1. Introduction
Over the past year, humanity has been facing a challenge to global public health due to the novel coronavirus, SARS-CoV-2. This newly recognized virus belongs to the genus Betacoronavirus and is considered the third most pathogenic virus infecting humans in the 21st century (1). SARS-CoV-2 appeared in December, 2019 in Wuhan, China, and subsequently spread to other countries worldwide, posing a global threat. In late January, 2020, the World Health Organization (WHO) announced the rapid spread of the virus as a global epidemic, and in early March, 2020, the disease was declared a pandemic (2). The main symptoms of the disease are cough, fever and shortness of breath, while in the later stages, there are pneumonia-like symptoms (3), while it can also cause damage to the kidneys and can even cause unexpected mortality. The mortality rate is higher among the elderly (~20%), and >33 million confirmed cases and >1,003,569 deaths have been recorded worldwide due to coronavirus by the end of September, 2020(4).
The COVID-19 pandemic is the first pandemic in history to be caused by a coronavirus (5). The COVID-19 pandemic is primarily a global health emergency with severe consequences, mainly for global public health, as well as for the global economy. To date, no specialized antiviral drug or even the recently developed vaccine can prevent the disease with absolute effectiveness. Thus far, social distancing is considered the most effective strategy to protect public health. Therefore, social lockdown is considered the most effective measure to control the spread of COVID-19(6).
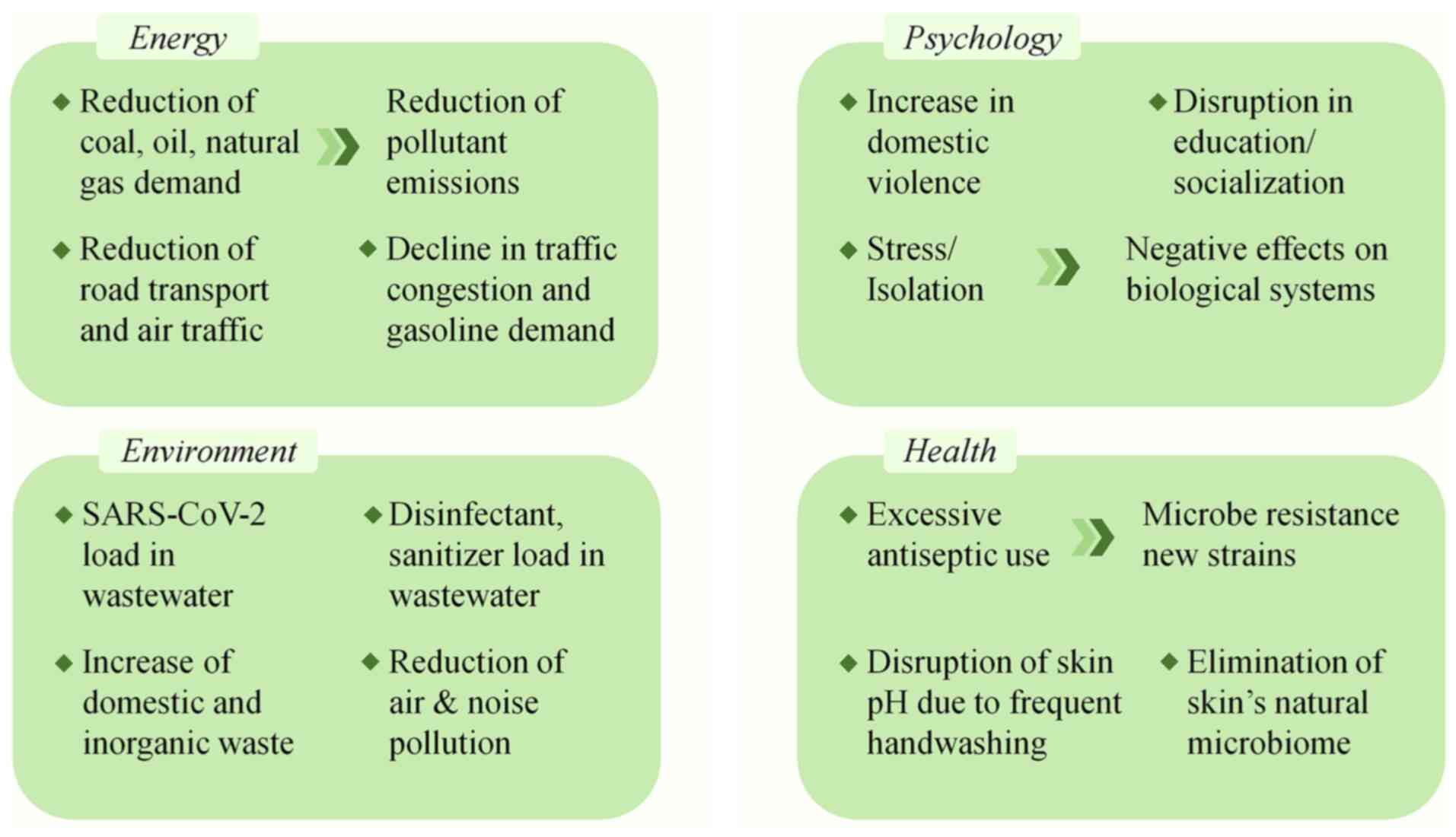
The impact of this change in lifestyle and everyday conditions is evident on the health, financial, social, energy-related and environmental sectors (Fig. 1). According to research, due to lockdown, there has been an increase in the development or severity of mental illnesses (7), such as psychological stress, fear and panic attacks (8). Sleep disorders, such as insomnia and a significant increase in the consumption of psychotropic substances and alcoholic beverages have also been observed, mainly due to concerns regarding virus infection or the loss of family members that are more susceptible in viral infection and belong to high-risk groups (9). In addition, some of the effects of the global lockdown on the financial sector are the displacement of workers, the closure of businesses and the crashes of stocks, where according to the International Monetary Fund (IMF), the impact of COVID-19 will lead to a reduction in global economic growth by 3% (10). However, despite the negative effects of quarantine on the socioeconomic and health domains, various positive results have been recorded, mainly in the environmental sector, as there has been a reduction in air and water pollution due to the reduction of the industry activity and traffic restrictions, thus leading to improved urban sustainability (11,12). The present review aimed to analyze the impact of global social lockdowns in the context of the COVID-19 pandemic, focusing on its impacts on health, socio-psychological, economic sectors and the environment.
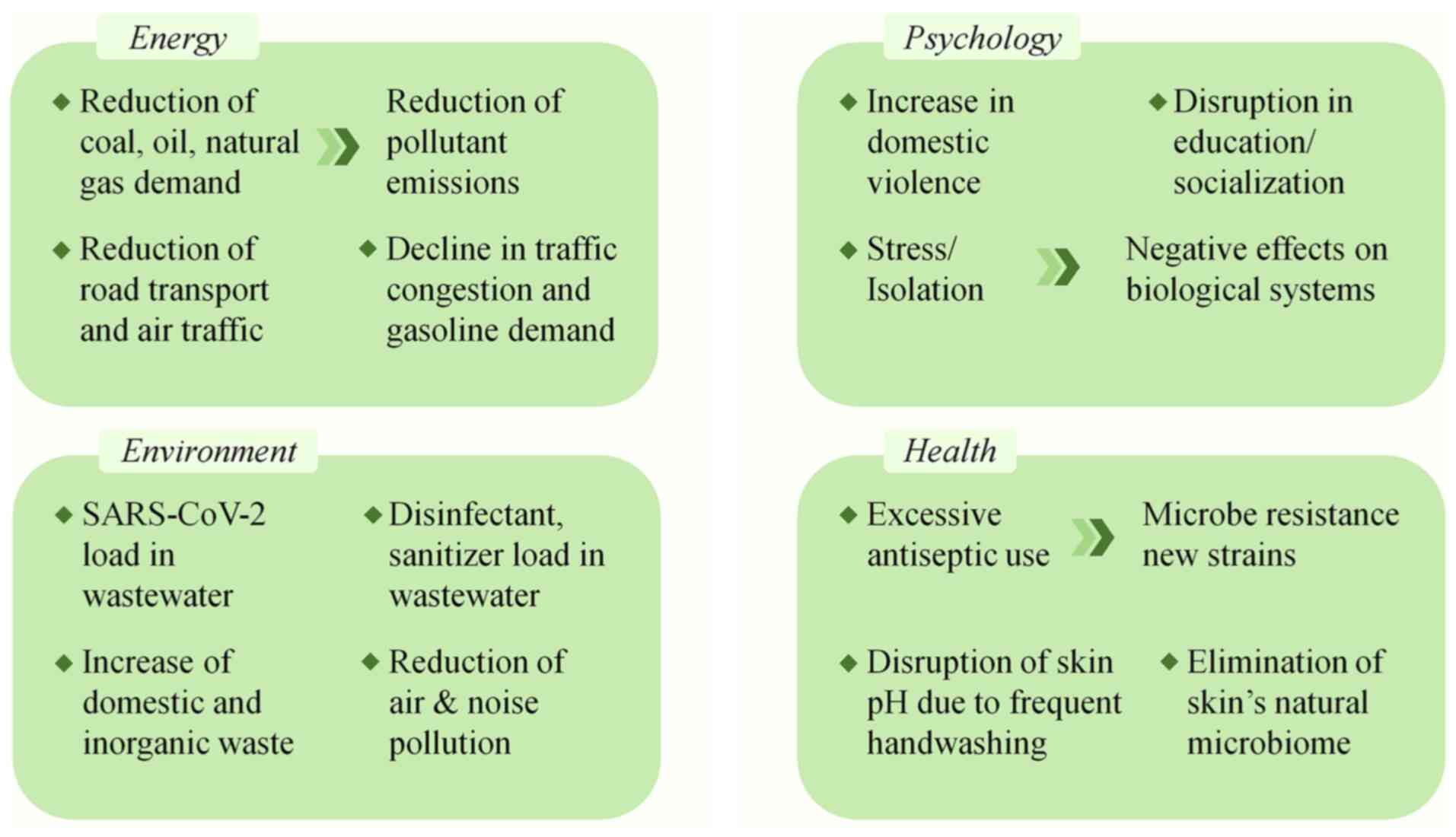 |
Figure 1
Impact of the change in lifestyle and everyday conditions due to the pandemic and social lockdown on health, financial, social, energy-related and environmental sectors.
|
2. Energy impacts
Faced with the rapid transmission of SARS-CoV-2, countries worldwide have taken measures to slow down the infection rate and alleviate the pressure on their health systems. In a number of cases, authorities have declared widespread lockdowns, temporarily shutting down local industries, businesses, institutes, and imposing travel restrictions. In parallel, work has largely turned remote, with an increasing number of individuals working online from their homes. The observed shifts in industrial activity and work practices with the parallel restriction of local and global transport can, in turn, impact the levels of energy consumption and subsequent emissions.
In a report published by the International Energy Agency for the first quarter of 2020, the global energy demand declined by 3.8% (net change in quarterly oil demand in 2020 and 2021 relative to 2019 shown in Table I) (13). More specifically, coal demand was reduced by 8%, oil demand by ~5%, and natural gas by ~2%. Global road transport marked a 50% decline by the end of March, 2020, while global air traffic was reduced by 60% by the end of the first quarter of 2020, with percentages reaching as high as 90% in some European countries (13). Given its widespread use in commercial, domestic, transportation and industrial uses, the oil demand was severely negatively affected during the pandemic, with an estimated decline of 5.6 millions of barrels per day (mb/d) reported by the IEA for the first quarter of 2020. Furthermore, jet fuel and kerosene demand presented an estimated decline of 27% in March, following the implementation of widespread travel bans and aviation traffic restrictions. The same report detailed a decline in traffic congestion and gasoline demand following the establishment of lockdown measures and mobility restrictions, with the gasoline demand decline reaching 1,7 mb/d in the first quarter of 202 on a global scale (13). The study by Gillingham et al (14) explored the effects of the pandemic on energy consumption in the US, reporting a 50% reduction in jet fuel and a 30% reduction in the levels of gasoline. Additionally, natural gas consumption in commercial and private establishments was found to be decreased by ~20%. Of note, although it originally decreased, electricity consumption was shown to have returned to its standard levels by June, largely due to elevated electricity demands as individuals spent an increasing amount of time at home (14). An electricity market report by IEA for the third quarter of 2020 reported the recovery of electricity demand after dropping under early lockdowns (15). More specifically, China's electricity demand was reported to have rebounded entirely, while other major markets such as Europe and the US showed similar recovery patterns, but not to the same levels as in 2019(15).
 |
Table I
Net change in quarterly oil demand (Qi) in 2020 and 2021 relative to 2019.
|
Table I
Net change in quarterly oil demand (Qi) in 2020 and 2021 relative to 2019.
| Yearly demand |
USA |
China |
India |
EU |
Other |
Net |
| 2020 Q1 |
-1,0 |
-1,5 |
-0,2 |
-0,6 |
-1,7 |
-5,1 |
| 2020 Q2 |
-4,4 |
+0,5 |
-1,2 |
-2,3 |
-8,7 |
-16,3 |
| 2020 Q3 |
-2,4 |
+0,7 |
-0,5 |
-1,3 |
-4,5 |
-7,9 |
| 2020 Q4 |
-1,9 |
+0,7 |
0,0 |
-1,2 |
-3,4 |
-5,8 |
| 2021 Q1 |
-1,8 |
+1,2 |
0,0 |
-1,3 |
-3,1 |
-5,1 |
| 2021 Q2 |
-1,1 |
+1,2 |
-0,1 |
-0,8 |
-3,0 |
-3,8 |
| 2021 Q3 |
-0,6 |
+1,2 |
0,0 |
-0,8 |
-2,0 |
-2,3 |
| 2021 Q4 |
-0,4 |
+1,1 |
0,0 |
-0,3 |
-1,5 |
-1,0 |
Changes in transport activity and oil consumption exert a prominent effect on environmental quality, mainly by reducing the emissions of air pollutants. Nitrogen dioxide (NO2) is a pollutant emitted mainly through fossil fuel use and has been found to be associated with severe health issues (16). As presented in the study by Muhammad et al (17), data collected by NASA and the European Space Agency (ESA) evidenced the improvement in environmental quality and the reduction of NO2 emissions by 30% during the COVID-19 pandemic. The reduction levels ranged from 20-30% in China and European countries, such as France, Italy and Spain, and up to 30% in the US. Carbon dioxide (CO2) emissions followed a similar pattern, with a reduction of ~15% in the US daily CO2 emissions (14), and a similar 17% reduction in emissions globally by April (18). In the first quarter of 2020, the IEA reported the largest declines of CO2 emissions in regions that had suffered the earliest impacts of COVID-19, such as China and Europe, with an 8% decline (13). Overall, the limitations of transport that were implemented during the COVID-19 pandemic have led to unprecedented changes in the global field of energy demand and supply, with multi-faceted effects on the environment and the global economy. The positive impact of energy-saving on the environment quality can serve as an example of the importance of a more sustainable approach in the field of energy and fuel.
3. Environmental impacts
The production of different types of waste is indirectly the cause of a number of environmental concerns (19). The detection of SARS-CoV-2 in sewage (20,21) indicated viral persistence in water-related environments and wastewater treatment plants. Protocols for the disinfection in systems of drinking water and wastewater treatment plants are already in place for a variety of pathogenic organisms, such as bacteria and viruses. Coronaviruses are enveloped, single-stranded RNA viruses that exhibit surface glycoproteins, including the spike protein that enables the binding to ACE-2 receptors within the host body (22). While it is considered that established disinfection protocols, such as ultraviolet radiation and chlorination are sufficient in order to remove SARS-CoV-2 during the process of wastewater treatment, the highest achievable level of efficacy is necessary, particularly in areas where poorly treated wastewater may be discharged to surface water bodies. Efficient disinfection and safe disposal are even more important when considering the increasing production of domestic wastewater, as an increasing number of individuals self-isolate and there is a shift to remote work at home. Furthermore, the changing load within the wastewater, comprising of products, such as disinfectants and sanitizers, harbors dangers for both the environment, as well as for the potential emergence of resistance among pathogens, such as bacteria.
The quarantine conditions, that have occurred in the majority of countries worldwide, indirectly result in an increase in domestic waste, as consumers have exhibited increased domestic online shopping activity. In addition to domestic waste, inorganic waste has also increased, mainly due to the rise of the online shopping of packaged food; in addition, a significant increase has been reposted in hospital and medical waste (23). This unprecedented situation leads to significant problems in the management, recycling, and implementation of waste collection services. Thus, as there is no clear information on the retention time of SARS-CoV-2, waste disposal is a major environmental concern (24). During the pandemic, large amounts of domestic and hospital waste, mainly plastic waste, were generated and this has accumulated. This acts as a deterrent to ongoing efforts to reduce plastic waste and its disposal to the environment. Recycling projects have been suspended in various cities due to the pandemic and fears of the virus spreading, while in affected European countries, waste management is limited; for example, in Italy, where the collection of waste from infected citizens has been banned (25). In general, further efforts must be made to identify alternatives to plastics that are widely used (25).
The source of atmospheric NO2 is mainly the burning of fossil fuels, such as coal, oil and gas, and the largest percentage of its atmospheric emissions in the cities is due to emissions from ~80% of motor vehicles (26). In addition, the refining of petroleum and metals, the production of electricity through coal combustion, and other food production and processing industries are also sources of significant emission rates of this molecule. Nitric oxide (NO) and NO2 are responsible for the formation of acid rain that is toxic to the environment (25), and according to the WHO, NO2 is one of the six typical air pollutants. For this reason, atmospheric NO2 is used as an accurate measure to determine whether the COVID-19 epidemic is affecting environmental pollution. NO2 is an atmospheric pollutant that leads to photochemical smog formation and has significant effects on human health (27). Exposure to high concentrations of NO2 can lead to respiratory symptoms, such as cough, wheezing, flu, etc., as well as to the deterioration of respiratory diseases, such as asthma. According to the ESA, which is responsible for monitoring air pollution, it was predicted that global NO2 emissions would increase by ~1% on a 5-year basis without quarantine conditions. However, due to social lockdown, which has led to a reduction in both motor vehicle traffic and industrial production, there has been a significant reduction in global greenhouse emissions (25). Respectively, the reduction of CO2 emissions is also a positive effect of the lockdown. Global CO2 emissions decreased by 17% by April 7, 2020 compared to the average emission level in 2019(18).
Particulate matter are also important air pollutants. Their main sources are pollutants emitted from vehicles, factories and the burning of fossil fuels (28), as well as from grilling, cigarette smoking and burning wood in a fireplace or stove. These particles are categorized into two categories according to their diameter, which include PM10, which are inhalable particles with a diameter of ≤10 µm, and PM2.5, which are equally inhalable particles with a diameter of ≤2.5 µm. Exposure to PM2.5 causes severe health issues, such as heart rate abnormality, increased asthma, decreased lung function and increased respiratory symptoms. However, during quarantine, both PM10 and PM2.5 levels have been significantly reduced and in particular, a study conducted in 22 cities in India recorded a reduction of PM10 and PM2.5 by 43 and 31% (25).
In addition to the reduction of air pollution during social lockdowns, a significant reduction has also been observed in noise pollution. Noise is one of the most important sources of disturbance to both humans and the environment, as it can cause health issues and can change the physical condition of ecosystems (29). Sleep disorders, adverse effects on the heart and metabolic system, and cognitive impairment in children are some of the major consequences of long-term noise exposure. According to the European Environment Agency, noise pollution is the cause of 48,000 new cases of heart disease and 12,000 premature deaths each year, as well as a chronic sleep disorder for 6.5 million individuals. However, during quarantine, this new lifestyle has led to a significant reduction in noise levels, as commercial activities have almost completely stopped, and private or public transport has been significantly reduced (25).
Environmental compounds and atmospheric pollutants have been shown to exert epigenetic effects, namely in terms of fertility and reproduction, as well as during fetal development. Exposure to air pollutants such as O3 and NO2 in the prenatal stage has been associated with neonate DNA methylation, with the affected genes pointing to a link between prenatal exposure to pollutants and alterations in inflammatory, mitochondrial and metabolism-related biological processes (30). Fuel industry hydrocarbons, such as JP-8, can promote epigenetic transgenerational inheritance of diseases such as obesity, reproductive disorders, and gamete epimutations. Lastly, the epigenetic impact of environmental stressors has been demonstrated through the identification of aberrant levels of circulating epigenetic modifications in individuals residing in urban zones with significant air pollution (31).
4. Psychological strain and epigenetic impact
The COVID-19 pandemic has presented immense challenges for the general population with profound psychosocial effects (32). The most commonly implemented measures, which are national-level lockdowns and implementation of social-distancing rules, have been sources of anxiety, anger, confusion, and grief, and have led to the emergence of symptoms of depression (33,34). Moreover, existing socioeconomic and racial divides have an effect on the consequences of COVID-19 infection in individuals, which also affects the effectiveness of the measures mentioned above (34,35).
The social implications of COVID-19 are most evident in households. Domestic violence appears to increase following the implementation of lockdown (36). The most vulnerable individuals to domestic abuse are children and their mothers (37). There are multiple factors that can lead to such an increase. Firstly, the economic distress created by the increasing unemployment rates, the loss of income, or the lack of social support increases emotional distress and may lead to violent behavior in couples. Moreover, increased interactions inside the household due to the increasing amount of time spent with other household members may expose behaviors that are not compatible within a family setting. Lastly, the increase in time spent together also decreases the ‘safe-time’ when a victim of abuse is alone (38). These factors are further exacerbated due to the decreased accessibility to social support services (39). Therefore, it is essential to devise specific policies to combat these effects of the pandemic.
The social implications of the pandemic are also quite evident in specific age groups, particularly among children, teenagers and young adults (40,41). Disruption in education and socialization appears to cause multiple issues (42). For numerous students, educational institutions provide important services that allow the report of abuse, violence and harm. These services are essential since, as mentioned above, such incidences have increased during the pandemic. Moreover, a number of students with socioeconomic disadvantages and disabilities rely on such institutions for nutrition and health support (43). Education itself is negatively affected, since not all students have the resources needed for digital communication, while a barrier in the educational relationship is created between teachers and students (43). Lastly, some of the most important problems that arise in children, teenagers and young adults are due to the lack of social interaction. The decrease in social interaction negatively affects growth and learning, while it may lead to the loss of a sense of community (44). Specifically, children may be more vulnerable since the toxic stress associated with social isolation may lead to losses in brain development and long-term impairment of cognition, physical, and mental health (45). These facts indicate the need to develop distinct strategies for specific age groups.
All these social effects of COVID-19 also have a biological impact. Acute and chronic stress have deleterious effects on multiple biological systems, including the cardiovascular system, the immune system and cognition (46). Persistent stress also activates the hypothalamic-pituitary-adrenal axis (HPA) and leads to the release of cortisol (32). This activation of this mechanism is crucial as cortisol levels seem to influence the outcome of possible SARS-CoV-2 infection. Specifically, patients with a fatal outcome have displayed higher serum cortisol levels (47). Consequently, the psychosocial effects of COVID-19 can themselves worsen the outcome of a possible infection. It is, thus essential to extensively study these effects.
Aiming at reducing the negative psychological, physical and social consequences of the pandemic, that are mentioned above, the positive impact of physical exercise on psychological health is proven. Nevertheless, according to the literature, a significant reduction in physical activity has been observed during the COVID-19 quarantine, thus resulting in a significant reduction in the psychological well-being of individuals of all age groups. Individuals who exercise regularly have generally been shown to be less likely to develop symptoms of depression and anxiety due to changes in the HPA axis and mediated endogenous opioid system, which are involved in stress, mood and emotional responses (48,49). In addition, increased levels of brain-derived neurotrophic factor (BDNF) have been reported following exercise, which is the brain's most abundant neurotrophin and exerts a positive effect on stress and depressive disorders. The lack of access to exercise and physical activity due to quarantine has had significant effects on mental health, compound stress or anxiety in isolation from normal social life. Thus, the benefits of physical exercise in psychological well-being prove to be very useful, particularly in times of stress, crisis, and fear, such as the period of the COVID-19 pandemic that is currently affecting humanity (48,49).
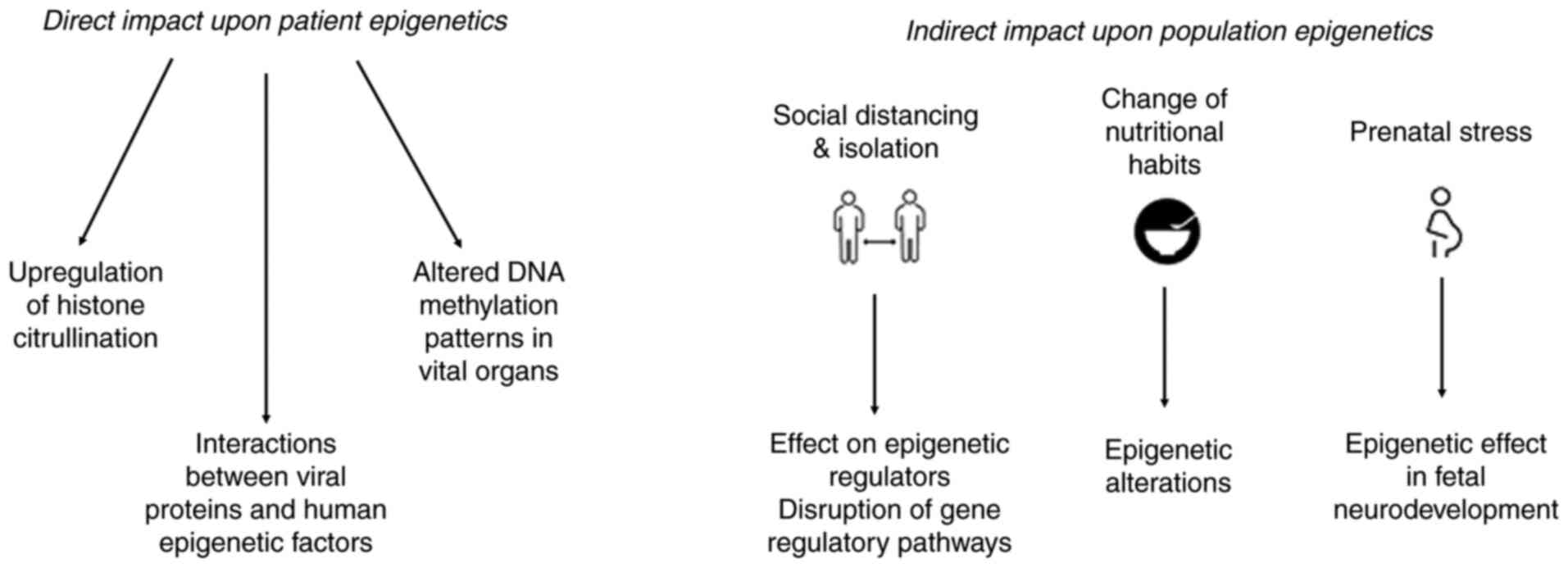
During the current pandemic, the undergoing stressors, worldwide instability and the deterioration of the well-being of individuals, the epigenetic effects should also be considered. Alterations in epigenetic patterns can be triggered by environmental, nutritional, social and psychological factors, all of which are currently affected by the COVID-19 pandemic. Nutritional habits have changed due to social lockdowns and the accessibility of various nutrients, and even though no consequent studies have been conducted, it is well known that changes in dietary patterns can cause epigenetic alterations, as nutrients are involved in brain function and development, and influence DNA methylation and histone modifications (50,51). Generally, in nutrition epigenetics, food is considered an environmental exposure of the organism. More specifically, the nutrients in food that enter the body constitute either on their own, or as determinants of maternal metabolism, information about the world in which a body will be born or raised. This is particularly evident during the critical growth periods of the body, as food molecules form the metabolic systems with which the body will process food in the future (52). This fact is more evident in cases of insufficient maternal care and nutrition, that have an impact on the epigenetic formation of the offspring and are reflected in the methylation state of their DNA (53). Thus, nutrients form the environment in which the activity of the genome and the physiology of the body are formed (52).
As previously discussed, social distancing can have an impact on the psychology and health status of individuals. However, the epigenetic imprint during stressful periods and prolonged social isolation can have long-term consequences and even a transgenerational effect (54). It has been shown that 15 genetic variants enriched for epigenetic modifications are strongly associated with loneliness and chronic isolation and regulate gene expression in the brain (55). Additionally, isolation has been shown to affect a wide range of epigenetic regulators, including transcription factors and ncRNAs, and to disrupt gene regulatory pathways (56), and is also involved in all reward deficiency syndrome (RDS) addictive behaviors (57). Another point considered is the impact of prenatal stress and the epigenetic effect in the neurodevelopment of the offspring of pregnant women during this period, where long-term exposure to stress can cause is linked to increased risk of neuropsychiatric disorders (58). The general epigenetic risk of extensive social distancing and stress is alarming, and individuals are anticipated to experience a wide range of mental health issues with longstanding consequences.
5. Health impacts
In order to reduce the transmission of the coronavirus strain SARS-CoV-2 and control the COVID-19 pandemic, governments in cooperation with the WHO have applied a range of optional or mandatory measures, along with social distancing, in public places, which include the use of mask and antiseptics.
Although there is a large controversy on whether a mask can protect someone from an infection or not, recent research suggests that they can help to prevent the spread of viruses. A study performed in 2013 revealed that masks led to a significant reduction in the number of seasonal influenza virus aerosols sprayed into the air via droplets exhaled from infected individuals; in that case, masks produced a 3.4-fold reduction in viral aerosol shedding (59). Respectively, results from various epidemiological and clinical studies assessing the effectiveness of masks in reducing disease transmission have led to the conclusion that mask-wearing can provide some significant benefits for public health (60-64). Masks also protect healthy individuals against aerosol particles emitted from infected individuals, such as those emitted during sneezing and coughing. Experts insist on wearing and properly removing a mask in order to eliminate viral transmission through the nose, mouth and eyes with contaminated hands. Individuals who are not vigilant with the use of masks face a high risk of infection (65-67). In addition, the use of masks may lead to undesirable results for the general population. Aside from this, the WHO insists that wearing a mask does not lead to difficulties in breathing when properly worn and does not cause CO2 intoxication or oxygen deficiency (68).
Hand hygiene is the second crucial factor for virus prevention along with the use of masks (69). Ethanol is the most commonly used substance in commercial antiseptics. The majority of products contain 70 to 90% v/v alcohol in water solutions. However, its benefits for public health, frequent hand washing, and the excessive use of antiseptic solutions can severely damage the skin, leading to irritations and dehydration, as natural oils are removed from the skin (70). Doctors claim that an increase in dermatitis of the hands has been noted since the beginning of the pandemic (71).
The immune system represents the optimal defense against infection as it supports the natural defense of the body against pathogens, such as viruses, bacteria, fungi and protozoa, and resists infections. The human body has a two-line defense system against pathogens. The skin, the largest human organ, represents the body's first line of defense and hosts a great number of beneficial microbes, which consist the natural flora. This microbiome is the greatest barrier on the surface of the skin. The skin microbiome is a complex collection of distinct micro-ecosystems specifically adapted to thrive in the conditions encountered across different body sites (72).
It has been proven that frequent handwashing with antimicrobial soaps and the excessive use of antiseptics disrupt the natural environment of the skin, altering the pH level, a crucial factor for microorganisms. In addition, ethanol dissolves lipid membranes and denatures proteins of the bacterial cell wall and cell membrane. As a result, the elimination of the natural microbiome is observed. In addition, the excessive use of alcohol-containing antiseptics could increase the resistance of certain germs and can thus create new strains that could threaten public health.
In addition to the aforementioned strategies of defense against pathogens, in this context, exercise has been shown to play an important role in strengthening the immune system against viruses that mainly infect the respiratory system. According to a study conducted in Italy, it was demonstrated that moderate physical exercise can promote the treatment of respiratory infections caused by viruses, such as coronavirus, thus promoting the proper functioning of the immune system and improving the pathological results (73). This occurs as exercise causes the release of catecholamines and glucocorticoids, which are stress hormones that reduce excessive local inflammation in the respiratory tract. In parallel, exercise, through the secretion of anti-inflammatory cytokines, such as IL-4 and IL-10, promotes the transition from a T helper type 1 (Th1) cell population to a T helper type 2 (Th2) population, thus avoiding the excessively prolonged activity of Th1 against the pathogen, which can lead to cell damage and necrosis. In summary, regular and balanced exercise leads to improved antibacterial and antiviral immune response and reduced inflammation through stimulated circulation, both between the lymphoid tissues and the bloodstream, and innate immune system agents, including immunoglobulins, neutrophils, cytokines, NK cells and T- and B-lymphocytes, which promotes more effective inspection against pathogens, cancer cells, and inflammatory mediators (73).
On the other hand, it should be stressed that due to the measures referred, there has been a reduction in the transmission of other pathogens. Although the data are limited and are derived from only a short period of time, experts claim that infections from other viruses such as those which cause seasonal influenza and gastroenteritis are also reduced (74,75).
From the scope of the view of epigenetics, the COVID-19 pandemic has already radically altered the lifestyles of individuals, leading to the possibility of a more permanent change in the future (76). However, this new way of life may leave humans vulnerable to epigenetic alterations. The frequent use of masks and frequent hand washing, which are used extensively to protect against coronavirus transmission, have created, in a number of individuals, a variety of dermatological conditions, such as psoriasis, which is a chronic inflammatory skin disease, and atopic dermatitis. According to a study that examined the role of epigenetics in skin control and its association with skin pathologies, it was found that in the case of psoriasis, there was hypermethylation and a decrease in p16INK4A levels, where it is found mainly in affected areas of the skin than in unaffected ones. Accordingly, in the case of atopic dermatitis, decreased levels of DNA methyltransferase 1 (DNMT1) were observed in the blood of infected patients, suggesting that DNA methylation levels may contribute to the pathogenesis of this disease. Finally, according to the results of that study, the proliferation and differentiation of skin cells can be modified by epigenetic regulators (77). Thus, environmental conditions and factors can affect an organism's epigenetic modifications, such as DNA methylation and histone modifications, through the direct activation or deactivation of genes in response to a stimulus or environment. These changes are likely to be inherited from one generation to the next, thus affecting skin health. For this reason, it is important to further study the epigenetic alterations that occur mainly in the skin cells through the extensive use of masks and hand washing, and lead to pathological dermatological conditions.
6. Conclusion
By the end of 2019 and to date, the world is experiencing an unprecedented situation of the 21st century. Ongoing research is being performed to identify effective drug targets to treat this highly contagious virus (78-83). In addition to the proteins encoding the virus, several studies have focused on the search for and identification of non-coding RNAs involved in the SARS-CoV-2-induced inflammatory response with the aim of finding new specific prognostic biomarkers and therapeutic targets in patients with COVID-19(84). Epigenetic configurations involving non-coding RNAs (ncRNAs), DNA methylation and histone acetylation are known to be involved in inflammatory cytokines and the inflammatory complex, including IL-6, tumor necrosis factor α (TNF-α) and the NLR family pyrin domain containing 3 (NLRP3) inflammasome (85). Therefore, the design of anti-inflammatory drugs to target inflammatory cytokines, particularly IL-6 and the inflammatory complex, may be a promising strategy for the treatment of SARS-CoV-2(86). An increasing number of studies have demonstrated that long ncRNAs (lncRNAs) play a key role in the development of inflammatory diseases, as they are strongly involved in the regulation of NLRP3 inflammasome and IL-6 signaling (87), while they are involved in innate immune responses through their association with the IFN mechanistic pathways (88). Therefore, understanding the effects of differential expression and the modes of action of long non-covalent DNAs will greatly influence the fields of immunology and infectious diseases.
Despite intensive research worldwide, no highly specific antiviral drug has been developed, and the recently developed vaccine is promising, although there is still no clear evidence of its effectiveness (89). For this reason, social distancing and lockdowns remain effective ways of protecting public health (90). The new living conditions evidently affect not only the individuals themselves (individually and socially), but also have impacts on the energy, economic and environmental sectors. The present review reports the effects of quarantine on health, energy, environmental pollution and the socioeconomic sector. In the socio-economic sector, the global pandemic results in higher unemployment and poverty rates, lower oil prices, distorted education sectors, changes in the nature of work, and increased risks for healthcare workers (91,92). Along with this global economic situation, there has been an increase in domestic violence and the occurrence of mental illnesses, such as stress, insomnia, anger and panic attacks (93). On the other hand, the impact on the energy sector includes an increased domestic energy demand due to reduce mobility and a change in the working environment. Global lockdowns and traffic congestion have reduced the demand for industrial and commercial energy. This reduction in demand and traffic has resulted in significant reductions in NO2, NO, CO2, PM and environmental noise emissions and, consequently, a significant reduction in environmental pollution (94). Finally, the measures applied in health, including the use of mask and hand hygiene, have, generally, a positive impact on pandemic control. Masks can successfully block droplets containing the virus to spread (95). However, the misuse of masks can lead to opposite results for public health. As regards hand hygiene, although it is necessary, excessive hand washing and antiseptic use leads to dermatological issues and weakens the immune system. In addition, when antiseptics are applied for a long period of time, new microbial strains that are more resistant may threaten humanity. In conclusion, social lockdowns have significantly affected the psychosynthesis and habits of individuals, as well as their epigenetic profile and the ongoing changes in society and the environment should be well-considered for their long-term consequences in all levels discussed, from the molecular basis of epigenetic modifications to the global impact on health, social, economic, and environmental factors.
In summary, all the changes that have occurred due to the COVID-19 quarantine, both environmental, and in the daily life, psychology and health of humans, have a significant epigenetic impact (Fig. 2). Epigenetic modifications are responsible for regulating gene expression in response to an environment or stimulus. Thus, the new lifestyle that includes changes in exercise, diet, habits, sociability and human psychology, combined with the environmental changes that have occurred during lockdowns, such as the reduction of air pollution, can lead to epigenetic modifications in the human genome which may be passed on to future generations. Finally, epigenetics also plays an important role in the process of discovering pharmacological targets and prognostic biomarkers for the treatment of this virus, as it focuses on non-coding RNAs, DNA methylation and histone modifications to factors involved in the immune and inflammatory response, such as cytokines.
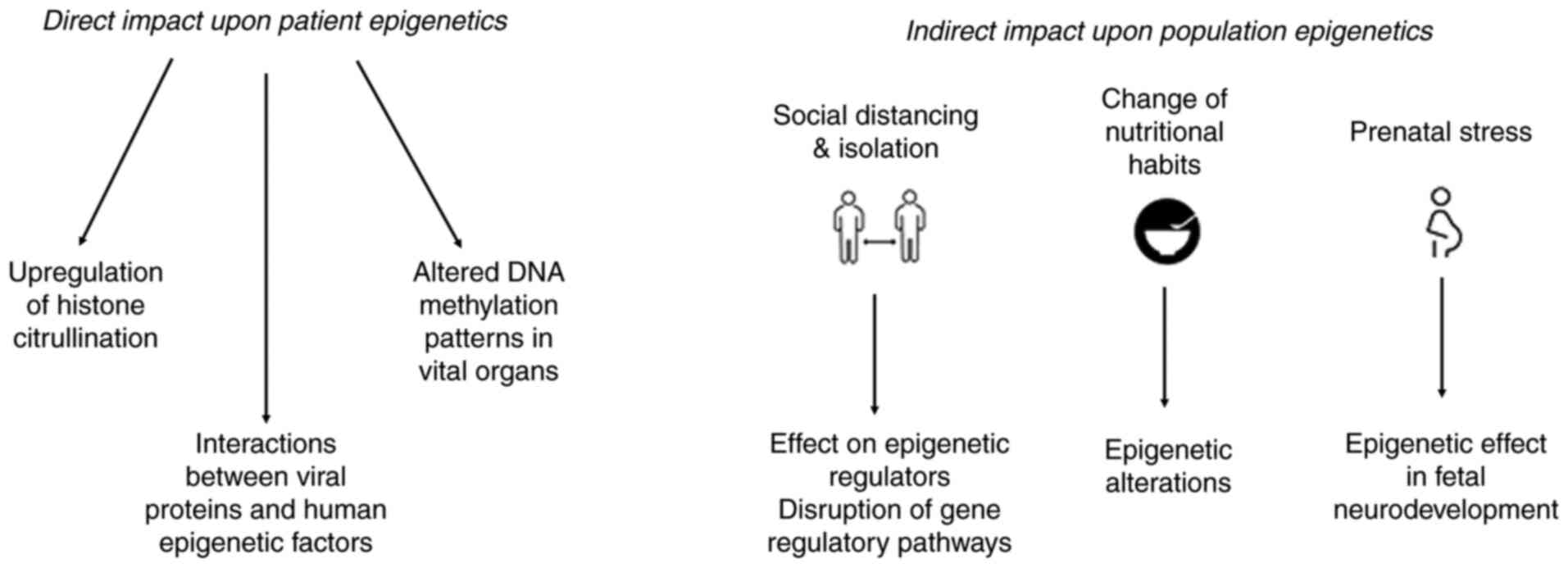 |
Figure 2
Summary of the changes that have occurred due to the quarantine measures for the COVID-19 pandemic. This has led to changes in the environment, and to the daily life, psychology and health of humans, exerting a significant epigenetic impact.
|
Acknowledgements
Not applicable.
Funding
The authors would like to acknowledge funding from the following organizations: i) AdjustEBOVGP‑Dx (RIA2018EF‑2081): Biochemical Adjustments of native EBOV Glycoprotein in Patient Sample to Unmask target Epitopes for Rapid Diagnostic Testing. A European and Developing Countries Clinical Trials Partnership (EDCTP2) under the Horizon 2020 ‘Research and Innovation Actions’ DESCA; and ii) ‘MilkSafe: A novel pipeline to enrich formula milk using omics technologies’, a research co-financed by the Figure 2. Summary of the changes that have occurred due to the quarantine measures for the COVID‑19 pandemic. This has led to changes in the environment, and to the daily life, psychology and health of humans, exerting a significant epigenetic impact. 8 PAPAKONSTANTINOU et al: COVID-19 GLOBAL SOCIAL LOCKDOWNS European Regional Development Fund of the European Union and Greek national funds through the Operational Program Competitiveness, Entrepreneurship and Innovation, under the call RESEARCH‑CREATE‑INNOVATE (project code: T2EDK‑02222).
Availability of data and materials
Not applicable.
Authors' contributions
All authors (EP, KP, TM, KID, AMP, FB, GPC, EE and DV) contributed to the conceptualization, design, writing, drafting, revising, editing and reviewing of the manuscript. All authors confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
GPC is the Editor in Chief of the journal, and DV and EE are Editors of the journal. However, they had no personal involvement in the reviewing process, or any influence in terms of adjudicating on the final decision, for this article. The other authors declare that they have no competing interests.
References
|
1
|
El Zowalaty ME and Järhult JD: From SARS to COVID-19: A previously unknown SARS-related coronavirus (SARS-CoV-2) of pandemic potential infecting humans-call for a one Health approach. One Health. 9(100124)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chowdhury MA, Shuvho MBA, Shahid MA, Haque AKMM, Kashem MA, Lam SS, Ong HC, Uddin MA and Mofijur M: Prospect of biobased antiviral face mask to limit the coronavirus outbreak. Environ Res. 192(110294)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, et al: First case of 2019 novel coronavirus in the united states. N Engl J Med. 382:929–936. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Abdullah S, Mansor AA, Napi NNLM, Mansor WNW, Ahmed AN, Ismail M and Ramly ZTA: Air quality status during 2020 Malaysia Movement Control Order (MCO) due to 2019 novel coronavirus (2019-nCoV) pandemic. Sci Total Environ. 729(139022)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
El Zowalaty ME, Young SG and Järhult JD: Environmental impact of the COVID-19 pandemic-a lesson for the future. Infect Ecol Epidemiol. 10(1768023)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Paital B, Das K and Parida SK: Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ. 728(138914)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhai Y and Du X: Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 288(113003)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Blake H, Bermingham F, Johnson G and Tabner A: Mitigating the psychological impact of COVID-19 on healthcare workers: A digital learning package. Int J Environ Res Public Health. 17(2997)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Severo EA, de Guimarães JCF and Dellarmelin ML: Impact of the COVID-19 Pandemic on environmental awareness, sustainable consumption and social responsibility: Evidence from generations in Brazil and Portugal. J Clean Prod. 124947:2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
IMF: World Economic Outlook, April 2020: The Great Lockdown. Journal, 2020.
|
|
11
|
Arora S, Bhaukhandi KD and Mishra PK: Coronavirus lockdown helped the environment to bounce back. Sci Total Environ. 742(140573)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Jiang P, Fu X, Fan YV, Klemeš JJ, Chen P, Ma S and Zhang W: Spatial-temporal potential exposure risk analytics and urban sustainability impacts related to COVID-19 mitigation: A perspective from car mobility behaviour. J Clean Prod. 279(123673)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
IEA: Global Energy Review 2020, IEA Paris, 2020a.
|
|
14
|
Gillingham KT, Knittel CR, Li J, Ovaere M and Reguant M: The Short-run and Long-run effects of Covid-19 on energy and the environment. Joule. 4:1337–1341. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
ΙΕΑ: Electricity Market Report-December 2020, IEA Paris, 2020b.
|
|
16
|
He MZ, Kinney PL, Li T, Chen C, Sun Q, Ban J, Wang J, Liu S, Goldsmith J and Kioumourtzoglou MA: Short- and intermediate-term exposure to NO2 and mortality: A multi-county analysis in China. Environ Pollut. 261(114165)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Muhammad S, Long X and Salman M: COVID-19 pandemic and environmental pollution: A blessing in disguise? Sci Total Environ. 728(138820)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Le Quéré C, Jackson RB, Jones MW, Smith AJP, Abernethy S, Andrew RM, De-Gol AJ, Willis DR, Shan Y, Canadell JG, et al: Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat Climate Change. 10:647–653. 2020.
|
|
19
|
Schanes K, Dobernig K and Gözet B: Food waste matters-A systematic review of household food waste practices and their policy implications. J Cleaner Production. 182:978–991. 2018.
|
|
20
|
Ahmed W, Angel N, Edson J, Bibby K, Bivins A, O'Brien JW, Choi PM, Kitajima M, Simpson SL, Li J, et al: First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci The Total Environ. 728(138764)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Medema G, Heijnen L, Elsinga G, Italiaander R and Brouwer A: Presence of SARS-Coronavirus-2 in sewage. Environ. Sci. Technol. Lett. 7:511–516. 2020.
|
|
22
|
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS and McLellan JS: Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 367:1260–1263. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zambrano-Monserrate MA, Ruano MA and Sanchez-Alcalde L: Indirect effects of COVID-19 on the environment. Sci Total Environ. 728(138813)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Liu M, Tan S, Zhang M, He G, Chen Z, Fu Z and Luan C: Waste paper recycling decision system based on material flow analysis and life cycle assessment: A case study of waste paper recycling from China. J Environ Manage. 255(109859)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, Najafi G, Ahmed SF, Uddin MA and Mahlia TMI: Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustain Prod Consum. 26:343–359. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Munawer ME: Human health and environmental impacts of coal combustion and post-combustion wastes. J Sustainable Mining. 17:87–96. 2018.
|
|
27
|
Huang Y, Mok WC, Yam YS, Zhou JL, Surawski NC, Organ B, Chan EFC, Mofijur M, Mahlia TMI and Ong HC: Evaluating in-use vehicle emissions using air quality monitoring stations and on-road remote sensing systems. Sci Total Environ. 740(139868)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Baensch-Baltruschat B, Kocher B, Stock F and Reifferscheid G: Tyre and road wear particles (TRWP)-A review of generation, properties, emissions, human health risk, ecotoxicity, and fate in the environment. Sci Total Environ. 733(137823)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zambrano-Monserrate MA and Ruano MA: Does environmental noise affect housing rental prices in developing countries? Evidence from Ecuador. Land Use Policy. 87(104059)2019.
|
|
30
|
Ladd-Acosta C, Feinberg JI, Brown SC, Lurmann FW, Croen LA, Hertz-Picciotto I, Newschaffer CJ, Feinberg AP, Fallin MD and Volk HE: Epigenetic marks of prenatal air pollution exposure found in multiple tissues relevant for child health. Environ Int. 126:363–376. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Mishra PK, Bunkar N, Singh RD, Kumara R, Pushpendra GP, Tiwari R, Bhargava A and Chaudhury K: Comparative profiling of epigenetic modifications among individuals living in different high and low air pollution zones: A pilot study from India. Environmental Adv. 4(100052)2021.
|
|
32
|
Karnatovskaia LV, Johnson MM, Varga K, Highfield JA, Wolfrom BD, Philbrick KL, Ely EW, Jackson JC, Gajic O, Ahmad SR and Niven AS: Stress and fear: Clinical implications for providers and patients (in the Time of COVID-19 and Beyond). Mayo Clin Proc. 95:2487–2498. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L and Amore M: The psychological impact of COVID-19 on the mental health in the general population. QJM. 113:531–537. 2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Sardar S, Abdul-Khaliq I, Ingar A, Amaidia H and Mansour N: ‘COVID-19 lockdown: A protective measure or exacerbator of health inequalities? A comparison between the United Kingdom and India.’ a commentary on ‘the socio-economic implications of the coronavirus and COVID-19 pandemic: A review’. Int J Surg. 83:189–191. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Galea S and Abdalla SM: COVID-19 pandemic, unemployment, and civil unrest: Underlying deep racial and socioeconomic divides. JAMA. 324:227–228. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Dlamini J: Gender-based violence, twin pandemic to COVID-19. Crit Sociol. 47:583–590. 2021.
|
|
37
|
Bradbury-Jones C and Isham L: The pandemic paradox: The consequences of COVID-19 on domestic violence. J Clin Nurs. 29:2047–2049. 2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Sharma A and Borah SB: Covid-19 and domestic violence: An indirect path to social and economic crisis. J Fam Violence: Jul 28, 2020 (Epub ahead of print).
|
|
39
|
Usher K, Bhullar N, Durkin J, Gyamfi N and Jackson D: Family violence and COVID-19: Increased vulnerability and reduced options for support. Int J Ment Health Nurs. 29:549–552. 2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Singh S, Roy D, Sinha K, Parveen S, Sharma G and Joshi G: Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 293(113429)2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Glowacz F and Schmits E: Psychological distress during the COVID-19 lockdown: The young adults most at risk. Psychiatry Res. 293(113486)2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Farsalinos K, Poulas K, Kouretas D, Vantarakis A, Leotsinidis M, Kouvelas D, Docea AO, Kostoff R, Gerotziafas GT, Antoniou MN, et al: Improved strategies to counter the COVID-19 pandemic: Lockdowns vs. primary and community healthcare. Toxicol Rep. 8:1–9. 2021.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Colao A, Piscitelli P, Pulimeno M, Colazzo S, Miani A and Giannini S: Rethinking the role of the school after COVID-19. Lancet Public Health. 5:e370-2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Sikali K: The dangers of social distancing: How COVID-19 can reshape our social experience. J Community Psychol. 48:2435–2438. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Araújo LA, Veloso CF, Souza MC, Azevedo JMC and Tarro G: The potential impact of the COVID-19 pandemic on child growth and development: A systematic review. J Pediatr (Rio J). 97:369–377. 2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Yaribeygi H, Panahi Y, Sahraei H, Johnston TP and Sahebkar A: The impact of stress on body function: A review. EXCLI J. 16:1057–1072. 2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Ramezani M, Simani L, Karimialavijeh E, Rezaei O, Hajiesmaeili M and Pakdaman H: The role of anxiety and cortisol in outcomes of patients with Covid-19. Basic Clin Neurosci. 11:179–184. 2020.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Maugeri G and Musumeci G: Adapted physical activity to ensure the physical and psychological well-being of COVID-19 patients. J Funct Morphol Kinesiol. 6(13)2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Maugeri G, Castrogiovanni P, Battaglia G, Pippi R, D'Agata V, Palma A, Di Rosa M and Musumeci G: The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 6(e04315)2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Stevens AJ, Rucklidge JJ and Kennedy MA: Epigenetics, nutrition and mental health. Is there a relationship? Nutr Neurosci. 21:602–613. 2018.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Munoz Fernandez SS and Lima Ribeiro SM: Nutrition and Alzheimer disease. Clin Geriatr Med. 34:677–697. 2018.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Landecker H: Food as exposure: Nutritional epigenetics and the new metabolism. Biosocieties. 6:167–194. 2011.PubMed/NCBI View Article : Google Scholar
|
|
53
|
McGuinness D, McGlynn LM, Johnson PC, MacIntyre A, Batty GD, Burns H, Cavanagh J, Deans KA, Ford I, McConnachie A, et al: Socio-economic status is associated with epigenetic differences in the pSoBid cohort. Int J Epidemiol. 41:151–160. 2012.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Gonzalez-Jaramillo V, Portilla-Fernandez E, Glisic M, Voortman T, Ghanbari M, Bramer W, Chowdhury R, Nijsten T, Dehghan A, Franco OH and Nano J: Epigenetics and inflammatory markers: A systematic review of the current evidence. Int J Inflam. 2019(6273680)2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Day FR, Ong KK and Perry JRB: Elucidating the genetic basis of social interaction and isolation. Nat Commun. 9(2457)2018.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Arzate-Mejia RG, Lottenbach Z, Schindler V, Jawaid A and Mansuy IM: Long-term impact of social isolation and molecular underpinnings. Front Genet. 11(589621)2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Blum K, Cadet JL, Baron D, Badgaiyan RD, Brewer R, Modestino EJ and Gold MS: Putative COVID-19 induction of reward deficiency syndrome (RDS) and associated behavioral addictions with potential concomitant dopamine depletion: Is COVID-19 social distancing a double edged Sword? Subst Use Misuse. 55:2438–2442. 2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Kundakovic M and Jaric I: The epigenetic link between prenatal adverse environments and neurodevelopmental disorders. Genes (Basel). 8(104)2017.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Milton DK, Fabian MP, Cowling BJ, Grantham ML and McDevitt JJ: Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathog. 9(e1003205)2013.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Leung NHL, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, Hau BJP, Yen HL, Li Y, Ip DKM, Peiris JSM, et al: Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 26:676–680. 2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Green CF, Davidson CS, Panlilio AL, Jensen PA, Jin Y, Gibbs SG and Scarpino PV: Effectiveness of selected surgical masks in arresting vegetative cells and endospores when worn by simulated contagious patients. Infect Control Hosp Epidemiol. 33:487–494. 2012.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Chu DK, Akl EA, Duda S, Solo K, Yaacoub S and Schünemann HJ: COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet. 395:1973–1987. 2020.PubMed/NCBI View Article : Google Scholar
|
|
63
|
MacIntyre CR and Wang Q: Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet. 395:1950–1951. 2020.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Asadi S, Cappa CD, Barreda S, Wexler AS, Bouvier NM and Ristenpart WD: Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci Rep. 10(15665)2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Machida M, Nakamura I, Saito R, Nakaya T, Hanibuchi T, Takamiya T, Odagiri Y, Fukushima N, Kikuchi H, Amagasa S, et al: Incorrect use of Face Masks during the current COVID-19 pandemic among the general Public in Japan. Int J Environ Res Public Health. 17(6484)2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
World Health Organization (WHO): Coronavirus disease (COVID-19): Masks. WHO, Geneva, 2020. https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-masks. Accessed December 1, 2020.
|
|
67
|
World Health Organization (WHO): Mask use in the context of COVID-19: interim guidance. WHO, Geneva, 2020. https://apps.who.int/iris/handle/10665/337199. Accessed December 1, 2020.
|
|
68
|
World Health Organization (WHO): FACT: The prolonged use of medical masks* when properly worn, DOES NOT cause CO2 intoxication nor oxygen deficiency. WHO, Geneva, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters. Accessed June 5, 2020.
|
|
69
|
Smith SM, Sonego S, Wallen GR, Waterer G, Cheng AC and Thompson P: Use of non-pharmaceutical interventions to reduce the transmission of influenza in adults: A systematic review. Respirology. 20:896–903. 2015.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Goh CF, Ming LC and Wong LC: Dermatologic reactions to disinfectant use during the COVID-19 pandemic. Clin Dermatol. 39:314–322. 2021.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Patruno C, Fabbrocini G, Stingeni L and Napolitano M: The role of occupational dermatology in the COVID-19 outbreak. Contact Dermatitis. 83:174–175. 2020.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Grice EA, Kong HH, Conlan S, Deming CB, Davis J and Young AC: NISC Comparative Sequencing Program. Bouffard GG, Blakesley RW, Murray PR, et al: Topographical and temporal diversity of the human skin microbiome. Science. 324:1190–1192. 2009.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Ravalli S and Musumeci G: Coronavirus outbreak in Italy: Physiological benefits of home-based exercise during pandemic. J Functional Morphol Kinesiol. 5(31)2020.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Feng L, Zhang T, Wang Q, Xie Y, Peng Z, Zheng J, Qin Y, Zhang M, Lai S, Wang D, et al: Impact of COVID-19 outbreaks and interventions on influenza in China and the United States. Nat Commun. 12(3249)2021.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, Kim SY, Choi BS and Yi DY: Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. 36(e180)2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Alegría-Torres JA, Baccarelli A and Bollati V: Epigenetics and lifestyle. Epigenomics. 3:267–277. 2011.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Perdigoto CN, Valdes VJ, Bardot ES and Ezhkova E: Epigenetic regulation of epidermal differentiation. Cold Spring Harbor Perspect Med. 4(a015263)2014.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Vlachakis D, Papakonstantinou E, Mitsis T, Pierouli K, Diakou I, Chrousos G and Bacopoulou F: Molecular mechanisms of the novel coronavirus SARS-CoV-2 and potential anti-COVID19 pharmacological targets since the outbreak of the pandemic. Food Chem Toxicol. 146(111805)2020.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Vlachakis D: Genetic and structural analyses of ssRNA viruses pave the way for the discovery of novel antiviral pharmacological targets. Mol Omics. 17:357–364. 2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Vlachakis D and Vlamos P: Mathematical multidimensional modelling and structural artificial intelligence pipelines provide insights for the designing of highly specific AntiSARS-CoV2 agents. MathComputSci: Jun 12, 2021 (Epub ahead of print).
|
|
81
|
Cao L, Goreshnik I, Coventry B, Case JB, Miller L, Kozodoy L, Chen RE, Carter L, Walls AC, Park YJ, et al: De novo design of picomolar SARS-CoV-2 miniprotein inhibitors. Science. 370:426–431. 2020.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Riva L, Yuan S, Yin X, Martin-Sancho L, Matsunaga N, Pache L, Burgstaller-Muehlbacher S, De Jesus PD, Teriete P, Hull MV, et al: Discovery of SARS-CoV-2 antiviral drugs through large-scale compound repurposing. Nature. 586:113–119. 2020.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Peng Y, Du N, Lei Y, Dorje S, Qi J, Luo T, Gao GF and Song H: Structures of the SARS-CoV-2 nucleocapsid and their perspectives for drug design. EMBO J. 39(e105938)2020.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Paniri A and Akhavan-Niaki H: Emerging role of IL-6 and NLRP3 inflammasome as potential therapeutic targets to combat COVID-19: Role of lncRNAs in cytokine storm modulation. Life Sci. 257(118114)2020.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Atlante S, Mongelli A, Barbi V, Martelli F, Farsetti A and Gaetano C: The epigenetic implication in coronavirus infection and therapy. Clin Epigenetics. 12(156)2020.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Lariccia V, Magi S, Serfilippi T, Toujani M, Gratteri S and Amoroso S: Challenges and opportunities from targeting inflammatory responses to SARS-CoV-2 infection: A narrative review. J Clin Med. 9(4021)2020.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Luo D, Liu F, Zhang J, Shao Q, Tao W, Xiao R, Dai W and Qian K: Functional crosstalk between Long non-coding RNAs and the NLRP3 inflammasome in the regulation of diseases. Mol Immunol. 131:191–200. 2021.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Vishnubalaji R, Shaath H and Alajez NM: Protein coding and long noncoding RNA (lncRNA) transcriptional landscape in SARS-CoV-2 infected bronchial epithelial cells highlight a role for interferon and inflammatory response. Genes (Basel). 11(760)2020.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Rodriguez-Guerra M, Jadhav P and Vittorio TJ: Current treatment in COVID-19 disease: A rapid review. Drugs Context. 10:2020-2010-2023. 2021.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Qian M and Jiang J: COVID-19 and social distancing. Z Gesundh Wiss: May 25, 2020 (Epub ahead of print).
|
|
91
|
Fana M, Torrejón Pérez S and Fernández-Macías E: Employment impact of Covid-19 crisis: from short term effects to long terms prospects. J Industrial Business Economics. 47:391–410. 2020.
|
|
92
|
Gholami M, Fawad I, Shadan S, Rowaiee R, Ghanem H, Hassan Khamis A and Ho SB: COVID-19 and healthcare workers: A systematic review and meta-analysis. Int J Infect Dis. 104:335–346. 2021.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Haider II, Tiwana F and Tahir SM: Impact of the COVID-19 pandemic on adult mental health. Pak J Med Sci. 36 (COVID19-S4):S90–S94. 2020.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Jiang P, Fan YV and Klemeš JJ: Impacts of COVID-19 on energy demand and consumption: Challenges, lessons and emerging opportunities. Applied Energy. 285(116441)2021.PubMed/NCBI View Article : Google Scholar
|
|
95
|
MacIntyre CR and Chughtai AA: A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int J Nurs Stud. 108:103629. 2020.PubMed/NCBI View Article : Google Scholar
|