Introduction
Defects in the canal of Nuck are rare abnormalities
of the female genitalia that are usually detected and repaired in
young girls more frequently during the first 5 years of life
(1). The first noted case defect in
the Canal of Nuck dates back to 1691 by Anton Nuck (2). The failure of the canal to close after
birth or within the first year of life in female infants can lead
to formation of hydrocele or herniation of intraabdominal
structures through the patent Canal of Nuck (1,3). Hydrocele
of the Nuck canal, cyst of the Canal of Nuck or female hydrocele
are equivalent terms for a rare developmental disorder of the
reproductive system of women and accounts for a limited number of
cases of benign painless or painful swelling in the inguinal region
or even to the labia majora (4,5). Hydrocele
of the Canal of Nuck constitutes a particular type of primary
idiopathic hydrocele, the enlargement of which has been attributed
to a defect of the secretory membranes resulting in an imbalance in
secretion and absorption of fluids of the processus vaginalis
(6).
Several reports of cysts of the Canal of Nuck are
presented in literature and describe the symptomatology and
surgical approaches used in their treatment (7-10).
Although a rare pathology of the inguinal canal in female patients,
it should be considered when diagnosing inguinal tumours in female
patients. In the present report, a case of cyst of Nuck in a female
patient, and a review of the current literature with special
consideration on clinical presentation, diagnostic approach and
management are presented.
Case presentation
A 40-year old female presented to our department
with a painful mass in her right inguinal region. The swelling was
first noticed two months ago, and the patient reported she never
suffered from regional pain before. There was no history of local
trauma, symptoms of nausea, vomiting or abdominal discomfort. Her
body mass index was 27 kg/m2. Her medical history was
negative for any pathology and surgical procedures. She had two
uncomplicated vaginal deliveries. At presentation, physical
examination revealed a small palpable mobile lump in the right
groin without overlying skin erythema or tenderness. Valsalva
maneuver did not make the mass more prominent. There was an absence
of incarceration or strangulation. Her abdomen was soft,
non-distended and non-tender with no signs of bowel occlusion.
Laboratory tests showed measured parameters were within the normal
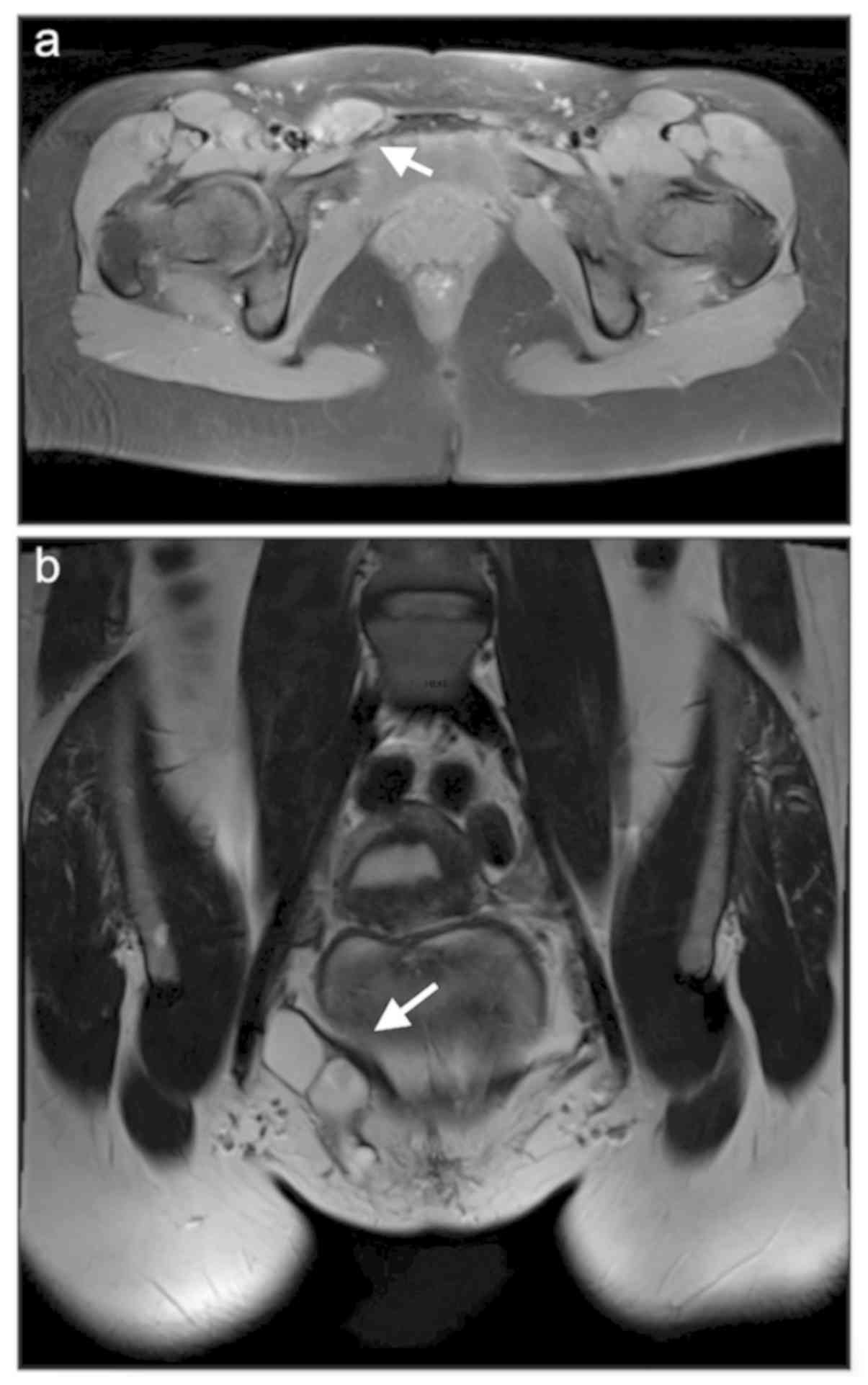
range. Magnetic resonance imaging (MRI) revealed a 3.5 cm
well-defined, thin-walled cystic structure in her right groin
(Fig. 1). There was no evidence of
bowel loops, omentum or other solid structures within the mass. The
diagnosis of a Nuck cyst was considered and the patient was
operated on. The cyst was dissected from the round ligament and was
completely excised. The defect of the internal inguinal ring was
primarily repaired without the use of a mesh. Histology confirmed
the presence of Nuck cyst. The patient's postoperative course was
uneventful, and she was discharged the next day. One year
postoperatively, the patient remained asymptomatic without any
recurrence. Written informed consent was obtained from the patient
for publication of this case report and any accompanying
images.
Review of the literature
A systematic search of the literature for articles
published between January 2000 and May 2019 was performed using the
Medline (1966-2019), Scopus (2004-2019) and Google Scholar
(2004-2019) databases along with the references in any articles.
For all articles, the full-text was retrieved. Studies regarding
adult women who were diagnosed with Nuck hydrocele were considered
eligible for inclusion. A total of five studies were excluded from
the present review (11-15).
Pandey et al (11) and Safak
et al (12) presented
radiological outcomes of a case with Nuck hydrocele and thus
excluded due to insufficient data. Noguchi et al (13) and Amu et al (14) were not considered eligible due the
fact that the cystic structure in the Nuck canal was histologically
confirmed as ectopic pregnancy and dermoid cyst, respectively, and
not as hydrocele. Finally, Sala et al (15) included a 17-year old patient with Nuck
cyst and was excluded due to age restrictions of the present
study.
A total of 16 case reports of 16 patients with
hydrocele of the Canal of Nuck, were included in the present
systematic review (3-5,7-10,16-24);
whereas 5 studies were excluded. The primary characteristics of the
included studies including the primary symptoms on presentation,
outcomes of clinical examination and imaging, the size of the mass
and the type of procedure performed are presented in Table I. The mean age of patients included
was 35.18±3.27 years and 13 (81.3%) of the patients were of
reproductive age (18-45 years). Two of the included women were
nulliparous; one of them presented with infertility and underwent
simultaneous surgery for an enlarged ovarian cyst. Three women had
one or more children. For the remaining 11 patients, data
concerning parity was not available. A right inguinal mass was
noted in the majority of the patients (n=13, 81.3%) whereas in the
remaining thee patients a left-sided mass was noted. The enrolled
patients were admitted with a groin swelling which was either
painful in 5/16 cases or painless in the remaining 11/16 cases. In
all except one case, preoperative imaging was performed; In six
patients an ultrasound (US) was performed, preoperative computed
tomography (CT) was performed in three cases, one patient underwent
MRI, in one case a CT along with an MRI was performed, in four
cases US and MRI were performed, and in one case US in combination
with CT was performed. In seven cases, imaging suggested the
presence of a cystic structure suggestive of the presence of
hydrocele of the Canal of Nuck. Clinical examination revealed a
reducible lump in the affected inguinal region in six women, and in
eight cases, the mass was irreducible. In two cases, the nature of
the mass was not specified.
 | Table IPublished studies included in the
literature review. |
Table I
Published studies included in the
literature review.
| Author, year
(Ref) | Primary symptom;
physical examination | Imaging modality | Size, cm | Surgical approach,
Lap/Open | Type of repair |
|---|
| Bhattacharjee and
Ghosh, 2006(3) | Left painless
swelling; reducible, soft, cystic, non-tender | U/S: Encysted
echofree lesion in the left inguinal canal. | 7.5x5.0 | Open | Hydrocelectomy and
wound closure |
| Caviezel et
al, 2009(4) | Right painless
swelling; irreducible, increased volume in standing position
reduced by manual compression | U/S and MRI:
Anechogenic cystic mass with. thin wall | 5.0x5.0 | Open | Hydrocelectomy and
round ligament excision |
| Jagdale et al,
2012(16) | Right painful
swelling; irreducible tender, cystic and fluctuant | U/S: Well-defined,
avascular, oval, anechoic cystic swelling within the inguinal
canal. | 4.3x2.6 | Open | Hydrocelectomy and
NMR |
| Ferreira et
al, 2017(17) | Painless vulval
swelling; irreducible soft fluctuant sausage-shaped mass | U/S: Well-defined
hypoechoic elongated mass with 5.5 cm of long axis, septated,
extending from the superficial inguinal canal to labia majora. | 4.0 | Open | Hydrocelectomy and
vulva correction |
| Karapolat et
al, 2018(18) | Right painless
swelling; irreducible mass of medium hardness with smooth surface
and limited mobilization | U/S: Thick-walled
cystic lesion with thin internal septae. MRI: cystic lesion with
lobulated contours T1A hypointense and T2A hyperintense intensities
neighboring. | 2.5x5.0, 3.5x4.7 | Open | Hydrocelectomy and
inguinal ring ligation |
| Matsumoto et
al, 2014(7) | Left painless
swelling; reducible | U/S: Hypoechoic and
homogeneous without solid components. MRI, simple cystic lesion,
which appeared to be in contact with the left ovary connected at
its base with the parietal peritoneum. | 4.5 | Lap (TEP) | Hydrocelectomy and
MR |
| Ozel et al,
2009(19) | Right painless
swelling for 3 months; irreducible fluctuant sausage shaped | U/S: Tubular cystic
structure with thin internal septae not change its shape when
compressed by the transducer with no abnormal vascularity. MRI:
Well defined lobulated tubular mass which was hypoin tense on
T1-weighted images and hyperintense on T2-weighted image | 6.0x4.0x1.5 | Open | Hydrocelectomy |
| Patnam et al,
2016(9) | Painless right
swelling for 3 months; irreducible positive fluctuation. No change
in size on Valsalva maneuver, nor did it expansible cough impulse,
no peristaltic activity and no abnormal vascularity associated with
the swelling | U/S: Elongated,
anechoic fluid collection, not suggest a communication to the
peritoneal cavity. CT: Well-defined, peripherally enhancing thin
walled tubular cystic structure extending from the right iliac
fossa along the course of the round liga ment through the right
inguinal canal to the ipsilateral labia | 6.3x3.4x2.0 | Open | Hydrocelectomy and
wound closure |
| Qureshi and Lakshman,
2014(8) | Left painful swelling
for 1 month; irreducible, oval, tender, cystic and fluctuant
swelling | U/S: Left inguinal
hernia, with well-defined, oval, anechoic cystic swelling within
the inguinal canal | 4.0x3.0 | Lap | Hydrocelectomy and
MR |
| Yen et al,
2001(20) | Right painless mass;
reducible above labia major, reduced in supine position | Not performed | N/A | Lap (IP) | Hydrocelectomy,
inguinal ring ligation and NMR |
| Uzun et al,
2017(10) | Right painful
swelling for 2 days, 4 days following vaginal delivery | CT: Inguinal
hernia, with a suspicion of herniation of the adnexal organs | N/A | Open | Hemorrhagic cyst
and necrotic liga mentum rotundum excision |
| Zawaideh et
al, 2018(5) | Right painful
swelling. | U/S: Oval anechoic
mass | N/A | Open | Hydrocelectomy |
| Kim et al,
2016(21) | Right painless
swelling for 4 months; reducible | CT: Cystic mass in
the inguinal canal. MRI: Cystic mass in the inguinal canal included
thin septa | 7.1x3.8 | Open | Hydrocelectomy and
high inguinal ring ligation |
| Sethi and Patel,
2016(23) | Right painless
swelling for 1 year; reducible fluctuant, and minimally tender
mass, without a bruit or thrill | CT: Oval fluid
collection in the right inguinal region extending to the right
labia majora. | 11.7x4.9x3.6 | Open | Hydrocelectomy |
| Kono et al,
2015(22) | Right painless
swelling for 2 years; palpable mass | MRI: Irregularly
shaped cystic mass lesion and a smaller cystic lesion and fluid
collection evident in the right side of the pelvic cavity. | 4.8x3.7 | Open | Hydrocelectomy
(outside lesion), inguinal ring ligation, MR |
| Ryan et al,
2009(24) | Right painful
swelling for 2 days; irreducible, ecchymosis, tender, firm,
palpated superolateral to the pubic tubercle | U/S: Mass within
the right groin, with both cystic and solid components present with
the suggestion of the possibility of bowel contents. | N/A | Open | Hematoma evacuation
and hydrocelectomy |
All the included patients underwent surgery to
examine the lesion and repair the defect. In 13 patients the
surgical approach was open, and the other three patients underwent
laparoscopy. Two cases underwent excision of the hydrocele and
inguinal ring ligation, and in six cases a simple cystectomy was
performed, which was followed by a vulva correction in one case. In
2 cases the round ligament was excised, with the hydrocele in one
of them due to necrosis and presence of a haemorrhagic cyst. A
hematoma within a Nuck hydrocele was found in one case and
evacuated along with the hydrocelectomy. Hernia repair along with
hydrocelectomy was performed in five cases (three laparoscopic and
two open); among which, in two cases, a herniorrhaphy (no mesh
repair) was performed, whereas three patients underwent a hernia
repair with the use of a mesh. An additional inguinal ring ligation
was performed in two patients; one laparoscopic and one open.
Postoperative recovery was uneventful, and no postoperative deaths
or complications were observed. According to 7 of the included
studies, no recurrence of the lesion was reported in the follow up
period, which ranged from 2-24 months after surgery (3,8,9,16,18,20,22). Data
concerning hospital stay was reported in 4 studies with a range of
20-72 h (7,10,18,20).
Discussion
The Canal of Nuck runs through the inguinal canal
adjacent to the round ligament and is considered the female
analogue of the processus vaginalis in males (25). Normally, the Canal of Nuck is
obliterated within the first year of life. Failure of the Canal to
close during that period in female infants can result in Nuck
hydrocele or herniation of intraabdominal structures through the
patent Canal of Nuck (1). Thus,
failure of closure is typically detected in childhood. Due to its
rarity, accurate information regarding the exact prevalence of
hydrocele during childhood is not available. Akkoyun et al
(26) reported that only 0.76% of
girls <12 years exhibited hydrocele of Nuck among their study
population. A comparable prevalence of Nuck hydrocele (0.74%) was
also reported by Papparella et al (27), who reviewed 353 female patients, aged
1-14 years, with inguinal swelling. Literature regarding Nuck
hydrocele in adulthood are even more scarce. A systematic review
performed in the present study revealed a total of 16 cases of
adult patients who underwent surgery for Nuck cyst.
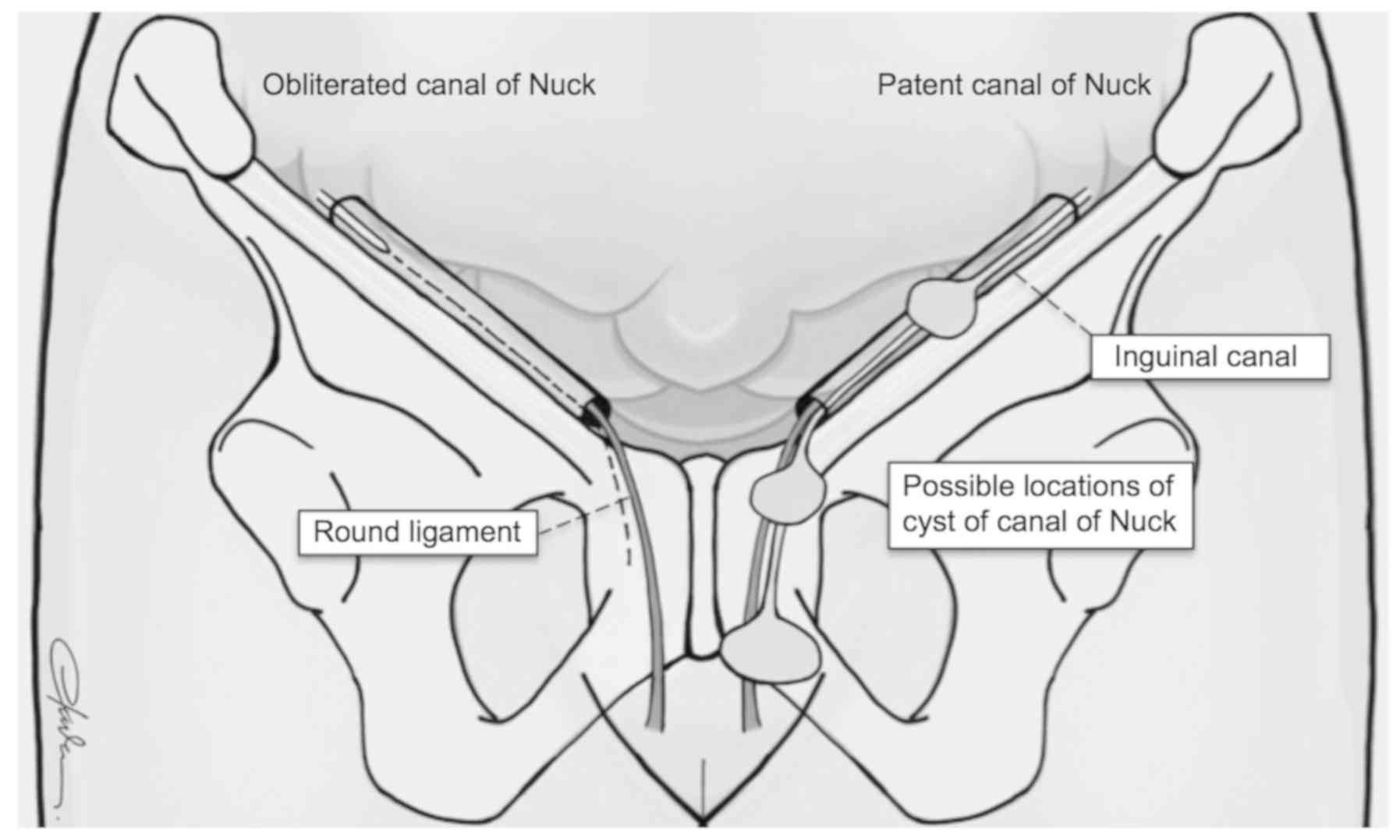
Fig. 2 schematically
presents the anatomy of the inguinal canal with a physiologically
obliterated Canal of Nuck and the potential sites where the cyst
may be recognized when the canal is patent. At clinical
examination, the cyst of the Canal of Nuck is frequently described
as a painless or mildly painful irreducible or reducible mass in
the inguinal region, which typically extends to the labia majora,
and does not expand when performing the Valsalva manoeuvre
(23). In approximately one-third of
patients an associated inguinal hernia is present. Consistent with
this, nearly one-third of the patients included in the present
study underwent a simultaneous hernia repair. Differential
diagnosis includes inguinal hernia, enlarged lymph nodes and soft
tissue tumours such as lipomas, leiomyomas and endometriosis of the
round ligament (28).
A cyst of the Canal of Nuck is frequently
misdiagnosed as inguinal hernia in females and is only correctly
diagnosed intraoperatively. Therefore preoperative imaging is
crucial for facilitating diagnosis and further guiding therapeutic
options. All except one of the included cases included in the
systematic review underwent preoperative imaging with US, CT, MRI,
or a combination of these. High-resolution real-time sonography
serves as an inexpensive and accurate modality for differentiating
hydrocele of the Canal of Nuck from the aforementioned conditions.
In an ultrasound scan, Nuck cyst appears as a thin walled, tubular
or dumbbell shaped, well defined, anechoic or hypoechoic,
unilocular or multilocular cystic structure (19,22). In a
colour Doppler scan, the Nuck cyst does not show any internal
vascularity (28,29). Additionally, an MRI may also be
performed, particularly in complicated cases, such as those
involving additional pathologies where hydrocele usually appears as
a well-defined, thin-walled cystic lesion in hypointense on
T1-weighted and hyperintense on T2-weighted series (1). Imaging with MRI allows for good
visualization of the anatomic structures surrounding the cyst,
communication between the cyst and the peritoneal cavity and the
extension of the cyst of the Canal of Nuck (22). However, despite the utility of imaging
in differential diagnosis, surgery along with histological and
immunohistological analysis of the excised mass is required for a
more conclusive diagnosis of a Nuck cyst.
Another issue that should be addressed is the
association of the pathology of the Canal of Nuck with fertility.
In the present case report as well as in the published literature,
there was only one association with infertility; a nulliparous
woman of reproductive age who underwent simultaneous ovarian cyst
excision and repair of patent Canal of Nuck (20). Nonetheless, infertility in this case
was not attributed to the Nuck canal pathology. Postoperative
courses of all published cases are uneventful. Unfortunately, data
concerning postoperative fertility was not available for any of the
reported cases. Other pathologies of the Canal of Nuck such as
ovary herniation or endometriosis of the canal may result in
infertility in young females (30).
Surgical management of a cyst of the Canal of Nuck
includes open or laparoscopic excision of the cystic structure with
concomitant closure of the inguinal internal defect primarily with
the use of a mesh (24,31,32). The
appropriate surgical approach is tailored based on the extent of
the disease, the accuracy of preoperative diagnosis and the
co-existence of an inguinal hernia. In the case of concomitant
identification of an inguinal hernia, an additional hernia repair
with or without mesh placement can be safely performed.
Furthermore, as described by Ferreira et al (17), an additional vulva correction may be
indicated in cases of mass extension to the labia majora.
To the best of our knowledge this is the first
literature review which presents a cumulative report of cases of
adult females with Nuck cyst. The risk of potential loss of
relevant literature was eliminated by performing a thorough search
of the current literature. Due to limited data from case reports
and small case series, the actual prevalence of Nuck cyst could not
be precisely estimated. The significant heterogeneity among the
included studies along with the lack of mention of certain
parameters by some authors were additional limitations. In
conclusion, the cyst of the canal of Nuck is a rare condition, but
it should be included in the differential diagnosis list of
inguinal tumours in female patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
APr and NM conceived and designed the study. APr,
APa, DS, CN and ES acquired, analysed and interpreted the data.
APr, APa, DS, CN, NM and ES drafted and revised the manuscript. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rees MA, Squires JE, Tadros S and Squires
JH: Canal of Nuck hernia: A multimodality imaging review. Pediatr
Radiol. 47:893–898. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tubbs RS, Loukas M, Shoja MM, Salter EG
and Oakes WJ: Indirect inguinal hernia of the urinary bladder
through a persistent canal of Nuck: Case report. Hernia.
11:287–288. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bhattacharjee PK and Ghosh G: Hydrocele of
the canal of Nuck. J Indian Med Assoc. 104:150–151. 2006.PubMed/NCBI
|
|
4
|
Caviezel A, Montet X, Schwartz J, Egger JF
and Iselin CE: Female hydrocele: The cyst of Nuck. Urol Int.
82:242–245. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zawaideh JP, Trambaiolo Antonelli C,
Massarotti C, Remorgida V and Derchi LE: Cyst of Nuck: A
disregarded pathology. J Minim Invasive Gynecol. 25:376–377.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Dagur G, Gandhi J, Suh Y, Weissbart S,
Sheynkin YR, Smith NL, Joshi G and Khan SA: Classifying hydroceles
of the pelvis and groin: An overview of etiology, secondary
complications, evaluation, and management. Curr Urol. 10:1–14.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Matsumoto T, Hara T, Hirashita T, Kubo N,
Hiroshige S and Orita H: Laparoscopic diagnosis and treatment of a
hydrocele of the canal of Nuck extending in the retroperitoneal
space: A case report. Int J Surg Case Rep. 5:861–864.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Qureshi NJ and Lakshman K: Laparoscopic
excision of cyst of canal of Nuck. J Minim Access Surg. 10:87–89.
2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Patnam V, Narayanan R and Kudva A: A
cautionary approach to adult female groin swelling: Hydrocoele of
the canal of Nuck with a review of the literature. BMJ Case Rep
2016: pii: bcr2015212547, 2016.
|
|
10
|
Uzun I, Inan C, Varol F, Erzincan S, Sutcu
H and Sayin C: Hemorrhagic cyst of the canal of Nuck after vaginal
delivery presenting as a painful inguinal mass in the early
postpartum period. Eur J Obstet Gynecol Reprod Biol. 213:147–148.
2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pandey A, Jain S, Verma A, Jain M,
Srivastava A and Shukla RC: Hydrocele of the canal of Nuck-Rare
differential for vulval swelling. Indian J Radiol Imaging.
24:175–177. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Safak AA, Erdogmus B, Yazici B and Gokgoz
AT: Hydrocele of the canal of Nuck: Sonographic and MRI
appearances. J Clin Ultrasound. 35:531–532. 2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Noguchi D, Matsumoto N, Kamata S and
Kaneko K: Ectopic pregnancy developing in a cyst of the canal of
Nuck. Obstet Gynecol. 123:472–476. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Amu OC, Udeh EI, Ugochukwu AI, Madu C and
Nzegwu MA: A case of vulval swelling secondary to female
circumcision posing a diagnostic dilemma. Int J Surg Case Rep.
3:431–434. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sala P, Palmeri A and Costantini S: Giant
cyst of the Nuck canal: A worrisome trouble for a girl. Am J Obstet
Gynecol. 218:530–531. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jagdale R, Agrawal S, Chhabra S and Jewan
SY: Hydrocele of the canal of Nuck: Value of radiological
diagnosis. J Radiol Case Rep. 6:18–22. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ferreira AF, Marques JP and Falcao F:
Hydrocele of the canal of Nuck presenting as a sausage-shaped mass.
BMJ Case Rep 2017: pii: bcr-2017-221024, 2017.
|
|
18
|
Karapolat B, Ata Korkmaz HA, Kocak G and
Bulut E: Image of the month: Cyst of the canal of Nuck. Acta Chir
Belg. 118:138–140. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ozel A, Kirdar O, Halefoglu AM, Erturk SM,
Karpat Z, Lo Russo G, Maldur V and Cantisani V: Cysts of the canal
of Nuck: Ultrasound and magnetic resonance imaging findings. J
Ultrasound. 12:125–127. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yen CF, Wang CJ, Chang PC, Lee CL and
Soong YK: Concomitant closure of patent canal of Nuck during
laparoscopic surgery: Case report. Hum Reprod. 16:357–359.
2001.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kim KS, Choi JH, Kim HM, Kim KP, Kwon YJ,
Hwang JH and Lee SY: Hydrocele of the canal of nuck in a female
adult. Arch Plast Surg. 43:476–478. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kono R, Terasaki H, Murakami N, Tanaka M,
Takeda J and Abe T: Hydrocele of the canal of Nuck: A case report
with magnetic resonance hydrography findings. Surg Case Rep.
1(86)2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Sethi V and Patel H: Hydrocele in the
Canal of Nuck-CT appearance of a developmental groin anomaly. J
Radiol Case Rep. 10:29–33. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Ryan JD, Joyce MR, Pierce C, Brannigan A
and O'Connell PR: Haematoma in a hydrocele of the canal of Nuck
mimicking a Richter's hernia. Hernia. 13:643–645. 2009.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Choi YM, Lee GM, Yi JB, Yoon KL, Shim KS,
Bae CW, Choi SI and Kim HC: Two cases of female hydrocele of the
canal of nuck. Korean J Pediatr. 55:143–146. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Akkoyun I, Kucukosmanoglu I and
Yalinkilinc E: Cyst of the canal of nuck in pediatric patients. N
Am J Med Sci. 5:353–356. 2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Papparella A, Vaccaro S, Accardo M, De
Rosa L, Ronchi A and Noviello C: Nuck cyst: A rare cause of
inguinal swelling in infancy. Minerva Pediatr: Jul 23, 2018 (Epub
ahead of print).
|
|
28
|
Stickel WH and Manner M: Female hydrocele
(cyst of the canal of Nuck): Sonographic appearance of a rare and
little-known disorder. J Ultrasound Med. 23:429–432.
2004.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Park SJ, Lee HK, Hong HS, Kim HC, Kim DH,
Park JS and Shin EJ: Hydrocele of the canal of Nuck in a girl:
Ultrasound and MR appearance. Br J Radiol. 77:243–244.
2004.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Choi KH and Baek HJ: Incarcerated ovarian
herniation of the canal of Nuck in a female infant:
Ultrasonographic findings and review of literature. Ann Med Surg
(Lond). 9:38–40. 2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Bagul A, Jones S, Dundas S and Aly EH:
Endometriosis in the canal of Nuck hydrocele: An unusual
presentation. Int J Surg Case Rep. 2:288–289. 2011.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Jimenez JS, Barbero P, Tejerizo A, Guillen
C and Strate C: A laparoscopic approach to Nuck's duct
endometriosis. Fertil Steril. 96:e103–e105. 2011.PubMed/NCBI View Article : Google Scholar
|