Introduction
Metastatic breast cancer is a prevalent cause of
mortality in the US population. The American Cancer Society has
projected approximately 246,660 newly diagnosed invasive breast
cancer cases and approximately 40,450 breast cancer-related deaths
in women in 2017 and the life time breast cancer risk is estimated
at 1 in 8 individuals (1). These
actuarial data emphasize a need to identify specific and sensitive
prognostic and predictive biomarkers and efficacious cancer subtype
specific-targeted therapy.
Conventional chemo-endocrine therapeutic options for
clinical breast cancer are based on the status of hormone
receptors, proliferation and cell apoptosis. Additionally, global
profiling of differentially expressed genes has facilitated the
molecular/genetic classification of breast cancer subtypes, and
thus, has provided rational subtype-based treatment options
(2).
The Luminal A molecular subtype is classified as
estrogen receptor (ER)-positive, progesterone receptor
(PR)-positive and human epidermal growth factor receptor-2
(HER-2)-negative breast cancer. The Luminal B subtype is
characterized by the presence of all three abovementioned
receptors. The treatment options for the two subtypes include the
use of selective ER modulators and aromatase inhibitors, with or
without HER-2 targeted therapy. The triple negative molecular
subtype is classified as ER-negative, PR-negative and
HER-2-negative breast cancer which responds only to conventional
chemotherapy and select cellular signaling pathway specific small
molecular inhibitors (2–5).
Current long-term treatment options for conventional
chemo-endocrine therapy and for small molecular based-targeted
therapy are frequently associated with acquired tumor resistance
due to the emergence of drug-resistant stem cell population. These
limitations compromise therapeutic efficacy and promote
drug-resistant disease progression (3,4,6). Preclinical studies on human tissue
derived cell culture models may facilitate investigations directly
on the target tissue to reduce extrapolation and enhance clinical
translatability, thereby, providing facile in vitro
experimental approaches that are complementary to conventional
in vivo approaches (3,4).
Natural products such as dietary supplements,
phytochemicals and herbal formulations have been extensively used
either as palliative or adjuvant treatment options for breast
cancer patients in complementary and alternative medicine (7–9). These
agents, due to their inherently minimal toxicity, may provide
testable alternatives for limitations of conventional
chemo-endocrine and small molecular-targeted therapeutic options.
Previously published data on cell culture models for Luminal A,
HER-2 enriched and triple negative molecular subtypes of clinical
breast cancer have demonstrated that several mechanistically
distinct natural phytochemicals and herbal extracts function as
cytostatic and pro-apoptotic agents conferring potent growth
inhibitory efficacy in these clinically relevant model systems
(10–21).
The present review summarizes experimental evidence
identifying novel mechanistic leads for the efficacy of select
natural products and their respective constituent bioactive
components in the clinically relevant cell culture model for triple
negative breast cancer, and provides experimental evidence
supporting the development of a drug-resistant cancer stem model.
Furthermore, this review suggests a testable approach for cancer
stem cell-targeted therapeutic options for chemoendocrine
therapy-resistant aggressive breast cancer.
Experimental models
184-B5 model
This model was derived from a human reduction
mammoplasty specimen. The cells were ER−, PR−
and HER-2− and non-tumorigenic (22). This cell line served as the baseline
control for quantitative growth parameters.
MDA-MB-231 model
The triple negative molecular subtype of clinical
breast cancer lacks the expression of ER, PR and HER-2 (2). The human mammary carcinoma-derived
MDA-MB-231 cells lack the expression of the three receptors
(23,24). This cell line represents a model for
the triple negative breast cancer subtype.
Mechanistic biomarkers
Growth parameters
Conventional quantitative parameters such as
population doubling time and saturation density have been widely
used as endpoints to quantify growth. Population doubling time is
monitored during the four-day exponential growth phase by
determining cell viability. The data are expressed as arithmetic
mean from the four time points. Saturation density is determined by
viable cell number at day 7 post-seeding (16–18).
Anchorage-independent growth
assay
Anchorage-independent growth is a sensitive and
specific in vitro surrogate endpoint for the tumorigenic
potential of carcinoma-derived cell lines (12–15,19–21). For
this assay, 184-B5 and MDA-MB-231 cell lines at a predetermined
cell density were suspended in 0.33% agar and overlaid on a
basement layer of 0.6% agar. The anchorage-independent colony
counts were performed at day 21 post-seeding.
Cell cycle progression and cell
apoptosis
The parameters were quantified by flow
cytometry-based fluorescence-assisted cell sorting. Cell
populations in the G1, S, G2/M and sub
G0 phases of cell cycle were then monitored. The data
are expressed as G1:S+G2/M ratio,
S+G2/M:sub G0 ratio, and % sub G0
population (17,19–21).
Drug-resistant cancer stem cells
Drug-resistant phenotype was isolated from a
subpopulation of Doxorubicin-resistant (DOX-R) MDA-MB-231 cells. To
isolate the DOX-R phenotype, MDA-MB-231 cells were treated with 0.5
µM DOX (maximum cytostatic concentration) for 7 days. The surviving
cell population was expanded in the presence of 0.5 µM DOX for at
least 5 passages prior to the experiments. The DOX-R cells were
monitored for the status of stem cell-specific markers, including
tumor spheroid formation, and expression of stem cell-specific
molecular markers CD44, NANOG and c-Myc. The spheroid formation was
monitored by tumor spheroid colony counts in serum-free culture
conditions on day 14 post-seeding of 100 drug-resistant cells in
ultralow adherence culture plates. The expression of stem
cell-specific molecular markers CD44, NANOG and c-Myc was monitored
by fluorescence-assisted cell sorting of DOX-R cells stained with
specific fluorescein isothiocyanate (FITC)-labeled antibodies
according to the optimized protocol provided by the vendors. These
data were then normalized to FITC-IgG, and expressed as log mean
fluorescence units (17).
Natural products
Non-fractionated extracts from dietary natural
products, as well as their constitutive bioactive phytochemicals
were selected as the test agents based on the evidence supporting
cancer chemo-preventive efficacy in the animal models for organ
site cancer (16–18). The test agents used in the experiments
are presented in Table I.
 | Table I.Natural product test agents. |
Table I.
Natural product test agents.
| Test agent | Natural source |
|---|
| Dietary
supplements |
|
|
OPE | Citrus fruits,
limonoids |
|
RME | Rosemary leaves,
phenolic terpenoids |
|
GTE | Green tea leaves,
polyphenols |
| Constitutive
bioactive phytochemicals |
|
| UA | Tri-terpenoid |
|
EGCG | Tea polyphenol |
Dose response experiments were utilized to identify
maximum cytostatic concentrations (IC90). The maximum
cytostatic concentration was defined as the highest concentration
of the test compound that produces a viable cell number that is
equal to the initial seeding density. The concentration producing
viable cell number that was lower than the initial seeding density
was considered toxic. These pre-determined maximum cytostatic
concentrations of the test compounds were used in the experiments
to evaluate their growth inhibitory effects and mechanistic
efficacy.
Efficacy of natural products
Status of homeostatic growth control
in triple negative model
To identify growth advantage of the model, growth
parameters of tumorigenic ER−, PR−and
HER-2− MDA-MB-231 (triple negative) cells were compared
against the non-tumorigenic ER−, PR− and
HER-2− 184-B5 (triple negative) cells, representing the
baseline control. These data demonstrated that relative to 184-B5
cells, the triple negative tumor-derived cell line exhibits a 54.7%
decrease in population doubling, and a 48.8% increase in saturation
density (Table II). Additionally,
this cell line exhibits a 72.2% decrease in
G1:S+G2/M ratio due to aberrant
hyper-proliferation and a 9-fold increase in the
S+G2/M:Sub G0 ratio due to downregulated cell
apoptosis. It is also noteworthy that unlike the non-tumorigenic
control cells, the tumor-derived cells exhibit
anchorage-independent growth as demonstrated by a substantial 97.5%
increase in the number of anchorage-independent colonies.
Collectively, these data demonstrate that the tumorigenic cell line
that is hyper-proliferative, less apoptotic and exhibits
anchorage-independent growth, displays loss of homeostatic growth
control and persistent cancer risk. Furthermore, these growth
properties of human tumorigenic cells, which are distinct from
those of non-tumorigenic human cells provide evidence to support a
clinical relevance for the experimental models (16,18–21).
 | Table II.Status of homeostatic growth control
in triple negative MDA-MB-231 cells. |
Table II.
Status of homeostatic growth control
in triple negative MDA-MB-231 cells.
|
| Relative to 184-B5
cellsa |
|---|
|
|
|
|---|
| Biomarker | Range | Median |
|---|
| Population
doubling | −53.6 to
−55.9% |
−54.7% |
| Saturation
density | +47.5
to +50.2% |
+48.8% |
|
G1:S+G2/M | −70.5 to
−73.9% | −72.2% |
| S+G2/M:
Sub G0 | +8.5 to +9.5X | +9.0X |
|
Anchorage-independent colony
formation | +95% to +100% | +97.5% |
Efficacy of natural products and
constitutive bioactive phytochemicals in triple negative model
The triple negative subtype lacks the expression of
hormone and growth factor receptors and therefore is resistant to
endocrine therapy and to HER-2-targeted therapy (2,4,5). The response of the triple negative
subtype to cytotoxic chemotherapy and to molecular pathway-targeted
therapy is associated with acquired tumor resistance and emergence
of drug-resistant cancer stem cells (4–6,25,26). The
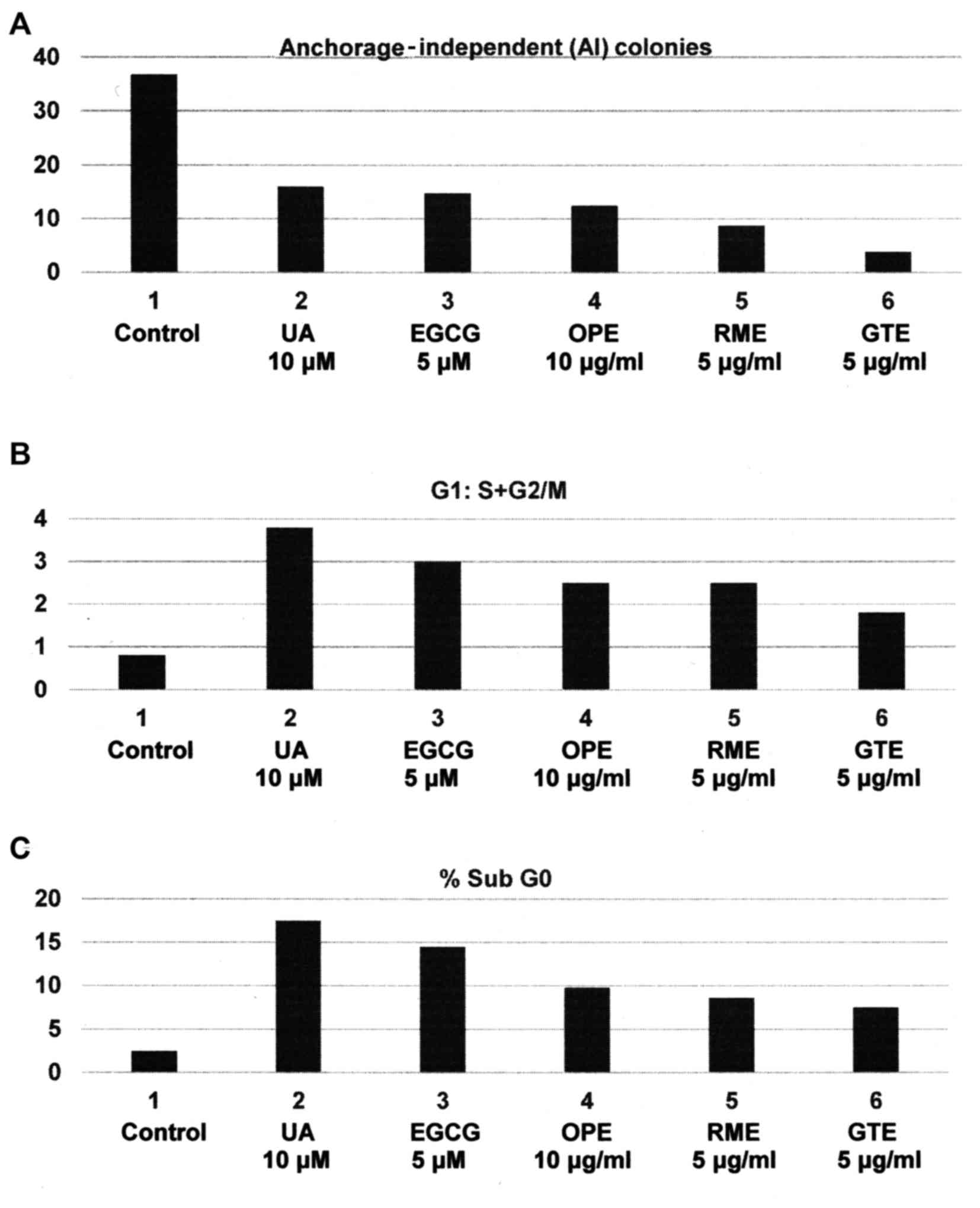
experiments presented in Fig. 1A-C
were designed to examine the growth inhibitory effects of dietary
supplements orange peel extract (OPE), rosemary extract (RME),
green tea extract (GTE) and their constitutive bioactive agents
ursolic acid (UA) and epigallocatechin gallate (EGCG) on the triple
negative MDA-MB-231 model. The test agents inhibited
anchorage-independent colony formation at their respective maximum
cytostatic concentrations (Fig. 1A).
The cytostatic effect of these test agents on cell cycle
progression was associated with G1 arrest, leading to an
increased G1:S+G2/M ratio (Fig. 1B). Increased
G1:S+G2/M ratio occured predominantly due to
G1 arrest and the resultant inhibition of G1
to S phase transition, leading to investigation on the status of
G1-specific cyclins and other relevant signaling
proteins. Additionally, the pro-apoptotic effect was evidenced by
increases of cell population in apoptotic sub G0 phase
of the cell cycle (Fig. 1C). The
observed increase in the sub G0 population leading to
investigation on the status of apoptosis-related proteins. The
statistical significance of these data were analyzed by one-way
analysis of variance (ANOVA) and Dunnett's multiple comparison test
(α=0.05). Collectively, these data provide mechanistic leads to
identify potential molecular targets responsible for the efficacy
of relatively non-toxic naturally occurring agents and suggest
testable alternative to therapy-resistant triple negative breast
cancer (16,18,27).
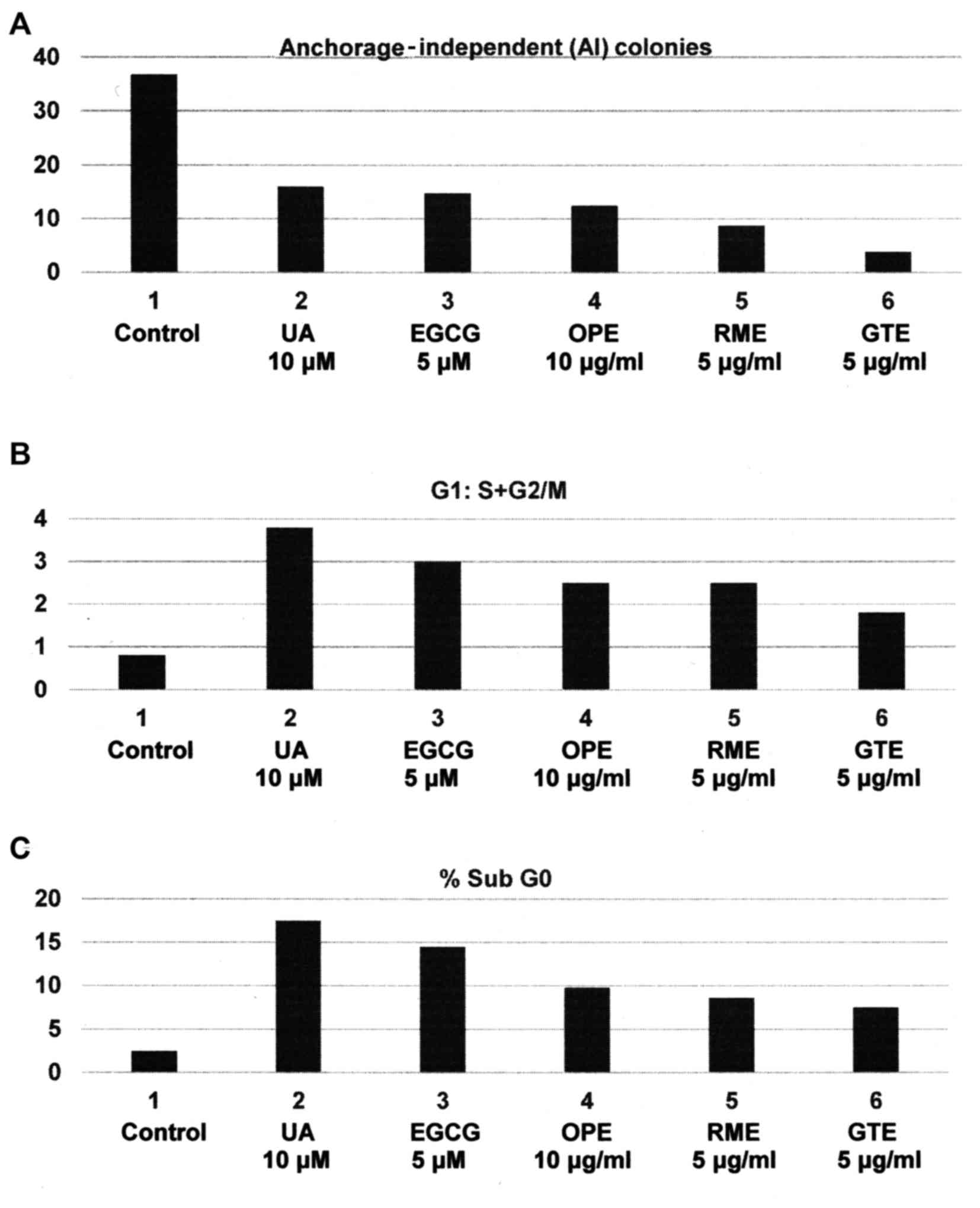 | Figure 1.Efficacy of natural products and
constitutive bioactive agents in triple negative MDA-MB-231 cells:
(A) Inhibition of anchorage-independent colony formation. Treatment
with respective maximum cytostatic concentrations of constitutive
bioactive agents UA and EGCG, and dietary supplements OPE, RME and
GTE. Colony counts at day 21 post-seeding of 1,000 cells. Control
> UA, EGCG, OPE, RME and GTE (one-way ANOVA) and Dunnett's
multiple comparison test (α=0.05). (B) Increase in
G1:S+G2/M ratio. Cells treated for 24 h with
maximum cytostatic concentrations of constitutive bioactive agents
and dietary supplements. Cell cycle analysis by flow cytometry.
Control < UA, EGCG, OPE, RME and GTE. One-way ANOVA and
Dunnett's multiple comparison test (α=0.05). (C) Induction of cell
apoptosis. Cells treated for 24 h with maximum cytostatic
concentrations of constitutive bioactive agents and dietary
supplements. Quantification of cells in the sub G0
(apoptotic) phase by flow cytometry. Control < UA, EGCG, OPE,
RME and GTE. One-way ANOVA and Dunnett's multiple comparison test
(α=0.05). UA, ursolic acid; EGCG, epigallocatechin gallate; OPE,
orange peel extract; RME, rosemary extract; GTE, green tea
extract. |
Several mechanistically distinct natural products
have exhibited growth inhibitory efficacy in HER-2 expressing human
mammary epithelial cells that represent a cellular model for HER-2
enriched breast cancer. The molecular mechanisms responsible for
the anti-proliferative and pro-apoptotic efficacy of these agents
include G1 arrest and inhibition of
G1-specific cyclins and modulation of apoptotic-specific
proteins (16,18). Additionally, chemo-preventive agents
including resveratrol, retinoids and rosemary terpenoids exhibit
effective inhibition of inducible cyclo-oxygenase-2 (COX-2)
activity in this model (28–31).
In the current context it is noteworthy that in the
triple negative subtype, the tumor suppressive function of the
RB gene is frequently compromised (32,33). Thus,
the CyclinD-CDK4/6-pRB pathway has been exploited as a therapeutic
target (34,35). Additionally, the present cellular model
for triple negative breast cancer subtype harbors a
gain-of-function R280K mutation in the tumor suppressor TP53
gene that confers survival advantage via the upregulation of cell
migration and invasion (36). Thus,
the present status of TP53 may be an additional therapeutic
target.
Nutritional herbs are commonly used in herbal
formulations for the treatment of breast cancer patients (7–9,37). Thus, preliminary evidence suggests that
in the present triple negative model, nutritional herbs Tabebiua
avellandae, Cornus officinalis and Dipsacus
asperoides confer growth inhibitory effects via the RB pathway,
and pro-apoptotic effects via the intrinsic mitochondrial BAX and
caspase pathways (19–21).
Cancer stem cells in triple negative
model
Acquired tumor resistance to chemo-endocrine therapy
is associated with the emergence of drug-resistant stem cells
(4,6).
Furthermore, acquired resistance to small molecular inhibitors of
PI3K/AKT/mTOR pathways in the triple negative subtype (4,5,25), emphasizes investigations focused on a
therapy-resistant stem cell population.
Select nuclear transcription factors Oct-3/4, Klf4,
Sox2 and c-Myc (Yamanaka factors) are expressed in cancer stem
cells derived from multiple organ sites (38–43). These
transcription factors are also essential for the induction of
pluripotent stem cells derived from adult somatic cells (44–47). The
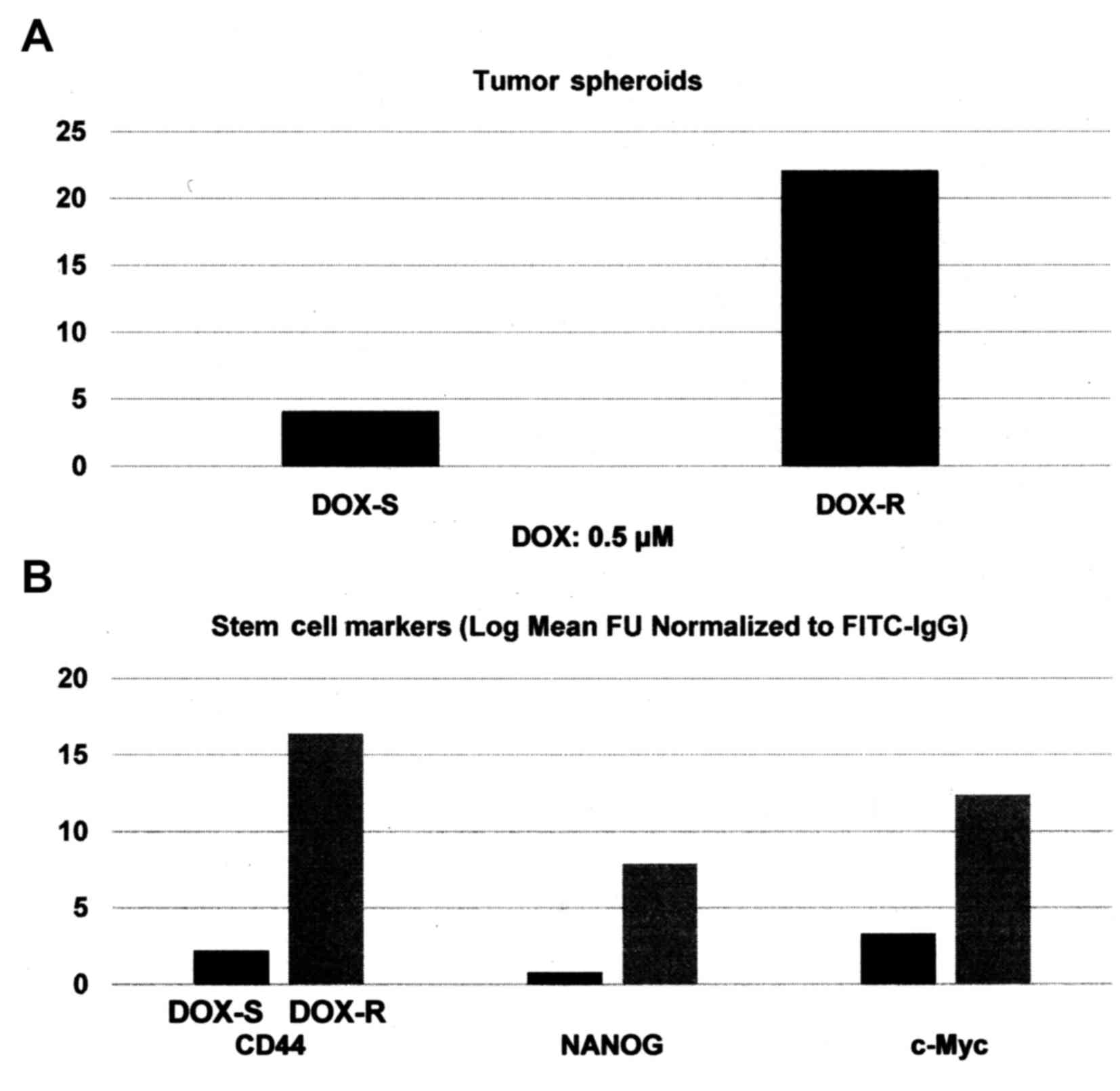
experiments presented in Fig. 2A and B
were designed to examine the status of select stem cell markers in
DOX-R MDA-MB-231 phenotype. Relative to the drug sensitive
phenotype, the DOX-R phenotype exhibited a 4.4-fold increase
(P=0.02) in the number of tumor spheroids (Fig. 2A). Additionally, in the DOX-R phenotype
the expression of stem cell-specific cellular marker CD44 exhibited
a 6.4-fold increase (P=0.02), while the molecular markers NANOG
exhibited an 8.8-fold increase (P=0.01) and c-Myc exhibited a
2.7-fold increase (P=0.03), relative to the DOX-S phenotype
(Fig. 2B). These data were analyzed
for their statistical significance by the two-sample t-test.
Collectively, these data on the status of stem cell marker
expression characterize the DOX-R stem cell model, thereby
validating an experimental approach for the evaluation of
stem-targeted therapeutic efficacy.
Ongoing research directions include experiments
designed to examine the efficacy of promising natural products on
the developed triple negative breast cancer stem cell model. These
studies are expected to provide evidence for effective-targeted
intervention directly on therapy-resistant breast cancer stem
cells.
Conclusions and future directions
Human tissue-derived preclinical models may reduce
extrapolation of evidence for clinically relevant translational
potential (16,18,41). Current
research directions have provided optimized human tissue-derived
cell culture models for triple negative molecular subtype of
clinical breast cancer that represent a clinically relevant
experimental system. The present data on the growth inhibitory
efficacy of natural products such as dietary supplements and their
constitutive bioactive agents validates an experimental approach to
evaluate natural products as testable alternatives for
chemo-endocrine therapy-resistant breast cancer.
Acquired tumor resistance to conventional
chemo-endocrine therapy and selection of a survival
pathway-targeted therapy are frequently observed phenomena
responsible for compromised therapeutic efficacy and disease
progression. It occurs predominantly due to the emergence of
drug-resistant stem cells (6,40,41). Data
presented on the isolation and characterization of DOX-resistant
triple negative MDA-MB-231 cells validate a potential model for
stem cell-targeted therapy.
In the present context, it needs to be recognized
that the cell culture models derived from established cell lines
provide only limited clinical relevance. Therefore, future research
directions focusing on ex vivo approaches for
patient-derived xenografts from therapy-resistant breast cancer
subtypes, reliable stem cell models from clinical samples, and
cellular/molecular approaches to evaluate lead compound efficacy
targeted towards cancer stem cells are expected to provide valuable
means to attain better clinical translatability.
Acknowledgements
Productive collaborations with former colleagues Drs
Meena Katdare, Kotha Subbaramaiah, Andrew Dannenberg, Daniel
Sepkovic, H. Leon Bradlow, George Y.C. Wong and Michael P. Osborne
are gratefully acknowledged. Research Programs in the author's
laboratory have been funded by the National Cancer Institute
Grants/Contracts (CA-44741, CA-29502 and CN-75029-63), Department
of Defense Breast Cancer Research Program (IDEA Award
DAMD17-94-J-4208), and by philanthropic funds to the Strang Cancer
Prevention Center and to the American Foundation for Chinese
Medicine.
References
|
1
|
American Cancer Society - Facts and
Figures. American Cancer Society. Atlanta: 2016.
|
|
2
|
Sørlie T, Perou CM, Tibshirani R, Aas T,
Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M and Jeffrey
SS: Gene expression patterns of breast carcinomas distinguish tumor
subclasses with clinical implications. Proc Natl Acad Sci USA.
98:10869–10874. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Baselga J and Swain SM: Novel anti-cancer
agents: Revisiting ERBB2 and discovering ERBB3. Nat Rev Cancer.
9:463–475. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dinh P, Satirou C and Piccart MJ: The
evaluation of treatment strategies: Aiming at the target.
16:S10–S16. 2007.
|
|
5
|
Anders CK, Winer EP, Ford JM, Dent R,
Silver DP, Sledge GW and Carey LA: Poly (ADP-ribose) inhibition:
Targeted therapy for triple negative breast cancer. Clin Cancer
Res. 16:4702–4710. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dean M, Fojo T and Bates S: Tumor stem
cells and drug resistance. Nat Rev Cancer. 5:275–284. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tindle HA, Davis RB, Phillips RL and
Eisenburg DM: Trends in the use of complementary and alternative
medicines by US adults: 1997-2002. Altern Ther Health Med.
11:42–49. 2005.PubMed/NCBI
|
|
8
|
Molassiotis A, Scott JA, Kearney N, Pud D,
Magri M, Selvekerova S, Bruyns I, Fernadez-Ortega P, Panteli V,
Margulies A and Gudmundsdottir G: Complementary and alternative
medicine use in breast cancer patient in Europe. Support Care
Cancer. 14:206–267. 2006. View Article : Google Scholar
|
|
9
|
Helyer LK, Chin S, Chui BK, Fitzgerald B,
Verma S, Rakovitch E, Dranitsaris G and Clemons M: The use of
complementary and alternative medicine among patients with locally
advanced breast cancer. A descriptive study. BMC Cancer. 6:39–46.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mukherjee B, Telang N and Wong GYC: Growth
inhibition of estrogen receptor positive human breast cancer cells
by Taheebo from the inner bark of Tabebuia avellandae tree. Int J
Mol Med. 24:253–260. 2009.PubMed/NCBI
|
|
11
|
Li G, Sepkovic DW, Bradlow HL, Telang NT
and Wong GYC: Lycium barbarum inhibits growth of estrogen receptor
positive human breast cancer cells by favorably altering estradiol
metabolism. Nutr Cancer. 61:408–414. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Telang NT, Li G, Sepkovic DW, Bradlow HL
and Wong GYC: Anti-proliferative effects of Chinese herb Cornus
officinalis in a cell culture model for estrogen receptor positive
clinical breast cancer. Mol Med Rep. 5:22–28. 2012.PubMed/NCBI
|
|
13
|
Telang N, Li G, Sepkovic D, Bradlow HL and
Wong GYC: Comparative efficacy of extracts form Lycium barbarum
bark and fruit on estrogen receptor positive human mammary
carcinoma MCF-7 cells. Nutr Cancer. 66:278–284. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Telang N, Li G, Katdare M, Sepkovic D,
Bradlow L and Wong GYC: Inhibitory effects of Chinese nutritional
herbs in isogenic breast carcinoma cells with modulated estrogen
receptor function. Oncol Lett. 12:3949–3957. 2016.PubMed/NCBI
|
|
15
|
Telang NT, Li G, Katdare M, Sepkovic DW,
Bradlow HL and Wong GYC: The nutritional herb Epimedium
grandiflorum inhibits the growth in a model for the Luminal A
molecular subtype of breast cancer. Oncol Lett. 13:2477–2482.
2017.PubMed/NCBI
|
|
16
|
Katdare M, Osborne MP and Telang NT: Novel
cell culture models for prevention of human breast cancer. Int J
Oncol. 22:505–519. 2003.(Review).
|
|
17
|
Katdare M, Osborne MP and Telang NT: Soy
isoflavone genestein modulates cell cycle progression and induces
apoptosis in HER-2/neu oncogene expressing human breast epithelial
cells. Int J Oncol. 21:809–816. 2002.PubMed/NCBI
|
|
18
|
Telang N and Katdare M: Epithelial cell
culture models for prevention and therapy of clinical breast cancer
(Review). Oncol Lett. 3:744–750. 2012.PubMed/NCBI
|
|
19
|
Telang NT, Nair HB and Wong GYC: Efficacy
of Tabebuia avellandae extract on a cell culture model for triple
negative breast cancer. Cancer Res. 74:(Suppl.): SABCS Abstract no.
P5-14-02. 2014.
|
|
20
|
Telang NT, Nair HB and Wong GYC: Effect of
Cornus officinalis (CO) on a model for triple negative breast
cancer. Cancer Res. 75:(Suppl.): SABCS Abstract no. P3-09-04.
2015.
|
|
21
|
Telang N, Nair HB and Wong GYC: Efficacy
of Dipsacus asperoides (DA) in a model for triple negative breast
cancer. Cancer Res. 76:(Suppl.): SABCS Abstract no. P4-13-04.
2016.
|
|
22
|
Stampfer MR and Bartley JC: Induction of
transformation and continuous cell lines from normal human mammary
epithelial cells after exposure to Benzo (α) pyrene. Proc Natl Acad
Sci USA. 82:2394–2398. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Neve RM, Chin K, Fridlyand J, Yeh J,
Baehner FL, Fevr T, Clark L, Bayani N, Coppe JP, Tong F and Speed
T: A collection of breast cancer cell lines for the study of
functionally distinct cancer subtypes. Cancer Cell. 10:515–527.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Subik K, Lee JF, Baxter L, Strzepek T,
Costello D, Crowley P, Xing L, Hung MC, Bonfiglio T, Hicks DG and
Tang P: Expression patterns of ER, PR, HER-2, CK5/6, Ki67 and AR by
immuno-histochemical analysis in breast cancer cell lines. Breast
Cancer. 4:35–41. 2010.PubMed/NCBI
|
|
25
|
Hudis CA and Gianni L: Triple negative
breast cancer: An unmet medical need. Oncologist. 16:1–11. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lin NU, Vanderplas A, Hughes ME, Theriault
RL, Edge SB, Wong YN, Blayney DW, Niland JC, Winer EP and Weeks JC:
Clinicopathological features, patterns of recurrence and survival
amongst women with triple negative breast cancer in National
Comprehensive Cancer Network. Cancer. 118:5463–5472. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gorsky DH: Integrative oncology: Really
the best of both worlds? Nat Rev Cancer. 14:692–700. 2014.
|
|
28
|
Huang MT, Ho CT, Wang ZY, Ferraro T, Lou
YR, Stauber K, Ma W, Georgiadis C, Laskin JD and Conney AH:
Inhibition of skin tumorigenesis by rosemary and its constituents
carnosol and ursolic acid. Cancer Res. 54:701–708. 1994.PubMed/NCBI
|
|
29
|
Subbaramaiah K, Chung WJ, Michaluart P,
Telang N, Tanabe T, Inoue H, Jang M, Pezzuto JM and Dannenberg AD:
Resveratrol inhibits Cyclo-oxygenase transcription and activity in
phorbol ester treated human mammary epithelial cells. J Biol Chem.
273:21875–21882. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Subbaramaiah K, Michaluart P, Sporn MB and
Dannenberg AJ: Ursolic acid inhibits cyclo-oxygenase-2
transcription in human mammary epithelial cells. Cancer Res.
60:2399–2404. 2000.PubMed/NCBI
|
|
31
|
Subbaramaiah K, Cole PA and Dannenberg AJ:
Retinoids and carnasol suppress cyclo-oxygenase-2 transcription by
CREB binding protein/p300-dependent and independent mechanisms.
Cancer Res. 62:2522–2530. 2002.PubMed/NCBI
|
|
32
|
Cox LA, Chen G and Lee EY: Tumor
suppressor genes and their role in breast cancer. Breast Cancer Res
Treat. 32:19–38. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Burkhart DL and Sage J: Cellular
mechanisms of tumor suppression by the retinoblastoma gene. Nat Rev
Cancer. 8:671–682. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bosco EE and Knudson ES: RB in breast
cancer: At the crossroads of tumorigenesis and treatment. Cell
Cycle. 6:667–671. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Van Arsdale T, Boschoff C, Arndt KT and
Abraham RT: Molecular pathways: Targeting the Cyclin D-CDK 4/6 axis
for cancer treatment. Clin Cancer Res. 21:2905–2910. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Muller PAJ and Vousden KH: Mutant p53 in
cancer: New functions and therapeutic opportunities. Cancer Cell.
25:304–317. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ye L, Jia Y, Ji KE, Sanders AJ, Xue K, Ji
J, Mason MD and Jiang WG: Traditional Chinese medicine in the
prevention and treatment of breast cancer and cancer metastasis.
Oncol Lett. 10:1240–1250. 2015.PubMed/NCBI
|
|
38
|
Stingl J and Caldas C: Molecular
heterogeneity of breast carcinoma and the cancer stem cell
hypothesis. Nat Rev Cancer. 7:791–799. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lobo NA, Shimono Y, Quan D and Clarke MF:
The biology of cancer stem cells. Annu Rev Cell Dev Biol.
23:675–699. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Patel SA, Ndabahaliye A, Lim PK, Milton R
and Rameshwar P: Challenges in the development of future treatments
for breast cancer stem cells. Breast Cancer. 2:1–11.
2010.PubMed/NCBI
|
|
41
|
Telang N: Putative cancer initiating stem
cells in cell culture models for molecular subtypes of clinical
breast cancer. Oncol Lett. 10:3840–3846. 2015.PubMed/NCBI
|
|
42
|
Telang N: Anti-inflammatory drug
resistance selects putative cancer stem cells in a cellular model
for genetically predisposed colon cancer. Oncol Lett (In
press).
|
|
43
|
Zhang F, Song C, Ma Y, Tang L, Xu Y and
Wang H: Effect of fibroblasts on breast cancer cell mammosphere
formation and regulation of stem cell related gene expression. Int
J Mol Med. 28:365–371. 2011.PubMed/NCBI
|
|
44
|
Takahashi K, Tanabe K, Ohnuki M, Narita M,
Ichisaka T, Tomoda K and Yamanaka S: Induction of pluripotent stem
cells from adult human fibroblasts by defined factors. Cell.
131:861–872. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Park IH, Zhao R, West JA, Yabuuci A, Huo
H, Ince TA, Lerou PH, Lansch MW and Daley GQ: Reprograming of human
somatic cells to pluripotency with defined factors. Nature.
451:141–146. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yu J, Hu K, Smuga-Otto K, Tian S, Stewart
R, Slukvin II and Thomson JA: Human induced pluripotent stem cells
free of vector and transgene sequences. Science. 324:797–800. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ishida R, Koyanagi-Aoi M, Oshima N, Kakeji
Y and Aoi T: The tissue reconstructing ability of colon CSCs is
enhanced by FK506 and suppressed by GSK3 inhibition. Mol Cancer
Res. July 14–2017.(Epub ahead of print). https://doi.org/10.1158/1541-7786.MCR-17-0071
View Article : Google Scholar
|