Introduction
Pulmonary contusion (PC) is the most commonly
diagnosed intrathoracic injury resulting from chest blunt trauma,
which is usually caused by a high-kinetic energy chest wall impact
(1). It has been reported that the
incidence of PC is 25-35% of all blunt chest traumas (1-3).
Patients with PC are vulnerable to negative pulmonary outcomes,
which include pneumonia, acute respiratory distress syndrome
(ARDS), respiratory failure and death (4). The possible mechanisms are based on
inertial effects, primarily on different tissue densities of light
alveolar tissue and heavy hilar structures (2). Interstitial oedema and inflammatory
cell infiltration following parenchymal injury result in lung
hemorrhage, and PC develops slowly over the course of 24-48 h after
chest injury. Supportive care, including mechanical ventilation, is
the primary clinical management course for PC, and it is typically
resolved within 3-14 days, depending on the size (1).
Interleukin (IL)-17 belongs to the IL-17 cytokine
family and has a molecular weight of 35 kDa. IL-17 was initially
shown to be secreted by a subset of CD4+ T cells, termed
Th17 cells. These cells also secrete cytokines IL-22 and
IL-21(5). IL-17 primarily affects
epithelial cells in tissues, such as the gut, lung and skin
(5), and was found to serve a key
role in host defense against infection, development of inflammatory
diseases (6), and enhancement of
mucosal barrier repair and maintenance by stimulating epithelial
cell proliferation and tight junction protein production (5). It was reported that IL-17 is a useful
biomarker for predicting the outcomes in patients who have suffered
a physical trauma (7,8). However, whether IL-17 is related to the
severity and outcomes of PC remains unknown.
IL-22 belongs to the IL-10 cytokine family and is
produced primarily by innate and adaptive T cells, such as Th22,
Th17, and Th1 cells (9). It has the
ability to strengthen homeostatic epithelial barrier functions in
addition to the robustness and strength resistance of tissue
(10). IL-22 has been reported to
serve a critical role in maintaining epithelial integrity during
pulmonary infection (11) and
ventilator-induced lung injury (12). It has also been shown that IL-22
interacts with IL-17 to coordinate pulmonary immune defense during
lung inflammation (13).
Furthermore, the IL-17/IL-22 axis was found to serve important
roles in burn injuries (14) and
sepsis-induced lung injury (15).
However, whether IL-22 is related to the severity and outcomes of
PC remains unknown.
In the present study, the hypothesis that IL-17 and
IL-22 may be used as predictors of the severity and outcomes of PC
patients was assessed. The results showed that the severity of PC
was a risk factor for in-patient outcomes, and IL-17, but not
IL-22, could be used as a biomarker to predict the severity of PC.
Furthermore, IL-17 could also be used as a biomarker for predicting
the outcomes of in-patients who had suffered a PC.
Materials and methods
Patient enrolment
All trauma patients admitted to The First Affiliated
Hospital of Guangxi Medical University between January 2015 and
December 2017, were studied. All patients who met the following
criteria were included: Age, >14 years old; patients with chest
computed tomography (CT) scans and those diagnosed with PC at
admission to the Department of Emergency, The First Affiliated
Hospital of Guangxi Medical University. All patients lacking
clinical or biological data and chest CT investigations were
excluded. Clinical information, including sociodemographic
parameters, clinical data, biological findings and therapeutic
interventions, was recorded for all patients who were enrolled. The
injury severity score (ISS) was measured to evaluate the
seriousness of patients as previously described (16). Written informed consent was obtained
from each participant prior to enrolment, and this study was
approved by the Medical Ethics Committee of The First Affiliated
Hospital of Guangxi Medical University.
During the present study period, 23,246 trauma
patients were admitted to The First Affiliated Hospital of Guangxi
Medical University. Of these, 438 patients (438/23 246, 1.9%) had
blunt chest trauma, of which 128 patients were excluded (53
patients lacking data, 51 patients lacking chest imaging
investigation, 24 patients died shortly after admission to the
hospital), and thus 310 patients were enrolled in the present
study, 151 patients with PC (34.5%, PC group) and 159 patients
without PC (65.5%, non-PC group). Additionally, 50 healthy
individuals were enrolled as controls. A similar percentage of
participants were male [PC group vs. non-PC group, 116 (76.8%) vs.
115 (72.3%)], respectively (P=0.364), and mean ages were also
similar in each group (PC group vs. non-PC group, mean ± standard
deviation, 42.2±15.9 vs. 39.0±15.1. The median age was 42 years old
(range, 15-86 years) in the PC group vs. 37 years old (range, 15-89
years) in the non-PC group, and did not differ significantly
(P=0.066; Table I).
 | Table ISociodemographic characteristics of
the patients with or without pulmonary contusion. |
Table I
Sociodemographic characteristics of
the patients with or without pulmonary contusion.
| Characteristics | PC group,
n=151a | Non-PC group,
n=159a | P-value |
|---|
| Age, years | 42.2±15.9 | 39.0±15.1 | 0.066 |
| Sex
(male/female) | 116/35 | 115/44 | 0.364 |
| Mechanism of
injury | | |
<0.001b |
|
Motor
vehicle crash | 61 | 44 | 0.018b |
|
Bicycle | 22 | 21 | |
|
Pedestrian | 10 | 35 | |
|
Fall | 39 | 25 | |
|
Explosion | 19 | 34 | |
| Comorbidities | | | 0.637 |
|
Diabetes
mellitus | 10 | 13 | |
|
Hypertension | 15 | 11 | |
|
Smoking | 20 | 27 | |
|
COPD | 5 | 8 | |
|
None | 101 | 100 | |
| Localization |
|
Right | 23 | - | |
|
Left | 18 | - | |
|
Bilateral | 110 | - | |
| Other types of
chest trauma |
|
None | 84 | 126 |
<0.001b |
|
Pneumothorax/Haemothorax/ | 5/13/23/26 | 7/7/5/14 | |
|
Haemopneumothorax/Rib
fractures | | | |
| Rib fractures, ≤3;
>3 | 115/36 | 157/2 |
<0.001b |
| ISS | 31.9±10.0 | 29.9±9.5 | 0.071 |
|
ISS, ≤16;
>16 | 15/136 | 25/134 | 0.129 |
| Polytrauma,
yes/no | 129/22 | 120/39 | 0.027b |
| SaO2,
% | 98.8±2.9 | 98.4±3.4 | 0.324 |
| Thoracic trauma
treatment | | | <0.001 |
|
Conservative | 110 | 146 | |
|
Pleurocan
drainage | 41 | 13 | |
| Complications | | | <0.001 |
|
None | 56 | 140 | |
|
Pneumonia | 49 | 14 | |
|
Pleural
effusion | 26 | 5 | |
|
Pneumonia
and pleural effusion | 20 | 0 | |
| ARDS, yes/no | 28/123 | 12/147 | 0.004c |
| Blood products,
yes/no | 32/119 | 27/132 | 0.345 |
| ICU admission,
yes/no | 20/131 | 9/150 | 0.022b |
| ICU stay, days | 5.2±1.7 | 3.8±1.4 | 0.040b |
| Mechanical
ventilation, yes/no | 19/132 | 9/150 | 0.034b |
| Ventilatory,
days | 4.2±1.6 | 2.9±0.9 | 0.029b |
| Hospital stay,
days | 26.2±21.7 | 13.3±10.7 |
<0.001d |
| Mortality,
yes/no | 3/148 | 4/155 | 0.754 |
Blood samples
Whole-blood samples were taken within 2 h after
admission, and then taken on days 3, 5 and 7 after trauma. Blood
samples were centrifuged at 500 x g for 10 min in a refrigerated
(4˚C) centrifuge, and then the plasma was collected and stored at
-80˚C until assayed. Blood samples were taken only once in the
healthy group.
Pulmonary contusion volume
measurement
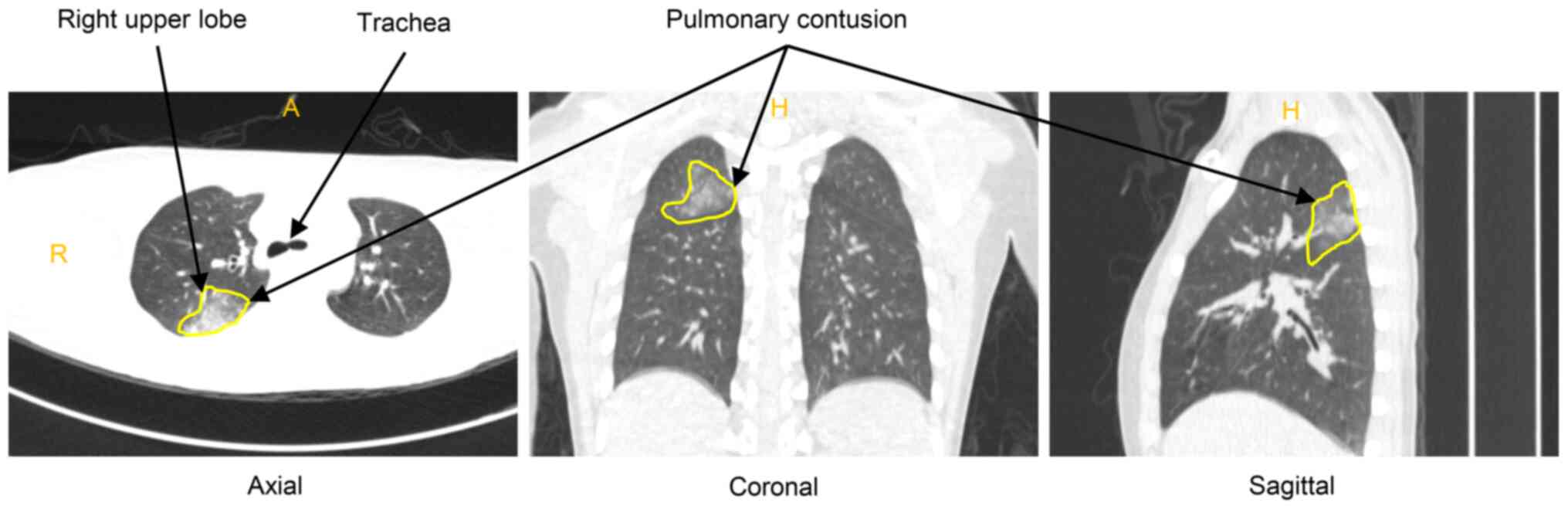
The appearance of CT scan for PC shows nonspecific,
focal, or diffuse alveolar infiltrates over the lung fields, and it
always appears as areas of lung consolidation (Fig. 1). PC volume was measured as
previously described (17). Briefly,
trauma patients with suspected chest injuries were scanned with a
64-slice CT scanner (Siemens Healthcare GmbH). The volume of lung
contusion was measured by the CT volume, which was calculated based
on the ratio of contused lung to the total lung volume. Images were
evaluated by two consultant radiologists and 3-dimensional
volumetric analysis of the data was calculated on the workstation
(ReconCT version 13.8.2.0; Siemens Healthcare GmbH). The total
volume of lung contusions in both lungs was calculated and
expressed as a percentage of the total lung volume.
ELISA
The plasma levels of IL-17 and IL-22 were measured
by ELISA according to the manufacturer's protocol (IL-17, cat. no.
D1700; IL-22, cat. no. D2200; R&D Systems, Inc.).
Statistics
SPSS version 22.0 (IBM Corp.) was used to perform
the statistical analyses. Differences in continuous variables are
presented as the mean ± standard deviation, and were calculated
using a Student's t-test or a Mann-Whitney U test, whereas a
χ2 test or Fisher's exact test was used to analyze
categorical variables. Spearman's rank correlation coefficient
analysis was performed to determine correlations. Factors
independently associated with PC outcomes were determined by the
binary logistical regression model. Receiver operating
characteristic (ROC) curve analysis was performed to determine the
predictive value of PC volume and IL-17 for PC outcomes. P<0.05
was considered to indicate a statistically significant
difference.
Results
Sociodemographic characteristics of
patients with or without pulmonary contusion
There were no significant differences between
preexisting comorbidity status (diabetes mellitus, hypertension and
chronic obstructive pulmonary disease) or smoking history between
the groups. There was a higher percentage of individuals who had
experienced a motor vehicle crash in the PC group compared with the
non-PC group [61 (40.4%) vs. 44 (27.7%), respectively; P=0.018],
whereas other causes, such as falling off a bicycle, falling down
whilst walking/running, falling from a high place, or getting hit
in the chest by an explosion, were similar between groups (Table I). For the control group, the male
percentage of participants was 76.0% (38/50), and the mean age was
40.3±14.6 years old. There were no significant differences in the
sex distribution between any of the groups.
A total of 23 patients had PC in the right lung, 18
in the left lung and 110 in the bilateral lungs. Except for PC, the
other types of chest trauma in the PC group and non-PC group were
pneumothorax, haemothorax, haemopneumothorax and rib fractures. A
total of 36 patients in the PC group had >3 rib fractures,
whilst only 2 patients in the non-PC group had >3 rib fractures
(23.8 vs. 1.3%, P<0.001). The ISS was 31.9±10.0 for the PC group
and 29.9±9.5 for the non-PC group (P=0.071). A total of 136
patients had serious injuries (ISS>16) in the PC group, whereas
134 patients had serious injuries in the non-PC group (P=0.129).
Significantly more patients had polytrauma in the PC group (129
patients compared with the non-PC group (120 patients; P=0.027).
The arterial oxygen saturation was similar in both groups (P=0.324)
(Table I).
There were 41 patients (27.2%) receiving Pleurocan
drainage treatment in the PC group and only 13 patients (8.2%) in
the non-PC group (P<0.001). Additionally, 49 patients (32.5%)
had pneumonia complications in the PC group, whereas 13 patients
(8.2%) had pneumonia complications in the non-PC group
(P<0.001). Other complications, including pleural effusion and
pneumonia with pleural effusion, were similar amongst both groups.
A total of 28 patients experienced ARDS in the PC group, whereas 12
patients experienced ARDS in the non-PC group (P=0.004).
Additionally, 20 patients (13.2%) were admitted to the intensive
care unit (ICU) in the PC group, whereas only 9 patients (5.7%) in
the non-PC group were admitted (P=0.022). Patients admitted to the
ICU in the PC group stayed in hospital for a longer time period
than those in the non-PC group (5.2±1.8 vs. 3.8±1.4 days,
respectively; P=0.040). In the PC group, 19 patients (12.6%)
received mechanical ventilation, whereas only 9 patients (5.7%) in
the non-PC group received mechanical ventilation (P=0.034). The
average ventilatory days for PC patients were greater than that for
non-PC patients (4.2±1.6 vs 2.9±0.9 days, respectively; P=0.029).
Overall, PC patients had a longer hospital stays than non-PC
patients (26.2±21.7 vs. 13.3±10.7 days, respectively; P<0.001).
However, the mortality rate was similar in both groups (2.0 vs.
2.5%; P=0.754; Table I).
Severity of pulmonary contusion is a
risk factor for in-patient outcomes
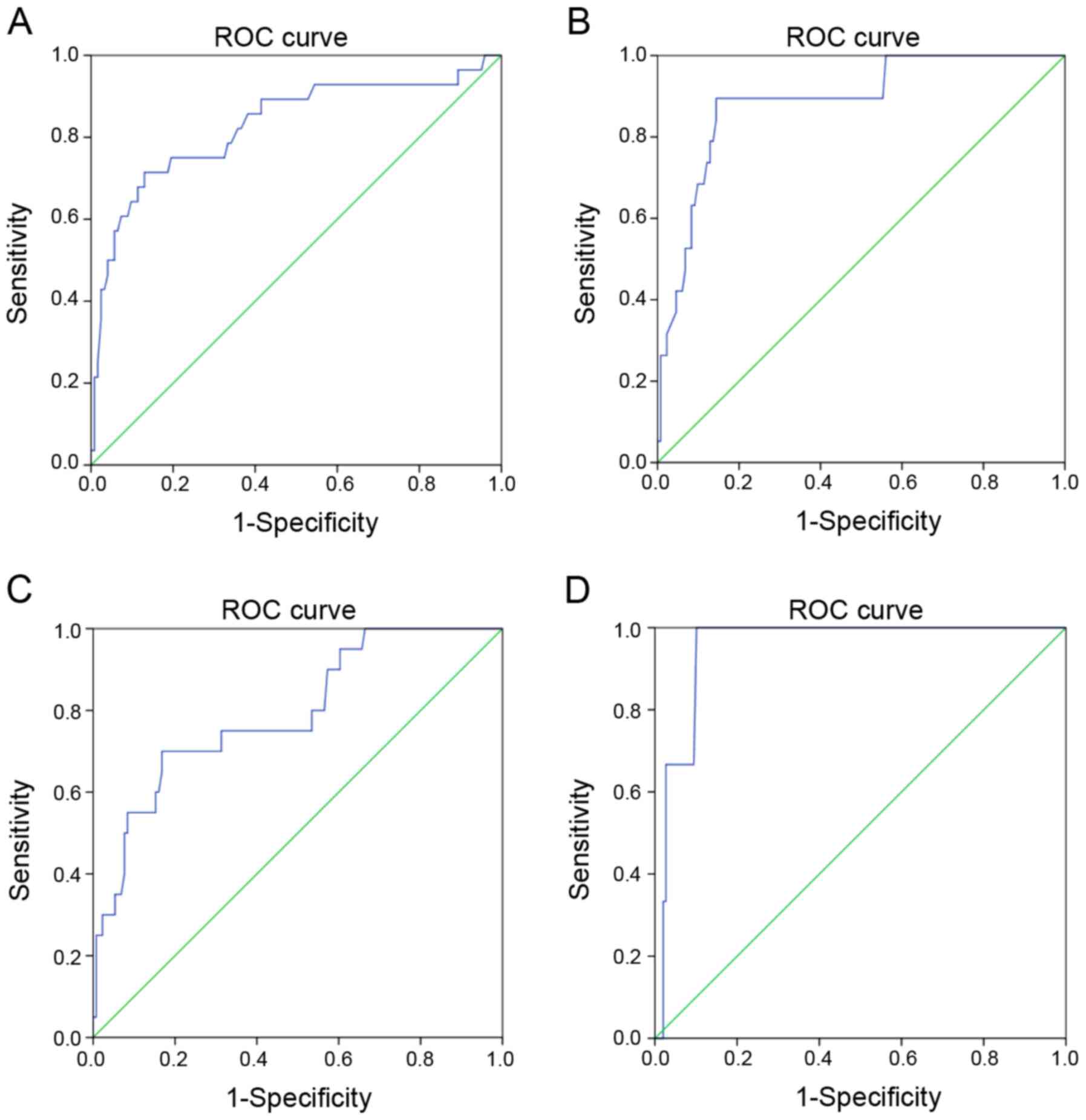
To determine whether PC volume was associated with
in-patient outcomes, the data were analyzed using ROC curves. The
area under the curve (AUC) value of 0.828 [standard error, 0.050;
95% confidence intervals (CI), 0.730-0.927] significantly
determined the predictive value of PC volume for the occurrence of
ARDS (P<0.001; Fig. 2A). The AUC
value of 0.886 (standard error, 0.040; 95% CI, 0.808-0.964)
significantly determined the predictive value of PC volume for
mechanical ventilation (P<0.001; Fig.
2B). The AUC value of 0.793 (standard error, 0.055; 95% CI,
0.684-0.901) significantly determined the predictive value of PC
volume for ICU admission (P<0.001; Fig. 2C). The AUC value of 0.952 (standard
error, 0.025; 95% CI, 0.902-1.000) significantly determined the
predictive value of PC volume for mortality (P=0.008; Fig. 2D).
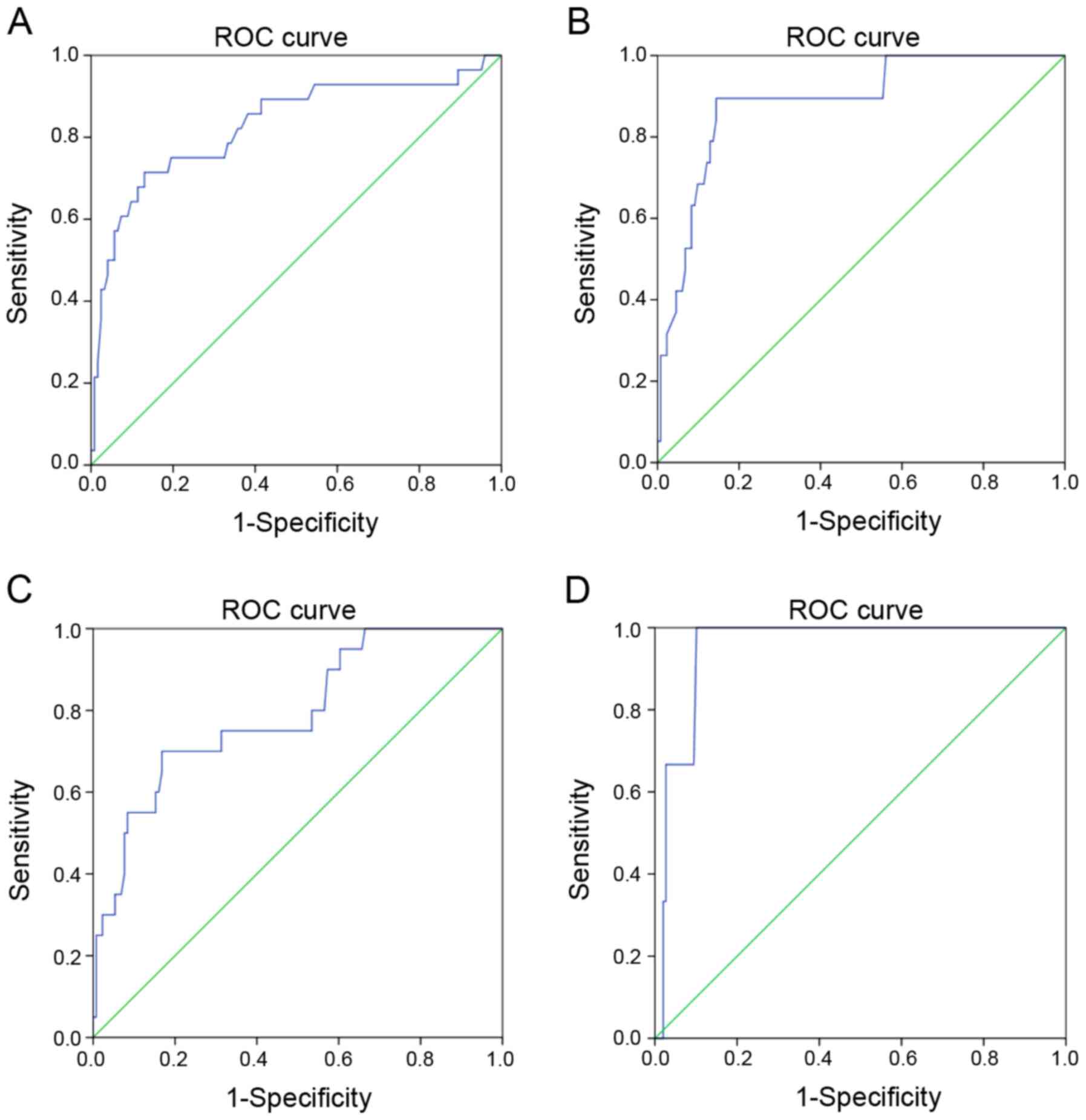 | Figure 2ROC curves of PC volume in predicting
in-patient outcomes. (A) ROC curves for PC volume and ARDS. AUC,
0.828; standard error, 0.050; 95% CI, 0.730-0.927; P<0.001. (B)
ROC curves for PC volume and mechanical ventilation. AUC, 0.886;
standard error, 0.040; 95% CI, 0.808-0.964; P<0.001. (C) ROC
curves for PC volume and ICU admission. AUC, 0.793; standard error,
0.055; 95% CI, 0.684-0.901; P<0.001. (D) ROC curves for PC
volume and mortality. AUC, 0.828; standard error, 0.025; 95% CI,
0.902-1.000; P=0.008. ROC, receiver operating characteristic; PC,
pulmonary contusion; ARDS, acute respiratory distress syndrome;
AUC, area under the curve; CI, confidence interval; ICU, intensive
care unit. |
To further evaluate the impact of PC on in-patient
outcomes, binary logistical regression analysis was performed. PC
volume was an independent factor influencing the occurrence ratio
of ARDS (P=0.001) and mechanical ventilation (P=0.018; Table II). Furthermore, ARDS was predicted
to prolong ICU stay (P=0.010; Table
III). Mechanical ventilation was also predicted to increase the
amount of time the patient was required to stay in ICU stay
(P=0.035) and to increase the mortality rate (P=0.018; Table IV).
 | Table IILogistical regression analysis of
variables associated with pulmonary contusion outcomes. |
Table II
Logistical regression analysis of
variables associated with pulmonary contusion outcomes.
| | | | | | 95% confidence
interval for Exp(β) |
|---|
| Clinicopathological
characteristic | β | Standard error | P-value | Exp(β) | Lower | Upper |
|---|
| Mortality |
|
PC
volume | -0.664 | 0.396 | 0.094 | 0.515 | 0.237 | 1.120 |
| Mechanical
ventilation |
|
Rib
fractures | -5.439 | 2.029 | 0.007 | 0.004 | 0.000 | 0.232 |
|
Blood
products | 2.863 | 1.163 | 0.014 | 17.514 | 1.792 | 171.158 |
|
PC
volume | -0.283 | 0.119 | 0.018 | 0.753 | 0.596 | 0.952 |
|
ARDS | 3.263 | 1.191 | 0.006 | 26.127 | 2.531 | 269.701 |
| ARDS |
|
SaO2 | 0.504 | 0.137 | <0.001 | 1.655 | 1.266 | 2.164 |
|
PC
volume | -0.124 | 0.036 | 0.001 | 0.883 | 0.823 | 0.948 |
 | Table IIIRelationship between ARDS and patient
outcomes. |
Table III
Relationship between ARDS and patient
outcomes.
| Variables | ARDSa |
Non-ARDSa | P-value |
|---|
| ICU stay,
days, | 5.7±1.9 | 3.8±1.3 | 0.010b |
| Hospital stay,
days | 18.9±9.5 | 19.7±8.0 | 0.792 |
| Mortality,
yes/no | 2/38 | 5/265 | 0.224 |
 | Table IVRelationship between mechanical
ventilation and patient outcomes. |
Table IV
Relationship between mechanical
ventilation and patient outcomes.
| Variables |
Ventilationa |
No-Ventilationa | P-value |
|---|
| ICU stay, days | 5.4±2.0 | 3.4±0.5 | 0.035b |
| Hospital stay,
days | 18.6±7.4 | 19.7±8.2 | 0.763 |
| Mortality,
yes/no | 3/25 | 4/278 | 0.018b |
IL-17 can be used as a biomarker to
predict the severity of pulmonary contusion
Several studies have indicated that IL-17 and IL-22
are useful predictive biomarkers in lung diseases (18), infectious diseases (5) and trauma outcomes (7,8,19). However, whether IL-17 and IL-22 are
useful biomarkers to predict the severity of PC remains unknown. As
expected, IL-17 and IL-22 increased significantly after trauma and
peaked on day 5 after trauma. The plasma levels of IL-17 were
significantly different between the PC group and the non-PC group
on different days after trauma. However, there were no differences
in IL-22 between the PC and non-PC groups (Table V). Furthermore, the plasma levels of
IL-17 on day 1 or the median of 7 days after trauma were correlated
with PC volume (Table VI). Taken
together, these data indicate that IL-17 may be used as a biomarker
to predict the severity of PC.
 | Table VPlasma levels of IL-17 and IL-22 in
the patients with or without PC. |
Table V
Plasma levels of IL-17 and IL-22 in
the patients with or without PC.
| Cytokines | Control | PC group,
n=151 | Non-PC group,
n=159 | P-value |
|---|
| IL-17, pg/ml
(range) | 32.1±11.2
(0-45) | | |
<0.001a,b |
|
Day 1 | |
179.5±167.7a |
95.0±81.6b | <0.001 |
|
Day 3 | | 330.2±244.8 | 212.6±175.2 | <0.001 |
|
Day 5 | | 535.7±285.3 | 321.9±218.4 | <0.001 |
|
Day 7 | | 267.3±218.1 | 193.5±171.0 | 0.001 |
| IL-22, pg/ml
(range) | 33.7±9.3
(0-53.3) | | |
<0.001c,d |
|
Day 1 | |
62.9±44.9c |
62.3±41.3d | 0.902 |
|
Day 3 | | 127.5±85.9 | 126.1±77.4 | 0.878 |
|
Day 5 | | 222.9±130.2 | 239.6±125.4 | 0.25 |
|
Day 7 | | 89.8±51.0 | 97.1±52.0 | 0.216 |
 | Table VIRelationship between plasma levels of
IL-17 and PC volume. |
Table VI
Relationship between plasma levels of
IL-17 and PC volume.
| Statistical
parameter | IL-17 (Day 1) and
PC volume | IL-17 (median) and
PC volume |
|---|
| Spearman's rho
correlation coefficient | 0.922 | 0.923 |
| P, two-tailed |
<0.001a |
<0.001a |
| n | 151 | 151 |
IL-17 can be used as a biomarker to
predict in-patient outcomes of trauma patients
To determine whether IL-17 was a biomarker for
predicting in-hospital outcomes of patients with PC, the
relationship between IL-17 and pro-inflammatory complications was
assessed, and the predictive value of IL-17 in ARDS, mechanical
ventilation, ICU admission and mortality was also determined. High
levels of plasma IL-17 were related to a high occurrence ratio of
PC. Furthermore, patients with high levels of plasma IL-17 suffered
more serious trauma and were more vulnerable to developing ARDS
(Table VII).
 | Table VIIRelationship between IL-17 and
pro-inflammatory complications. |
Table VII
Relationship between IL-17 and
pro-inflammatory complications.
| | IL-17, Day
1a | | IL-17,
mediana | |
|---|
| Complications | ≤45 pg/ml | >45 pg/ml | P-value | ≤90 pg/ml | >90 pg/ml | P-value |
|---|
| PC | | | 0.009 | | |
<0.001c |
|
PC | 28 | 123 | | 29 | 122 | |
|
Non-PC | 50 | 109 | | 61 | 98 | |
| ISS | 23.4±10.6 | 29.1±11.1 | <0.001 | 23.8±10.5 | 29.2±11.2 |
<0.001c |
| ARDS | | | 0.018 | | | 0.036b |
|
ARDS | 4 | 36 | | 6 | 34 | |
|
Non-ARDS | 74 | 196 | | 84 | 186 | |
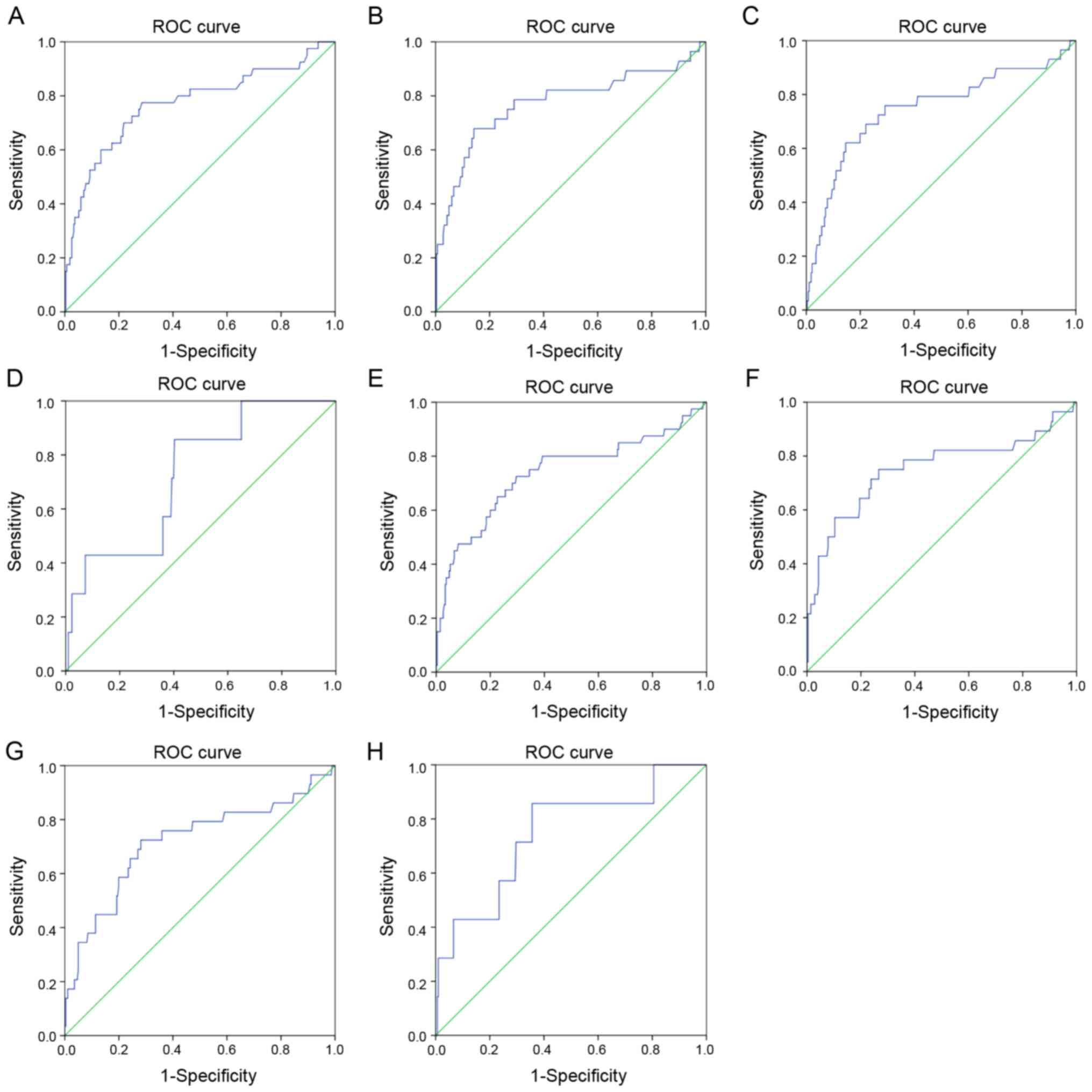
ROC analysis was used to calculate the predictive
value of IL-17 for in-patient outcomes and found that the levels of
plasma IL-17 were useful for predicting ARDS occurrence, mechanical
ventilation, ICU admission and mortality (Fig. 3).
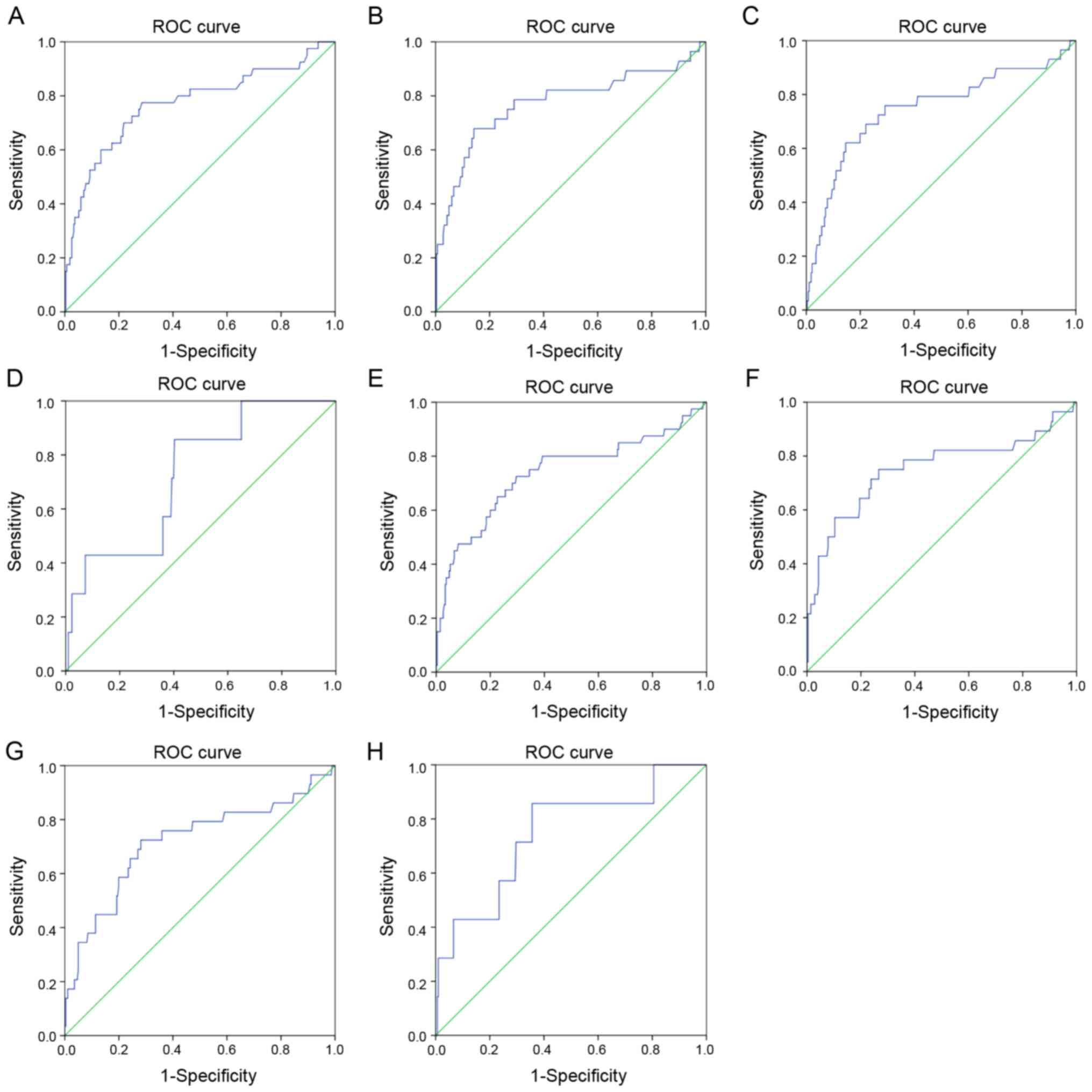 | Figure 3ROC curves of IL-17 for predicting the
in-hospital outcomes of patients. (A) ROC curves for IL-17 (day 1)
and ARDS. AUC, 0.770; standard error, 0.047; 95% CI, 0.679-0.862;
P<0.001. (B) ROC curves for IL-17 (day 1) and mechanical
ventilation. AUC, 0.773; standard error, 0.058; 95% CI,
0.659-0.887; P<0.001. (C) ROC curves for IL-17 (day 1) and ICU
admission. AUC 0.747; standard error, 0.057; 95% CI, 0.636-0.858;
P<0.001. (D) ROC curves for IL-17 (day 1) and mortality. AUC,
0.727; standard error, 0.086; 95% CI, 0.558-0.897; P=0.040. (E) ROC
curves for IL-17 (median) and ARDS. AUC, 0.737; standard error,
0.051; 95% CI, 0.638-0.837; P<0.001. (F) ROC curves for IL-17
(median) and mechanical ventilation, AUC, 0.752; standard error,
0.061; 95% CI, 0.632-0.871; P<0.001. (G) ROC curves for IL-17
(median) and ICU admission. AUC, 0.717; standard error, 0.059; 95%
CI, 0.602-0.832; P<0.001. (H) ROC curves for IL-17 (median) and
mortality. AUC, 0.747; standard error, 0.099; 95% CI, 0.552-0.941;
P=0.026. ROC, receiver operating characteristic; IL, interleukin;
ARDS, acute respiratory distress syndrome; AUC, area under the
curve; CI, confidence interval; ICU, intensive care unit. |
Discussion
PC is very common in patients who suffer blunt chest
traumas, and the severity of PC ranges from mild to
life-threatening (3,20). In the present study, the incidence of
blunt chest trauma was 1.9%, and the incidence of PC in these
patients was 34.5%, which was similar to previous studies (1-3).
The major cause of injury was motor vehicle crashes, which was also
the major cause of PC. This was primarily because in motor vehicle
crashes, patients are hit in the chest with a powerful impact, and
the chest wall is compressed and then rebounds. This was
hypothesized to be the primary cause of PC (1,21). Other
causes, including injuries related to bicycles, walking, falling
and explosions, were similar in the PC group and the non-PC group.
The baseline data of participants, which included age, sex and
comorbidities, were similar in the PC and non-PC groups. Thus,
these cohorts were suitable for comparing between the PC group and
the non-PC group.
Isolated PC is rare, and PC is often accompanied by
serious bony thorax damage, such as rib fractures (22). In the present study, the majority of
the PC was located in both the lungs. PC patients had a high
incidence of other types of chest traumas, including pneumothorax,
haemothorax, haemopneumothorax and rib fractures. Furthermore,
patients with >3 rib fractures were more likely to experience
PC. Previous studies have shown that the number of rib fractures
was a predictor of the severity of PC (22), and the number of fractured ribs best
predicted the appearance of complications (such as delayed
pleuropulmonary complications and increased bleeding) (23). In the present study, it was also
shown that patients with PC had a higher rate of polytraumas. A
possible explanation for this was that patients with more rib
fractures or polytraumas had higher-energy impacts, which were
always accompanied by blunt chest trauma.
Several studies have shown that PC patients have
high incidences of negative pulmonary outcomes (4,22). The
present study showed that patients with PC were more likely to
develop ARDS, were more likely to be admitted to the ICU and
receive mechanical ventilation. Patients with PC had longer periods
receiving assisted ventilation, ICU stays and total length of
hospital stays. These findings were consistent with those of a
previous study (4). However, there
was no difference in mortality between the PC group and the non-PC
group. A possible explanation for this is that mortality was
related to several factors, and PC usually affects the pulmonary
situation, which recovers very well after effective supportive
care.
PC volume represents the size of contused lung, and
a previous study showed that quantifying PC volume could allow
identification of patients at high risk of ARDS and that CT
contusion volume was significantly correlated with injury severity
in patients with blunt chest trauma (17). In the present study, PC volume was
significantly associated with ARDS occurrence, mechanical
ventilation rate, ICU admission and mortality. Furthermore, in the
logistical regression analysis, PC volume was an independent
predictive factor for ARDS occurrence and mechanical ventilation
rate. The data also showed that ARDS and mechanical ventilation
could prolong ICU stay. Mortality rates were also higher amongst
patients receiving mechanical ventilation. Thus, these findings
support the hypothesis that PC volume was effective in predicting
the outcomes of PC patients.
IL-17 is a glycosylated protein that is associated
with the severity of inflammation in tissues by inducing the
production of other pro-inflammatory mediators, including IL-1,
TNF, IL-6, IL-8, CCL20 and G-CSF, which collectively results in an
influx of neutrophils (24). IL-17
exhibits synergistic function with other mediators, including IL-1,
IL-6 and TNF-α, to activate tissue-infiltrating neutrophils, and
these neutrophils facilitate the effective elimination of invading
bacteria or fungi (25). Previous
studies have shown that IL-17 serves a central role in the
pathogenesis of the systemic inflammatory response to injury
(26). A high plasma IL-17
concentration has a unique and independent association with
susceptibility to sepsis in polytrauma patients (7). In the present study, IL-17 and IL-22
levels were increased significantly after PC and peaked on day 5
after PC diagnosis. However, only the plasma IL-17 levels were
significantly different between the PC group and the non-PC group.
Furthermore, both plasma IL-17 levels on the initial day and median
levels of IL-17 on day 7 were strongly associated with PC volume.
The results indicated that IL-17 was a biomarker for predicting the
severity of PC. Dai et al (27) found that cytokines (IL-17) and an
imbalance of Treg/Th17 were significantly relevant to tissue (lung
and intestine) inflammation and injury in the acute phase (within 8
h) after multiple traumas. This group also found that IL-17 was
crucially involved in the pathogenesis of multiple traumas in rats,
and IL-17 inhibition might ameliorate lung inflammation in the
acute phase after multiple traumas (8). The potential explanation was that IL-17
might induce production of other pro-inflammatory cytokines and
increase the uncontrolled inflammatory response induced by
high-energy traumas, which may be the primary cause of lung
impairment.
Given that PC volume was effective in predicting the
outcomes of PC patients and that IL-17 had a strong relationship
with PC volume, whether IL-17 could be used as a biomarker to
predict in-patient outcomes of patients with PC was next assessed.
High levels of plasma IL-17 were associated with a high occurrence
ratio of PC. Furthermore, patients with a high level of plasma
IL-17 suffered a more serious trauma and were more vulnerable to
developing ARDS. Using ROC analysis to calculate the predictive
value of IL-17 for the in-patient outcomes showed that the levels
of plasma IL-17 were useful for predicting the occurrence of ARDS,
mechanical ventilation, ICU admission and mortality. These results
suggest that IL-17 was significantly associated with
pro-inflammatory complications in serious trauma patients and could
be used as a biomarker to predict in-patient outcomes of patients
with PC. However, whether increased levels of IL-17 was due to
polytrauma or the PC was not determined. However, PC seemed to
increase the levels of IL-17. To the best of our knowledge, this is
the first time that IL-17 has been associated with the severity of
PC and the outcomes of PC patients, though the underlying
mechanisms require further clarification.
IL-22 is a homeostatic cytokine with pronounced
tissue-protective properties (10).
It was found to preserve the integrity of boundary organs and
tissues (28), and serves an
important role in the resolution of sterile and nonsterile
inflammation, organ injury, wound healing and regeneration
(29,30). IL-22 is also associated with burn
injuries and sepsis (14,15). In the present study, IL-22 increased
significantly following PC and peaked on day 5 after PC diagnosis.
However, there was no association between IL-22 and PC outcomes. A
potential explanation for this is that IL-22 may not be a specific
cytokine for PC during multiple traumas. It may be secreted at
various sites during serious trauma. This is different from lung
injuries which are induced by burns or infection (14,15).
Further studies are required to determine the specific role of
IL-22 in multiple traumas.
In summary, the present study showed that PC volume
was effective in predicting the outcomes of PC patients. IL-17
could be used as a biomarker to predict the severity of PC and was
strongly associated with PC volume. IL-17 was significantly
associated with pro-inflammatory complications in PC patients and
could be used as a biomarker to predict outcomes of PC in-patients.
IL-17 is thus a potential biomarker for predicting the severity and
outcomes of PC in trauma patients. However, whether elevated plasma
IL-17 concentrations can be used as a marker of other processes of
post-trauma, and whether it is a causal factor for PC remains
unknown. Further studies are thus required to explore the
mechanisms.
Acknowledgements
Not applicable.
Funding
This work was supported by Talents Sub-Highland of
Emergency and Medical Rescue of Guangxi Province in China (grant
no. GXJZ201405), Health Commission of Guangxi (grant no. Z2016289),
the Young Teachers' Basic Ability Improvement in Guangxi University
Project (grant no. 2019KY0108) and the Medical Excellence Award
funded by the Creative Research Development Grant from the First
Affiliated Hospital of Guangxi Medical University.
Availability of data and materials
All data generated and/or analyzed during the
present study are included in this published article. Raw data is
available from the corresponding authors upon reasonable request
and with the permission of the First Affiliated Hospital of Guangxi
Medical University.
Authors' contributions
SL analyzed the clinical data, performed the
experiments and wrote the original draft. QQ, DL, WP, YW and YX
collected the patient samples and revised the manuscript. JW and XY
collected the clinical data. JZ and LS designed the study, and
reviewed and edited the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from each
participant prior to enrolment, and this study was approved by the
Medical Ethics Committee of The First Affiliated Hospital of
Guangxi Medical University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cohn SM and Dubose JJ: Pulmonary
contusion: An update on recent advances in clinical management.
World J Surg. 34:1959–1970. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ganie FA, Lone H, Lone GN, Wani ML, Singh
S, Dar AM, Wani NU, Wani SN and Nazeer NU: Lung contusion: A
clinico-pathological entity with unpredictable clinical course.
Bull Emerg Trauma. 1:7–16. 2013.PubMed/NCBI
|
|
3
|
Rodriguez RM, Friedman B, Langdorf MI,
Baumann BM, Nishijima DK, Hendey GW, Medak AJ, Raja AS and Mower
WR: Pulmonary contusion in the pan-scan era. Injury. 47:1031–1034.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Prunet B, Bourenne J, David JS, Bouzat P,
Boutonnet M, Cordier PY, Renaudin P, Meaudre E and Michelet P:
Patterns of invasive mechanical ventilation in patients with severe
blunt chest trauma and lung contusion: A French multicentric
evaluation of practices. J Intensive Care Soc. 20:46–52.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Valeri M and Raffatellu M: Cytokines IL-17
and IL-22 in the host response to infection. Pathog Dis.
74(ftw111)2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Becker KL, Snider R and Nylen ES:
Procalcitonin assay in systemic inflammation, infection, and
sepsis: Clinical utility and limitations. Crit Care Med.
36:941–952. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ahmed Ali M, Mikhael ES, Abdelkader A,
Mansour L, El Essawy R, El Sayed R, Eladawy A and Mukhtar A:
Interleukin-17 as a predictor of sepsis in polytrauma patients: A
prospective cohort study. Eur J Trauma Emerg Surg. 44:621–626.
2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Dai H, Xu L, Tang Y, Liu Z and Sun T:
Treatment with a neutralising anti-rat interleukin-17 antibody
after multiple-trauma reduces lung inflammation. Injury.
46:1465–1470. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mizoguchi A, Yano A, Himuro H, Ezaki Y,
Sadanaga T and Mizoguchi E: Clinical importance of IL-22 cascade in
IBD. J Gastroenterol. 53:465–474. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mühl H, Scheiermann P, Bachmann M, Härdle
L, Heinrichs A and Pfeilschifter J: IL-22 in tissue-protective
therapy. Br J Pharmacol. 169:761–771. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Alcorn JF: IL-22 plays a critical role in
maintaining epithelial integrity during pulmonary infection. Front
Immunol. 11(1160)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hoegl S, Bachmann M, Scheiermann P, Goren
I, Hofstetter C, Pfeilschifter J, Zwissler B and Muhl H: Protective
properties of inhaled IL-22 in a model of ventilator-induced lung
injury. Am J Respir Cell Mol Biol. 44:369–376. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
McAleer JP and Kolls JK: Directing
traffic: IL-17 and IL-22 coordinate pulmonary immune defense.
Immunol Rev. 260:129–144. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rendon JL and Choudhry MA: Th17 cells:
Critical mediators of host responses to burn injury and sepsis. J
Leukoc Biol. 92:529–538. 2012.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Li G, Zhang L, Han N, Zhang K and Li H:
Increased Th17 and Th22 cell percentages predict acute lung injury
in patients with sepsis. Lung. 198:687–693. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Baker SP, O'Neill B, Haddon W Jr and Long
WB: The injury severity score: A method for describing patients
with multiple injuries and evaluating emergency care. J Trauma.
14:187–196. 1974.PubMed/NCBI
|
|
17
|
Mahmood I, El-Menyar A, Younis B, Ahmed K,
Nabir S, Ahmed MN, Al-Yahri O, Mahmood S, Consunji R and Al-Thani
H: Clinical significance and prognostic implications of quantifying
pulmonary contusion volume in patients with blunt chest trauma. Med
Sci Monit. 23:3641–3648. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tufman A, Huber RM, Völk S, Aigner F,
Edelmann M, Gamarra F, Kiefl R, Kahnert K, Tian F, Boulesteix AL,
et al: Interleukin-22 is elevated in lavage from patients with lung
cancer and other pulmonary diseases. BMC Cancer.
16(409)2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Abboud A, Namas RA, Ramadan M, Mi Q,
Almahmoud K, Abdul-Malak O, Azhar N, Zaaqoq A, Namas R, Barclay DA,
et al: Computational analysis supports an early, type 17
cell-associated divergence of blunt trauma survival and mortality.
Crit Care Med. 44:e1074–e1081. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Pehlivanlar Küçük M, Küçük AO, Aksoy İ,
Aydın D and Ülger F: Prognostic evaluation of cases with thoracic
trauma admitted to the intensive care unit: 10-year clinical
outcomes. Ulus Travma Acil Cerrahi Derg. 25:46–54. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Požgain Z, Kristek D, Lovrić I, Kondža G,
Jelavić M, Kocur J and Danilović M: Pulmonary contusions after
blunt chest trauma: Clinical significance and evaluation of patient
management. Eur J Trauma Emerg Surg. 44:773–777. 2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Miller C, Stolarski A, Ata A, Pfaff A,
Nadendla P, Owens K, Evans L, Bonville D, Rosati C, Stain SC and
Tafen M: Impact of blunt pulmonary contusion in polytrauma patients
with rib fractures. Am J Surg. 218:51–55. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Flores-Funes D, Lluna-Llorens AD,
Jiménez-Ballester MÁ, Valero-Navarro G, Carrillo-Alcaráz A,
Campillo-Soto Á and Aguayo-Albasini JL: Is the number of rib
fractures a risk factor for delayed complications? A case-control
study. Eur J Trauma Emerg Surg. 46:435–440. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Dominguez-Villar M and Hafler DA:
Immunology. An innate role for IL-17. Science. 332:47–48.
2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Schwarzenberger P, Huang W, Ye P, Oliver
P, Manuel M, Zhang Z, Bagby G, Nelson S and Kolls JK: Requirement
of endogenous stem cell factor and granulocyte-colony-stimulating
factor for IL-17-mediated granulopoiesis. J Immunol. 164:4783–4789.
2000.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Frangen TM, Bogdanski D, Schinkel C,
Roetman B, Kälicke T, Muhr G and Köller M: Systemic IL-17 after
severe injuries. Shock. 29:462–467. 2008.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dai H, Sun T, Liu Z, Zhang J and Zhou M:
The imbalance between regulatory and IL-17-secreting
CD4+ T cells in multiple-trauma rat. Injury.
44:1521–1527. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Eyerich K, Dimartino V and Cavani A: IL-17
and IL-22 in immunity: Driving protection and pathology. Eur J
Immunol. 47:607–614. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Alabbas SY, Begun J, Florin TH and Oancea
I: The role of IL-22 in the resolution of sterile and nonsterile
inflammation. Clin Transl Immunology. 7(e1017)2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Brockmann L, Giannou AD, Gagliani N and
Huber S: Regulation of TH17 cells and associated cytokines in wound
healing, tissue regeneration, and carcinogenesis. Int J Mol Sci.
18(1033)2017.PubMed/NCBI View Article : Google Scholar
|