Introduction
Enterohemorrhagic Escherichia coli (EHEC) is
one of the most common pathogenic intestinal bacteria worldwide.
EHEC is a food-borne zoonotic pathogen associated with outbreaks
that pose a major public health concern worldwide. Once EHEC is
ingested, it produces and releases Shiga toxin (Stx) (1). Stx is one of the most important
pathogenic factors in EHEC infections (2). Stx binds to globotriaosylceramide (Gb3),
which is a Stx receptor expressed in the intestinal epithelium and
on the surface of endothelial cells (2). After Stx binds to Gb3, it inhibits
protein synthesis and induces cell apoptosis (1). Gb3 is also expressed on vascular
endothelial cells and nerve cells. Once Stx enters the bloodstream,
it may lead to kidney and brain injury (3,4). Stx
comprises Stx1 and Stx2(1). Stx1 has
the same structure as the Shiga toxin produced by Shigella
dysenteriae (1), whereas Stx2 has
a different structure (5), and it has
been reported that Stx2 is associated with the severity of EHEC
infection (5). EHEC colonizes the
colon and causes diarrhea, hemorrhagic colitis and hemolytic uremic
syndrome (HUS) or encephalopathy in humans (6,7). EHEC has
several serotypes (8), and EHEC
O157:H7 is the strain with the highest rate of isolation (1). In 1982, EHEC O157:H7 was isolated and
identified in America as a food-borne pathogen (1). It was the first identification of a
food-borne pathogen causing worldwide colitis outbreaks (9). In 1996, a big outbreak of EHEC O157:H7
infection occurred, starting with a school lunch in Japan (10). Therefore, EHEC O157:H7 has been
recognized as one of the most serious food-borne pathogens.
In a previous study, it was reported that the
susceptibility to EHEC infection varies among different
individuals, with infants, children and the elderly being highly
susceptible (11). In particular,
patients younger than 5 years are at high risk for the development
of severe symptoms, such as HUS (11).
Cattle are major carriers of EHEC; however, EHEC
colonization in adult ruminants is asymptomatic (1). While EHEC colonizes the colon of humans
and forms pathological lesions, it may colonize the recto-anal
junction of cattle without Stx-related manifestations (1). The differential susceptibility to Stx
and selectivity in colonization sites are associated with host
tolerance to EHEC. Cattle transmit EHEC to humans by shedding the
pathogen in the feces. Fecal shedding leads to contamination of
farm environments by EHEC (12). In a
recent study, Wang et al investigated the role of the
microbiome in EHEC shedding, and indicated that shedding is
affected by the composition of the microbiome (12). In particular, it was demonstrated that
Firmicutes, Bacteroidetes and Proteobacteria promote EHEC shedding.
These phyla also represent the predominant microorganisms in the
human and mouse gut microbiome (13).
Therefore, it was suggested that these strains may play an
important role in EHEC infection in humans and mice.
Intestinal microbiota play an important role in
protecting hosts from enteric infections. It has been reported that
gastrointestinal microbiota act protectively against enteric
infections (14-16).
Furthermore, the susceptibility to EHEC infections is affected by
the composition of the intestinal microbiome in mice (17). Several studies have investigated the
association between specific bacterial strains and EHEC infection
(18-23),
focusing on probiotic strains. Probiotics are live organisms that,
when ingested in adequate amounts, confer a health benefit on the
host (24). By protecting the host
from pathogen colonization (23) and
modulating host immune response (25), probiotic bacteria can contribute to
the defense against and recovery from pathogenic infections. In
particular, Bifidobacterium and Lactobacillus strains
are the predominant and subdominant groups of gastrointestinal
microbiota, respectively (26). These
strains are the most widely used probiotic bacteria and are
included in a number of functional foods and dietary supplements
(26-28).
Bifidobacterium and Lactobacillus are highly relevant
for the prevention of tissue invasion by enteropathogens (29).
It was recently reported that the ratio of
Bacteroides in intestinal microbiota gradually increases
with aging (30). Bacteroides
is one of the most predominant microbial genera within the
gastrointestinal tract (31).
Furthermore, Bacteroides exerts negative effects on their
hosts (31,32). It is generally considered that
Bacteroides may promote infections and cause inflammatory
diarrhea and ulcerative colitis, among others (33-35).
However, to the best of our knowledge, the association between
Bacteroides and EHEC infection has not yet been
reported.
The aim of the present study was to examine the
association between Bacteroides and EHEC infections. Two
Bacteroides strains were used, namely B. fragilis and
B. vulgatus. These strains generally promote infections
(33-35).
However, a recent study demonstrated that B. fragilis can
modulate the host immune system (36), exerting not only negative but also
positive effects on the host. Therefore, to elucidate the role of
Bacteroides in intestinal microbiota, the association
between Bacteroides and EHEC infection was investigated.
Materials and methods
Bacterial strains, media and
cultures
EHEC O157:H7 EDL931k was obtained from the EDL931
strain (37). B. fragilis
RIMD0230001 and Bacteroides vulgatus JCM5826 were the
strains of Bacteroides used in the present study (36,38). EHEC
and Bacteroides were propagated in 10 ml of brain heart
infusion (BHI) medium (Difco Laboratories, Detroit, MI, USA) and
Gifu Anaerobic Medium (GAM) broth (Nissui Pharmaceutical Co.,
Tokyo, Japan), respectively. All bacteria were incubated
anaerobically in Anaero-Pack systems (Mitsubishi Gas Chemical,
Tokyo, Japan) at 37˚C for 24 h. The BHI and GAM media were
sterilized at 121˚C for 15 min and 115˚C for 15 min,
respectively.
Animals
Male germ-free (GF) mice (IQI/Jic, 5 weeks old) were
obtained from Japan Clea Co. Ltd (Tokyo, Japan). Each group of mice
was housed in a cage with a BBH box isolator on a 12:12 light:dark
cycle at 24±2˚C under aseptic conditions. The mice were provided
autoclaved diet and water ad libitum.
Cell culture
Enterocyte-like HT29 cells (39) were used for analysis with the MUSE
Cell Analyzer (Merck KGaA, Darmstadt, Germany). HT29 cells were
obtained from American Type Culture Collection (Manassas, VA, USA).
Cells were routinely grown in Dulbecco's modified Eagle's minimal
essential medium (DMEM) (Nacalai Tesque, Inc., Kyoto, Japan)
supplemented with 10% sterilized fetal bovine serum (Valley
Biomedical, Inc., Winchester, VA, USA) and 1%
antibiotic/antimycotic mixed stock solution (Nacalai Tesque, Inc.).
HT29 cells were incubated in 5% CO2 at 37˚C. Cell
treatment was performed as previously described (40).
Inoculation and EHEC infection
The EHEC infection protocols were based on the
methods described by Isogai et al (41). The mice were divided into 6 groups as
follows: B. fragilis pre-colonized group (with or without
EHEC inoculation), B. vulgatus pre-colonized group (with or
without EHEC inoculation), EHEC mono-colonized group and
medium-only-inoculated mice. The EHEC mono-colonized group and
medium-only-inoculated mice were used at the same time by Koyanagi
et al (unpublished data).
The strains of Bacteroides were incubated
overnight at 37˚C under anaerobic conditions and suspended at a
concentration of 108 colony-forming units (CFU)/ml in
sterile Dulbecco's phosphate-buffered saline (D-PBS) (Nissui
Pharmaceutical). The suspension of Bacteroides strains (100
µl/mouse) was inoculated orally through a soft polyethylene
catheter that was immediately removed. After 24 h of
Bacteroides strain inoculation, 100 µl of the EHEC
suspension (1.0x107 CFU/ml) or sterile BHI medium were
inoculated in each mouse using the same method. Seven days after
EHEC inoculation, the mice were sacrificed by cervical
dislocation.
Histopathological analysis
The mouse kidneys and intestines were fixed
overnight in 10% formaldehyde at ~25˚C and the tissues were
embedded in paraffin and stained with hematoxylin and eosin.
Confirmation of EHEC translocation to
organs
Seven days after EHEC inoculation, the mice were
dissected and the lungs, liver, spleen, brain and heart were
removed. The sections of these organs were stamped on CHROMagar™
O157 for the detection of EHEC O157:H7 (CHROMagar Microbiology,
Paris, France). After incubation for 48 h at 37˚C under aerobic
conditions, colony formation was examined.
EHEC count and Stx detection in mouse
fecal samples
At 1, 3 and 7 days after the inoculation of EHEC,
feces were collected from mice in different groups. Fecal samples
were suspended in BHI broth at a 1:19 (w/v) ratio. To quantify the
number of colonized EHEC, fecal suspensions were serially diluted
and plated on CHROMagar™ O157 for detection of EHEC O157:H7. After
48 h of anaerobic incubation at 37˚C, the CFU/ml of EHEC O157:H7
was determined. Stx1 and Stx2 titers were qualified using a
verotoxin detection kit based on reserved passive latex
agglutination (Denka Seikan Co., Ltd., Tokyo, Japan). The fecal
suspensions were centrifuged at 900 x g for 10 min at room
temperature, and the supernatant was used for Stx1 and Stx2
detection. The number of EHEC and the levels of Stx1 and Stx2 we
defined as low, medium and high. The ranges are defined and
provided in Table I.
 | Table IDefinition of low, medium and high
level of EHEC CFU, and Stx1 and Stx2. |
Table I
Definition of low, medium and high
level of EHEC CFU, and Stx1 and Stx2.
| Level | Number of EHEC
(log10 CFU/ml) | Stx1 and Stx2 |
|---|
| High | ≥9.0 | ≥30.0 |
| Medium | 7.0-8.9 | 10.0-39.9 |
| Low | ≤6.9 | ≤9.9 |
Suppression of apoptosis caused by Stx
using Annexin V and 7-AAD combination assays
Muse Annexin V and Dead Cell kit (Merck KGaA) was
used for the detection of apoptosis in this experiment. This kit
has been used previously for sensitive detection of apoptosis
(42,43). HT29 cells were seeded at a density of
1.0x105 cells/well in a 12-well plate and incubated at
37˚C and 5% CO2 until reaching confluence. The DMEM was
replaced with 900 µl fresh medium without antibiotic/antimycotic
mixed stock solution 30 min prior to bacterial inoculation. Culture
solutions of Bacteroides strains incubated in GAM broth
overnight were adjusted to 1.5x108 CFU/ml and
resuspended in PBS. Following incubation for 30 min in DMEM without
antibiotic/antimycotic mixed stock solution, 1 ml
Bacteroides suspension was inoculated into the cells.
Similarly, culture solutions of EHEC incubated in BHI broth
overnight were adjusted to 1.5x108 CFU/ml and
resuspended in PBS. After 1 h of incubation, 100 µl EHEC suspension
was inoculated into the cells. After 9 h, the culture supernatants
were collected for Stx detection, as described above. Subsequently,
the cells were washed 3 times with 1 ml PBS, treated with trypsin
and transferred into microtubes. The cells were centrifuged at 800
x g for 5 min and resuspended in 100 µl fresh DMEM. A total of 100
µl Annexin V and Dead Cell Dye assay reagent (Merck KGaA) were
added to the samples and mixed. After incubation for 20 min at room
temperature in the dark, the samples were applied to the Muse Cell
Analyzer (Merck KGaA).
Statistical analysis
Significant differences in lethality and EHEC
translocation were calculated using the Steel's test. Furthermore,
the statistical differences in EHEC viable counts, Stx levels in
fecal samples and apoptotic cells in the co-culture of
Bacteroides and EHEC were determined by Dunnett's test or
the Tukey-Kramer test. Significant differences were defined as
probability values of <0.05. Experiments in vitro were
performed in triplicates or more.
Results
Prevention of EHEC infection-related
lethality by Bacteroides colonization
The effect of intestinal Bacteroides strains
against EHEC infection was examined using GF mice. Colonization
with B. fragilis was found to significantly decrease the
lethality of EHEC infection (P<0.05; Table II). In the B. fragilis
pre-colonized group, all mice survived until day 7, whereas in the
B. vulgatus pre-colonized group, 25% of the mice died within
the first 5 days while the rest survived until day 7. However, all
the mice in the EHEC-mono-colonized group had died by day 5. All
the mice of the EHEC-mono-colonized and B. vulgatus
pre-colonized groups exhibited intestinal edema and hemorrhagic
lesions (Table II).
 | Table IIEffects of bacterial colonization on
mouse lethality 7 days after EHEC O157:H7 infection. |
Table II
Effects of bacterial colonization on
mouse lethality 7 days after EHEC O157:H7 infection.
| | | | No. of mice |
|---|
| Groups | EHEC
inoculation | Total no. of
mice | Dead | Exhibiting
intestinal edema and hemorrhagic lesions |
|---|
| B. fragilis
pre-colonized group | + | 5 | 0a | 0a |
| | - | 5 | 0 | 0 |
| B. vulgatus
pre-colonized group | + | 4 | 1 | 4 |
| | - | 4 | 0 | 0 |
| EHEC mono-colonized
group | + | 4 | 4 | 4 |
|
Medium-only-inoculated mice | - | 3 | 0 | 0 |
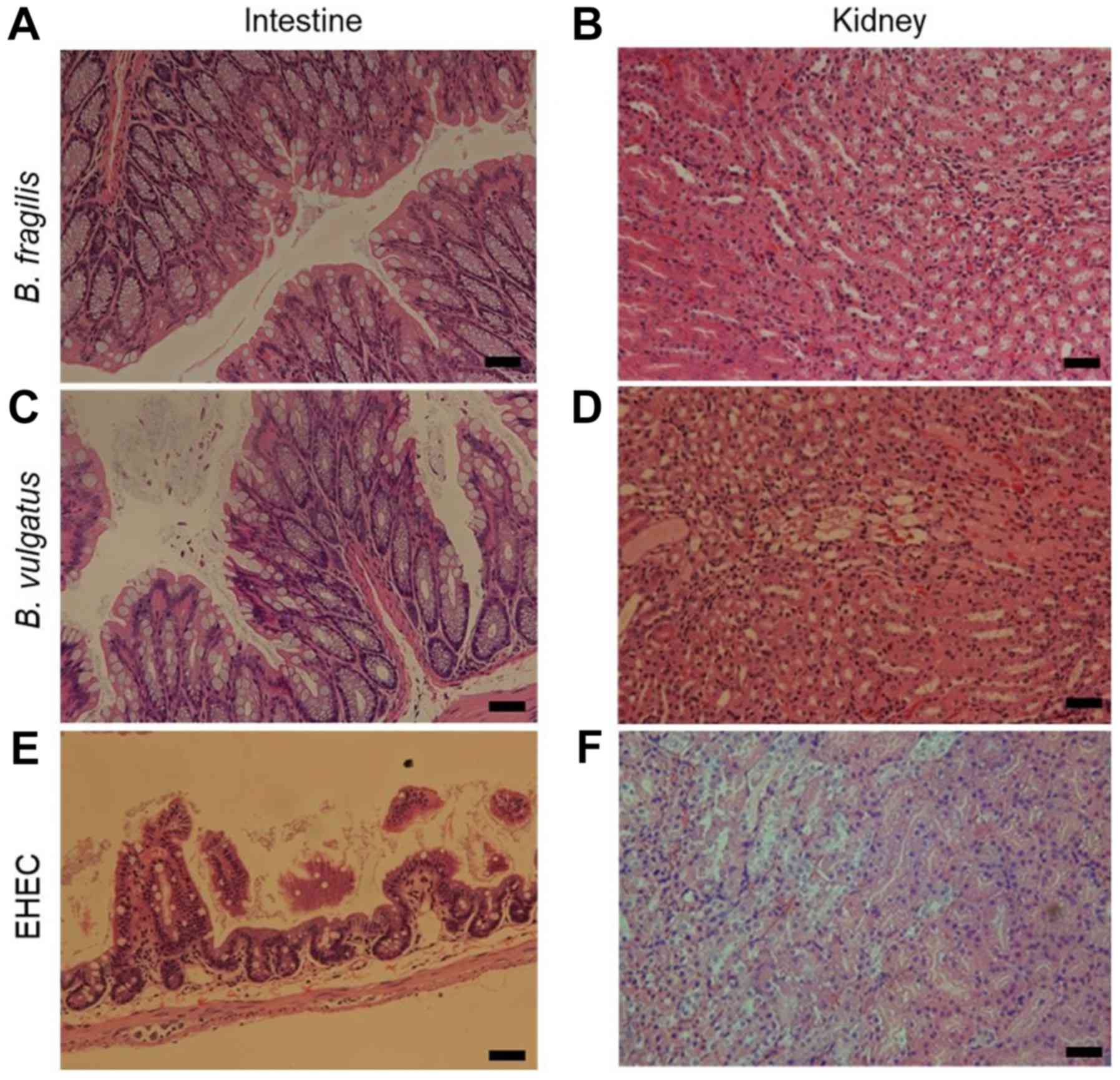
Suppressive effects of colonization by
Bacteroides strains on the histopathological changes in the
intestine and kidney
As determined by histological analysis, B.
fragilis protected the host from the development of
histopathological lesions and almost fully suppressed the
inflammatory symptoms caused by EHEC inoculation (Fig. 1A and B).
B. vulgatus also protected the host from death following
EHEC inoculation (Table II);
however, neutrophil migration was observed in the intestine and
cytopathic changes were observed in the kidneys (Fig. 1C and D).
In the EHEC mono-colonized group, shedding of epithelial cells was
observed in the intestine, and necrosis of renal tubules was
observed in the kidney (Fig. 1E and
F).
Suppression of EHEC translocation to
other organs by Bacteroides colonization
In the B. fragilis pre-colonized group, no
translocation of EHEC was observed (Table III). However, in the B.
vulgatus pre-colonized and EHEC-mono-colonized groups, EHEC
translocation to other organs, such as the heart, liver, spleen and
kidney, was observed. When comparing the translocation rate between
B. vulgatus and the EHEC group, translocation in the EHEC
mono-colonized group was higher compared with that in the B.
vulgatus pre-colonized group, but the difference between the
two groups was not statistically significant (P=0.13).
 | Table IIIEffects of bacterial colonization on
EHEC translocation to organs. |
Table III
Effects of bacterial colonization on
EHEC translocation to organs.
| | | | No. of mice
detected with EHEC in each organ |
|---|
| Groups | EHEC
inoculation | Total no. of
mice | Heart | Liver | Spleen | Kidney |
|---|
| B.
fragilis-colonized group | + | 5 | 0 | 0 | 0 | 0 |
| | - | 5 | 0 | 0 | 0 | 0 |
| B.
vulgatus-colonized group | + | 4 | 1 | 2 | 3 | 1 |
| | - | 4 | 0 | 0 | 0 | 0 |
| EHEC-infected GF
mice | + | 4 | 2 | 3 | 3 | 3 |
|
Medium-only-inoculated mice | - | 3 | 0 | 0 | 0 | 0 |
Comparison of the effects of
Bacteroides colonization on viable counts of EHEC O157:H7
On day 1, the EHEC viable count in the B.
fragilis pre-colonized group was lower compared with that in
the EHEC mono-inoculated group (P=0.0538), although the difference
was not significant (Table IV).
However, the EHEC count gradually increased from day 3 to day 7. In
the B. vulgatus pre-colonized group, no significant
differences were observed among the different time points.
Furthermore, the EHEC count in the EHEC-mono-colonized group was
not examined on day 7, as all the mice had died by day 5 following
EHEC inoculation.
 | Table IVExcretion levels of EHEC, Stx1 and
Stx2 in the feces. |
Table IV
Excretion levels of EHEC, Stx1 and
Stx2 in the feces.
| | | | EHEC colonization
level | Stx level in the
feces |
|---|
| | | | | Stx 1 | Stx 2 |
|---|
| Groups | EHEC
inoculation | Total no. of
mice | Day1a | Day 3 | Day 7 | Day 3 | Day 7 |
|---|
| B.
fragilis-colonized group | + | 5 | L | Mb | L | Mb | L |
| | - | 5 | ND | ND | ND | ND | ND |
| B.
vulgatus-colonized group | + | 4 | M | Mb | M | Hb | M |
| | - | 4 | ND | ND | ND | ND | ND |
| EHEC-colonized
group | + | 4 | H | Hc | NT | Hc | NT |
|
Medium-only-inoculated group | - | 3 | ND | ND | ND | ND | ND |
Inhibitory effects of colonization by
Bacteroides strains on Stx1 and Stx2 levels in fecal samples
In the B. fragilis pre-colonized group, Stx1
and Stx2 levels were significantly lower compared with those in the
EHEC mono-colonized group on day 3 (Table IV). Furthermore, in the B.
vulgatus pre-colonized group, the Stx1 level was significantly
lower compared with that in the EHEC group. By contrast, no
significant differences were observed in Stx2 levels between the
B. vulgatus pre-colonized and the EHEC-mono-colonized groups
on day 3. EHEC mono-colonized mice exhibited >10-fold higher
Stx2 levels compared with mice colonized with Bacteroides.
The Stx levels in the EHEC mono-colonized group were not tested on
day 7, as all the mice had died by day 5 following EHEC
inoculation.
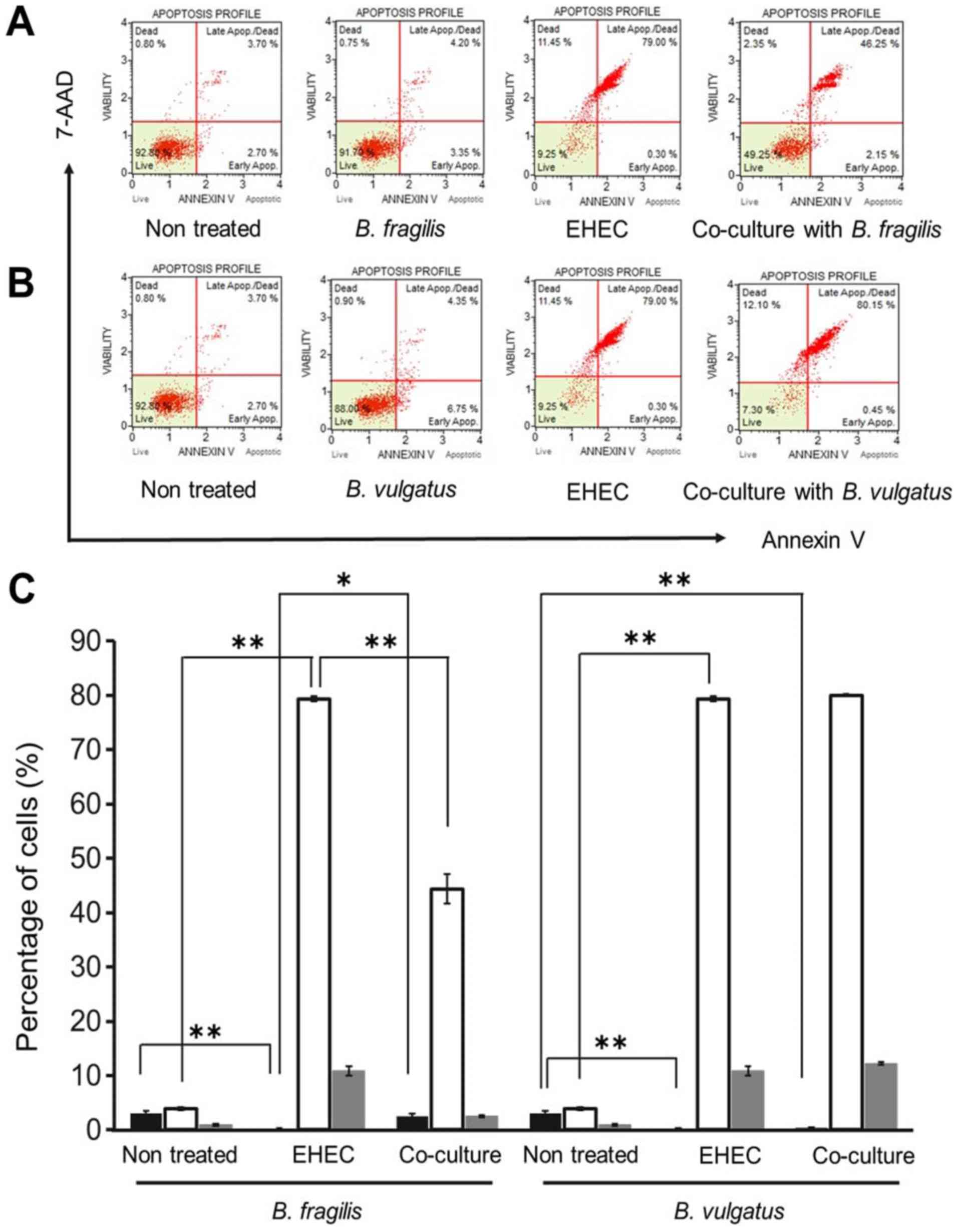
Detection of apoptosis of HT29 cells
co-cultured with Bacteroides strains and EHEC
The apoptosis of epithelial cells was detected to
investigate the factors mediating the protective effects of
Bacteroides strains in vitro. EHEC O157:H7 is
generally known to promote apoptosis of intestinal epithelial cells
(1,44). However, in this experiment, in the
B. fragilis-colonized group, no tissue lesions were observed
in the small intestine (Fig. 1A),
suggesting that B. fragilis exerted inhibitory effects on
the apoptosis of epithelial cells. Therefore, the inhibitory effect
of apoptosis was further examined in the B. fragilis
strain.
In the B. fragilis and B. vulgatus
mono-colonized groups, the majority of cells were non-apoptotic
(Fig. 2A and B). However, in the EHEC-mono-colonized
group, most cells were apoptotic or necrotic. Mono-colonization by
EHEC was significantly increased during early apoptosis (Fig. 2C; P<0.01). Interestingly,
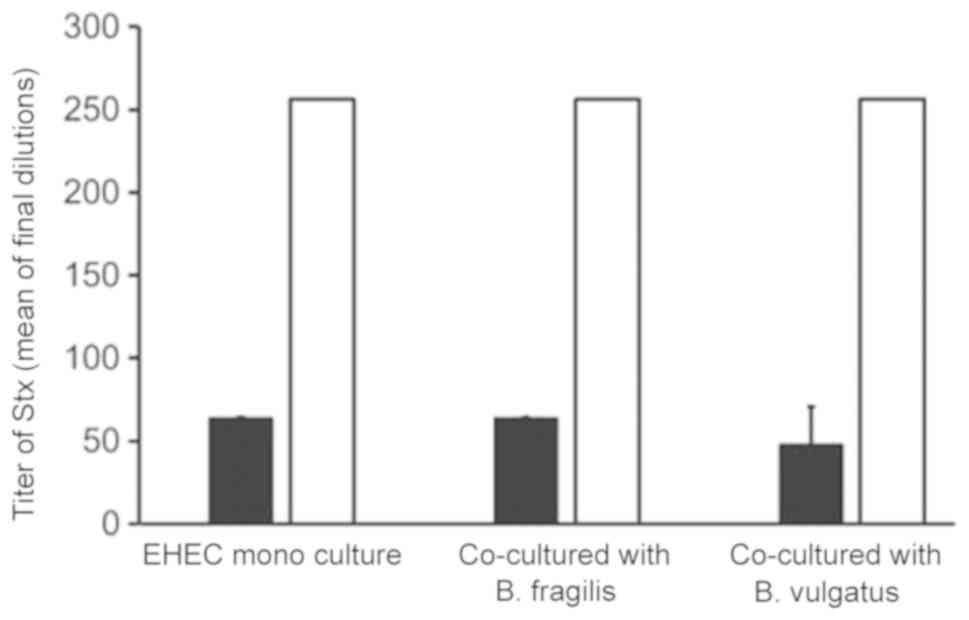
co-culture with B. fragilis and EHEC significantly decreased
the apoptotic cell percentage (P<0.01). However, co-culture with
B. vulgatus and EHEC did not significantly affect apoptosis.
Furthermore, Stx1 and Stx2 production by EHEC was not significantly
suppressed in cells co-cultured with B. fragilis or B.
vulgatus (Fig. 3).
Discussion
It has been reported that B. fragilis
contributes to diarrheal disease in animals and humans (31), and that B. vulgatus is
pathogenic in individuals with underlying conditions, such as
patients with ulcerative colitis (45). In the present study, we demonstrated
the protective effects of Bacteroides against EHEC
infection. The findings of the study revealed that intestinal flora
are implicated in the susceptibility to EHEC infection. In fact, GF
mice inoculated with EHEC displayed severe symptoms and high
lethality (Fig. 1, Table I). By contrast, colonization by a
single Bacteroides strain exerted a protective effect. B.
fragilis suppressed lethality from EHEC infection. Similarly,
B. vulgatus suppressed EHEC lethality, albeit to a lesser
extent. Furthermore, the EHEC count in the intestines of mice
colonized by B. fragilis or B. vulgatus was reduced,
although the difference was not significant (Table IV). Moreover, Stx production in the
mouse intestine was significantly suppressed in the B.
fragilis-colonized group (Table
IV). These results demonstrated that B. fragilis and
B. vulgatus effectively decreased the lethality of EHEC
infection (Table II), particularly
in the B. fragilis pre-colonized group (P<0.05). In the
present study, the mechanisms by which each bacterium protected
mice from EHEC infection were not fully elucidated. However, to the
best of our knowledge, this study is the first to demonstrate that
Bacteroides strains may act protectively against lethal EHEC
infection in mice.
Our study suggested that the EHEC count in the early
stages of EHEC infection is a key factor affecting the severity of
the infection. Frankel et al reported that the locus of
enterocyte effacement type III secretion system of EHEC is crucial
for bacterial adhesion to the host's intestinal cells during the
early stages of infection (46).
Adhesion to the epithelial cells enables disease establishment
(47). The results of our study
demonstrated that B. fragilis lowered the EHEC count in
vivo (P=0.0538; Table IV). In
addition, B. fragilis fully protected the host from EHEC
infection and suppressed the formation of pathological lesions
(Fig. 1A and B; Table II).
However, B. vulgatus did not lower the EHEC count in the
early stages of infection (Table IV)
and did not completely suppress the development of symptoms
(Table II). Therefore, the type of
Bacteroides colonization and the early stages of the EHEC
infection are key factors in determining disease severity.
The present study also demonstrated that
translocation may be another factor associated with the severity of
EHEC infection. Generally, EHEC is taken up orally and colonizes
the intestinal tract (1). Considering
the route of EHEC translocation, if the barrier of the intestinal
tract wall is compromised, Stx can circulate in the entire body.
Fukuda et al reported that Stx translocation is associated
with EHEC infection lethality (23).
In the present study, the B. fragilis-colonized group did
not exhibit EHEC translocation to the other organs examined
(Table III), and there were no
pathological lesions identified (Fig.
1). However, in the B. vulgatus pre-colonized and
EHEC-mono-colonized groups, EHEC translocation was observed in all
the organs examined (Table III). In
addition, the EHEC-mono-colonized group displayed the highest ratio
of EHEC translocation in each organ (Table III). Furthermore, Stx levels in the
feces were examined and the B. fragilis pre-colonized group
exhibited the lowest Stx level among all groups (Table IV). Therefore, the findings of the
present study demonstrated that B. fragilis suppressed the
susceptibility to EHEC infection.
Protecting the intestinal tract helps prevent lethal
EHEC infections (16). Stx produced
by EHEC promotes apoptosis of intestinal epithelial cells (23). Inhibition of Stx circulation in the
body is crucial for the prevention of lethal EHEC infection
(16). In the present study, the
inhibitory effect of Bacteroides on epithelial intestinal
cell apoptosis was demonstrated (Fig.
2). In the EHEC-mono-colonized group, the majority of the cells
were apoptotic in vitro (Fig.
2C). However, in the B. fragilis-co-cultured group,
apoptosis of HT29 cells was significantly reduced (P<0.01;
Fig. 2C), whereas apoptosis was not
suppressed in the B. vulgatus-co-culture group (Fig. 2C). Of note, Stx production was not
found to be significantly suppressed following apoptosis analysis
(Fig. 3). The reason apoptosis was
suppressed in HT29 cells remains unclear, and the underlying
mechanisms were not elucidated in the present study. However, B.
fragilis was confirmed to exert an inhibitory effect on
intestinal epithelial cell apoptosis.
In conclusion, the present study demonstrated that
Bacteroides prevented EHEC infection. It was also suggested
that Bacteroides may be associated with susceptibility to
EHEC infection in mice, in addition to cattle. Our findings using
single-flora systems demonstrated that Bacteroides
contributed to the prevention of EHEC infection, and B.
fragilis was shown to fully protect against EHEC infection. The
interaction between EHEC and Bacteroides in GF mice provides
little information regarding their behavior in the microbiome.
However, understanding the role of each intestinal bacterium is
relevant when considering treatment against EHEC infection. Further
studies are required to elucidate the mechanism underlying the
protective role of B. fragilis against EHEC infection.
Acknowledgements
We would like to thank our laboratory staff for
helpful discussions and support.
Funding
The present study was supported by a Grant-in-Aid
for Scientific Research from Yakult Bio-Science Foundation.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Ethics approval and consent to
participate
Each experimental protocol was performed in
accordance with the Regulations for Animal Experiments and Related
Activities at Tohoku University (approval no. 2011AgA-30).
Patient consent for publication
Not applicable.
Authors' contributions
KS, RS, HI and EI performed the experiments; KS, RS,
YK and EI designed the study; KS, YK, HY and EI wrote the
manuscript.
Competing interests
The authors declare that they have no competing
interests to disclose.
References
|
1
|
Nguyen Y and Sperandio V:
Enterohemorrhagic E. coli (EHEC) pathogenesis. Front Cell
Infect Microbiol. 2(90)2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jones NL, Islur A, Haq R, Mascarenhas M,
Karmali MA, Perdue MH, Zanke BW and Sherman PM: Escherichia
coli Shiga toxins induce apoptosis in epithelial cells that is
regulated by the Bcl-2 family. Am J Physiol Gastrointest Liver
Physiol. 278:G811–G819. 2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hughes AK, Stricklett PK, Schmid D, Kohan
DE and Hughes AK: Cytotoxic effect of Shiga toxin-1 on human
glomerular epithelial cells. Kidney Int. 57:2350–2359.
2000.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rutjes NW, Binnington BA, Smith CR,
Maloney MD and Lingwood CA: Differential tissue targeting and
pathogenesis of verotoxins 1 and 2 in the mouse animal model.
Kidney Int. 62:832–845. 2002.PubMed/NCBI View Article : Google Scholar
|
|
5
|
O'Brien AD and Holmes RK: Shiga and
Shiga-like toxins. Microbiol Rev. 51:206–220. 1987.PubMed/NCBI
|
|
6
|
Karmali MA, Steele BT, Petric M and Lim C:
Sporadic cases of haemolytic-uraemic syndrome associated with
faecal cytotoxin and cytotoxin-producing Escherichia coli in
stools. Lancet. 1:619–620. 1983.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yoshimitsu M, Hayashi N, Kaneko Y and
Doyama H: An adult case of combined encephalopathy and hemolytic
uremic syndrome caused by Escherichia coli O157. Nihon
Shokakibyo Gakkai Zasshi. 108:74–79. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gyles CL: Shiga toxin-producing
Escherichia coli: An overview. J Anim Sci. 85
(Suppl):E45–E62. 2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Remis RS, MacDonald KL, Riley LW, Puhr ND,
Wells JG, Davis BR, Blake PA and Cohen ML: Sporadic cases of
hemorrhagic colitis associated with Escherichia coli
O157:H7. Ann Intern Med. 101:624–626. 1984.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fukushima H, Hashizume T, Morita Y, Tanaka
J, Azuma K, Mizumoto Y, Kaneno M, Matsuura M, Konma K and Kitani T:
Clinical experiences in Sakai City Hospital during the massive
outbreak of enterohemorrhagic Escherichia coli O157
infections in Sakai City, 1996. Pediatr Int. 41:213–217.
1999.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Terajima J, Izumiya H, Wada A, Tamura K
and Watanabe H: Shiga toxin-producing Escherichia coli
O157:H7 in Japan. Emerg Infect Dis. 5:301–302. 1999.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wang O, McAllister TA, Plastow G, Stanford
K, Selinger B and Guan LL: Interactions of the Hindgut
Mucosa-Associated Microbiome with Its Host Regulate Shedding of
Escherichia coli O157:H7 by Cattle. Appl Environ Microbiol.
84(pii): e01738–17. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ley RE, Bäckhed F, Turnbaugh P, Lozupone
CA, Knight RD and Gordon JI: Obesity alters gut microbial ecology.
Proc Natl Acad Sci USA. 102:11070–11075. 2005.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Momose Y, Hirayama K and Itoh K: Effect of
organic acids on inhibition of Escherichia coli O157:H7
colonization in gnotobiotic mice associated with infant intestinal
microbiota. Antonie van Leeuwenhoek. 93:141–149. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yoshimura K, Matsui T and Itoh K:
Prevention of Escherichia coli O157:H7 infection in
gnotobiotic mice associated with Bifidobacterium strains.
Antonie van Leeuwenhoek. 97:107–117. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
de Sablet T, Chassard C,
Bernalier-Donadille A, Vareille M, Gobert AP and Martin C: Human
microbiota-secreted factors inhibit shiga toxin synthesis by
enterohemorrhagic Escherichia coli O157:H7. Infect Immun.
77:783–790. 2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Momose Y, Hirayama K and Itoh K:
Antagonism of intestinal bacteria isolated from human infants
against Escherichia coli O157:H7 infection in gnotobiotic
mice. Microb Ecol Health Dis. 17:9–14. 2005. View Article : Google Scholar
|
|
18
|
Asahara T, Shimizu K, Nomoto K, Hamabata
T, Ozawa A and Takeda Y: Probiotic bifidobacteria protect mice from
lethal infection with Shiga toxin-producing Escherichia coli
O157:H7. Infect Immun. 72:2240–2247. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chen YP, Lee TY, Hong WS, Hsieh HH and
Chen MJ: Effects of Lactobacillus kefiranofaciens M1
isolated from kefir grains on enterohemorrhagic Escherichia
coli infection using mouse and intestinal cell models. J Dairy
Sci. 96:7467–7477. 2013.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rund SA, Rohde H, Sonnenborn U and
Oelschlaeger TA: Antagonistic effects of probiotic Escherichia
coli Nissle 1917 on EHEC strains of serotype O104:H4 and
O157:H7. Int J Med Microbiol. 303:1–8. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Eaton KA, Honkala A, Auchtung TA and
Britton RA: Probiotic Lactobacillus reuteri ameliorates
disease due to enterohemorrhagic Escherichia coli in
germfree mice. Infect Immun. 79:185–191. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ogawa M, Shimizu K, Nomoto K, Takahashi M,
Watanuki M, Tanaka R, Tanaka T, Hamabata T, Yamasaki S and Takeda
Y: Protective effect of Lactobacillus casei strain Shirota
on Shiga toxin-producing Escherichia coli O157:H7 infection
in infant rabbits. Infect Immun. 69:1101–1108. 2001.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Fukuda S, Toh H, Hase K, Oshima K,
Nakanishi Y, Yoshimura K, Tobe T, Clarke JM, Topping DL, Suzuki T,
et al: Bifidobacteria can protect from enteropathogenic infection
through production of acetate. Nature. 469:543–547. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Food and Agriculture Organization of
United Nations and World Health Organization Working Group Report:
Guidelines for the evaluation of probiotics in food. FAO/WHO,
London, ON, 2002.
|
|
25
|
Resta-Lenert S and Barrett KE: Live
probiotics protect intestinal epithelial cells from the effects of
infection with enteroinvasive Escherichia coli (EIEC). Gut.
52:988–997. 2003.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Shreiner AB, Kao JY and Young VB: The gut
microbiome in health and in disease. Curr Opin Gastroenterol.
31:69–75. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Macpherson AJ and Harris NL: Interactions
between commensal intestinal bacteria and the immune system. Nat
Rev Immunol. 4:478–485. 2004.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Frick JS, Schenk K, Quitadamo M, Kahl F,
Köberle M, Bohn E, Aepfelbacher M and Autenrieth IB:
Lactobacillus fermentum attenuates the
proinflammatory effect of Yersinia enterocolitica on human
epithelial cells. Inflamm Bowel Dis. 13:83–90. 2007.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kang HJ and Im SH: Probiotics as an Immune
Modulator. J Nutr Sci Vitaminol (Tokyo). 61 (Suppl):S103–S105.
2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Mariat D, Firmesse O, Levenez F, Guimarăes
V, Sokol H, Doré J, Corthier G and Furet JP: The
Firmicutes/Bacteroidetes ratio of the human microbiota changes with
age. BMC Microbiol. 9(123)2009.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Border M, Firehammer BD, Shoop DS and
Myers LL: Isolation of Bacteroides fragilis from the feces
of diarrheic calves and lambs. J Clin Microbiol. 21:472–473.
1985.PubMed/NCBI
|
|
32
|
Kim JM, Lee JY and Kim YJ: Inhibition of
apoptosis in Bacteroides fragilis enterotoxin-stimulated
intestinal epithelial cells through the induction of c-IAP-2. Eur J
Immunol. 38:2190–2199. 2008.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chen LA, Van Meerbeke S, Albesiano E,
Goodwin A, Wu S, Yu H, Carroll K and Sears C: Fecal detection of
enterotoxigenic Bacteroides fragilis. Eur J Clin Microbiol
Infect Dis. 34:1871–1877. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Onderdonk AB, Bronson R and Cisneros R:
Comparison of Bacteroides vulgatus strains in the
enhancement of experimental ulcerative colitis. Infect Immun.
55:835–836. 1987.PubMed/NCBI
|
|
35
|
Rashidan M, Azimirad M, Alebouyeh M,
Ghobakhlou M, Asadzadeh Aghdaei H and Zali MR: Detection of B.
fragilis group and diversity of bft enterotoxin and antibiotic
resistance markers cepA, cfiA and nim among intestinal
Bacteroides fragilis strains in patients with inflammatory
bowel disease. Anaerobe. 50:93–100. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Mazmanian SK, Liu CH, Tzianabos AO and
Kasper DL: An immunomodulatory molecule of symbiotic bacteria
directs maturation of the host immune system. Cell. 122:107–118.
2005.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Riley LW, Remis RS, Helgerson SD, McGee
HB, Wells JG, Davis BR, Hebert RJ, Olcott ES, Johnson LM, Hargrett
NT, et al: Hemorrhagic colitis associated with a rare
Escherichia coli serotype. N Engl J Med. 308:681–685.
1983.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Li J, Mandal G and Rosen BP: Expression of
arsenic resistance genes in the obligate anaerobe Bacteroides
vulgatus ATCC 8482, a gut microbiome bacterium. Anaerobe.
39:117–123. 2016.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Cohen E, Ophir I and Shaul YB: Induced
differentiation in HT29, a human colon adenocarcinoma cell line. J
Cell Sci. 112 (Pt 16):2657–2666. 1999.PubMed/NCBI
|
|
40
|
Kuroda K, Fukuda T, Krstic-Demonacos M,
Demonacos C, Okumura K, Isogai H, Hayashi M, Saito K and Isogai E:
miR-663a regulates growth of colon cancer cells, after
administration of antimicrobial peptides, by targeting CXCR4-p21
pathway. BMC Cancer. 17(33)2017.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Isogai E, Isogai H, Kimura K, Hayashi S,
Kubota T, Fujii N and Takeshi K: Role of tumor necrosis factor
alpha in gnotobiotic mice infected with an Escherichia coli
O157:H7 strain. Infect Immun. 66:197–202. 1998.PubMed/NCBI
|
|
42
|
Koopman G, Reutelingsperger CP, Kuijten
GA, Keehnen RM, Pals ST and van Oers MH: Annexin V for flow
cytometric detection of phosphatidylserine expression on B cells
undergoing apoptosis. Blood. 84:1415–1420. 1994.PubMed/NCBI
|
|
43
|
Zelenin AV, Poletaev AI, Stepanova NG,
Barsky VE, Kolesnikov VA, Nikitin SM, Zhuze AL and Gnutchev NV:
7-Amino-actinomycin D as a specific fluorophore for DNA content
analysis by laser flow cytometry. Cytometry. 5:348–354.
1984.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Eaton KA, Fontaine C, Friedman DI, Conti N
and Alteri CJ: Pathogenesis of colitis in germ-free mice infected
with EHEC O157:H7. Vet Pathol. 54:710–719. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Bamba T, Matsuda H, Endo M and Fujiyama Y:
The pathogenic role of Bacteroides vulgatus in patients with
ulcerative colitis. J Gastroenterol. 30 (Suppl 8):45–47.
1995.PubMed/NCBI
|
|
46
|
Frankel G, Phillips AD, Rosenshine I,
Dougan G, Kaper JB and Knutton S: Enteropathogenic and
enterohaemorrhagic Escherichia coli: More subversive
elements. Mol Microbiol. 30:911–921. 1998.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Pifer R and Sperandio V: The interplay
between the microbiota and enterohemorrhagic Escherichia
coli. Microbiol Spectr. 2:2014.PubMed/NCBI View Article : Google Scholar
|