Introduction
Stroke prevention is central in the management of
patients with atrial fibrillation (AF) (1). The European Society of Cardiology (ESC)
guidelines recommend a risk score system, the
CHA2DS2-VASc schema, that accounts for
congestive heart failure, hypertension, age 65–74 or ≥75 (risk
doubled), diabetes, stroke (risk doubled), vascular disease, age
and sex (female), to evaluate individual risk of thromboembolism
(2,3).
Risk assessment should be performed for each case prior to the
initiation of antithrombotic therapy to determine the possibility
of bleeding and ischemic events. The HAS-BLED scoring system based
on hypertension, abnormal renal/liver function,
stroke/thromboembolism, bleeding history, labile international
normalized ratio (INR), elderly age (>65 years) and drug
consumption/alcohol abuse may be used to calculate the risk of
bleeding (4–6). This system has been clinically confirmed
to accurately predict the risk of thromboembolism and bleeding in
patients with AF (2–6).
The majority of patients with AF (70–80%) require
continuous oral anticoagulation (OAC) therapy. Additionally, 20–30%
patients with AF have comorbid coronary artery disease (CAD)
(7–10). Clinicians face a therapeutic challenge
in that 5–10% patients undergoing percutaneous coronary
intervention with stenting (PCIS) typically require long-term OAC
(11–14). Acute coronary syndrome (ACS),
incorporating unstable angina/non-ST segment elevation myocardial
infarction (MI) and ST-segment elevation MI, constitutes another
cardiovascular disease type (15). It
is associated with risks of mortality and morbidity from MI, heart
failure and ventricular arrhythmia (16). Dual antithrombotic treatment
consisting of low-dose acetylsalicylic acid and the P2Y12
inhibitors clopidogrel, prasugrel and ticagrelor is a primary
strategy for reducing the risk of recurrence of ischemic outcomes,
particularly in the first year after acute events (17–19). A
particular challenge regarding antithrombotic treatment is patients
who present with AF and ACS, particularly as these patients have a
high risk of cardiovascular mortality and morbidity (7–15). The
present recommendation is triple oral antithrombotic therapy (TOAT;
aspirin, clopidogrel and warfarin) for patients with previous MI
and/or PCI and concurrent AF, as OAC has been associated with
stroke risk factors in patients with AF, while dual antiplatelet
therapy (DAPT; aspirin and clopidogrel) has been associated with
ACS following PCI (20). However, the
prevalence of major bleeding with triple therapy increases with
treatment duration (21–22).
To date, there is a lack of randomized studies
comparing the safety and efficacy of the antithrombotic regimens
TOAT and DAPT. The nine observational trials included in the
current meta-analysis had the inherent limitations of a
nonrandomized study design; however, the meta-analysis was feasible
as the grouping criteria were similar. The primary end points of
DAPT and triple therapy among patients with AF concurrent to PCIS
were evaluated, and subgroup analysis of major adverse cardiac
events (MACE), stroke and bleeding events was performed to compare
the treatment strategies. This aimed to provide a basis for
rational clinical decisions on the optimal treatment for individual
patients with AF concurrent to PCIS.
Materials and methods
Eligibility criteria
The search strategy focused on observational studies
in which patients were receiving DAPT (clopidogrel + aspirin)
classified into those with concomitant warfarin treatment or
non-warfarin users. The outcomes of interest were MACE (defined as
death, ACS, stent thrombosis, revascularization and nonfatal MI),
ischemic stroke, major bleedings and minor bleedings (23–31). Major
bleeding was defined as severe or moderate bleeding according to
the Global Utilization of Streptokinase and Tissue Plasminogen
Activator for Occluded Coronary Arteries criteria (25). Minor bleeding was defined as any
clinically overt sign of bleeding associated with a decrease in
hemoglobin between 3 and 5 g/l (32).
Reviews, letters, comments, nonclinical investigations, articles
with data on platelet activity only or no relevant data and article
published in languages other than Chinese or English were
excluded.
Search strategy and selection
criteria
A comprehensive search was performed for studies
published prior to July 7, 2017 that focused on TOAT or DAPT
antithrombotic therapy and evaluated the outcomes of the different
strategies in patients with atrial fibrillation (AF) receiving
PCIS. Searches were performed on Medline (http://www.nlm.nih.gov/bsd/pmresources.html),
Embase (https://www.elsevier.com/solutions/embase-biomedical-research),
Cochrane (http://uk.cochrane.org/) and the Chinese
Biomedical Literature Database (CBM; http://www.sinomed.ac.cn/).
Data sources and searches
Electronic searches were performed using the search
terms ‘AF’, ‘clopidogrel’, ‘Plavix’, ‘aspirin’, ‘warfarin’, ‘TOAT’,
‘DAPT’, and ‘PCIS’. Searches were conducted according to the
characteristics of each database. Bibliographies from included
articles and review articles were hand-searched, and cardiovascular
research professionals were consulted to ensure inclusion of all
pertinent studies.
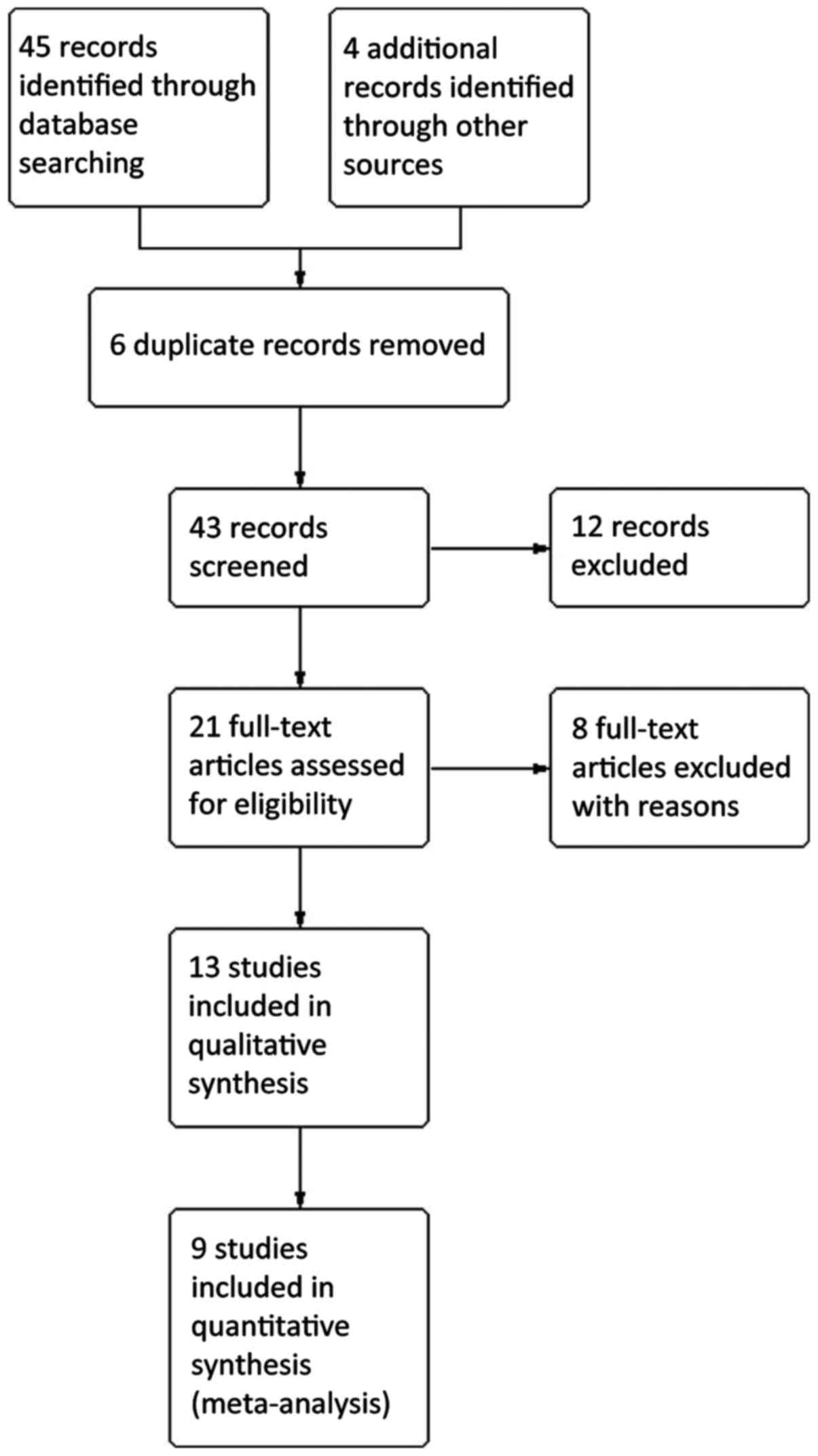
Study selection
Two reviewers independently screened the abstracts
and titles of the studies from the electronic search to identify
all potential eligible studies. Potential relevant literatures were
then retrieved as full-text manuscripts for further assessment of
eligibility. Any discrepancies or uncertainties between the
reviewers were resolved by consultation or consensus with a third
reviewer. The authors were also contacted if any areas of
uncertainty required clarification.
Data extraction
Two investigators independently extracted data on
patient and study characteristics, exposure factors, outcomes and
study quality for each study using a standard data extraction form
(33). Consensus with the third
reviewer resolved any discrepancies. The following information was
extracted from each study: First author, year of publication,
location, study design and number of patients, mean age (and
standard deviation), sex, underlying disease, type of
anti-thrombosis drug used (TOAT or DAPT), duration of follow-up,
outcomes, analyzed effect, odds ratio (OR) and adjusted
variables.
Data analysis
Extracted information from included studies was
entered into a table to assess the study subjects, exposure
factors, outcomes, quality and design of each study and the
heterogeneity of included studies. ORs with 95% confidence
intervals (CIs) were determined for binary outcomes. Statistical
heterogeneity was assessed using the χ2 test and was
quantified using the I2 statistic. When there was
significant heterogeneity with P<0.1, a random-effects model was
used via the DerSimonian and Laird method; otherwise, a
fixed-effects model was used via the Mantel-Haenszel method. The
clinical outcomes of patients with AF following percutaneous
intervention and treatment with different oral antithrombotic
therapies (TOAT or DAPT) were evaluated. The Mantel-Haenszel method
was used to calculate the ORs for clinical outcomes between the
DAPT and TOAT groups. For meta-regression, sensitivity analyses of
primary outcomes were conducted after eliminating the maximum and
minimum of effect size to determine the stability of results.
Finally, small study bias and/or publication bias was assessed by
visual inspection of a funnel plot and Egger's test. Additionally,
the Newcastle-Ottawa Scale for assessing the quality of
nonrandomised studies in meta-analyses was used (34), which is based on three domains:
Selection of study groups, comparability of groups and
ascertainment of exposure/outcome.
Results
Description of the studies
A total of nine observational trials were included
in the present study, consisting of 19,035 patients in total
(23–31). The flow of included studies through
the selection process is depicted showed in Fig. 1. The baseline and design
characteristics of the selected studies are listed in Table I. The range of participant number was
87–4,959, including men and women (1.6:1 ratio). The effects of
DAPT and TOAT among these patients with AF concurrent to PCIS were
compared.
 | Table I.Design and baseline characteristics
of the selected studies. |
Table I.
Design and baseline characteristics
of the selected studies.
|
| DAPT | TOAT |
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|---|
| Author, year | Events, no. | Total patients,
no. | Events, no. | Total patients,
no. | Clinical
outcome | Median, follow-up
years |
CHA2DS2 VASc score
patients,(%) | Refs. |
|---|
| Choi et al,
2017 | 112 | 629 | 16 | 75 | The primary outcome
was a composite of cardiovascular mortality, non fatal MI or
nonfatal stroke (from any cause). The principal secondary outcomes
were mortality (from any cause, cardiovascular or
non-cardiovascular), MI, stroke (from any cause, ischemic or
hemorrhage), stent thrombosis, repeat revascularization and
bleeding (major or nonmajor). | 6.2 | DAPT: ≥2 (71.1)
TOAT: ≥2 (73.3) | (23) |
| Lamberts et
al, 2012 | 725 | 3,144 | 269 | 1,495 | The primary outcome
was nonfatal or fatal bleeding. The secondary outcomes were,
ischemic stroke nonfatal MI or nonfatal ischemic stroke. | 8.0 | DAPT: ≥2 (56.5)
TOAT: ≥2 (60.8) | (24) |
| Kang et al,
2015 | 42 | 236 | 29 |
131 | The primary end
point was a 2-year net clinical outcome: A composite of major
bleeding and major adverse cardiac and cerebral events. | 2.0 | DAPT: ≥2 (76.6)
TOAT: ≥2 (90.0) | (25) |
| Gao et al,
2010 | 67 | 334 | 12 |
136 | The primary end
point was defined as the occurrence of MACE, including mortality,
MI, target vessel revascularization, stent thrombosis or stroke at
12 months. Secondary safety end points were major or minor bleeding
complications during the follow-up period. | 1.0 | CHADS2
score ≥2 (45.8) | (26) |
| Fosbol et
al, 2012 | 922 | 2,841 | 187 |
731 | The primary outcome
was a major cardiac event within 1 year defined as a composite end
point of mortality, hospitalization for recurrent MI or hospital
for ischemic stroke. The second outcome was 1-year hospitalization
for bleeding, intracranial hemorrhage, hemarthrosis,
hemopericardium, unspecified hemorrhage or acute posthemorrhagic
anemia. | 1.0 | n/a | (27) |
| Manzano-Fernandez
et al, 2008 | 0 | 38 | 2 | 49 | The primary end
point was defined as the occurence of major bleeding complications
(fatal bleeding, a decrease in the blood hemoglobin level >4g/l,
need for transfusion of ≥2 U blood, need for corrective surgical
intervention, the occurrence of intracranial or retroperitoneal
bleeding or any combination of these events. The secondary end
points were cardiovascular mortality, myocardial infarction, need
of new revascularization, stent thrombosis, or thromboembolic
complications (MACE). | 1.0 | n/a | (28) |
| Maegdefessel et
al, 2008 | 18 | 103 | 1 | 14 | A combined end
point comprised of severe bleeding events, myocardial infarctions,
strokes and cardiovascular death. | 1.4 | n/a | (29) |
| Hansen et
al, 2010 | 94 | 2,859 | 64 | 1,261 | The primary end
point was bleeding. Bleeding was defined as an admission to a
Danish hospital with a bleeding diagnosis (primary or secondary), a
nonfatal bleeding episode or a diagnosis of bleeding as a cause of
mortality. The second end points were ischemic stroke, defined as
nonfatal ischemic or unspecified stroke diagnosis. | 3.3 | n/a | (30) |
| Hess et al,
2015 | 1,173 | 3,589 | 446 | 1,370 | The primary outcome
was 2-year MACE comprising of mortality, readmission for MI or
stroke. Secondary effectiveness outcomes included individual
components of composite MACE, as well as ischemic stroke
alone. | 2.0 | n/a | (31) |
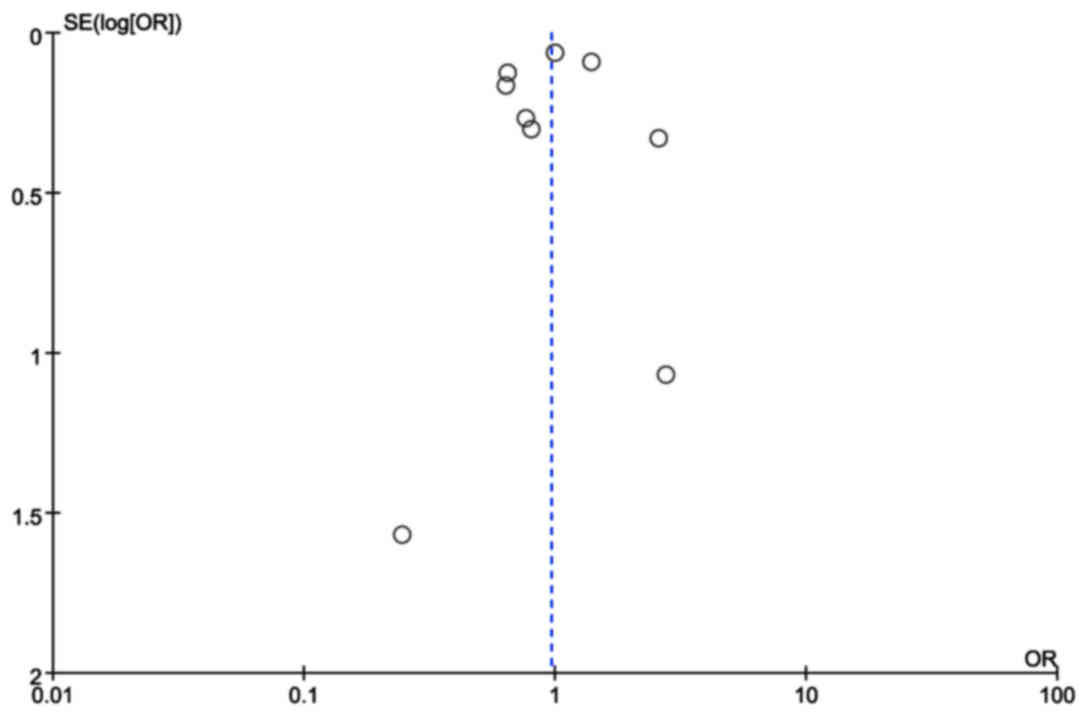
Quality assessment of the trials and
publication bias
According to the Newcastle-Ottawa Scale assessment,
the selected trials in the meta-analysis were well-designed and
reasonably conducted. Publication bias was assessed by Egger's test
as depicted in Fig. 2. The funnel
plot was not markedly skewed, indicating the absence of publication
bias in the meta-analysis.
Effect of antithrombotic therapy on
primary end point, MACE, ischemic stroke and major bleeding
events
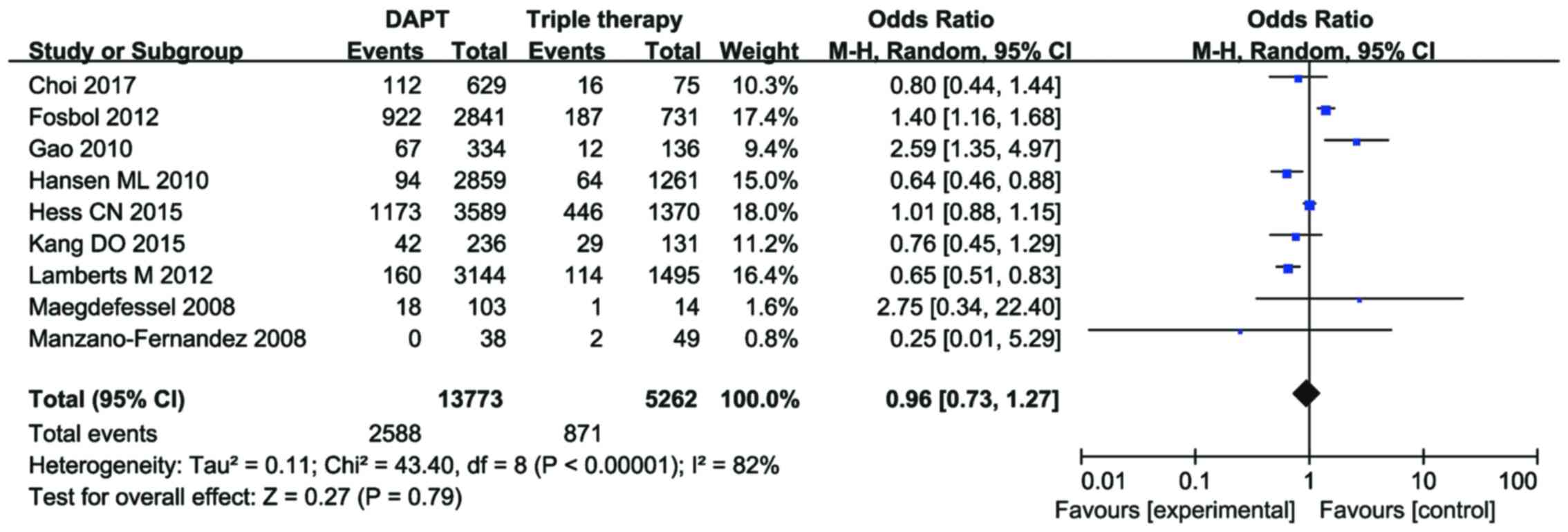
Analysis of baseline characteristics indicated no
significant in the history of co-existent disease or conventional
therapies between the DAPT and TOAT groups. The primary end point
incidence was 2,588 patients in the DAPT group (n=13,773) and 871
patients in the TOAT group (n=5,262) on pooling of all nine trials.
There was no statistically significant difference in the incidence
of primary end points between the groups (OR=0.96, 95%
CI=0.73–1.27, P=0.79; Fig. 3) with
heterogeneity between trials (I2=82%, P<0.00001).
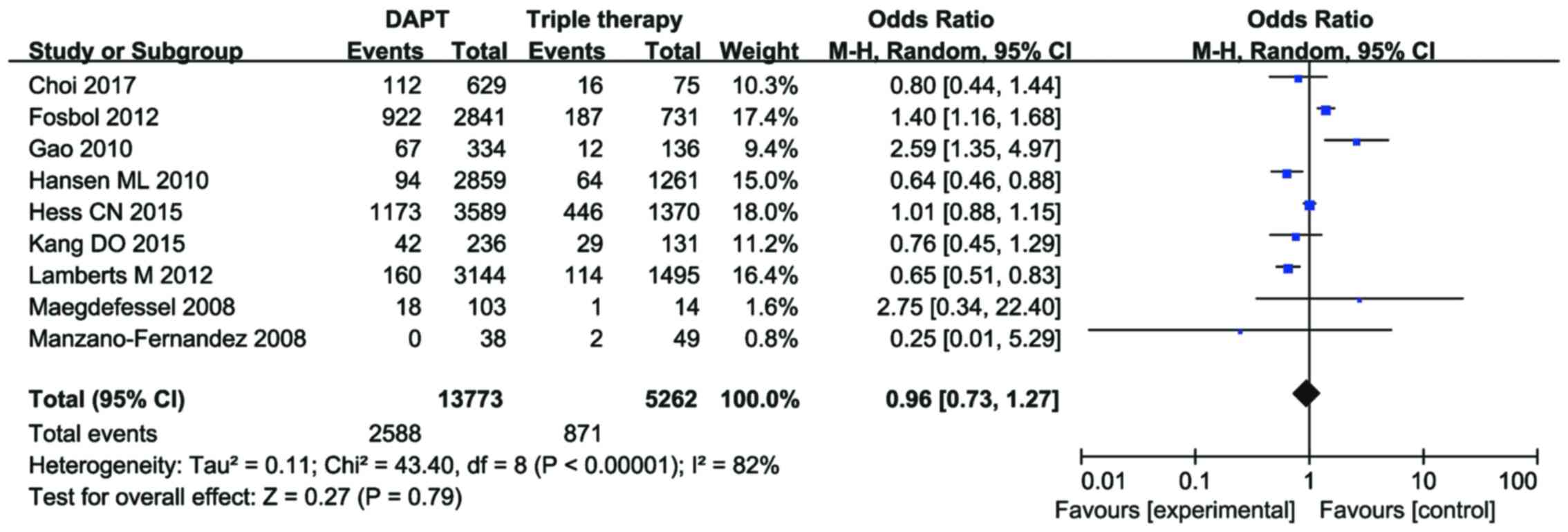 | Figure 3.Forest plot showing relative risk of
the primary end point incidence. Primary end point incidence was
2,588 patients in the DAPT group (n=13,773) and 871 patients in the
TOAT group (n=5,262) on pooling all nine trials. There was no
statistically significant difference in primary end point incidence
(OR=0.96, 95% CI=0.73–1.27, P=0.79.) with heterogeneity between
trials (I2=82%, P<0.00001). The M-H method was used
to estimate the pooled OR for all strata. DAPT, dual antiplatelet
therapy; TOAT, triple oral antithrombotic therapy; OR, odds ratio;
CI, confidence interval; M-H, Mantel-Haenszel. |
This high heterogeneity in the nine trials
(I2=82%, P<0.00001) may be due to differing
definitions of the primary end point. The primary end points of
Choi et al (23), Kang et
al (25), Gao et al
(26), Fosbol et al (27) and Hess et al (31) were generally nonfatal MI,
cardiovascular mortality and nonfatal stroke. By contrast, the
primary end point of Lamberts et al (24), Manzano-Fernández et al
(28), Maegdefessel et al
(29) and Hansen et al
(30) was fatal or nonfatal
bleeding.
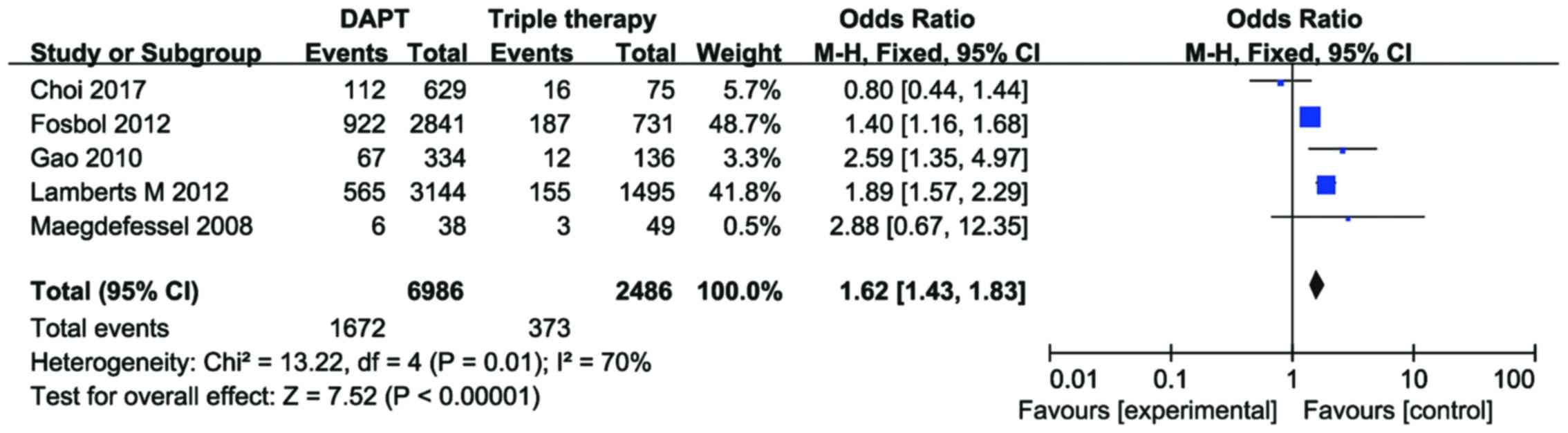
The data of Choi et al (23), Lamberts et al (24), Gao et al (26), Fosbol et al (27), and Manzano-Fernández et al
(28) were pooled for subgroup
analysis in order to compare the incidence of MACE plus ischemic
stroke in the DAPT and TOAT groups. An increased risk of MACE plus
ischemic stroke was identified in the DAPT group compared with the
TOAT group among patients with AF concurrent to PCIS (OR=1.62, 95%
CI=1.43–1.83, P<0.00001) with heterogeneity between the trials
(I2=70%, P=0.01; Fig.
4).
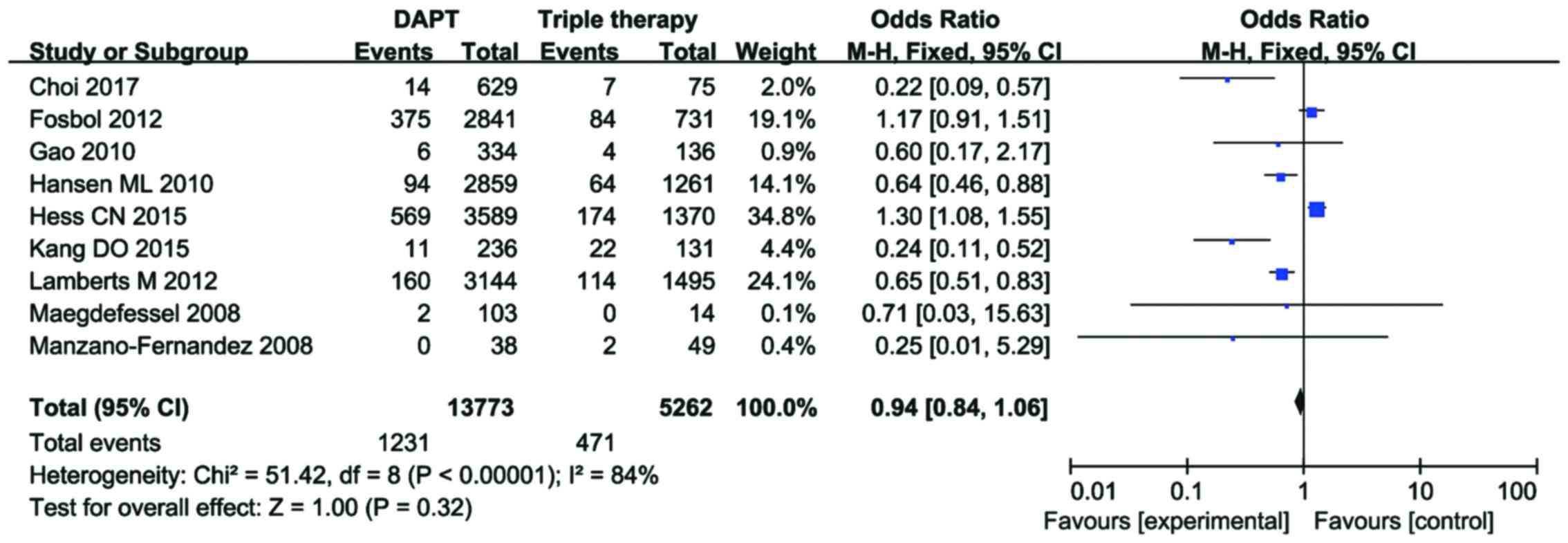
Furthermore, data regarding major bleeding events in
the nine studies were pooled to compare the incidence of major
bleeding between the DAPT and TOAT groups. No increased risk of
major bleeding was observed in the DAPT or TOAT group (OR=0.94, 95%
CI=0.84–1.06, P=0.32; Fig. 5).
However, there was significant heterogeneity among the nine studies
(I2=84%, P<0.00001).
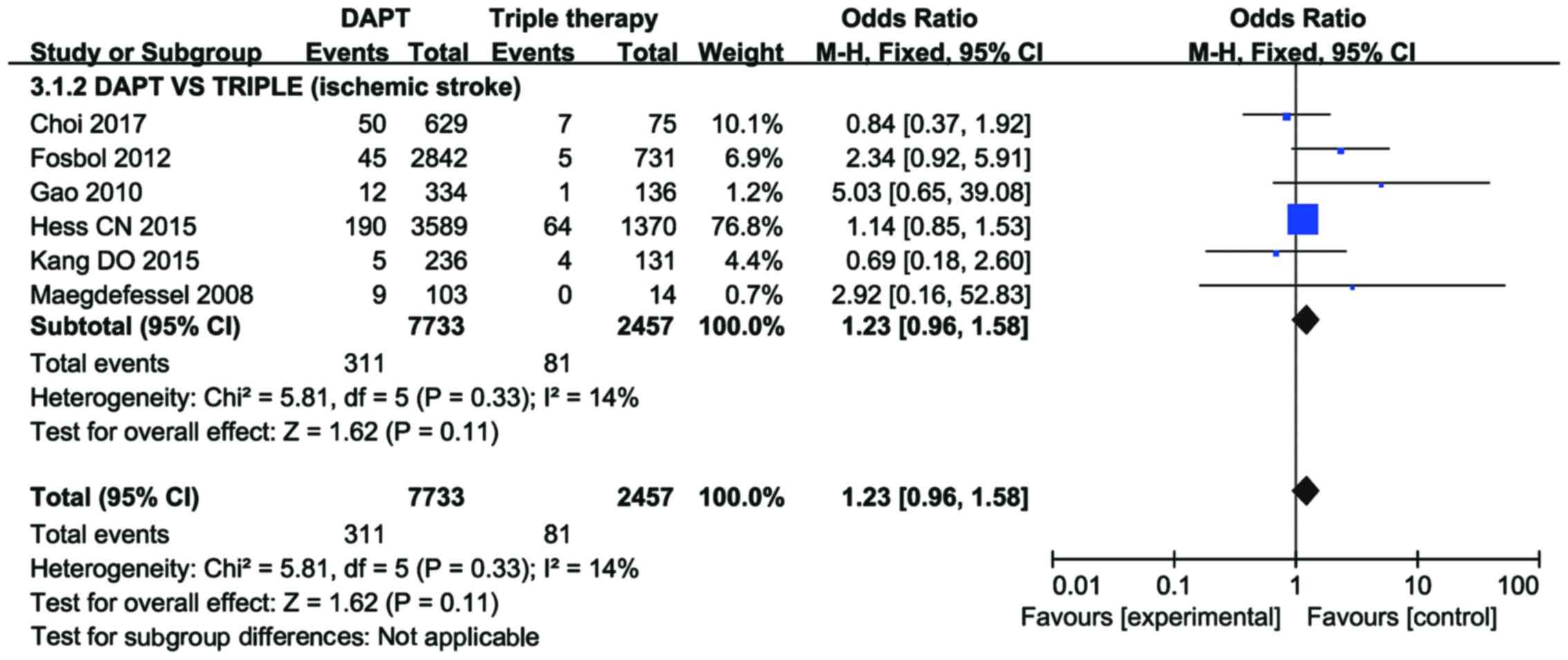
Data regarding ischemic stroke in Choi et al
(23), Kang et al (25), Gao et al (26), Fosbol et al (27), Maegdefessel et al (29) and Hess et al (31) were also pooled to compare the
incidence of ischemic stroke between the DAPT and TOAT groups. No
increased risk of ischemic stroke was identified in the DAPT group
compared with the TOAT group among patients with AF concurrent to
PCIS (OR=1.23, 95% CI=0.96–1.58, P=0.11; Fig. 6) with no significant heterogeneity
between the trials (I2=14%, P=0.33).
Discussion
In the present meta-analysis, nine observational
trials were pooled to determine the optimal antithrombotic strategy
in patients with AF following PCIS. On comparing DAPT (aspirin and
clopidogrel) with TOAT (aspirin + clopidogrel + warfarin), the
results indicated that neither TOAT nor DAPT were associated with
an increased incidence of primary end point, major bleeding or
ischemic stroke in patients with AF following percutaneous
intervention. However, there was an increased incidence of MACE
plus stroke in AF patients treated with DAPT when compared with the
TOAT group.
AF is a common cardiac arrhythmia, particularly in
older individuals (35), with a
prevalence of approximately 10% in patients above 80 years old
(36). It is established that AF is
an independent risk factor for stroke (37). In the presence of other risk factors
of cardiovascular disease, the occurrence of stroke due to AF
ranges from 2 to 18% (38). The ESC
guidelines have recommended the use of the
CHA2DS2-VASc score for stroke risk assessment
and define ‘low-risk’ patients as those with a
CHA2DS2-VASC score of 0 (males) or ≤1
(females) (39). Furthermore, scores
of HAS-BLED may be used to calculate the risk of bleeding (35,39,40). These
scores have been clinically confirmed to accurately predict the
risk of thromboembolism and bleeding in AF patients (2–6). Among the
different oral antithrombotic therapies studied, warfarin has been
demonstrated to reduce stroke risk by 64% when compared with
placebo and by 39% when compared with aspirin in patients with AF
(41). Furthermore, TOAT has been
demonstrated to have greater efficiency than DAPT when tested as an
alternative antithrombotic treatment (23–31).
Since 2001, the standard antithrombotic strategy has
been DAPT therapy with aspirin plus clopidogrel for patients with
ACS and for patients undergoing PCIS, in order to prevent
complications including stent thrombosis, recurrent MI and stroke
(42–45). Although aspirin is established to
significantly reduce cardiovascular events in ACS, concurrent
clopidogrel as a second antiplatelet has been demonstrated to
significantly improve ACS outcomes compared with aspirin alone.
Previously, other antiplatelet agents (prasugrel or ticagrelor)
have been clinically used as substitutions for clopidogrel in the
occurrence of ACS; these agents have been reported to achieve a
higher degree inhibition of platelet aggregation compared with
clopidogrel and do not seem to be affected by CYP2C19 polymorphism
(18,46). Additionally, a previous study reported
improved clinical outcomes of patients with ACS following treatment
with prasugrel or ticagrelor compared with clopidogrel, though this
was accompanied by an increase in bleeding risk, particularly in
those undergoing PCI (46). The use
of DAPT has been recommended by recent European guidelines for at
least four weeks following bare-metal stenting and for at least six
months following drug-eluting stenting (35,47). The
majority of patients with AF (70–80%) require continuous OAC, and
CAD develops in 20–30% of these patients (7–10).
Clinicians are faced with a therapeutic challenge in that 5–10%
patients undergoing PCIS typically require long-term OAC therapy
(11–14). A particular challenge in
antithrombotic therapy is patients who present with both AF and ACS
(7–14). There is a slight difference in the
pathogenesis of thrombi development between patients with AF or
CAD: The type of thrombi in patients with CAD is platelet-rich,
while thrombi in AF patients is fibrin-rich (48–50).
Compared with OAC alone, combined aspirin and clopidogrel therapy
is less effective in preventing stroke in patients with AF
following PCIS; however OAC alone is insufficient for preventing
stent thrombosis. TOAT is typically necessary to prevent ischemic
stroke, MI or stent thrombosis associated with PCIS or ACS in
patients with comorbid CAD and AF (48). TOAT can completely prevent these
thrombotic complications, though at the expense of increased
bleeding risk (49,50). Future studies should aim to provide
safety and efficacy data for guiding clinical practice, to overcome
the challenge of determining the optimal antithrombotic treatment
for patients. Optimal treatments may include: Omitting aspirin,
reducing TOAT duration, exchanging warfarin for a direct OAC
(DOAC), the use of DOAC in combination with a single antiplatelet
agent, exchanging clopidogrel for a novel antiplatelet agent, and
DAPT (51,52). The omission of clopidogrel in patients
receiving coronary stents has been associated with an increased
risk of thrombotic outcomes, including MI and stent thrombosis
(42,43). Although omitting aspirin and reducing
TOAT duration may be effective in selected AF patients with a low
risk of thrombosis, the role of DOACs and novel antiplatelet agents
in TOAT is yet to be determined, and there is limited data to
support their use at present (23–31). To
date, there has been a lack of randomized studies comparing the
safety and efficacy of TOAT and classical DAPT. Meta-analyses of
observational studies have the potential to provide clinically
useful data on adverse event rates of a given therapy and in
comparison with other treatments. The nine trials included in the
present study had all the inherent limitations of a nonrandomized
study design; however, the meta-analysis was very feasible as the
grouping standards were similar. In patients with AF, triple
therapy was not associated with decreased primary end point events,
stroke or major bleeding, though was associated with decreased MACE
and stroke incidence, compared with DAPT.
Gao et al (53)
previously assessed patients with indications of chronic OAC, and
confirmed the cardiovascular benefits of triple antithrombotic
therapy through reducing ischemic stroke risk, though also
demonstrated an increased risk of major bleeding. A meta-analysis
by Zhao et al (54) included
nine clinical trials, and identified that triple antithrombotic
treatment was adequate and more efficient in reducing the
occurrence of cardiovascular events and mortality in PCIS patients
potentially requiring long-term OAC compared with DAPT. Although
these previous meta-analyses combined several studies and reported
significant differences in the occurrence of MACE or ischemic
stroke in patients receiving different antithrombotic treatments,
results were limited as less than 5,200 participants were included
in each. Additionally, patients with conditions other than AF,
including mechanical prosthetic heart valves, deep venous
thrombosis, left ventricular thrombus and pulmonary embolism, were
also included (53,55). Saheb et al (55) performed a meta-analysis of triple
antithrombotic therapy compared with DAPT following PCI with
implantation in patients requiring chronic OAC therapy. They
identified that the occurrence of ischemic stroke in PCIS patients
potentially requiring chronic OAC was more effectively reduced by
triple therapy compared with DAPT. However, the patients were not
solely confined to individuals with AF and CHADS2>1
(6), but also those with mechanical
prosthetic heart valves, deep venous thrombosis, left ventricular
thrombus or pulmonary embolism (55).
Andrade et al (56) performed
a meta-analysis of observational trials concerning triple
antithrombotic therapy following PCIS. They concluded that the rate
of major bleeding associated with TOAT was clinically significant
and higher than that for DAPT. However, the meta-analysis included
patients with left ventricular mural thrombus, pulmonary embolism,
venous or systematic thromboembolism or ACS along with AF subjects
undergoing PCIS (56). Previous
results have demonstrated that patients receiving triple
antiplatelet therapy with an INR within the lower therapeutic range
(2.0–2.5), as the recommended target, had a severe bleeding risk
compared with patients receiving dual therapy only (55). Conversely, the lower INR was effective
in preventing ischemic complications, demonstrated by low MACE rate
at long-term follow-up (55).
However, these results are not applicable to patients with
mechanical valve prostheses, who typically present with higher INR
values (54–56).
The present meta-analysis included only patients
with AF concurrent to PCIS who had undergone TOAT or DAPT. The
results suggested that TOAT reduced the occurrence of MACE and
ischemic stroke in the AF patients, potentially due to the
following factors: i) The type of thrombus in AF is mainly
fibrin-rich, and thus platelets serve a smaller role, enabling OAC
to have a more efficient prophylactic effect compared with
antiplatelet therapy for stroke prevention; and ii) anticoagulation
reduces the occurrence of thrombosis in chambers of the heart or
other locations to lower the rate of embolism events in the
coronary artery (48–50). Large-scale, randomized, prospective
and multicenter studies are now required to confirm the optimal
therapeutic strategy for patients with AF undergoing coronary
stenting.
The current meta-analysis had several limitations.
Many studies were implicated to have risk of bias. The
heterogeneity may partly be due to the variability in the
definition of clinical outcomes across studies. Information was
also lacking on the baseline characteristics of participants
regarding key variables including left ventricular ejection
fraction, smoking, body mass index, use of implantable
defibrillators and function of the CYP2C19 allele, which may have
been important confounders. Instead, much of the data were from
computerized data-bases, which may not record or classify accurate
information on study outcomes and exposures.
For future studies, a standardized individual
cardiovascular outcome should be defined based on hard end points
including MI, mortality, stroke and hemorrhage, despite the ease of
applying composite results with higher event rates. However, a
large-scale randomized controlled trial with broad rather than
restrictive selection criteria may be more useful for clinical
practice. Thus, well-designed, randomized trials are now required
to assess the optimal antithrombotic treatments in patients with AF
following PCI.
In conclusion, the current meta-analysis of nine
observational trials indicated that TOAT for patients with AF
concurrent to PCIS significantly reduced the risk of MACE and
stroke when compared with DAPT. To date, trials are too
inconsistent to establish a conclusion on the efficacy of dual and
triple therapy. Therefore, further randomized clinical controlled
trials are required to confirm the efficacy of the optimal
antithrombotic therapy in patients with AF following PCIS.
Acknowledgements
The present study was supported by the Science Fund
for Distinguished Young Scholars of the Fourth Affiliated Hospital
of Harbin Medical University (grant no: HYDSYJQ201504). The funders
had no role in the study design, data collection or analysis,
decision to publish, or preparation of the manuscript. JXL devised
and participated in the study design, collected the data and
drafted the manuscript. YL, SJY, ZYS, WS collected the data, SHL,
JWG, BHH, SY, YPC, and DJX performed the statistical analyses. XL
and XQL helped to collect the data. EZJ devised the study and
contributed to the manuscript draft. All authors read the approved
final manuscript.
References
|
1
|
Kanagaratnam L, Kowey P and Whalley D:
Pharmacological therapy for rate and rhythm control for atrial
fibrillation in 2017. Heart Lung Circ. 26:926–933. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Boriani G, Botto GL, Padeletti L, Santini
M, Capucci A, Gulizia M, Ricci R, Biffi M, De Santo T, Corbucci G,
et al: Italian AT-500 registry investigators: Improving stroke risk
stratification using the CHADS2 and CHA2DS2-VASc risk scores in
patients with paroxysmal atrial fibrillation by continuous
arrhythmia burden monitoring. Stroke. 42:1768–1770. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mazurek M, Shantsila E, Lane DA, Wolff A,
Proietti M and Lip GYH: Guideline-adherent antithrombotic treatment
improves outcomes in patients with atrial fibrillation: Insights
from the community-based Darlington atrial fibrillation registry.
Mayo Clin Proc. 92:pp. 1203–1213. 2017; View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koene RJ, Win S, Naksuk N, Adatya SN,
Rosenbaum AN, John R and Eckman PM: HAS-BLED and CHA2DS2-VASc
scores as predictors of bleeding and thrombotic risk after
continuous-flow ventricular assist device implantation. J Card
Fail. 20:800–807. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Roldán V, Marín F, Manzano-Fernández S,
Gallego P, Vílchez JA, Valdés M, Vicente V and Lip GY: The HAS-BLED
score has better prediction accuracy for major bleeding than CHADS2
or CHA2DS2-VASc scores in anticoagulated patients with atrial
fibrillation. J Am Coll Cardiol. 62:2199–2204. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Apostolakis S, Lane DA, Buller H and Lip
GY: Comparison of the CHADS2, CHA2DS2-VASc and HAS-BLED scores for
the prediction of clinically relevant bleeding in anticoagulated
patients with atrial fibrillation: The AMADEUS trial. Thromb
Haemost. 110:1074–1079. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Angiolillo DJ, Goodman SG, Bhatt DL,
Eikelboom JW, Price MJ, Moliterno DJ, Cannon CP, Tanguay JF,
Granger CB, Mauri L, et al: Antithrombotic therapy in patients with
atrial fibrillation undergoing percutaneous coronary intervention:
A North American Perspective-2016 Update. Circ Cardiovasc Interv.
9:92016. View Article : Google Scholar
|
|
8
|
Kralev S, Schneider K, Lang S, Süselbeck T
and Borggrefe M: Incidence and severity of coronary artery disease
in patients with atrial fibrillation undergoing first-time coronary
angiography. PLoS One. 6:e249642011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nieuwlaat R, Capucci A, Camm AJ, Olsson
SB, Andresen D, Davies DW, Cobbe S, Breithardt G, Le Heuzey JY,
Prins MH, et al European Heart Survey Investigators, : Atrial
fibrillation management: A prospective survey in ESC member
countries: The Euro Heart Survey on Atrial Fibrillation. Eur Heart
J. 26:2422–2434. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nabauer M, Gerth A, Limbourg T, Schneider
S, Oeff M, Kirchhof P, Goette A, Lewalter T, Ravens U, Meinertz T,
et al: The registry of the German competence NETwork on atrial
fibrillation: Patient characteristics and initial management.
Europace. 11:423–434. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rossini R, Musumeci G, Lettieri C, Molfese
M, Mihalcsik L, Mantovani P, Sirbu V, Bass TA, Della Rovere F,
Gavazzi A, et al: Long-term outcomes in patients undergoing
coronary stenting on dual oral antiplatelet treatment requiring
oral anticoagulant therapy. Am J Cardiol. 102:1618–1623. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang TY, Robinson LA, Ou FS, Roe MT, Ohman
EM, Gibler WB, Smith SC Jr, Peterson ED and Becker RC: Discharge
antithrombotic strategies among patients with acute coronary
syndrome previously on warfarin anticoagulation: Physician practice
in the CRUSADE registry. Am Heart J. 155:361–368. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rubboli A, Colletta M, Valencia J,
Capecchi A, Franco N, Zanolla L, La Vecchia L, Piovaccari G and Di
Pasquale G; WARfarin and Coronary STENTing (WAR-STENT) study group,
: Periprocedural management and in-hospital outcome of patients
with indication for oral anticoagulation undergoing coronary artery
stenting. J Interv Cardiol. 22:390–397. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Capodanno D and Angiolillo DJ: Management
of antiplatelet and anticoagulant therapy in patients with atrial
fibrillation in the setting of acute coronary syndromes or
percutaneous coronary interventions. Circ Cardiovasc Interv.
7:113–124. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Authors/Task Force members, ; Windecker S,
Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm
C, Head SJ, et al: 2014 ESC/EACTS guidelines on myocardial
revascularization: The task force on myocardial revascularization
of the European Society of Cardiology (ESC) and the European
Association for Cardio-Thoracic Surgery (EACTS). Developed with the
special contribution of the European Association of Percutaneous
Cardiovascular Interventions (EAPCI). Eur Heart J. 35:2541–2619.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Windecker S, Kolh P, Alfonso F, Collet JP,
Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüniet P, et al:
2014 ESC/EACTS guidelines on myocardial revascularization. Rev Esp
Cardiol. 68:4522015.
|
|
17
|
Gurbel PA, Bliden KP, Hiatt BL and
O'Connor CM: Clopidogrel for coronary stenting: Response
variability, drug resistance, and the effect of pretreatment
platelet reactivity. Circulation. 107:2908–2913. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
James SK, Roe MT, Cannon CP, Cornel JH,
Horrow J, Husted S, Katus H, Morais J, Steg PG, Storey RF, et al
PLATO Study Group, : Ticagrelor versus clopidogrel in patients with
acute coronary syndromes intended for non-invasive management:
Substudy from prospective randomised PLATelet inhibition and
patient outcomes (PLATO) trial. BMJ. 342:35272011. View Article : Google Scholar
|
|
19
|
Held C, Asenblad N, Bassand JP, Becker RC,
Cannon CP, Claeys MJ, Harrington RA, Horrow J, Husted S, James SK,
et al: Ticagrelor versus clopidogrel in patients with acute
coronary syndromes undergoing coronary artery bypass surgery:
Results from the PLATO (Platelet Inhibition and Patient Outcomes)
trial. J Am Coll Cardiol. 57:672–684. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gwyn JCV, Thomas MR and Kirchhof P: Triple
antithrombotic therapy in patients with atrial fibrillation
undergoing percutaneous coronary intervention: A viewpoint. Eur
Heart J Cardiovasc Pharmacother. 3:157–162. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lopes RD, Rao M, Simon DN, Thomas L,
Ansell J, Fonarow GC, Gersh BJ, Go AS, Hylek EM, Kowey P, et al:
Triple vs dual antithrombotic therapy in patients with atrial
fibrillation and coronary artery disease. Am J Med. 129:592–599.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pareek M, Bhatt DL, Ten Berg JM,
Kristensen SD and Grove EL: Antithrombotic strategies for
preventing long-term major adverse cardiovascular events in
patients with non-valvular atrial fibrillation who undergo
percutaneous coronary intervention. Expert Opin Pharmacother.
18:875–883. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Choi HI, Ahn JM, Kang SH, Lee PH, Kang SJ,
Lee SW, Kim YH, Lee CW, Park SW, Park DW, et al: Prevalence,
management, and long-term (6-year) outcomes of atrial fibrillation
among patients receiving drug-eluting coronary stents. JACC
Cardiovasc Interv. 10:1075–1085. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lamberts M, Olesen JB, Ruwald MH, Hansen
CM, Karasoy D, Kristensen SL, Køber L, Torp-Pedersen C, Gislason GH
and Hansen ML: Bleeding after initiation of multiple antithrombotic
drugs, including triple therapy, in atrial fibrillation patients
following myocardial infarction and coronary intervention: A
nationwide cohort study. Circulation. 126:1185–1193. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kang DO, Yu CW, Kim HD, Cho JY, Joo HJ,
Choi RK, Park JS, Lee HJ, Kim JS, Park JH, et al: Triple
antithrombotic therapy versus dual antiplatelet therapy in patients
with atrial fibrillation undergoing drug-eluting stent
implantation. Coron Artery Dis. 26:372–380. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gao F, Zhou YJ, Wang ZJ, Shen H, Liu XL,
Nie B, Yan ZX, Yang SW, Jia de A and Yu M: Comparison of different
antithrombotic regimens for patients with atrial fibrillation
undergoing drug-eluting stent implantation. Circ J. 74:701–708.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fosbol EL, Wang TY, Li S, Piccini JP,
Lopes RD, Shah B, Mills RM, Klaskala W, Alexander KP, Thomas L, et
al: Safety and effectiveness of antithrombotic strategies in older
adult patients with atrial fibrillation and non-ST elevation
myocardial infarction. Am Heart J. 163:720–728. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Manzano-Fernández S, Pastor FJ, Marín F,
Cambronero F, Caro C, Pascual-Figal DA, Garrido IP, Pinar E, Valdés
M and Lip GYH: Increased major bleeding complications related to
triple antithrombotic therapy usage in patients with atrial
fibrillation undergoing percutaneous coronary artery stenting.
Chest. 134:559–567. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Maegdefessel L, Schlitt A, Faerber J, Bond
SP, Messow CM, Buerke M, Raaz U, Werdan K, Muenzel T and Weiss C:
Anticoagulant and/or antiplatelet treatment in patients with atrial
fibrillation after percutaneous coronary intervention. A
single-center experience. Med Klin (Munich). 103:628–632. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hansen ML, Sørensen R, Clausen MT,
Fog-Petersen ML, Raunsø J, Gadsbøll N, Gislason GH, Folke F,
Andersen SS, Schramm TK, et al: Risk of bleeding with single, dual,
or triple therapy with warfarin, aspirin, and clopidogrel in
patients with atrial fibrillation. Arch Intern Med. 170:1433–1441.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hess CN, Peterson ED, Peng SA, de Lemos
JA, Fosbol EL, Thomas L, Bhatt DL, Saucedo JF and Wang TY: Use and
outcomes of triple therapy among older patients with acute
myocardial infarction and atrial fibrillation. J Am Coll Cardiol.
66:616–627. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rao AK, Pratt C, Berke A, Jaffe A, Ockene
I, Schreiber TL, Bell WR, Knatterud G, Robertson TL and Terrin ML:
Thrombolysis in Myocardial Infarction (TIMI) Trial-phase I:
Hemorrhagic manifestations and changes in plasma fibrinogen and the
fibrinolytic system in patients treated with recombinant tissue
plasminogen activator and streptokinase. J Am Coll Cardiol.
11:1–11. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li JX, Jin EZ, Yu LH, Li Y, Liu NN, Dong
YM, Li X and Li XQ: Oral N-acetylcysteine for prophylaxis of
contrast-induced nephropathy in patients following coronary
angioplasty: A meta-analysis. Exp Ther Med. 14:1568–1576. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Stang A: Critical evaluation of the
Newcastle-Ottawa scale for the assessment of the quality of
nonrandomized studies in meta-analyses. Eur J Epidemiol.
25:603–605. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lip GY, Windecker S, Huber K, Kirchhof P,
Marin F, Ten Berg JM, Haeusler KG, Boriani G, Capodanno D, Gilard
M, et al: Document reviewers: Management of antithrombotic therapy
in atrial fibrillation patients presenting with acute coronary
syndrome and/or undergoing percutaneous coronary or valve
interventions: A joint consensus document of the European Society
of Cardiology Working Group on Thrombosis, European Heart Rhythm
Association (EHRA), European Association of Percutaneous
Cardiovascular Interventions (EAPCI) and European Association of
Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society
(HRS) and Asia-Pacific Heart Rhythm Society (APHRS). Eur Heart J.
35:3155–3179. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
JCS Joint Working Group, . Guidelines for
pharmacotherapy of atrial fibrillation (JCS 2013). Circ J.
78:1997–2021. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Heidenreich PA, Solis P, Estes NA III,
Fonarow GC, Jurgens CY, Marine JE, McManus DD and McNamara RL: 2016
ACC/AHA Clinical performance and quality measures for adults with
atrial fibrillation or atrial flutter: A report of the American
College of Cardiology/American Heart Association Task Force on
Performance Measures. J Am Coll Cardiol. 68:525–568. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Elewa H, Ahmed D and Barnes GD: Triple
oral antithrombotic therapy in atrial fibrillation and coronary
artery stenting: Searching for the best combination. Semin Thromb
Hemost. 42:662–670. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Camm AJ, Kirchhof P, Lip GY, Schotten U,
Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G,
Prendergast B, et al European Heart Rhythm Association, ; European
Association for Cardio-Thoracic Surgery, : Guidelines for the
management of atrial fibrillation: The Task Force for the
management of Atrial Fibrillation of the European Society of
Cardiology (ESC). Eur Heart J. 31:2369–2429. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Halvorsen S, Storey RF, Rocca B, Sibbing
D, Ten Berg J, Grove EL, Weiss TW, Collet JP, Andreotti F, Gulba
DC, et al ESC Working Group on Thrombosis, : Management of
antithrombotic therapy after bleeding in patients with coronary
artery disease and/or atrial fibrillation: Expert consensus paper
of the European Society of Cardiology working group on thrombosis.
Eur Heart J. 38:1455–1462. 2017.PubMed/NCBI
|
|
41
|
Hart RG, Pearce LA and Aguilar MI:
Meta-analysis: Antithrombotic therapy to prevent stroke in patients
who have nonvalvular atrial fibrillation. Ann Intern Med.
146:857–867. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Peters RJ, Mehta SR, Fox KA, Zhao F, Lewis
BS, Kopecky SL, Diaz R, Commerford PJ, Valentin V and Yusuf S;
Clopidogrel in Unstable angina to prevent Recurrent Events (CURE)
Trial Investigators, : Effects of aspirin dose when used alone or
in combination with clopidogrel in patients with acute coronary
syndromes: Observations from the clopidogrel in unstable angina to
prevent recurrent events (CURE) study. Circulation. 108:1682–1687.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sabatine MS, Cannon CP, Gibson CM,
López-Sendón JL, Montalescot G, Theroux P, Lewis BS, Murphy SA,
McCabe CH and Braunwald E; Clopidogrel as Adjunctive Reperfusion
Therapy (CLARITY)-Thrombolysis in Myocardial Infarction (TIMI) 28
Investigators, : Effect of clopidogrel pretreatment before
percutaneous coronary intervention in patients with ST-elevation
myocardial infarction treated with fibrinolytics: The PCI-CLARITY
study. JAMA. 294:1224–1232. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wijns W, Kolh P, Danchin N, Di Mario C,
Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, et al Task
Force on Myocardial Revascularization of the European Society of
Cardiology (ESC) and the European Association for Cardio-Thoracic
Surgery (EACTS), ; European Association for Percutaneous
Cardiovascular Interventions (EAPCI), : Guidelines on myocardial
revascularization. Eur Heart J. 31:2501–2555. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wallentin L, James S, Storey RF, Armstrong
M, Barratt BJ, Horrow J, Husted S, Katus H, Steg PG, Shah SH, et
al: Effect of CYP2C19 and ABCB1 single nucleotide polymorphisms on
outcomes of treatment with ticagrelor versus clopidogrel for acute
coronary syndromes: A genetic substudy of the PLATO trial. Lancet.
376:1320–1328. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Khayata M, Gabra JN, Nasser MF, Litman GI,
Bhakta S and Raina R: Comparison of clopidogrel with prasugrel and
ticagrelor in patients with acute coronary syndrome: Clinical
outcomes from the national cardiovascular database ACTION registry.
Cardiol Res. 8:105–110. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
O'Gara PT, Kushner FG, Ascheim DD, Casey
DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM,
Franklin BA, et al American College of Emergency Physicians, ;
Society for Cardiovascular Angiography and Interventions, : 2013
ACCF/AHA guideline for the management of ST-elevation myocardial
infarction: A report of the American College of Cardiology
Foundation/American Heart Association Task Force on Practice
Guidelines. J Am Coll Cardiol. 61:e78–e140. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Reed GW and Cannon CP: Triple oral
antithrombotic therapy in atrial fibrillation and coronary artery
stenting. Clin Cardiol. 36:585–594. 2013.PubMed/NCBI
|
|
49
|
Dzeshka MS, Brown RA and Lip GY: Patients
with atrial fibrillation undergoing percutaneous coronary
intervention. Current concepts and concerns: Part I. Pol Arch Med
Wewn. 125:73–81. 2015.PubMed/NCBI
|
|
50
|
Dzeshka MS, Brown RA and Lip GY: Patients
with atrial fibrillation undergoing percutaneous coronary
intervention: Current concepts and concerns: Part II. Pol Arch Med
Wewn. 125:172–180. 2015.PubMed/NCBI
|
|
51
|
Lamberts M, Gislason GH, Olesen JB,
Kristensen SL, Schjerning Olsen AM, Mikkelsen A, Christensen CB,
Lip GY, Køber L, Torp-Pedersen C, et al: Oral anticoagulation and
antiplatelets in atrial fibrillation patients after myocardial
infarction and coronary intervention. J Am Coll Cardiol.
62:981–989. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Thompson PL and Verheugt FW: Managing
antithrombotic therapy in patients with both atrial fibrillation
and coronary heart disease. Clin Ther. 36:1176–1181. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Gao F, Zhou YJ, Wang ZJ, Yang SW, Nie B,
Liu XL, Jia A and Yan ZX: Meta-analysis of the combination of
warfarin and dual antiplatelet therapy after coronary stenting in
patients with indications for chronic oral anticoagulation. Int J
Cardiol. 148:96–101. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Zhao HJ, Zheng ZT, Wang ZH, Li SH, Zhang
Y, Zhong M and Zhang W: ‘Triple therapy’ rather than ‘triple
threat’: A meta-analysis of the two antithrombotic regimens after
stent implantation in patients receiving long-term oral
anticoagulant treatment. Chest. 139:260–270. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Saheb KJ, Deng BQ, Hu QS, Xie SL, Geng DF
and Nie RQ: Triple antithrombotic therapy versus double
antiplatelet therapy after percutaneous coronary intervention with
stent implantation in patients requiring chronic oral
anticoagulation: A meta-analysis. Chin Med J (Engl). 126:2536–2542.
2013.PubMed/NCBI
|
|
56
|
Andrade JG, Deyell MW, Khoo C, Lee M,
Humphries K and Cairns JA: Risk of bleeding on triple
antithrombotic therapy after percutaneous coronary
intervention/stenting: A systematic review and meta-analysis. Can J
Cardiol. 29:204–212. 2013. View Article : Google Scholar : PubMed/NCBI
|