Introduction
Hepatocellular carcinoma (HCC) is the sixth most
common type of neoplasm and the third most frequent cause of
cancer-related mortality in Western countries (1). The Barcelona Clinic Liver Cancer
(BCLC) strategy is a classification which stratifies patients
according to prognosis, providing a link to treatment. Patients
with advanced HCC (BCLC stage C) exhibit cancer-related symptoms
[symptomatic tumors; Eastern Cooperative Oncology Group (ECOG)
grades 1–2], including macrovascular invasion (segmental or portal
invasion) or extrahepatic spread (lymph node involvement or
metastases) which carry a poor prognosis, with a predicted median
survival time of six months or survival rate of 25% at one year.
The standard treatment for advanced HCC (BCLC stage C) is
sorafenib, an oral multikinase inhibitor that inhibits the
following: i) Serine-threonine kinases, Raf-1 and B-Raf, of the
Raf/MEK/ERK signaling pathway; and ii) the receptor tyrosine kinase
activity of VEGFR1,2 and 3, PDGFR-β, c-Kit, Flt-3 and RET (2,3).
Sorafenib inhibits tumor cell proliferation and tumor angiogenesis,
and increases the rate of apoptosis in a number of tumors (4). In two randomized clinical trials
[Sorafenib HCC Assessment Randomized Protocol Trial (SHARP) and
Asia Pacific Liver Cancer Study], sorafenib treatment resulted in
longer median survival time and time to progression (TTP) in
advanced hepatocellular cancer when compared with the placebo
(5,6).
Electro-hyperthermia (EHY), also known as
oncothermia or extracellular hyperthermia, is a method of
locoregional hyperthermia, established by the direct absorption of
an electric field energy in the extracellular liquid with a
subsequent temperature gradient between the extra- and
intracellular compartments; this gradient destroys cancer cell
membranes, leading to necrosis or apoptosis. As the conductivity
and the dielectric constant of the extracellular matrix in
malignant tissue are higher than in the normal tissue, this
technique results in selective tumor tissue destruction. For this
reason, energy absorption at the applied frequency is significantly
increased. Furthermore, malignant cells typically exhibit
relatively rigid membranes due to increased phospholipid
concentrations, therefore, EHY is likely to selectively destroy
malignant cells prior to affecting the healthy cells. EHY increases
apoptosis (producing membrane heat shock proteins), blocks further
proliferation, terminates tumor cell dissemination (re-establishing
the adherent connections) and increases immunogenicity. EHY is a
complementary treatment in various types of tumors, such as brain,
soft tissue, liver and abdominal, pancreatic, and head and neck
tumors (7).
Hyperthermia inhibits angiogenesis through
endothelial cell (EC) damage and increases PAI-1 genetic expression
in ECs (8). Several
pharmacodynamics (including the acceleration of the primary mode of
action and an increased intracellular drug concentration) and
pharmacokinetics (for example drug uptake, distribution, metabolism
and excretion) interactions have been described between drugs and
temperature. The cytotoxic effect of the majority of alkylating
agents (including cyclophosphamide and ifosfamide) and platinum
compounds are linearly enhanced with increasing temperature from 37
to >40°C. Conversely, doxorubicin appears to have a defined
temperature threshold, whilst the majority of antimetabolites (such
as 5-fluorouracil), as well as vinca alkaloids and taxanes, show no
dependency to hyperthermia (9). In
certain animal models, several drugs (including KB-R8498, flavone
acetic acid, vinblastine and combretastatin) have been observed to
induce a temporary reduction in tumor blood, but only in
combination with hyperthermia significant tumor responses (10).
The potential synergic antiangiogenic and
proapoptotic effects are the rationale for combining sorafenib and
EHY for the treatment of HCC (11,12).
The present study evaluated the efficacy and safety of this
combination in patients with advanced HCC in a phase II study at
the National Cancer Institute ‘Giovanni Paolo II’ (Bari,
Italy).
Materials and methods
A mono-institutional uncontrolled phase II trial was
conducted on advanced HCC patients. The Ethical Committee of the
National Cancer Institute ‘Giovanni Paolo II’ approved the protocol
which was in accordance with the ethical guidelines of the 1975
Declaration of Helsinki. Written informed consent was obtained from
each patient.
Patient eligibility
Between February 2009 and September 2010, 21
patients, comprising 14 (67%) males and seven (33%) females with a
median age of 64 years (range, 55–73 years), were enrolled in this
study at the at the National Cancer Institute ‘Giovanni Paolo II’.
Patients with measurable, histologically confirmed and inoperable
HCC who had not received prior systemic treatment for HCC were
eligible for enrollment. The inclusion criteria included age of ≥18
years; Eastern Cooperative Oncology Group performance status of ≤2;
Child-Pugh (CP) score of A or B; life expectancy of ≥12 weeks;
adequate hematological status (platelet count of
≥60×109/l; hemoglobin level of ≥ 8.5 g/dl; and
prothrombin time international normalized ratio of ≤2.3 or
prothrombin time of ≤6 sec above the control); adequate liver
function tests (albumin level of ≥2.8 g/dl, total bilirubin level
of ≤3 mg/dl and alanine aminotransferase and aspartate
aminotransferase levels of ≤5 times the upper limit of the normal
range) and adequate renal function tests (serum creatinine level of
≤1.5 times the upper limit of the normal range). Hepatitis B virus
(HBV) or hepatitis C virus (HCV) infection status at baseline were
collected from the medical history or laboratory tests. The
patients were required to have at least one untreated target lesion
that could be measured in one dimension, according to the Response
Evaluation Criteria in Solid Tumors (RECIST) (13).
Treatment and dose modifications
Patients received 400 mg sorafenib twice a day and
EHY with capacitative electrodes with a deep hypothermia
radiofrequency field of 13.56 Mhz at 80 W for 60 min, three times a
week for six weeks, followed by two weeks without treatment.
Regional hyperthermia and thermal mapping were performed according
to the European Society of Hyperthermic Oncology guidelines for
quality and safety assurance (14).
Locoregional deep-hyperthermia was performed using the Oncotherm
EHY-2000 medical device (Oncotherm GmbH, Traisdorf, Germany). A
large, water-cooled bolus asymmetric electrode (30 cm in diameter)
was used.
Sorafenib treatment interruptions and dose
reductions (initially 200 mg twice daily, then reduced to 200 mg
once daily) were allowed for drug-related toxicity, measured
according to the National Cancer Institute Common Toxicity Criteria
(v 3.0) (15).
Patients with dermatologic toxicities of grade 3/4
and patients with hematological toxicity of grade 3 received lower
doses. A dose delay was introduced for grade 4 hematologic
toxicities and grade 3 non-hematologic toxicities, until toxicity
was grade 2 or less; patients were then treated at one dose level
lower and therapy was discontinued if recovery time was three weeks
or longer. Patients with drug-related grade 4 non-hematologic
toxicities were removed from the study.
For hand-foot skin reaction (HFSR), dose
modifications based on prescribing information and 2008 consensus
panel recommendations were used (16).
Treatment was continued until disease progression
(PD) or unacceptable drug-related toxicities.
Response assessment
Bidimensional tumor measurements were performed at
baseline and every eight weeks (one cycle), according to RECIST, by
computed tomography or magnetic resonance imaging. Throughout the
study, the lesions were measured at baseline and evaluated using
the same technique. Overall tumor response was scored as a complete
response (CR), partial response (PR) or stable disease (SD) if the
response was confirmed at least four weeks later. The disease
control rate (DCR) was the proportion of patients who had the best
response rating of CR, PR or SD, according to RECIST, which was
maintained for at least four weeks from the initial manifestation
of that rating. Patient visits were scheduled every three weeks and
at the end of treatment to monitor safety, compliance and determine
side effects. The safety assessment included documentation of the
adverse events, clinical laboratory tests (hematological and
biochemical analyses), physical examination and measurement of
vital signs.
Statistical analysis
This was an uncontrolled mono-institutional phase II
trial. The primary endpoint of this trial was the progression-free
survival (PFS) rate at four months. The secondary endpoints were:
Overall tumor response (CR, PR and SD), TTP (initial treatment
until PD) and overall survival (OS; initial treatment to
mortality). The two-stages of Simon’s optimal design were used to
test the null hypothesis (H0) that the PFS rate at four months was
20% against the alternative hypothesis (H1) of 60% With a sample
size of 21 patients, this study had 80% power and an α level of
0.01. TTP and OS were estimated according to the Kaplan-Meier
method. All the analyses were performed using Stata 11.0 (Stata
Corporation, College Station, TX, USA).
Results
Patient characteristics
The baseline characteristics of the patients are
shown in Table I. Initially, the
ECOG performance status was 0 in 11 patients (50%) and 1 in 10
patients (50%). All patients had documented background chronic
liver disease and 17 of the 21 patients had a CP classification of
A. Considering viral infections, five patients were positive for
HBV, 15 patients were positive for HCV and only one patient was
positive for the two viruses, HBV/HCV. The α-fetoprotein range was
1–108 ng/ml (median, 41.6 ng/ml). Extrahepatic spread was present
in only five patients (three bone and two lung), while portal vein
thrombosis was observed in 11 patients (50%).
 | Table IPatient baseline characteristics. |
Table I
Patient baseline characteristics.
| Characteristics | n (%) |
|---|
| Age, years |
| Median | 64 |
| Range | 55–73 |
| Gender |
| Male | 14 (67) |
| Female | 7 (33) |
| ECOG performance
status |
| 0 | 11 (50) |
| 1 | 10 (50) |
| 2 | 0 |
| Child-Pugh
status |
| A | 17 (80) |
| B | 4 (4) |
| Hepatitis virus
status |
| HBV infection | 5 (20) |
| HCV infection | 15 (75) |
| HBV/HCV
infections | 1 (5) |
| α-fetoprotein
>ULN |
| Yes | 15 (75) |
| No | 6 (25) |
| Macroscopic vascular
invasion |
| Yes | 11 (50) |
| No | 10 (50) |
| Extrahepatic
spread |
| Yes (bone and
lung) | 5 (25) |
| No | 16 (75) |
Dose and duration of therapy
The median time of treatment was 4.5 months (range,
2–7 months). A total of 48.3 treatment cycles were administered
(mean, 2.3 cycles for each patient; range, 1–3.6) and 11 patients
(60%) received 100% of the planned study drug. Sorafenib was
administered at a daily mean dose of 700 mg (range, 600–800 mg).
For nine patients, the treatment was discontinued (45%) due to
PD.
Efficacy
All patients were considered evaluable for the
primary endpoint. The PFS rate at four months was 70%. One patient
(5%) achieved PR and 11 patients achieved SD (50%); however, no CR
was reported. The DCR was 45% (Table
II).
 | Table IIResponse rates according to the
Response Evaluation Criteria in Solid Tumors. |
Table II
Response rates according to the
Response Evaluation Criteria in Solid Tumors.
| Response | n (%) |
|---|
| Complete
response | 0 |
| Partial response | 1 (5) |
| Stable disease | 11 (50) |
| Progressive
disease | 9 (45) |
| Disease control
rate | 9 (45) |
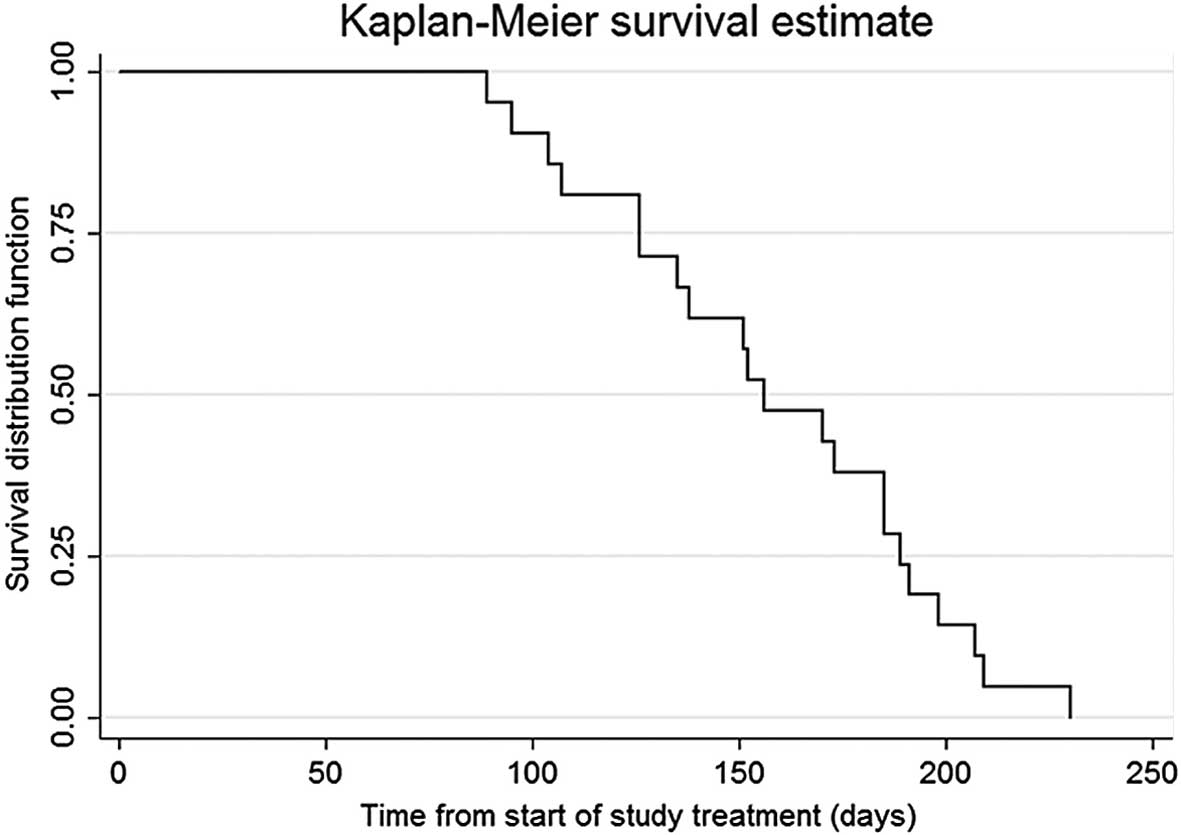
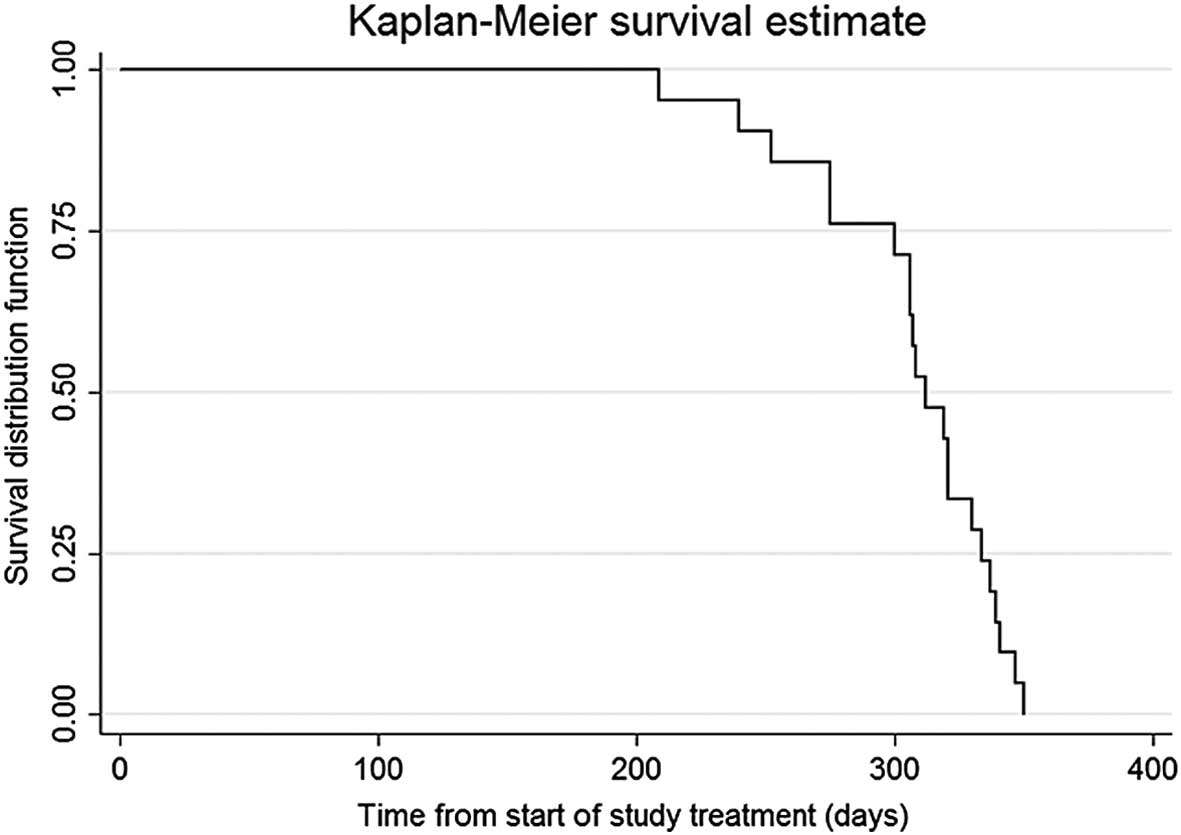
TTP and OS
The median TTP was 5.2 months [95% confidence
interval (CI), 4.2–6.2 months] and the median OS time was 10.4
months (95% CI, 10–11 months) (Figs.
1 and 2).
Toxicity
All patients were evaluable for toxicity. The
overall incidence of treatment-related adverse events (any grade)
was 80% (18 patients). The adverse events that were predominantly
reported were grade 1 or 2; the most common adverse events were
dermatologic, constitutional and gastrointestinal. Grade 1 and 2
toxicity included 20% hyperemia, 25% anorexia and 10% vomiting.
Grade 3 toxicity included fatigue (5%), diarrhea (5%), HFSR (10%)
and hypertension (5%). No grade 4 treatment-related toxicities were
reported.
Discussion
In this phase II trial, the combination of sorafenib
and EHY was well tolerated and showed noteworthy antitumor
activity; a four month PFS rate of 70% was reported, with 50% of
patients achieving SD and 5% achieving PR. The DCR was 45% and the
median TTP and OS time were 5.2 and 10.4 months, respectively. No
grade 4 treatment-related toxicities were reported, while the most
frequently reported grade 3 adverse events were similar to those
reported in previous studies (fatigue, diarrhea and HFSR) (5,6).
These results compare favorably with the sorafenib
phase II study conducted by Abou-Alfa et al (17) in patients with advanced HCC; three
(2.2%) of the 137 treated patients achieved PR, eight (5.8%)
achieved a minor response and 46 (33.6%) achieved SD for at least
16 weeks. The TTP and OS time were 4.2 and 9.2 months,
respectively. In the SHARP phase III trial, sorafenib was found to
improve the OS by 44% in patients with HCC (P=0.0006) versus the
placebo group; the median OS was 10.7 months in sorafenib-treated
patients compared with 7.9 months in those administered with the
placebo. No significant difference was identified between the two
groups in the median time to symptomatic progression (TTSP; 4.1 vs.
4.9 months, respectively; P=0.77). The median time to radiological
progression was 5.5 months in the sorafenib group and 2.8 months in
the placebo group (P<0.001). In total, 2% of patients achieved
PR and 71% achieved SD. The DCR was 43%. The most commonly observed
adverse events in patients receiving sorafenib were diarrhea,
weight loss, HFSR and hypophosphatemia (5). In the phase III Asia-Pacific Liver
Cancer Study, treatment with sorafenib was associated with a
significantly longer OS time (median, 6.5 vs. 4.2 months for
sorafenib and placebo, respectively; HR, 0.57; 95% CI, 0.42–0.79;
P=.0005). The median TTSP was 3.5 months. A total of 3.3% of
patients achieved PR and 54% achieved SD. The DCR was 35.3%. The
most frequent grade 3/4 drug-related adverse events reported for
sorafenib were HFSR (10.7%), diarrhea (6%) and fatigue (3.4%)
(6). Since sorafenib was found to
improve OS in these two phase III trials, sorafenib became the
standard of care for advanced HCC; however, the benefits remain
modest. Combining this drug with locoregional or systemic therapy
may improve the outcome of advanced HCC patients.
As previously reported, experimental data for
sorafenib indicate that hyperthermia inhibits angiogenesis and
increases apoptosis. Furthermore, certain in vitro studies
have shown that hyperthermia may alter the properties of metastatic
potential in cancer cells and inhibit tumor metastasis due to the
inhibition of hypoxia and TGF-β1-induced epithelial-mesenchymal
transition in HepG2 HCC cells (17,19).
The heat sensitivity of this tumor cell line decreases with rising
percentages of the hepatic stellate LX-1 cell line (model of liver
fibrosis) in coculture (20,21).
Few studies have analyzed EHY treatment in HCC and
the efficacy of targeted therapy plus EHY remains unknown. Breast
cancer in vitro and in vivo studies have indicated
that mild hyperthermia sensitizes cancer cells to PARP-1 inhibitors
(22,23).
In our previously reported study, the feasibility
and safety of combining a chemical treatment (transarterial
chemoembolization) with a physical treatment (radiofrequency
ablation) in patients with hepatic malignancies was investigated.
Therefore, we further hypothesized that combining a chemical
systemic drug with a physical locoregional treatment may exhibit a
synergistic effect (24). In the
current study, a phase II trial was conducted in advanced HCC
patients to evaluate whether EHY may potentiate the effect of
sorafenib through reduction of angiogenesis and increased
apoptosis.
These combinations act on the microenvironment of
tumor cells. The multikinase inhibitory profile of sorafenib leads
to effects in cancer cells, as well as the ECs and pericytes of
tumor vasculature. First, EHY determines a energy absorption in the
extracellular fluid and then, through a temperature gradient
between the extracellular and the intracellular compartment, a
destruction of tumor cells is observed (4,7).
The results of the present study showed that the
sorafenib plus EHY combination is feasible and well tolerated; no
major complications were observed. The initial findings suggested
that this combination offers a promising option for advanced HCC,
representing a new and challenging area for future clinical study.
Further large studies are required to confirm these preliminary
results.
References
|
1
|
Ferlay J, Shin HR, Bray F, et al:
Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int
J Cancer. 127:2893–2917. 2010.
|
|
2
|
Forner A, Llovet JM and Bruix J:
Hepatocellular carcinoma. Lancet. 379:1245–1255. 2012.
|
|
3
|
European Association For The Study Of The
Liver1; European Organisation For Research And Treatment Of Cancer.
EASL-EORTC clinical practice guidelines: management of
hepatocellular carcinoma. J Hepatol. 56:908–943. 2012.
|
|
4
|
Ranieri G, Gadaleta-Caldarola G, Goffredo
V, et al: Sorafenib (BAY 43-9006) in hepatocellular carcinoma
patients: from discovery to clinical development. Curr Med Chem.
19:938–944. 2012.
|
|
5
|
Llovet JM, Ricci S, Mazzaferro V, et al:
Sorafenib in advanced hepatocellular carcinoma. N Engl J Med.
359:378–390. 2008.
|
|
6
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, et al:
Efficacy and safety of sorafenib in patients in the Asia-Pacific
region with advanced hepatocellular carcinoma: a phase III
randomised, double-blind, placebo-controlled trial. Lancet Oncol.
10:25–34. 2009.
|
|
7
|
Fiorentini G and Szasz A: Hyperthermia
today: electric energy, a new opportunity in cancer treatment. J
Cancer Res Ther. 2:41–46. 2006.
|
|
8
|
Roca C, Primo L, Valdembri D, et al:
Hyperthermia inhibits angiogenesis by a plasminogen activator
inhibitor 1-dependent mechanism. Cancer Res. 63:1500–1507.
2003.
|
|
9
|
Hildebrandt B, Wust P, Ahlers O, et al:
The cellular and molecular basis of hyperthermia. Crit Rev Oncol
Hematol. 43:33–56. 2002.
|
|
10
|
van der Zee J: Heating the patient: a
promising approach? Ann Oncol. 13:1173–1184. 2002.
|
|
11
|
Horsman MR: Angiogenesis and vascular
targeting: relevance for hyperthermia. Int J Hyperthermia.
24:57–65. 2008.
|
|
12
|
Ranieri G, Catino A, Mattioli V, et al:
Targeting tumour vascularization from bench to bedside: Some
suggestions for combination with hyperthermia. Cancer
Microenvironment and Therapeutic Implications. Baronzio G,
Fiorentini G and Cogle CR: 1st edition. Springer Science + Business
Media B.V; Dordrecht: pp. 203–219. 2009
|
|
13
|
Therasse P, Arbuck SG, Eisenhauer EA,
Wanders J, et al: New guidelines to evaluate the response to
treatment in solid tumors. European Organization for Research and
Treatment of Cancer, National Cancer Institute of the United
States, National Cancer Institute of Canada. J Natl Cancer Inst.
92:205–216. 2000.
|
|
14
|
Bruggmoser G, Bauchowitz S, Canters R,
Crezee H, et al; ESHO Technical Committee in the Interdisciplinary
Working Group Hyperthermia (IAH) in the German Cancer Society.
Quality assurance for clinical studies in regional deep
hyperthermia. Strahlenther Onkol. 187:605–610. 2011.
|
|
15
|
NCI. Common Terminology Criteria for
Adverse Events v3.0 (CTCAE). http://ctep.cancer.gov/forms/CTCAEv3.pdf.
Accessed January 8, 2009
|
|
16
|
Lacouture ME, Wu S, Robert C, Atkins MB,
et al: Evolving strategies for the management of hand-foot skin
reaction associated with the multitargeted kinase inhibitors
sorafenib and sunitinib. Oncologist. 13:1001–1011. 2008.
|
|
17
|
Abou-Alfa GK, Schwartz L, Ricci S, Amadori
D, et al: Phase II study of sorafenib in patients with advanced
hepatocellular carcinoma. J Clin Oncol. 24:4293–4300. 2006.
|
|
18
|
Cancer Therapy Evaluation Program. Common
Terminology Criteria for Adverse Events, Version 3.0. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
Accessed August 9, 2006
|
|
19
|
Yuan GJ, Li QW, Shan SL, et al:
Hyperthermia inhibits hypoxia-induced epithelial-mesenchymal
transition in HepG2 hepatocellular carcinoma cells. World J
Gastroenterol. 18:4781–4786. 2012.
|
|
20
|
Xu XM, Yuan GJ, Li QW, Shan SL and Jiang
S: Hyperthermia inhibits transforming growth factor beta-induced
epithelial-mesenchymal transition (EMT) in HepG2 hepatocellular
carcinoma cells. Hepatogastroenterology. 59:2059–2063. 2012.
|
|
21
|
Mayrhauser U, Stiegler P, Stadlbauer V,
Koestenbauer S, et al: Effect of hyperthermia on liver cell lines:
important findings for thermal therapy in hepatocellular carcinoma.
Anticancer Res. 31:1583–1588. 2011.
|
|
22
|
Ferrari VD, De Ponti S, Valcamonico F, et
al: Deep electro-hyperthermia (EHY) with or without thermo-active
agents in patients with advanced hepatic cell carcinoma: Phase II
study. J Clin Oncol. 25(S): Abstract 151682007.
|
|
23
|
Krawczyka PM, Eppinkb B, Essers J, Stap J,
et al: Mild hyperthermia inhibits homologous recombination, induces
BRCA2 degradation, and sensitizes cancer cells to poly (ADP-ribose)
polymerase-1 inhibition. Proc Natl Acad Sci USA. 24:9851–9856.
2011.
|
|
24
|
Gadaleta CD, Catino A, Ranieri G, Fazio V,
et al: Single-step therapy - feasibility and safety of simultaneous
transarterial. chemoembolization and radiofrequency ablation for
hepatic malignancies. In vivo. 23:813–820. 2009.
|