Introduction
Small intestinal transplantation is a procedure
involving several aspects, such as anti-immune rejection treatment,
transplanted organ procurement, surgical technique, perioperative
management and prevention of infection following surgery (1). Rejection and infection are the two
major issues compromising surgical success. Currently, allogeneic
small intestinal transplantation appears to be a viable treatment
option for intestinal failure and short bowel syndrome. Small
intestinal transplantation between ABO-incompatible individuals may
cause a severe rejection response, affecting the survival of the
intestinal recipient (1–3). The ABO blood antigens are
glycoproteins on the membrane surface of red blood cells. These
antigens are also detectable on the vascular endothelial cells of
the grafted small intestine. The small intestinal transplantation
between ABO-incompatible individuals may lead to a series of
complement reactions. Once the complement system is activated, it
may quickly occlude the blood vessels and cause thrombosis,
resulting in graft failure (4).
This is the report of a successful small intestinal transplantation
case between ABO-incompatible individuals.
Case report
Patient and donor characteristics
The patient was a 17-year-old female, weighing 40.5
kg, with A Rh+ blood type and an anti-B antibody titer
of 1:64, who underwent a small intestinal and partial colon
resection following acute diffuse peritonitis and mesenteric artery
thrombosis. The donor was the recipient’s father (43-years old;
blood type, AB).
Plasma exchange and antibody titers
Rituximab (Rh+) was used to reduce the
patient’s B lymphocyte numbers 18 days prior to surgery. In order
to reduce the patient’s antibody titers, the double-filtration and
separation method was used for plasma exchange (5). The first plasma exchange was performed
9 days prior to transplantation. A total of 4 plasma exchanges were
performed. Therefore, the blood IgM antibody titers were reduced to
1:1. The patient’s small intestine was resected due to of serve
necrosis. After 1 year and 2 months, a section of the small
intestine (length, 190 cm) from the donor was transplanted into the
recipient. The titers of anti-B IgM antibodies remained 1:4 1–7
days after surgery and were <1:4 at 4 months after surgery.
Colonoscopy and pathological examination suggested that the
transplanted small intestinal mucosa was slightly swollen and no
erosions or ulcers were observed, while the mucosal villi was
clear. There was marginal mucosal hyperemia, which indicated mild
rejection. Therefore, we asministered 100 mg ATG, rehydration
mutritional support and corrected electrolyte balance. Following
treatment, the colonoscopy and pathological examination was
performed again. The results showed that the mild rejection had
markedly faded. The patient stayed in the hospital for 65 days and
showed no acute rejection response. Tacrolimus (2.0 g/d) was
injected through an intravenous miro-pump on the day of the surgery
as well as on the following day. The doses of anti-thymoglobulin
(ATG) were maintained at 100 mg/d 3 days prior to and after
surgery. Pawnee Long succinate (1,000 mg/d) was used on the day of
the surgery and the dose was gradually reduced to 10 mg/day within
the first month following surgery.
Post-surgical findings
No bleeding was detected in the stoma effluent after
the surgery. The patient developed no complications, such as
diarrhea, had stable weight and normal periodic blood hemoglobin,
total serum protein and albumin levels. The D-xylose absorption
test (6) revealed a normal urine
discharge rate of 30–40%.
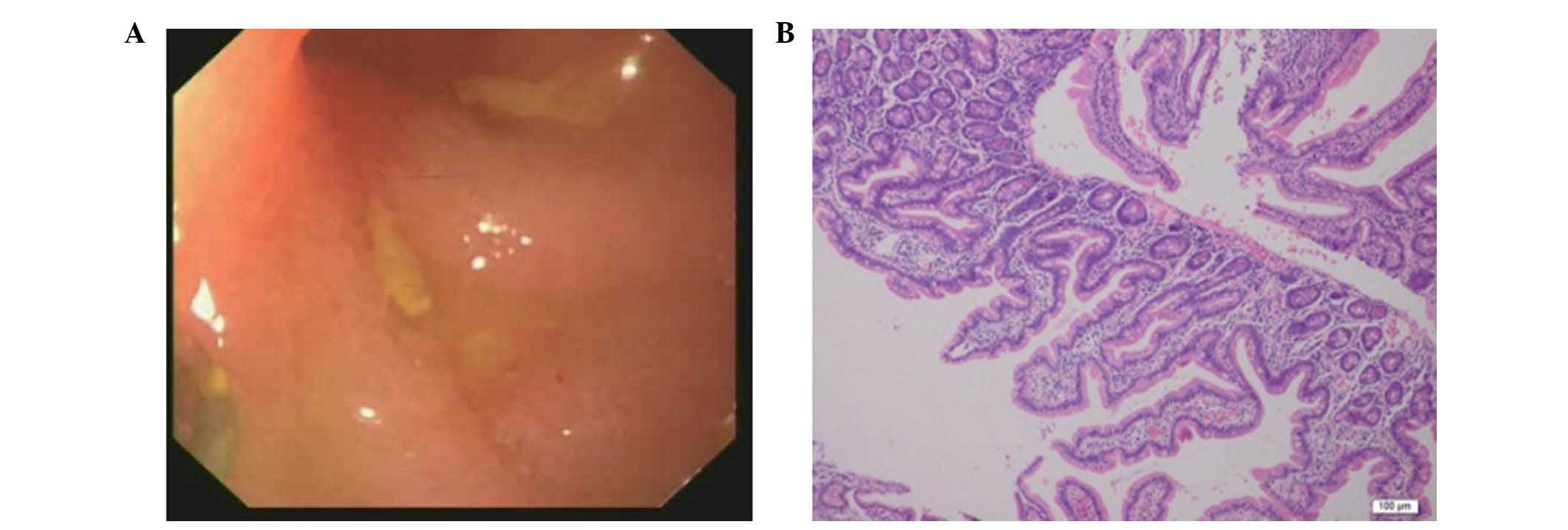
Single-balloon enteroscopy of the small intestine
was performed at 8 months post-surgery to assess the efficacy of
the procedure. The mucosa at the anastomosis site was smooth, of
rosy colour, with clearly visible villi under enteroscopy, without
erosions or exudation (Fig. 1A). On
microscopic examination, the hematoxylin and eosin (H&E)
staining revealed no abnormal mucosal structure at a distance of 4
and 10 cm from the stoma, with a neutrophilic infiltration of the
lamina propria, but no detectable rejection reaction (Fig. 1B). These results suggested that
surgery was successful.
Discussion
Small intestinal transplantation under conditions of
blood group incompatibility may stimulate a hyperacute and acute
rejection reaction (7). If the
titers of blood type antibodies are relatively high, a hyperacute
rejection reaction may occur within minutes to hours after the
transplantation. Hyperacute rejection is one of the main reasons
leading to early death of the recipients (8). Therefore, plasma exchange was
performed several times prior to transplantation in order to reduce
the anti-B antibody titers in the serum of the recipient in the
present case, which were maintained between 1:1 and 1:4.
Tacrolimus, ATG, Pawnee Long succinate and mycophenolate mofetil
capsules were used to avoid immune rejection. Sulperazon,
ornidazole, vancomycin and ganciclovir were administered in order
to prevent infection, whereas γ globulin and albumin were used to
prevent hypoproteinemia, thus protecting against rejection,
infection and any additional complications (9,10).
To summarize, the purpose of small intestinal
transplantation is to restore small intestinal function. The
presented case was successful, indicating that the use of plasma
exchange in combination with immunosuppressants is applicable in
organ transplantation between ABO-incompatible individuals.
References
|
1
|
Cicalese L, Sileri P, Asolati M, et al:
Infectious complications following living-related small bowel
transplantation in adults. Transplant Proc. 33:1554–1555. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Abu-Elmagd K, Todo S, Tzakis A, et al:
Three years clinical experience with intestinal transplantation. J
Am Coll Surg. 179:385–400. 1994.PubMed/NCBI
|
|
3
|
Middleton SJ and Jamieson NV: The current
status of small bowel transplantation in the UK and
internationally. Gut. 54:1650–1657. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ziring D, Tran R, Edelstein S, et al:
Infectious enteritis after intestinal transplantation: incidence,
timing, and outcome. Transplantation. 79:702–709. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Morioka D, togo S, Kumamoto T, et al: Six
consecutive cases of successful adult ABO-incompatible living donor
liver transplantation: a proposal of grading the severity of
antibody-mediated rejection. Transplantation. 85:171–178. 2008.
View Article : Google Scholar
|
|
6
|
Reyes J, Tzakis A, Todo S, et al:
Nutritional management of intestinal transplant recipients.
Transplant Proc. 25:1200–1201. 1993.PubMed/NCBI
|
|
7
|
Rostaing L, Massari P, Garcia VD, et al:
Switching from calcineurin inhibitor-based regimens to a
belatacept-based regimen in renal transplant recipients: a
randomized phase II study. Clin J Am Soc Nephrol. 6:430–439. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kato T, Tzakis AG, Selvaggi G, et al:
Transplantation of the spleen: effect of splenic allograft in human
multivisceral transplantation. Ann Surg. 246:436–444. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Green M, Reyes J, Jabbour N, et al: Use of
quantitative PCR to predict onset of Epstein-Barr viral infection
and post- transplant lymphoproliferative disease after intestinal
transplantation in children. Transplant Proc. 28:2759–2760.
1996.
|
|
10
|
Takahashi H, Kato T, Selvaggi G, et al:
Subclinical rejection in the initial postoperative period in small
intestinal transplantation: a negative influence on graft survival.
Transplantation. 84:689–696. 2007. View Article : Google Scholar
|