Introduction
Giant cell tumors (GCTs) of the bone are expansile
osteolytic tumors in young adults that usually occur at the end of
the long bones. Although only 6% of GCTs occur in the sacrum, GCTs
are the second most common type of primary tumor involving bone in
the sacrum (1,2). Recently, certain authors have claimed
that parathyroid hormone-related protein may act locally within
GCTs and be significant in the pathogenesis of these tumors
(3). It is rare to identify a GCT
complicating pregnancy, and a correlation between tumor growth and
pregnancy has not yet been clarified.
Sacral GCTs tend to be clinically silent during
their initial stages of development and cause few symptoms until
they achieve an extremely large size, particularly when occurring
during pregnancy. A number of patients have been initially
misdiagnosed with prolapses of lumbar intervertebral discs,
chordomas or other tumors. Lumbosacral magnetic resonance imaging
(MRI) is useful for the diagnosis of these conditions. Although
histologically benign, these osteolytic expansive tumors are
locally aggressive, and the local recurrence rate in the sacrum is
higher than recurrence rates at other skeletal locations. In
addition, sacral GCTs have been shown to metastasize (4). Treatment options include radiation
therapy, surgery (such as intralesional curettage and wide excision
by complete or partial en bloc sacrectomy), surgery plus adjuvant
treatment and serial arterial embolization (5,6). More
recently, the bisphosphonate zoledronic acid (7) and interferon α-2b (8) have been reported to be effective and
safe adjuvant treatments in patients with spinal GCT, particularly
in those with recurrent and metastatic tumors.
Case report
A 29-year-old female experienced severe pain in the
lumbosacral region on the seventh day after the delivery of a
child. The pain was initially considered to be due to pregnancy and
delivery and no further examination was performed. However, the
patient continued to experience persistent pain and a burning
sensation in the lumbosacral region, particularly at night. The
pain radiated from the lumbar spine into each thigh
posterolaterally and subsequently, into the bilateral crus
posterolaterally. The patient also experienced a change of bowel
habits. Eight months later, the patient presented at the XinNing
Country Sunshine Hospital (Shaoyang, China) with continuing
discomfort and pain in the lumbosacral region. MRI revealed a huge
tumor mass (95×70×90 mm in size) involving the sacrococcygeal
region, indicating a chordoma.
One week later, the patient was transferred to the
Hunan Xiang-ya Second Hospital (Changsha, China). The patient had
not menstruated during the eight months since delivery. A physical
examination upon admission showed that the patient was positive for
Lasegue’s sign at 70 degrees on each side. The patient experienced
pain on percussion of the sacrum and the temperature of the sacral
skin was high. Rectal examination revealed a huge presacral and
toughening mass of 9×7 cm in size. The mass exhibited a regular
surface, was firm in consistency, was not tender and was fixed to
the sacrum. Blood biochemistry analysis revealed that the alkaline
phosphatase, serum iron and C-reactive protein concentrations and
the erythrocyte sedimentation rate were all within normal ranges.
Chest X-ray observations were normal.
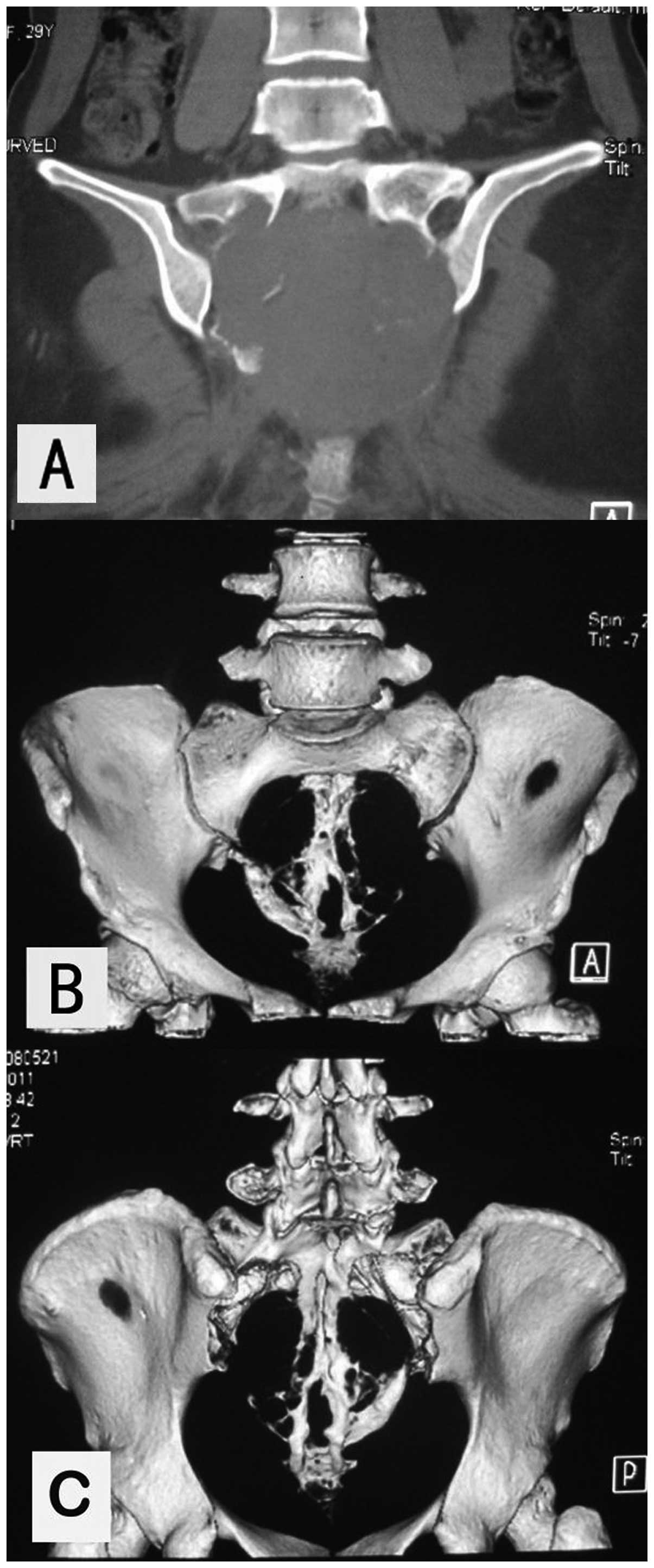
Plain X-rays of the lumbar spine, sacrum and pelvis
revealed a large amount of expansile osteolytic destruction of the
sacrum involving the upper foramina and right iliac bone, as well
as a pathological fracture. The lytic lesions were surrounded by a
soft-tissue mass, without peripheral bone sclerosis.
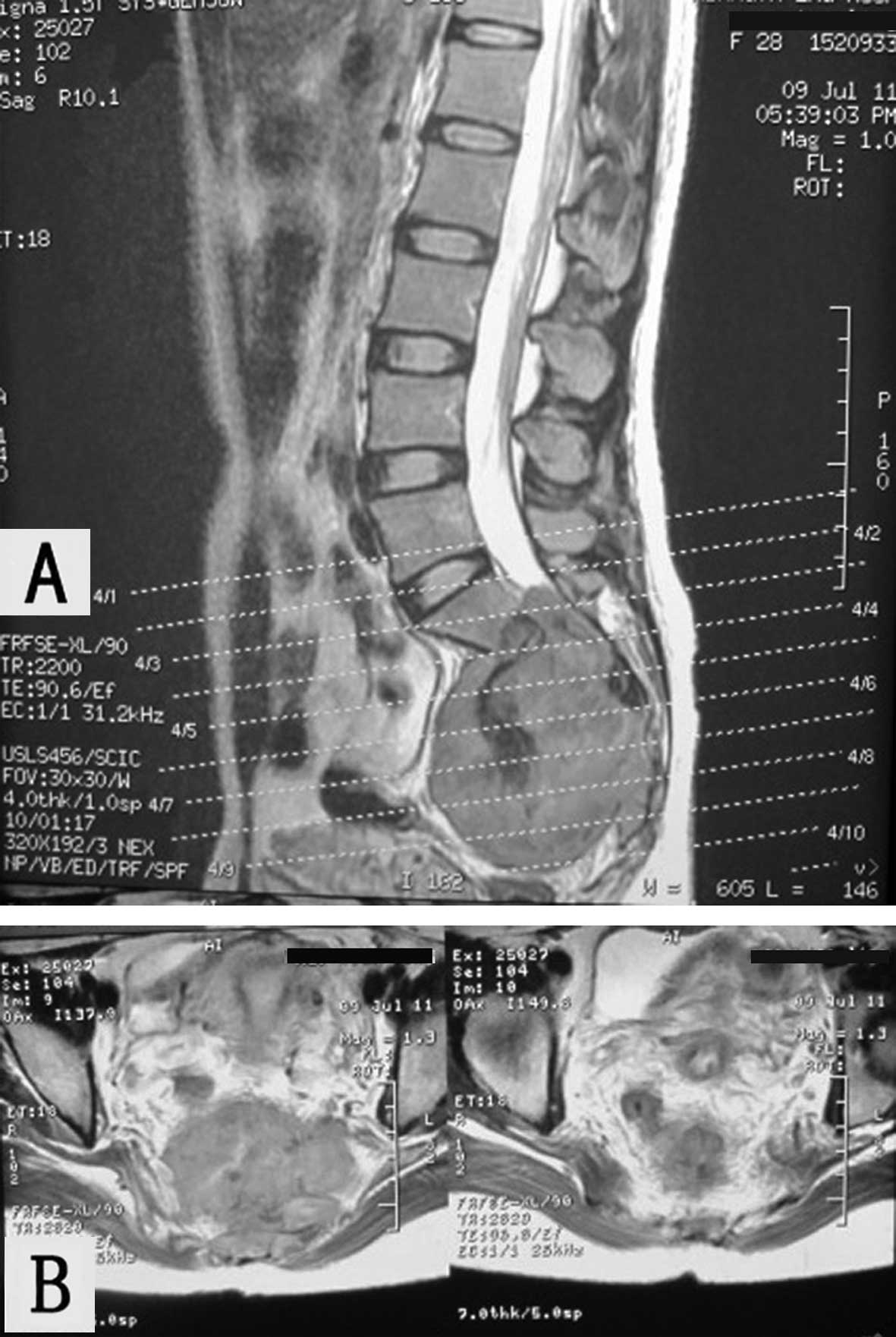
Three-dimensional reconstructions of computed tomography (CT) scans
(Fig. 1) and MRI (Fig. 2) revealed osteolytic destruction of
the sacrococcygeal bones, including parts of the first sacral
vertebra and underlying left internal ilium, as well as a huge
soft-tissue mass measuring 95×75 mm in size. The sacral canal was
enlarged. The lesion showed large patches of mixed signal shadows
on T1- and T2-weighted images, which followed the plane of the
first sacral vertebra. An unclear boundary was identified between
the mass and rectum. Upon enhanced scanning, the lesions appeared
more pronounced. The results of plain X-ray, CT and MRI indicated a
diagnosis of a chordoma.
The patient was treated surgically. The two sciatic
nerves were contained within the tumor. In addition, the tumor had
invaded the left sacroiliac joint and partially invaded the left
iliac surface. The thecal sac had been cut inferiorly to the S1
vertebrae. Therefore, the thecal sac was ligated at the S1–S2
level, the sacrum was cut with osteotomies under the S1 superior
border, keeping a thin layer of bone and ilium linked laterally,
and the sciatic nerves were separated from the tumor. The tumor was
resected en bloc as a section greater than 11×11×7 cm in size,
along with the sacral nerves, and the pelvic ring was reconstructed
using an arc pelvic reconstruction plate connected to the bilateral
ilia. The remaining sectional S1 vertebrae received two massive
allografts, which were fixed with screws. The patient required
transfusions with 1,950 ml of enriched red blood cell suspension
and 900 ml of platelets during surgery. The patient was diagnosed
with a conventional GCT based on the histopathological examination
of the resected specimen.
The patient and the patient’s family were informed
that a colostomy was likely to be required if the functions of the
bladder and anal sphincter were not recovered. Therefore, the
patient performed exercises to strengthen the function of the
bladder, anal sphincter and muscles of the lower limbs in bed 600
times per day. The patient was able to pass urine two months
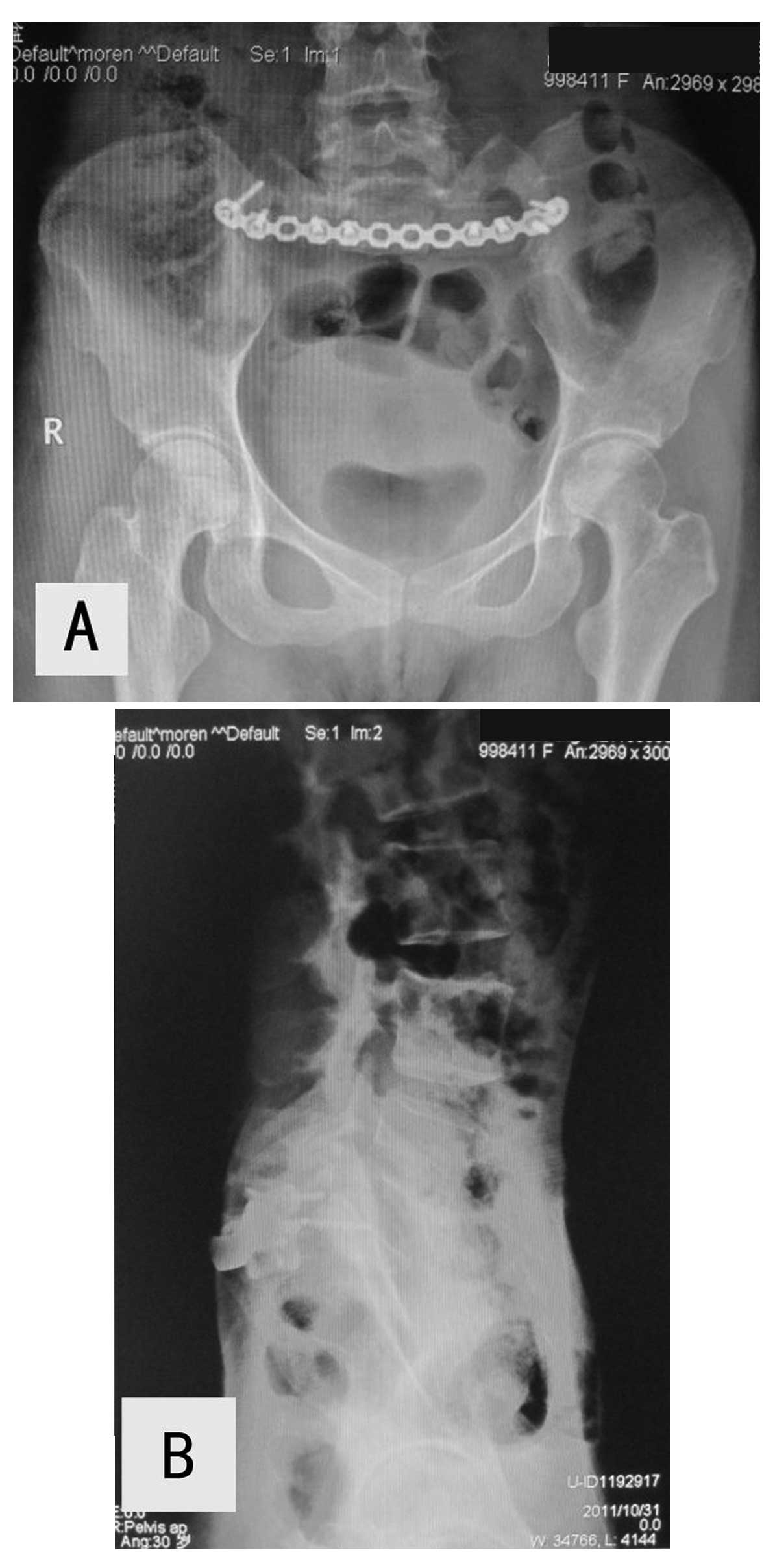
postoperatively and stool three months postoperatively. Plain
X-rays of the pelvic and sacroiliac regions at three months showed
no looseness or fractures of internal fixation and no new bone
destruction (Fig. 3). Six months
after surgery, the patient was able to walk with a cane and had
control of the urinary bladder and anal sphincter. One year later,
the patient was able to walk without a cane and had good control of
the urinary bladder and anal sphincter. Although the two bilateral
S2 nerve roots were lost, the patient recovered urinary and bowel
function by exercising. The patient provided written informed
consent.
Discussion
The detection of a GCT may be delayed, since
tumor-related pain is frequently misinterpreted as a symptom of
pregnancy, as observed in the present patient. Care must be taken
not to overlook the possibility of a tumor in the sacrum or
innominate bone during pregnancy.
Although surgery remains the first-line treatment
for sacral tumors, their difficult location and huge size, as well
as the possibility of life-threatening intraoperative bleeding,
make surgery difficult (9). In
addition, microscopic lesions may remain when the sacral nerve
roots are preserved, whereas bowel and bladder function may be
compromised when the sacral nerve roots are not preserved. Other
problems include difficulties reconstructing the stability of the
pelvis and spine and local recurrence. Notably, local recurrence
rates have been found to approach 50% in patients who do not
undergo surgery with wide margins, by complete or partial en bloc
sacrectomy (10). Although surgery
with wide margins results in a significant decrease in the local
recurrence rate, wide resection often requires the sacral nerve
roots to be sacrificed. In addition, effective control of massive
bleeding and a reconstruction of pelvic and spinal stability is
required, particularly since a number of GCTs involve the upper
sacral segments, frequently crossing the midline and even the
sacroiliac joint (4,6). The surgical technique used in the
current study consisted of curettage for tumors located at the
sacroiliac joint and underlying left ilium and a partial en bloc
sacrectomy (partial S1 and completely below). The pelvic ring was
reconstructed using an arc pelvic reconstruction plate and two
massive allografts.
Arterial embolization (5), followed by complete occlusion of the
artery, may minimize intraoperative bleeding and aid in directly
resecting the tumor and decreasing the local recurrence rate
(11). Therefore, in the present
study, the two internal iliac arteries were ligated to control
intraoperative hemorrhage. If the two S2 nerve roots may be
preserved, approximately half of patients are likely to retain
bowel and bladder function. However, bowel and bladder function are
lost if only the unilateral S2 nerve root is spared (6). Unilateral resection of the sacral
roots or preservation of at least one S3 nerve root upon bilateral
resection has been found to preserve bowel and bladder function in
the majority of patients (12).
Although the patient of the current study lost the two S2 nerve
roots, their desire to recover bowel and bladder function was
extremely strong. Therefore, the patient performed exercises to
strengthen the function of the bladder and anal sphincter and
increase muscle strength in the lower limbs.
Local malignant transformation has been reported to
occur in ≤16% of patients with primary GCTs, with 1–9% of patients
showing lung metastases of GCTs of the bone (6,13). To
date, the present patient has shown no evidence of local recurrence
on pelvic X-rays and no lung metastases on chest X-rays.
In conclusion, complaints, such as pain, discomfort
or numbness around the pelvis, particularly during pregnancy, may
be the direct result of a tumor in the pelvic bone. The current
study described a patient who, despite the loss of the bilateral S2
nerve roots, recovered function of the urinary bladder and anal
sphincter by exercising.
References
|
1
|
Bloem JL and Reidsma II: Bone and soft
tissue tumors of hip and pelvis. Eur J Radiol. 81:3793–3801. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Turcotte RE, Sim FH and Unni KK: Giant
cell tumor of the sacrum. Clin Orthop Relat Res. 291:215–221.
1993.PubMed/NCBI
|
|
3
|
Cowan RW, Singh G and Ghert M: PTHrP
increases RANKL expression by stromal cells from giant cell tumor
of bone. J Orthop Res. 30:877–884. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Leggon RE, Zlotecki R, Reith J and
Scarborough MT: Giant cell tumor of the pelvis and sacrum: 17 cases
and analysis of the literature. Clin Orthop Relat Res. 423:196–207.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lin PP, Guzel VB, Moura MF, Wallace S,
Benjamin RS, Weber KL, et al: Long-term follow-up of patients with
giant cell tumor of the sacrum treated with selective arterial
embolization. Cancer. 95:1317–1325. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Guo W, Ji T, Tang X and Yang Y: Outcome of
conservative surgery for giant cell tumor of the sacrum. Spine
(Phila Pa 1976). 34:1025–1031. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gille O, Oliveira Bde A, Guerin P, Lepreux
S, Richez C and Vital JM: Regression of giant cell tumor of the
cervical spine with bisphosphonate as single therapy. Spine (Phila
Pa 1976). 37:E396–E399. 2011. View Article : Google Scholar
|
|
8
|
Wei F, Liu X, Liu Z, Jiang L, Dang G, Ma Q
and Dang L: Interferon alfa-2b for recurrent and metastatic giant
cell tumor of the spine: report of two cases. Spine (Phila Pa
1976). 35:E1418–E1422. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wuisman P, Lieshout O, Sugihara S and van
Dijk M: Total sacrectomy and reconstruction: oncologic and
functional outcome. Clin Orthop Relat Res. 381:192–203. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Randall RL: Giant cell tumor of the
sacrum. Neurosurg Focus. 15:E132003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mi C, Lu H and Liu H: Surgical excision of
sacral tumors assisted by occluding the abdominal aorta with a
balloon dilation catheter: a report of 3 cases. Spine (Phila Pa
1976). 30:E614–E616. 2005. View Article : Google Scholar
|
|
12
|
Todd LT Jr, Yaszemski MJ, Currier BL,
Fuchs B, Kim CW and Sim FH: Bowel and bladder function after major
sacral resection. Clin Orthop Relat Res. 397:36–39. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Althausen PL, Schneider PD, Bold RJ, Gupta
MC, Goodnight JE Jr and Khatri VP: Multimodality management of a
giant cell tumor arising in the proximal sacrum: case report. Spine
(Phila Pa 1976). 27:E361–E365. 2002. View Article : Google Scholar
|