Introduction
Chronic pancreatitis (CP) is a type of pathologic
fibro-inflammatory syndrome of the exocrine pancreas, with genetic,
environmental and/or other risk factors, and patients develop
persistent responses to parenchymal injury and stress (1). In ~70% of tumors of the pancreas, the
tumor is primarily located within the head of the pancreas
(2), and ~5% of patients with CP
develop pancreatic cancer over the following 20 years (3). Pancreatic ductal adenocarcinoma (PDAC)
is a common type of cancer of the pancreas with a high mortality
rate, but does not have clearly defined symptoms (4). In >50% of pancreatic cancer cases,
patients are diagnosed with advanced stage cancer, which has the
lowest 5-year relative survival rate (9% for all stages) amongst
all types of cancer (5). In ~90% of
patients with PDAC, the development of the cancer is sporadic,
whereas in the other 10% of cases, there is a hereditary element
(6). Only 15% of patients with PDAC
are diagnosed at an early stage with an indication for surgical
treatment, and at present, this is the only established curative
means.
The majority of studies focused on differentiating
between CP and PDAC primarily include evaluation of basic
parameters, such as imaging, and clinical and biochemical markers.
Carbohydrate antigen 19-9 (CA 19-9) is the most widely used
biomarker for the diagnosis of pancreatic cancer in symptomatic
patients (7). Unfortunately, it is
not specific for this pathology, as CA 19-9 concentration in the
blood may increase in other diseases, such as cirrhosis of the
liver, cholangitis, CP and other tumors of the gastrointestinal
tract (8). In addition, 5-10% of the
population with a rare Lewis antigen system do not synthesize CA
19-9(7). Patients with elevated
levels of CA 19-9 are subjected to abdominal ultrasonography (US),
computed tomography (CT), magnetic resonance imaging (MRI) or
endoscopic ultrasound-guided fine-needle aspiration biopsy. The
research is performed with the hope that it will allow for
distinguishing between benign and neoplastic lesions, but these
techniques do not always precisely define the type of pathology and
are most often performed too late, and thus only confirm the fatal
diagnosis (9). In addition, the
symptoms of PDAC and CP are similar: Pain in the upper abdomen,
weight loss, nausea and occasionally, jaundice. Both groups of
patients often have a history of smoking and alcohol abuse. Novel
diagnostic tests are necessary to differentiate PDAC from CP from
which surgical and radical interventions, including
pancreatoduodenectomy, can be avoided if not needed, as such
treatments are associated with a large number of severe
complications (10,11).
To the best of our knowledge, there are no studies
which have identified non-invasive methods for distinguishing CP
from PDAC. Promising molecular candidates include short, non-coding
RNAs, such as microRNAs (miRs/miRNAs), which are involved in
regulation of key processes in all types of living cells, including
cellular differentiation, apoptosis and growth (9). MiRNA expression profiles are
tissue-specific, and aberrant miRNA expression can be indicative of
pathologies such as inflammation or cancer (12). Based on the literature search
performed for this study, four miRNAs: miR-10b-5p, miR-106b-5p,
miR-210-3p and miR-216a-5p were selected, and their expression in
the blood collected from patients with suspected CP and PDAC were
compared to allow distinguishment between these two types of
pathologies (13-17).
Materials and methods
Patients
A total of 77 patients were enrolled in the present
study at the Department and Clinic of Gastroenterology with
Endoscopic Unit, Medical University of Lublin. The study conformed
with the principles outlined in the Declaration of Helsinki
(18) and was approved by the
Research Ethics Committee of the Medical University of Lublin
(approval no. KE 0254-/54/2015). All participants provided written
informed consent prior to enrolment in the study. The patients were
divided into three groups: Group I consisted of 26 patients (17
males and 9 females; age range, 47-89, median age 58 years old) who
were diagnosed with PDAC without a history of CP; Group II
consisted of 34 patients with CP (27 males and 7 females; age
range, 21-78, median age 39.5 years old); and Group III which
consisted of 17 healthy patients (13 males, 4 females; age range,
22-50, median age 34 years old) and served as a control group
according to imaging tests (CT, US) that excluded the presence of
PDAC and CP, as well as any other acute and chronic inflammation
illnesses, verified by serum C-reactive protein (CRP) concentration
measurement. The patients' characteristics are presented in
Table I.
 | Table IClinicopathological characteristics of
the recruited patients. |
Table I
Clinicopathological characteristics of
the recruited patients.
| Clinicopathological
characteristic | Chronic pancreatitis
group | Pancreatic ductal
adenocarcinoma group | Control group | P-value |
|---|
| Sex, n
(%)c |
|
Female | 7 (20.59) | 9 (34.61) | 4 (23.53) | 0.455 |
|
Male | 27 (79.41) | 17 (65.38) | 13 (76.47) | |
| Median age, years
(range)d | 39.5 (21-78) | 58.0 (47-89) | 34.0 (22-50) | 0.001b |
| Smoking status, n
(%)a |
|
Smokers | 30 (88.23) | 20 (76.92) | 9 (52.94) | 0.019a |
|
Non-smokers | 4 (11.76) | 6 (23.08) | 8 (47.06) | |
| History of alcohol
abuse, n (%)c | 31 (91.18) | 17 (65.38) | 5 (29.41) | 0.001b |
| Diabetes n
(%)c | 14 (41.18) | 6 (23.08) | 2 (11.76) | 0.068 |
| Stage, n (%) |
|
Early
stage | - | 4 (15.38) | - | - |
|
Locally
advanced stage | - | 12 (46.15) | - | - |
|
Advanced
stage | - | 10 (38.46) | - | - |
Blood sample collection
For routine blood sample analysis, ~5 ml of venous
blood was collected into biochemical tubes without anticoagulant.
After the blood had clotted, it was centrifuged at 2,500 x g for 10
min at 4˚C twice to remove insoluble residues, then the supernatant
was aliquoted in RNase-free tubes and stored at -80˚C until
required for RNA isolation. The activity of lipase, amylase,
alanine aminotransferase, aspartate aminotransferase, alkaline
phosphatase (ALP), γ-glutamyltranspeptidase (GGTP), as well as
hemoglobin (Hb), bilirubin, CRP and CA19-9 levels were determined
by routine laboratory methods in The Central Laboratory
(Independent Public Clinical Hospital No. 4, Lublin, Poland).
RNA isolation and cDNA synthesis
Total RNA, including miRNAs was isolated from serum
using a miRCURY RNA Isolation kit according to the manufacturer's
protocol (Biofluids; Exiqon; Qiagen, AB). Spike-ins UniSp 2, UniSp
4 and UniSp 5 were mixed with MS2 bacteriophage RNA (Roche
Diagnostics) and were added to each sample to monitor RNA
isolation. After optimization, the cDNA was synthesized from 4 µl
isolated RNA using a Universal cDNA Synthesis kit II according to
the manufacturer's protocol (Exiqon; Qiagen, AB). Moreover, UniSp6
was used to monitor the quality of the reverse transcription
reaction. For the negative controls, three reactions were prepared
using the following reaction mixtures-without reverse
transcriptase, without RNA template and using MS2 bacteriophage RNA
as template.
Quantitative (q)PCR
Each cDNA sample was diluted with nuclease-free
water and 4 µl cDNA was mixed with 5 µl SYBR-Green MasterMix
(Exiqon; Qiagen, AB), and 1 µl LNA™ primers (Exiqon;
Qiagen, AB). The final volume of the reaction mixture was 10 µl and
each reaction was carried out in triplicate. Amplification with
real-time fluorescence detection was performed using a
LightCycler® 480 II instrument (Roche Applied Science)
as follows; Initial denaturation, 10 min at 95˚C; followed by 45
cycles of 10 sec at 95˚C and 1 min at 60˚C. The degree of hemolysis
of serum samples was evaluated using primers for miR-23a-3p and
miR-451a. Differences between the miR-23a-3p and miR-451a Cp values
<5 were considered hemolysis-free and such serum samples were
further analyzed.
In accordance with recommendations from Exiqon,
miR-30c, miR-103a-3p, miR-124-3p, miR-191-5p and miR-423-3p were
considered as potential reference genes, amongst which, miR-103a-3p
was selected for further analysis as it had the lowest degree of
variation between analyzed groups (P>0.05). The relative
expression of miRNAs was calculated using efficiency method with
the LightCycler® 480 SW version 1.5 software (Roche
Diagnostics) according to Roche Operator's manual.
The sequences of the microRNA LNA™
primers (Exiqon; Qiagen, AB) used in the present study are:
hsa-miR-30c-5p, UGUAAACAUCCUACACUCUCAGC; hsa-miR-103a-3p,
AGCAGCAUUGUACAGGGCUAUGA; hsa-miR-124-3p, UAAGGCACGCGGUGAAUGCC;
hsa-miR-191-5p, CAACGGAAUCCCAAAAGCAGCUG; and hsa-miR-423-3p,
AGCUCGGUCUGAGGCCCCUCAGU. For evaluation of the level of hemolysis
target miRNA sequences were: miR-23a-3p, AUCACAUUGCCAGGGAUUUCC; and
hsa-miR-451a, AAACCGUUACCAUUACUGAGUU. Target miRNA sequences for
potential miRNA biomarkers in differentiation of PDAC from CP were:
hsa-miR-10b-5p, UACCCUGUAGAACCGAAUUUGUG; hsa-miR-106b-5p,
UAAAGUGCUGACAGUGCAGAU; hsa-miR-210-3p, CUGUGCGUGUGACAGCGGCUGA; and
hsa-miR-216a-5p, UAAUCUCAGCUGGCAACUGUGA. Spike-in target sequences
used for RNA isolation control were: UniSp2, GUACUCGGCUUACGAUCGUAA;
UniSp 4, GAUGGCAUUCGAUCAGUUCUA; and UniSp 5,
GAUGCUACGGUCAAUGUCUAAG; for cDNA synthesis control, the UniSp 6
target sequence was CUAGUCCGAUCUAAGUCUUCGA.
Statistical analysis
Normality of distribution of miRNA expression was
assessed using histograms and a Kolmogorov-Smirnov or Shapiro-Wilk
tests. Since the distribution was not normal, differences in miRNA
expression amongst the three groups (CP, PDAC and the control
group) were analyzed using the non-parametric Kruskal-Wallis ANOVA
by ranks and Mann Whitney U tests. Correlations between variables
were analyzed using a Spearman-rank correlation coefficient test.
Differences in frequencies were compared using a χ2
test. P<0.05 was considered to indicate a statistically
significant difference. Statistical analysis was performed using
Statistica, version 13.3 (TIBCO Software Inc.).
Results
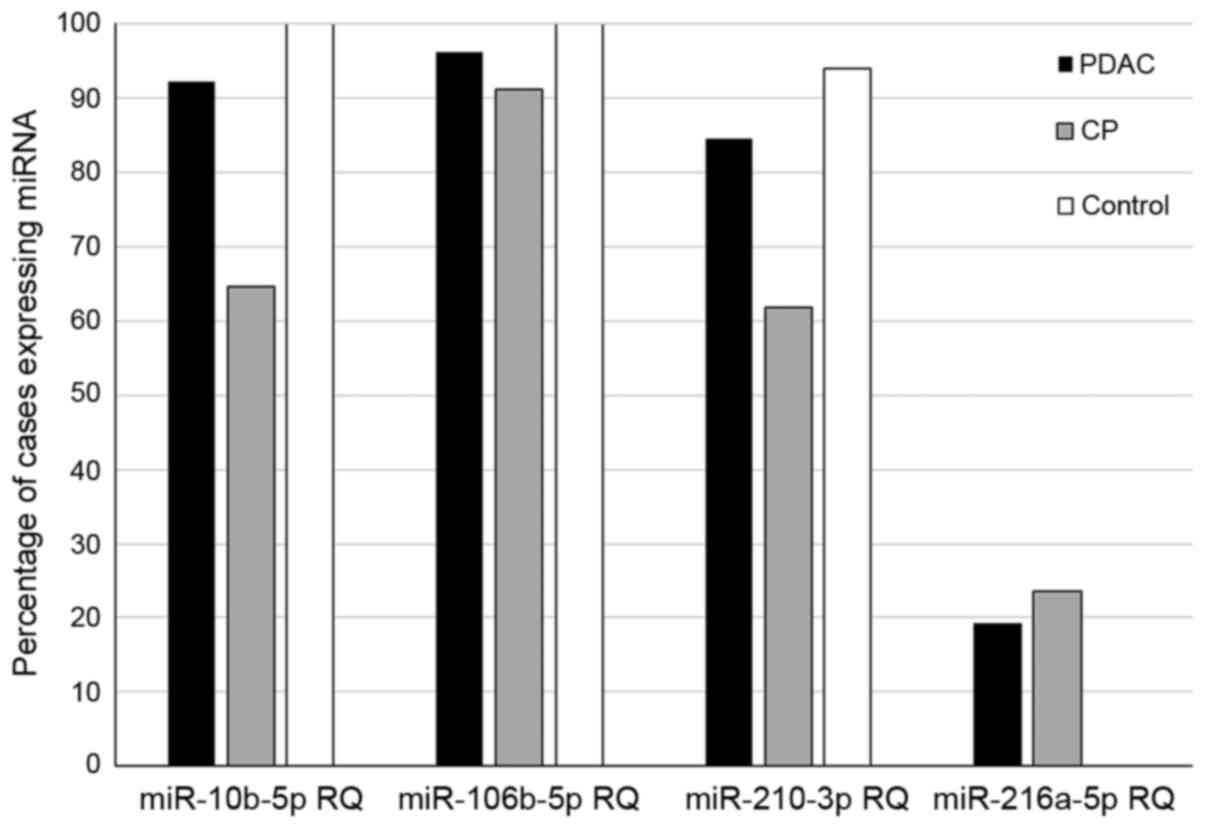
Expression of miR-10b-5p was observed in 24/26
patients with PDAC (92.3%), 22/34 patients with CP (64.7%) and in
17/17 individuals in the control group (100%). Expression of
miR-106b-5p was observed in 25/26 patients with PDAC (96.1%), 31/34
patients with CP (91.7%), and in 17/17 individuals in the control
group (100%). Expression of miR-210-3p was observed in 22/26
patients with PDAC (84.6%), 21/34 patients with CP (61.8%), and
16/17 patients in the control group (94.1%). Expression of
miR-216a-5p was observed in only two of the groups; in 5/26
patients with PDAC (19.2%) and in 8/34 patients with CP (20.6%).
The percentage of samples expressing each miRNA assessed is shown
in Fig. 1.
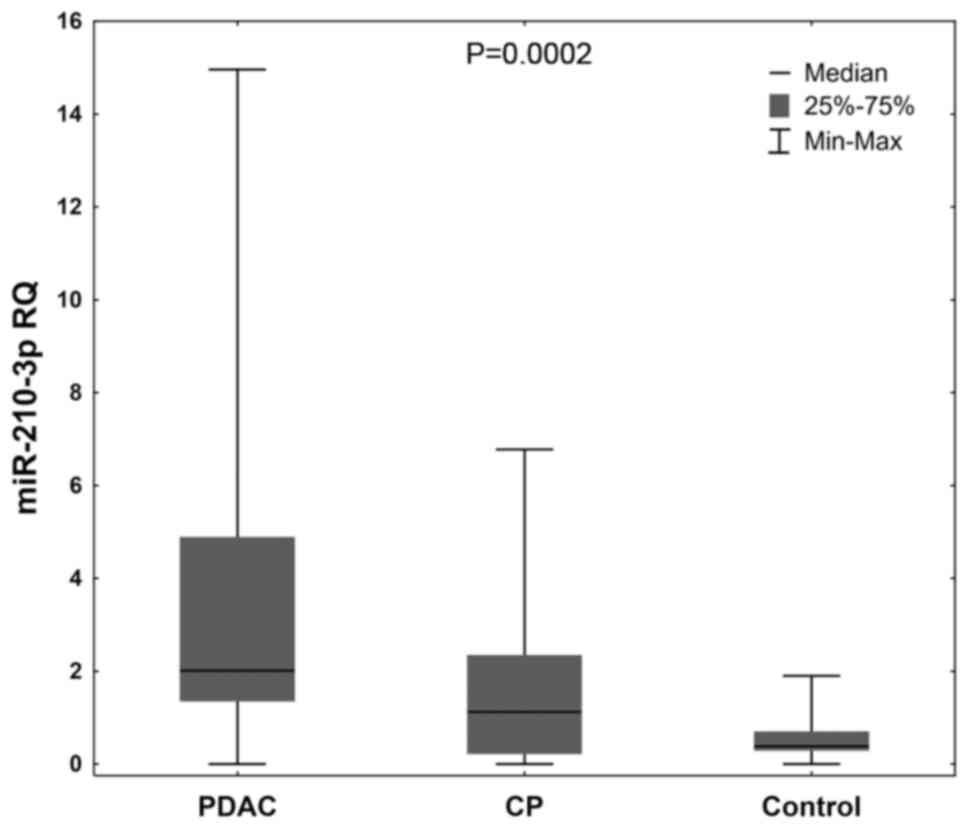
Serum miRNA levels were compared in the patients
with CP, PDAC and the control group. Significantly higher
expression levels of miR-210-3p were observed in the patients with
CP and PDAC compared with the control group (P=0.0002; Fig. 2).
Comparative analysis showed significantly higher
expression levels of miR-210-3p in the patients with PDAC compared
with the patients with CP (P=0.015), whereas expression of
miR-106b-5p and miR-10b-5p tended to be higher in the patients with
PDAC compared with those with CP, although the difference was not
significant (P=0.056 and P=0.080, respectively). When analyzing
miRNA expression in the PDAC group in comparison with the control
group, only miR-210-3p expression in PDAC patients was
significantly increased (P<0.001), and additionally its
expression was correlated with ALP activity (r=0.605, P=0.022), as
well as with GGTP activity (r=0.529, P=0.029).
Of minor clinical importance there was a
statistically significant correlation between miR-10b-5p and the
concentration of CRP (r=0.429, P=0.047) in the PDAC group, and with
CA 19-9 content (r=0.483, P=0.005) in the CP group. All four
statistically significant correlations between expression of miRNA
and basic clinical parameters in PDAC and CP are shown in Table II. There were no other statistically
significant correlations identified (P>0.05). Inter-correlations
between selected miRNAs within analyzed patient groups were also
identified, but they were not statistically significant (data not
shown).
Discussion
CP and PDAC are diseases with several similar
symptoms. There is an inherent problem of distinguishing
inflammation within the pancreas from neoplastic lesions, augmented
by the lack of non-invasive diagnostic methods. Often, surgical
interventions turn out to be an unnecessary risk that endangers a
patient's health, therefore, discovery of blood-based markers is
urgently required, which, together with determination of
conventional clinical parameters, can enable a physician to
distinguish between CP and PDAC. Complex networks formed by miRNAs
regulate cellular development, differentiation and homeostasis
(19). Alterations in the expression
of miRNAs are associated with the number of diseases, including
inflammatory diseases and cancer (20). In order to search for serum miRNAs
that can be used to differentiate between CP and PDAC, candidate
miRNAs associated with cancer and the inflammatory process were
assessed; specifically miR-10b-5p, miR-106b-5p, miR-210-3p and
miR-216a-5p, all of which have been previously found to be
significantly upregulated in PDAC (13,14,21,22).
Amongst the selected miRNAs, miR-210-3p was deemed to be the most
promising as a serum biomarker for use in differentiation between
CP and PDAC, as its expression was higher in the patients with PDAC
compared with those with CP, and miR-106b-5p expression tended to
be higher in patients with PDAC than those with CP. Studies using
larger cohorts are thus required to determine/confirm the
reliability of these miRs as markers to use to differentiate
between these two pathologies. In ~70% of cases of pancreatic
cancer, the cancer is located within the pancreatic head and the
majority of patients develop obstructive cholestasis resulting in
increased ALP and GGTP serum levels (23). Significant positive correlations were
identified between the expression of miR-210-3p and the activities
of the cholestasis-related enzymes ALP and GGTP in patients with
PDAC. This suggests that combined assessment of these parameters
(miR-210-3p levels and ALP/GGTP activity) may improve the accuracy
of early diagnosis and may provide a non-invasive diagnostic tool
for distinguishing between PDAC CP in the future. There was a
significant correlation between miR-10b-5p and CRP levels and CA
19-9 content. To date, there are no studies that have shown an
association between expression of miR-10b-5p and CP, to the best of
our knowledge. The role of miR-10b-5p in the course of
carcinogenesis has already been described (24). Moreover, recently published data has
shown that miR-10b may serve as a candidate predictive marker, as
its expression is associated with significantly improved overall
survival (~2 months) in PDAC patients treated with a combination of
gemcitabine and Galunisertib (a transforming growth factor β
receptor I inhibitor) (25,26).
The majority of published studies have focused on
comparative analysis of miR-210 expression in the serum, tissue
specimen or pancreatic juice of patients with PDAC in relation to
individuals with non-pancreatic diseases or healthy subjects
(27-29).
In the present study, significantly higher levels of miR-210-3p
were observed in the sera of patients with PDAC compared with the
healthy individuals, which confirms reports on the involvement of
miR-210 in the regulation of expression of a number of genes
associated with malignant transformation. The oncogenic effects of
miR-210 have been described in pancreatic, prostate, ovary,
bladder, breast and bone cancer (15,28,30-33).
Development of hypoxia in the most common pancreatic cancer,
adenocarcinoma, results in a poor response to radiotherapy and
chemotherapy (34). A state of
oxygen deficiency in tissues induces the expression of specific
miRNAs, including miR-210-3p, which is termed hypoxamiR (16,35).
Genes regulated by miR-210 are involved in cell division and
migration, angiogenesis, mitochondrial metabolism, DNA repair or
chromatin remodeling (36-38).
Anaerobic environments stimulate activation of pancreatic stellate
cells, angiogenesis and fibrosis (39-42).
Angiogenesis underlies the repair process that is observed in the
course of CP, and is a mechanism that also enables the development
and growth of cancer (43).
Upregulated expression of miR-210-3p expression in cells is
reflected by its high levels in the blood (28); experimentally confirmed higher serum
levels in patients with PDAC indicate higher expression of this
miRNA in the cells where the aforementioned molecular changes may
have occurred.
Limitations of the present study include the
variance in sample sizes and a relatively low number of enrolled
participants, and thus, the results of the present pilot study
should be validated using larger cohorts.
In conclusion, the role of miRNAs in the
pathogenesis of CP and PDAC highlights their potential use as
non-invasive markers for detection and diagnosis of these diseases.
It is hypothesized that miR-210-3p may be a useful biomarker for
differentiation between these two pancreatic diseases.
Additionally, the correlation between miR-210-3p with biochemical
parameters, such as the activity of GGTP and ALP, enhances its
prognostic value.
Acknowledgements
We would like to thank Ms. Agnieszka Styczyńska
(Department of Biochemistry and Molecular Biology at the Medical
University of Lublin) for editorial assistance and for proofreading
the manuscript.
Funding
This work was supported by The Polish Ministry of
Science and Higher Education Grant (grant no. MNmb 401).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
AM, MG and JKu designed, planned and supervised the
study. MG and AM wrote and revised the manuscript. MG and WJ
performed the experiments. MC performed the statistical analysis.
MG, WJ and MC interpreted the results. Samples and clinical data
were collected by JKo. All authors read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Research
Ethics Committee of the Medical University of Lublin (approval no.
KE 0254-/54/2015).
Patients consent for publication
All participants provided written informed consent
prior to enrolment in the study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Whitcomb DC, Frulloni L, Garg P, Greer JB,
Schneider A, Yadav D and Shimosegawa T: Chronic pancreatitis: An
international draft consensus proposal for a new mechanistic
definition. Pancreatology. 16:218–224. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ansari D, Tingstedt B, Andersson B,
Holmquist F, Sturesson C, Williamsson C, Sasor A, Borg D, Bauden M
and Andersson R: Pancreatic cancer: Yesterday, today and tomorrow.
Futur Oncol. 12:1929–1946. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Raimondi S, Lowenfels AB, Morselli-Labate
AM, Maisonneuve P and Pezzilli R: Pancreatic cancer in chronic
pancreatitis; aetiology, incidence, and early detection. Best Pract
Res Clin Gastroenterol. 24:349–358. 2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wu DJ, Jiang YS, He RZ, Tao LY, Yang MW,
Fu XL, Yang JY and Zhu K: High expression of WNT7A predicts poor
prognosis and promote tumor metastasis in pancreatic ductal
adenocarcinoma. Sci Rep. 8(15792)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2019. CA Cancer J Clin. 69:7–34. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Becker AE, Hernandez YG, Frucht H and
Lucas AL: Pancreatic ductal adenocarcinoma: Risk factors,
screening, and early detection. World J Gastroenterol.
20:11182–11198. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ballehaninna UK and Chamberlain RS: The
clinical utility of serum CA 19-9 in the diagnosis, prognosis and
management of pancreatic adenocarcinoma: An evidence based
appraisal. J Gastrointest Oncol. 3:105–119. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Duffy MJ, Sturgeon C, Lamerz R, Haglund C,
Holubec VL, Klapdor R, Nicolini A, Topolcan O and Heinemann V:
Tumor markers in pancreatic cancer: A European group on tumor
markers (EGTM) status report. Ann Oncol. 21:441–447.
2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Halkova T, Cuperkova R, Minarik M and
Benesova L: MicroRNAs in pancreatic cancer: Involvement in
carcinogenesis and potential use for diagnosis and prognosis.
Gastroenterol Res Pract. 2015(892903)2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Smith CD, Behrns KE, Van Heerden JA and
Sarr MG: Radical pancreatoduodenectomy for misdiagnosed pancreatic
mass. Br J Surg. 81:585–589. 1994.PubMed/NCBI View Article : Google Scholar
|
|
11
|
van Gulik TM, Reeders JW, Bosma A, Moojen
TM, Smits NJ, Allema JH, Rauws EA, Offerhaus GJ, Obertop H and
Gouma DJ: Incidence and clinical findings of benign, inflammatory
disease in patients resected for presumed pancreatic head cancer.
Gastrointest Endosc. 46:417–423. 1997.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Nana-Sinkam SP, Fabbri M and Croce CM:
MicroRNAs in cancer: Personalizing diagnosis and therapy. Ann N Y
Acad Sci. 1210:25–33. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sheedy P and Medarova Z: The fundamental
role of miR-10b in metastatic cancer. Am J Cancer Res. 8:1674–1688.
2018.PubMed/NCBI
|
|
14
|
Yonemori K, Seki N, Idichi T, Kurahara H,
Osako Y, Koshizuka K, Arai T, Okato A, Kita Y, Arigami T, et al:
The microRNA expression signature of pancreatic ductal
adenocarcinoma by RNA sequencing: Anti-tumour functions of the
microRNA-216 cluster. Oncotarget. 8:70097–70115. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ding L, Zhao L, Chen W, Liu T, Li Z and Li
X: miR-210, a modulator of hypoxia-induced epithelial-mesenchymal
transition in ovarian cancer cell. Int J Clin Exp Med. 8:2299–2307.
2015.PubMed/NCBI
|
|
16
|
Dang K and Myers KA: The role of
hypoxia-induced miR-210 in cancer progression. Int J Mol Sci.
16:6353–6372. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kaur S, Krishn SR, Rachagani S and Batra
SK: Significance of microRNA-based biomarkers for pancreatic
cancer. Ann Transl Med. 3(277)2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
World Medical Association. Declaration of
Helsinki world medical association declaration of Helsinki. Ethical
principles for medical research involving human subjects. Bull
World Health Organ. 79:373–374. 2001.PubMed/NCBI
|
|
19
|
Gebert LFR and MacRae IJ: Regulation of
microRNA function in animals. Nat Rev Mol Cell Biol. 20:21–37.
2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Raisch J, Darfeuille-Michaud A and Nguyen
HT: Role of microRNAs in the immune system, inflammation and
cancer. World J Gastroenterol. 19:2985–2996. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Li Y and Sarkar FH: MicroRNA targeted
therapeutic approach for pancreatic cancer. Int J Biol Sci.
12:326–337. 2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Vila-Casadesús M, Vila-Navarro E, Raimondi
G, Fillat C, Castells A, Lozano JJ and Gironella M: Deciphering
microRNA targets in pancreatic cancer using miRComb R package.
Oncotarget. 9:6499–6517. 2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Vogel A, Kullmann F, Kunzmann V, Al-Batran
SE, Oettle H, Plentz R, Siveke J, Springfeld C and Riess H:
Patients with advanced pancreatic cancer and hyperbilirubinaemia:
Review and German expert opinion on treatment with nab-paclitaxel
plus gemcitabine. Oncol Res Treat. 38:596–603. 2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Ouyang H, Gore J, Deitz S and Korc M:
microRNA-10b enhances pancreatic cancer cell invasion by
suppressing TIP30 expression and promoting EGF and TGF-β actions.
Oncogene. 33:4664–4674. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Melisi D, Garcia-Carbonero R, Macarulla T,
Pezet D, Deplanque G, Fuchs M, Trojan J, Kozloff M, Simionato F,
Cleverly A, et al: TGFβ receptor inhibitor galunisertib is linked
to inflammation- and remodeling-related proteins in patients with
pancreatic cancer. Cancer Chemother Pharmacol. 83:975–991.
2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Melisi D, Garcia-Carbonero R, Macarulla T,
Pezet D, Deplanque G, Fuchs M, Trojan J, Oettle H, Kozloff M,
Cleverly A, et al: Galunisertib plus gemcitabine vs. gemcitabine
for first-line treatment of patients with unresectable pancreatic
cancer. Br J Cancer. 119:1208–1214. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wang J, Raimondo M, Guha S, Chen J, Diao
L, Dong X, Wallace MB, Killary AM, Frazier ML, Woodward TA, et al:
Circulating microRNAs in pancreatic juice as candidate biomarkers
of pancreatic cancer. J Cancer. 5:696–705. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ho AS, Huang X, Cao H, Christman-Skieller
C, Bennewith K, Le QT and Koong AC: Circulating miR-210 as a novel
hypoxia marker in pancreatic cancer. Transl Oncol. 3:109–113.
2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Calatayud D, Dehlendorff C, Boisen MK,
Hasselby JP, Schultz NA, Werner J, Immervoll H, Molven A, Hansen CP
and Johansen JS: Tissue MicroRNA profiles as diagnostic and
prognostic biomarkers in patients with resectable pancreatic ductal
adenocarcinoma and periampullary cancers. Biomark Res.
5(8)2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Cheng HH, Mitchell PS, Kroh EM, Dowell AE,
Chéry L, Siddiqui J, Nelson PS, Vessella RL, Knudsen BS, Chinnaiyan
AM, et al: Circulating microRNA profiling identifies a subset of
metastatic prostate cancer patients with evidence of
cancer-associated hypoxia. PLoS One. 8(e69239)2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Irlam-Jones JJ, Eustace A, Denley H,
Choudhury A, Harris AL, Hoskin PJ and West CL: Expression of
miR-210 in relation to other measures of hypoxia and prediction of
benefit from hypoxia modification in patients with bladder cancer.
Br J Cancer. 115:571–578. 2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhang H, Mai Q and Chen J: MicroRNA-210 is
increased and it is required for dedifferentiation of osteosarcoma
cell line. Cell Biol Int. 41:267–275. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Foekens JA, Sieuwerts AM, Smid M, Look MP,
de Weerd V, Boersma AW, Klijn JG, Wiemer EA and Martens JW: Four
miRNAs associated with aggressiveness of lymph node-negative,
estrogen receptor-positive human breast cancer. Proc Natl Acad Sci
USA. 105:13021–13026. 2008.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Koong AC, Mehta VK, Le QT, Fisher GA,
Terris DJ, Brown JM, Bastidas AJ and Vierra M: Pancreatic tumors
show high levels of hypoxia. Int J Radiat Oncol Biol Phys.
48:919–922. 2000.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Yan Y, Wang C, Zhou W, Shi Y, Guo P, Liu
Y, Wang J, Zhang CY and Zhang C: Elevation of circulating
miR-210-3p in high-altitude hypoxic environment. Front Physiol.
7(84)2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Crosby ME, Kulshreshtha R, Ivan M and
Glazer PM: MicroRNA regulation of DNA repair gene expression in
hypoxic stress. Cancer Res. 69:1221–1229. 2009.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Mizuno Y, Tokuzawa Y, Ninomiya Y, Yagi K,
Yatsuka-Kanesaki Y, Suda T, Fukuda T, Katagiri T, Kondoh Y, Amemiya
T, et al: miR-210 promotes osteoblastic differentiation through
inhibition of AcvR1b. FEBS Lett. 583:2263–2268. 2009.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Chen Z, Li Y, Zhang H, Huang P and Luthra
R: Hypoxia-regulated microRNA-210 modulates mitochondrial function
and decreases ISCU and COX10 expression. Oncogene. 29:4362–4368.
2010.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Masamune A, Kikuta K, Watanabe T, Satoh K,
Hirota M and Shimosegawa T: Hypoxia stimulates pancreatic stellate
cells to induce fibrosis and angiogenesis in pancreatic cancer. Am
J Physiol Gastrointest Liver Physiol. 295:G709–G717.
2008.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Friess H, Yamanaka Y, Büchler M, Beger HG,
Do DA, Kobrin MS and Korc M: Increased expression of acidic and
basic fibroblast growth factors in chronic pancreatitis. Am J
Pathol. 144:117–128. 1994.PubMed/NCBI
|
|
41
|
Kobrin MS, Yamanaka Y, Friess H, Lopez ME
and Korc M: Aberrant expression of type I fibroblast growth factor
receptor in human pancreatic adenocarcinomas. Cancer Res.
53:4741–4744. 1993.PubMed/NCBI
|
|
42
|
Yamanaka Y, Friess H, Buchler M, Beger HG,
Uchida E, Onda M, Kobrin MS and Korc M: Overexpression of acidic
and basic fibroblast growth factors in human pancreatic cancer
correlates with advanced tumor stage. Cancer Res. 53:5289–5296.
1993.PubMed/NCBI
|
|
43
|
Kuehn R, Lelkes PI, Bloechle C, Niendorf A
and Izbicki JR: Angiogenesis, angiogenic growth factors, and cell
adhesion molecules are upregulated in chronic pancreatic diseases:
Angiogenesis in chronic pancreatitis and in pancreatic cancer.
Pancreas. 18:96–103. 1999.PubMed/NCBI View Article : Google Scholar
|