fixed, stained and counted.
In vitro migration/wound-healing
assay
In the in vitro migration/wound-healing assay
(19), a total of 40,000 cells were
seeded in a 24-well plate and, upon reaching confluence, the medium
was changed and the monolayer was scraped with a fine gauge needle
to create a wound. The plate was placed on a heated plate to
maintain a constant temperature of 37°C. Images of the cells were
captured following wounding and every 15 min during 1.5 h with a
digital camera (GXCAM-5; GT Vision Ltd., Suffolk, UK) attached to a
microscope (Leitz DMIRB; Leica Microsystems Ltd., Buckinghamshire,
UK) at ×200 magnification.
Electric cell-substrate impedance sensing
(ECIS)-based cellular motility assay
The 9600 model of the ECIS instrument (Applied
BioPhysics, Inc., Troy, NY, USA) was used for attachment (adhesion)
using a 96W1E plate, as well as a motility assay (wounding assay)
(20–22). ECIS measures the interaction between
cells and the substrate to which the cells are attached via
gold-film electrodes placed on the surface of culture dishes.
Following a stabilization, the same number of HOSwt,
HOSpEF6, HOSFAPrib, MGwt,
MGpEF6 or MGFAPrib (80,000 per well) in the
same volume of medium (200 μl) were added to each well. During the
initial 3 h when cells were attaching to the bottom of the wells,
impedance and resistance of the cell layer were recorded for the
attachment ability analysis. After 10 h, when confluence was
reached, the monolayer was electrically wounded at 6 V for 30 sec.
Impedance and resistance of the cell layer were immediately
recorded for a period of ≤20 h for the motility ability
analysis.
Statistical analysis
Experimental procedures were repeated independently
at least three times. Statistical analysis was performed using the
Minitab statistical software package (version 14; Minitab, Ltd.,
Coventry, UK). The two-sample t-test was used for normally
distributed data, and data are presented as the mean ± standard
error of the mean. P<0.05 was considered to indicate a
statistically significant difference.
Results
Expression of FAP in OS cell lines and
tissues
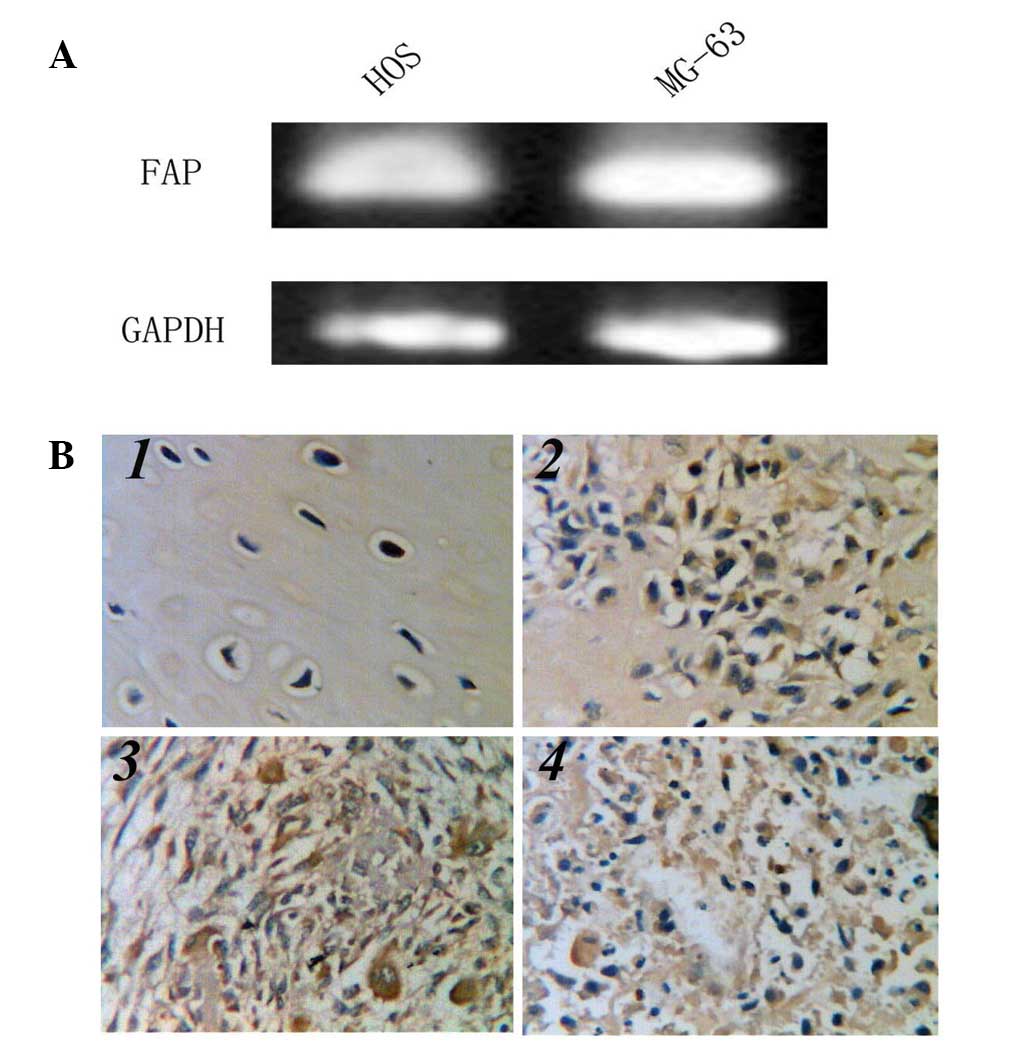
The presence of FAP was evident in the two human OS
cell lines (HOS and MG-63) tested through RT-PCR (Fig. 1A). To investigate the biological
function of FAP in OS, these cell lines were selected for knockdown
studies.
To assess the expression pattern of FAP at the
protein level, immunohistochemical staining of FAP was performed in
the human OS tissues. Using a specific anti-FAP monoclonal
antibody, FAP was detected in the cytoplasm of tumor cells, but was
absent from osteocytes in the background bone tissues (Fig. 1B).
Manipulation of FAP expression by
ribozyme transgene
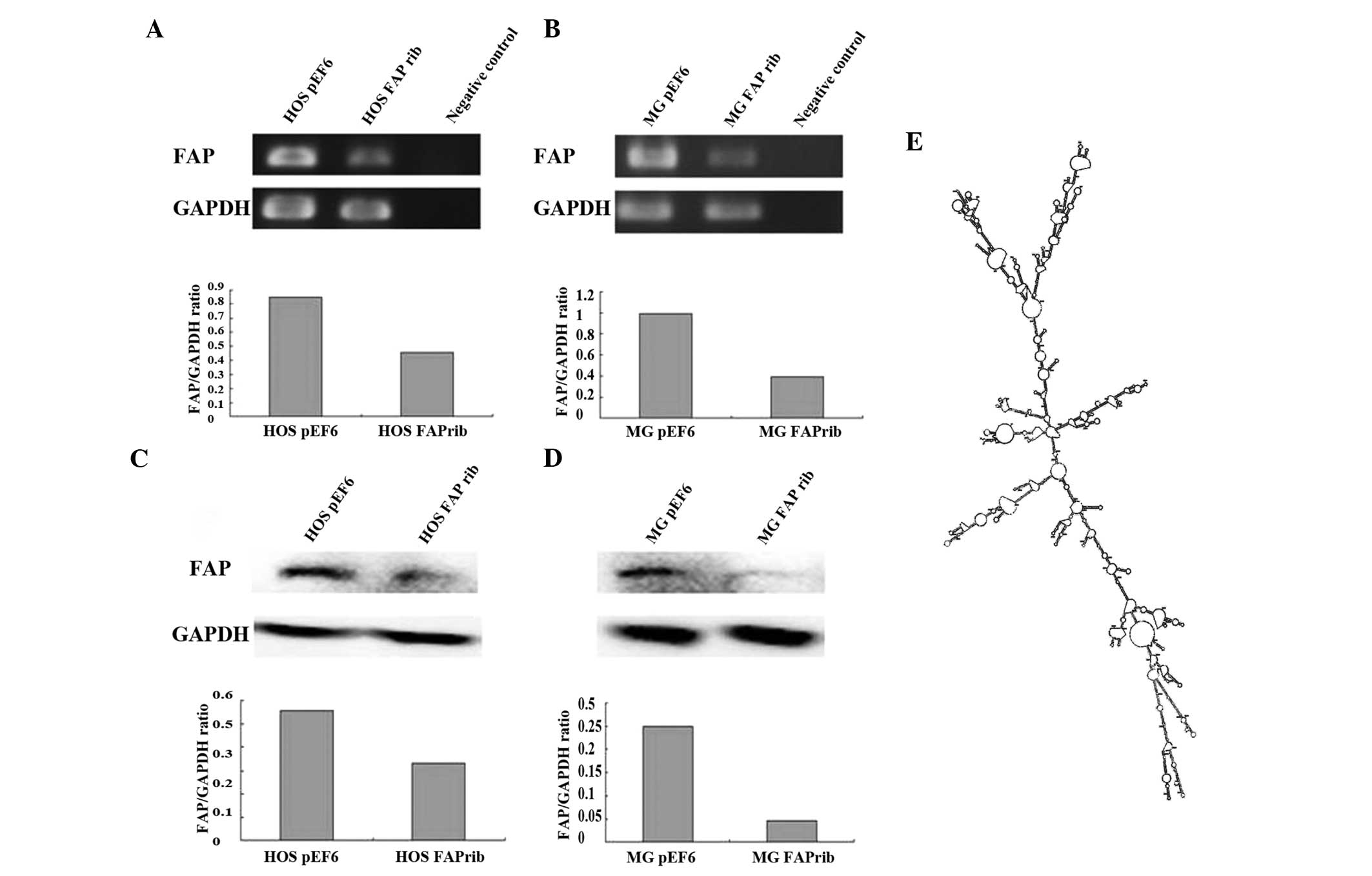
RT-PCR results demonstrated that FAP mRNA expression
was successfully knocked down in HOSFAPrib and
MGFAPrib cells in comparison with the level of
expression in empty plasmid cells (HOSpEF6 and
MGpEF6; Fig. 2A and B).
Additionally, western blotting was used to probe for FAP protein
levels in the control and transfected cell lines. Similar to the
trends observed at the mRNA level, FAP protein was found to be
highly expressed in all the control cell lines (HOSWT,
MGWT, HOSpEF6 and MGpEF6) and
expression of FAP protein exhibited a marked reduction in the
transfected cell lines (HOSFAPrib and
MGFAPrib) (Fig. 2C and
D).
Knockdown of FAP reduces OS cell
growth
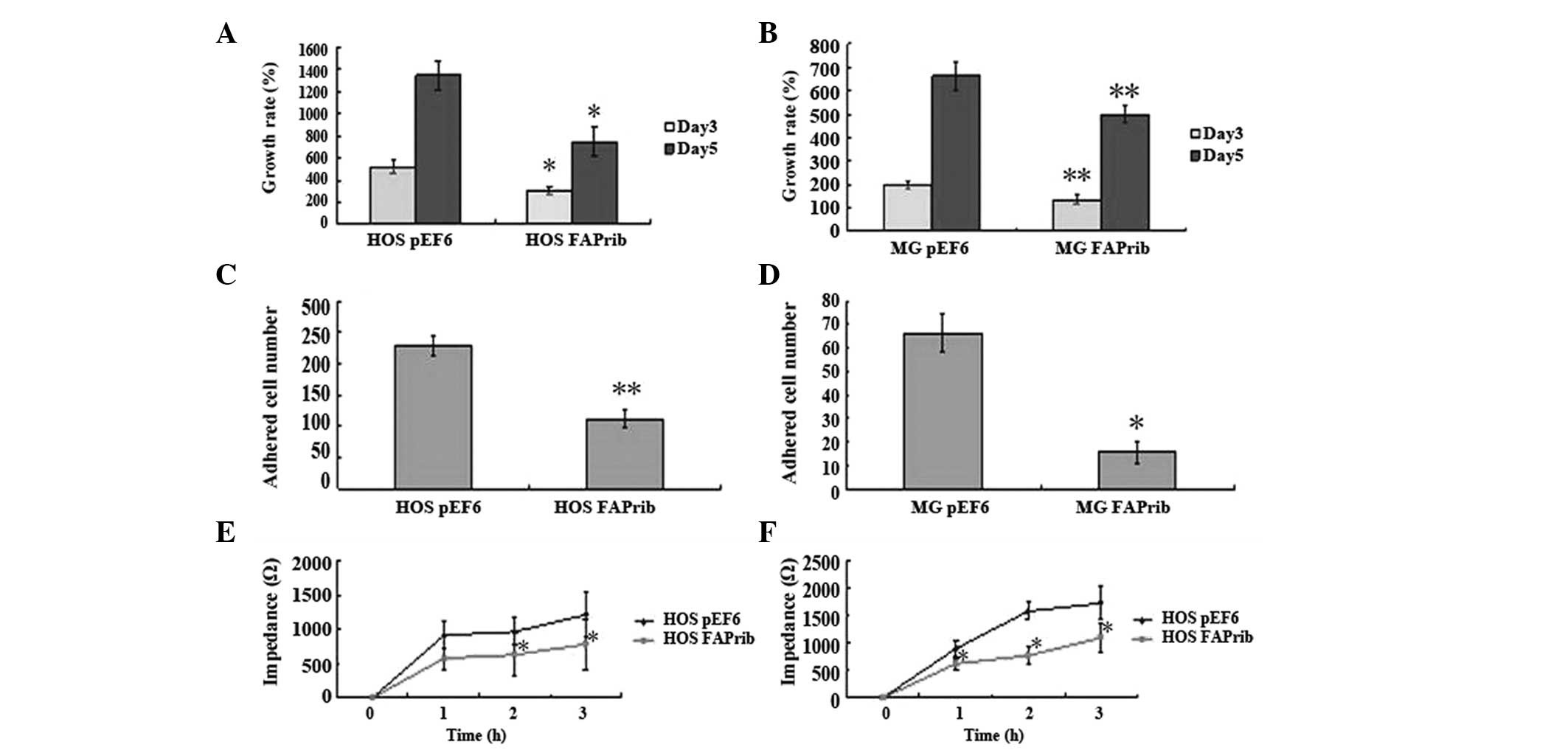
The in vitro tumor growth assay was used for
the detection of change in growth caused by FAP knockdown in HOS
and MG-63 cells. The same result was observed between these two
cell lines when the growth rates were analyzed following a total
5-day incubation, which was that absence of FAP caused a low growth
rate in OS cells, compared with their control cells. The results
exhibited a statistically significant difference at day 3
(HOSFAPrib vs. HOSpEF6: 137.7±19.8 vs.
199.1±15.6, P=0.027; and MGFAPrib vs. MGpEF6:
301.9±31.2 vs. 516.7±54.8, P=0.007) and day 5 (HOSFAPrib
vs. HOSpEF6: 499.4±36.4 vs. 661.2±56.0, P=0.036; and
MGFAPrib vs. MGpEF6: 740.4±132.9 vs.
1345.7.2±132.3, P=0.009) (Fig. 3A and
B).
Loss of endogenous FAP results in low
cell adhesion
To investigate the impact of the loss of FAP on the
adhesive capability in OS cells, a 45-min period in vitro
Matrigel adhesion assay and an ECIS assay were used. Cells adhering
to the artificial Matrigel basement membrane were counted. Notably,
the loss of FAP resulted in low adherence to the Matrigel in HOS
and MG-63 cells (HOSFAPrib vs. HOSpEF6:
111.0±15.0 vs. 227.3±15.6, P=0.009; and MGFAPrib vs.
MGpEF6: 15.5±4.4 vs. 66.2±8.1, P=0.025; Fig. 3C and D). In the attachment assay
detected by ECIS, the same tendency was observed where knockdown
cells showed a low adherence compared with their control cells
following seeding for 1–3 h (HOSFAPrib vs.
HOSpEF6, P<0.05 at 2 and 3 h after seeding; and
MGFAPrib vs. MGpEF6, P<0.05 at 1, 2 and 3
h after seeding; Fig. 3E and
F).
Knockdown of FAP decreases cell
invasion
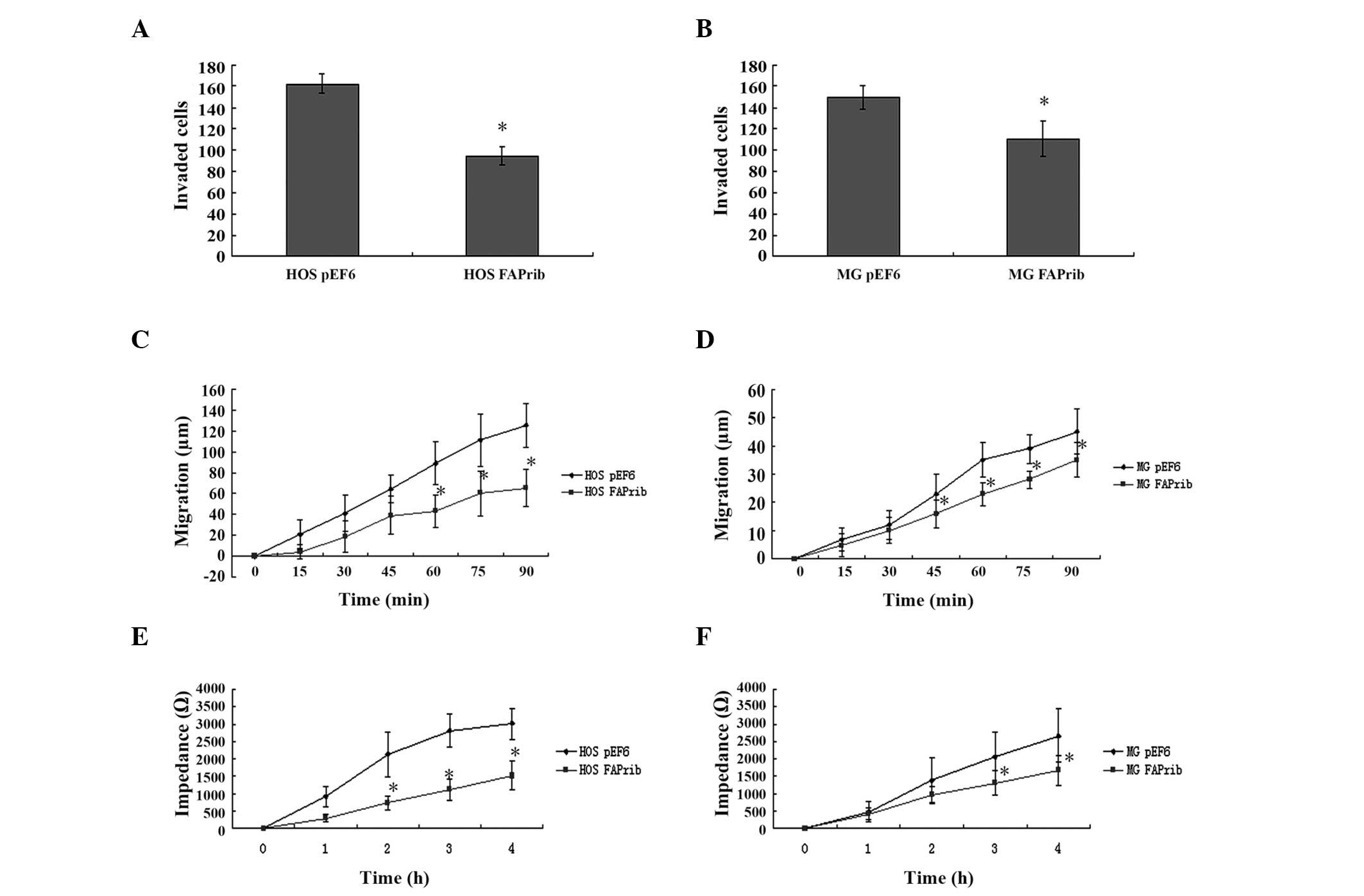
The FAP-knockdown cells exhibited a relatively lower
invasive capability than their control cells in the HOS and MG-63
cell lines (HOSFAPrib vs. HOSpEF6: 95.0±8.5
vs. 162.3±8.8, P=0.013; and MGFAPrib vs.
MGpEF6: 110.7±16.2 vs. 150.2±11.3, P=0.034; Fig. 4A and B).
Knockdown of FAP influences cell
motility
The wounding assay compared the migration
capabilities of OS cells between FAP-knockdown and control cells.
The migration of HOS and MG-63 cells was reduced when FAP was
absent during a 90 min incubation after the wounding
(HOSFAPrib vs. HOSpEF6, P<0.05 after 60
min; and MGFAPrib vs. MGpEF6, P<0.05 after
45 min; Fig. 4C and D). The effect
of FAP expression on cell motility was also assessed using an ECIS
assay. Following wounding at 10 h, the record of impedance and
resistance of the cell layer also showed the same result as the
wounding assay, which was that FAP influenced cell motility
(HOSFAPrib vs. HOSpEF6, P<0.05 at 2, 3 and
4 h after wounding; and MGFAPrib vs. MGpEF6,
P<0.05 at 3 and 4 h after wounding; Fig. 4E and F).
Discussion
FAP has been intensively investigated as a potential
diagnostic or therapeutic target since it is overexpressed by
activated stromal fibroblasts in malignant tumors and is absent in
normal adult tissues and benign tumors (23–26).
Since its identification, a number of previous studies have
analyzed the localization and expression of this protease in
diverse malignancies (27). FAP and
DPP-IV expression is also found in bone sarcomas (5). However, the role of FAP in
tumorigenesis and tumor growth, invasion and metastasis, as well as
the exact molecular mechanisms, remain unknown. There is a clear
discrepancy between FAP function in tumor promotion and suppression
(12,28–30).
Previously, Santos et al (26) showed that targeted gene disruption
or pharmacological inhibition of FAP proteinase activity reduces
the tumor growth in mouse models of lung and colon cancer. By
contrast, other studies have suggested that FAP has
tumor-suppressive activity (30,31).
In the current study, the gene expression of FAP was knocked down
through a hammerhead ribozyme transgene and the differences in the
cellular functions between the knockdown cells and their controls
were observed. The results of the current study indicated that
knockdown of FAP markedly reduces the ability of cell growth,
matrix adhesion, migration and invasion in MG-63 and HOS cell lines
compared with the control cells.
The cancer-specific distribution of FAP makes it a
novel therapeutic target in cancer treatment. While the function of
FAP within malignancies remains poorly understood, efforts have
been made to assess FAP as a therapeutic target, inhibiting its
proteinase activity. FAP is transiently expressed in specific fetal
mesenchymal tissues and is also expressed in certain disorders
associated with activated stroma, including wound healing,
rheumatoid arthritis, osteoarthritis, cirrhosis and pulmonary
fibrosis (5,27,32).
The effect of FAP on cellular functions and corresponding
implications in bone development and remodeling remain poorly
understood. The present study examined the function of FAP in OS
cells and the implication in the disease progression. FAP is
considered to promote tumor cell growth and proliferation (33). Chen et al (34) previously reported that FAP increases
the invasion, proliferation and migration of ovarian cancer cells.
The results of the present study revealed that bone sarcoma cell
lines express FAP. The knockdown of FAP markedly decreases the
in vitro growth, adhesion, migration and invasion of the OS
cells.
FAP influences OS cells and may play a role in OS
tumor progression and metastasis. Further investigation is likely
to shed light on the relevant diagnostic and therapeutic potential
of FAP in OS.
Acknowledgements
Dr L. Ding was a recipient of the Cardiff University
China Medical Scholarship, and the authors would like to thank the
Albert Hung Foundation and Cancer Research Wales for supporting the
study.
References
|
1
|
Hayden JB and Hoang BH: Osteosarcoma:
basic science and clinical implications. Orthop Clin North Am.
37:1–7. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Henry LR, Lee HO, Lee JS, et al: Clinical
implications of fibroblast activation protein in patients with
colon cancer. Clin Cancer Res. 13:1736–1741. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Javidroozi M, Zucker S and Chen WT: Plasma
seprase and DPP4 levels as markers of disease and prognosis in
cancer. Dis Markers. 32:309–320. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen SJ and Jiaang WT: Current advances
and therapeutic potential of agents targeting dipeptidyl
peptidases-IV, −II, 8/9 and fibroblast activation protein. Curr Top
Med Chem. 11:1447–1463. 2011.PubMed/NCBI
|
|
5
|
Dohi O, Ohtani H, Hatori M, et al:
Histogenesis-specific expression of fibroblast activation protein
and dipeptidylpeptidase-IV in human bone and soft tissue tumours.
Histopathology. 55:432–440. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rettig WJ, Garin-Chesa P, Beresford HR,
Oettgen HF, Melamed MR and Old LJ: Cell-surface glycoproteins of
human sarcomas: differential expression in normal and malignant
tissues and cultured cells. Proc Natl Acad Sci USA. 85:3110–3114.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ghersi G, Zhao Q, Salamone M, Yeh Y,
Zucker S and Chen WT: The protease complex consisting of dipeptidyl
peptidase IV and seprase plays a role in the migration and invasion
of human endothelial cells in collagenous matrices. Cancer Res.
66:4652–4661. 2006. View Article : Google Scholar
|
|
8
|
Cohen SJ, Alpaugh RK, Palazzo I, et al:
Fibroblast activation protein and its relationship to clinical
outcome in pancreatic adenocarcinoma. Pancreas. 37:154–158. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goscinski MA, Suo ZH, Nesland JM, et al:
Seprase, dipeptidyl peptidase IV and urokinase-type plasminogen
activator expression in dysplasia and invasive squamous cell
carcinoma of the esophagus. A study of 229 cases from Anyang Tumor
Hospital, Henan Province, China. Oncology. 75:49–59. 2008.
View Article : Google Scholar
|
|
10
|
Keane FM, Nadvi NA, Yao TW and Gorrell MD:
Neuropeptide Y, B-type natriuretic peptide, substance P and peptide
YY are novel substrates of fibroblast activation protein-alpha.
FEBS J. 278:1316–1332. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kennedy A, Dong H, Chen D and Chen WT:
Elevation of seprase expression and promotion of an invasive
phenotype by collagenous matrices in ovarian tumor cells. Int J
Cancer. 124:27–35. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kraman M, Bambrough PJ, Arnold JN, et al:
Suppression of antitumor immunity by stromal cells expressing
fibroblast activation protein-alpha. Science. 330:827–830. 2010.
View Article : Google Scholar
|
|
13
|
Yi YM, Zhang G, Zeng J, et al: A new tumor
vaccine: FAPtau-MT elicits effective antitumor response by
targeting indolamine2,3-dioxygenase in antigen presenting cells.
Cancer Biol Ther. 11:866–873. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sarto-Jackson I, Milenkovic I, Smalla KH,
et al: The cell adhesion molecule neuroplastin-65 is a novel
interaction partner of gamma-aminobutyric acid type A receptors. J
Biol Chem. 287:14201–14214. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Danilova N: The evolution of adaptive
immunity. Adv Exp Med Biol. 738:218–235. 2012. View Article : Google Scholar
|
|
16
|
Liu C, Lewis CM, Lou Y, et al: Agonistic
antibody to CD40 boosts the antitumor activity of adoptively
transferred T cells in vivo. J Immunother. 35:276–282. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kikuchi S, Iwai M, Sakurai-Yageta M, et
al: Expression of a splicing variant of the CADM1 specific to small
cell lung cancer. Cancer Sci. 103:1051–1057. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee G, Cheung AP, Ge B, et al: CA215 and
GnRH receptor as targets for cancer therapy. Cancer Immunol
Immunother. 61:1805–1817. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jiang WG, Hiscox S, Hallett MB, Scott C,
Horrobin DF and Puntis MC: Inhibition of hepatocyte growth
factor-induced motility and in vitro invasion of human colon cancer
cells by gamma-linolenic acid. Br J Cancer. 71:744–752. 1995.
View Article : Google Scholar
|
|
20
|
Estecha A, Aguilera-Montilla N,
Sánchez-Mateos P and Puig-Kröger A: RUNX3 regulates intercellular
adhesion molecule 3 (ICAM-3) expression during macrophage
differentiation and monocyte extravasation. PLoS One. 7:e333132012.
View Article : Google Scholar
|
|
21
|
Fujita-Hamabe W and Tokuyama S: The
involvement of cleavage of neural cell adhesion molecule in
neuronal death under oxidative stress conditions in cultured
cortical neurons. Biol Pharm Bull. 35:624–628. 2012. View Article : Google Scholar
|
|
22
|
Meeusen JW, Klein CJ, Pirko I, et al:
Potassium channel complex autoimmunity induced by inhaled brain
tissue aerosol. Ann Neurol. 71:417–426. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Christiansen VJ, Jackson KW, Lee KN, Downs
TD and McKee PA: Targeting inhibition of fibroblast activation
protein-alpha and prolyl oligopeptidase activities on cells common
to metastatic tumor microenvironments. Neoplasia. 15:348–358.
2013.
|
|
24
|
Hayward SW: Preclinical assessment of
fibroblast activation protein as a target for antitumor therapy.
Future Oncol. 6:347–349. 2010. View
Article : Google Scholar
|
|
25
|
Puré E: The road to integrative cancer
therapies: emergence of a tumor-associated fibroblast protease as a
potential therapeutic target in cancer. Expert Opin Ther Targets.
13:967–973. 2009.PubMed/NCBI
|
|
26
|
Santos AM, Jung J, Aziz N, Kissil JL and
Puré E: Targeting fibroblast activation protein inhibits tumor
stromagenesis and growth in mice. J Clin Invest. 119:3613–3625.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liu R, Li H, Liu L, et al: Fibroblast
activation protein: A potential therapeutic target in cancer.
Cancer Biol Ther. 13:123–129. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cheng JD, Valianou M, Canutescu AA, et al:
Abrogation of fibroblast activation protein enzymatic activity
attenuates tumor growth. Mol Cancer Ther. 4:351–360.
2005.PubMed/NCBI
|
|
29
|
Scanlan MJ, Raj BK, Calvo B, et al:
Molecular cloning of fibroblast activation protein alpha, a member
of the serine protease family selectively expressed in stromal
fibroblasts of epithelial cancers. Proc Natl Acad Sci USA.
91:5657–5661. 1994. View Article : Google Scholar
|
|
30
|
Wesley UV, Albino AP, Tiwari S and
Houghton AN: A role for dipeptidyl peptidase IV in suppressing the
malignant phenotype of melanocytic cells. J Exp Med. 190:311–322.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ramirez-Montagut T, Blachere NE,
Sviderskaya EV, et al: FAPalpha, a surface peptidase expressed
during wound healing, is a tumor suppressor. Oncogene.
23:5435–5446. 2004. View Article : Google Scholar
|
|
32
|
Bauer S, Jendro MC, Wadle A, et al:
Fibroblast activation protein is expressed by rheumatoid
myofibroblast-like synoviocytes. Arthritis Res Ther. 8:R1712006.
View Article : Google Scholar
|
|
33
|
Goodman JD, Rozypal TL and Kelly T:
Seprase, a membranebound protease, alleviates the serum growth
requirement of human breast cancer cells. Clin Exp Metastasis.
20:459–470. 2003. View Article : Google Scholar
|
|
34
|
Chen H, Yang WW, Wen QT, Xu L and Chen M:
TGF-beta induces fibroblast activation protein expression;
fibroblast activation protein expression increases the
proliferation, adhesion, and migration of HO-8910PM [corrected].
Exp Mol Pathol. 87:189–194. 2009.PubMed/NCBI
|