Introduction
According to the World Health Organization (WHO),
worldwide, ~2 billion individuals have been infected with hepatitis
B virus (HBV) and ~257 million individuals remain chronically
infected [defined as hepatitis B surface antigen (HBsAg)-positive]
(1). An estimated 887,000
individuals die due to complications associated with hepatitis B,
such as cirrhosis and hepatocellular carcinoma (HCC) each year. In
addition, ~71 million individuals have been infected with hepatitis
C virus (HCV) worldwide, and ~399,000 of these die annually
(2).
In Japan, the estimated number of individuals
infected with HBV and HCV is ~3 million. Despite a gradual decrease
in the mortality rates due to HCC, ~30,000 individuals die of HCC
annually, and 80% of these cases are caused by HBV and HCV
(3-6).
The Oita Prefecture, located in Kyushu in western Japan, has a high
death rate due to HCC, based on the statistics obtained from the
Ministry of Health, Labor and Welfare (Fig. 1).
The advent of direct antiviral agents has
significantly improved the treatment outcomes of HCV infection
(7-10).
Nucleoside analogs can also significantly suppress HBV replication,
leading to a reduction in cirrhosis decompensation and HCC
(11-13).
At present, the largest challenge faced in Japan regarding
hepatitis infection is the identification of individuals with
undiagnosed HCV and HBV infections.
In Japan, the Industrial Safety and Health Act was
enacted in 1972 to ensure the safety and health of workers in the
workplace. Article 66 of this law stipulates that ‘The employer
shall, as provided for by the Ordinance of the Ministry of Health,
Labour and Welfare, have medical examinations of workers conducted
by a physician’ (14). This general
medical checkup must be performed annually during a period of
employment. By law, all workers must undergo a periodical medical
examination with the same included checks; however, serological
testing for HCV and HBV are non-statutory medical examination
checks and are not required by law.
Infection control in dental medical institutions is
an important issue as dental healthcare workers (DHWs) often come
in contact with the blood and saliva of patients. DHWs are at high
risk due to occupational exposure to blood-borne pathogens, such as
HBV, HCV and human immunodeficiency virus (HIV). The risk of
transmission from HBV-, HCV- and HIV-positive patients is 3-30, 3
and 0.3%, respectively (15).
In our previous study, it was reported that DHWs do
not always have sufficient knowledge regarding hepatitis viruses,
and Japanese dentists present with a high rate of HBV infection and
low HB vaccine coverage (16-18).
In the United States, HB vaccination has been recommended for all
healthcare workers since 1982, but in Japan, mandatory HB
vaccination for healthcare workers has not yet been formalized. In
Japan, HB vaccination was started in certain medical institutions
in 1986(19), but there was a large
difference between facilities and there were no specific
guidelines. In 2009, the Japanese Society for Infection Prevention
and Control clarified vaccine guidelines for medical personnel
(20), and the standardization of HB
vaccination is progressing nationwide.
To the best of our knowledge, there are no recent
large-scale surveys in Japan since our previous study on hepatitis
virus infections in DHWs in the Fukuoka Prefecture in 2008(17). In the present study, the rates of
hepatitis virus infections amongst DHWs in the Oita Prefecture in
Kyushu were investigated, where the mortality rate as a result of
HCC is high. The results of the present study may prove useful in
developing strategies for promoting and maintaining the health of
DHWs.
Materials and methods
Subjects
A total of 1,834 members of the Dental National
Health Insurance Society in the Oita Prefecture, consisting of
dentists and other employees (dental hygienists, dental assistants,
dental technicians and clerks), were tested for hepatitis virus
during periodic medical examinations at medical institutions
contracted by the Dental National Health Insurance Society between
April 2018 and March 2019. Written informed consent regarding the
submission of the results of the medical examination to a third
party for health management and effective use was obtained from
each subject. The 1,834 subjects (530 males and 1,304 females) were
aged 18-91 years, with an mean age and standard deviation of
44.5±14.6 years (median age, 44.0 years) (Table I). There were 493 dentists and 1,341
employees.
 | Table ICharacteristics of the subjects. |
Table I
Characteristics of the subjects.
| Characteristic | Total | Dentists | Employees | P-value |
|---|
| Number of
subjects | 1,834 | 493 | 1,341 | |
| Sex,
male/female | 530/1,304 | 435/58 | 95/1,246 |
<0.0001b |
| Age, mean ±
standard deviation, years | 43.7±14.8 | 54.9±13.3 | 39.6±13.1 |
<0.0001b |
| Age, years, n
(%) | | | | |
|
18-19 | 7 | 0 (0) | 7(100) | 0.0361a |
|
20-29 | 388 | 4 (1.0) | 384 (99.0) |
<0.0001b |
|
30-39 | 384 | 74 (19.3) | 310 (80.7) | 0.0001b |
|
40-49 | 391 | 97 (24.8) | 294 (75.2) | NS |
|
50-59 | 359 | 115 (32.0) | 244 (68.0) | 0.0168a |
|
60-69 | 224 | 135 (60.3) | 89 (39.7) |
<0.0001b |
|
70-79 | 71 | 58 (81.7) | 13 (18.3) |
<0.0001b |
|
≥80 | 10 | 10(100) | 0 (0) |
<0.0001b |
| HBsAg, n (%) | | | | NS |
|
Positive | 11 (0.6) | 4 (0.8) | 7 (0.5) | |
|
Negative | 1,823 (99.4) | 489 (99.2) | 1,334 (99.5) | |
| Anti-HBs, n
(%) | | | |
<0.0001b |
|
Positive | 809 (44.1) | 278 (56.4) | 531 (39.6) | |
|
Negative | 1,025 (55.9) | 215 (43.6) | 810 (60.4) | |
| Anti-HCV | | | | NS |
|
Positive | 9 (0.5) | 4 (0.8) | 5 (0.4) | |
|
Negative | 1,825 (99.5) | 489 (99.2) | 1,336 (99.6) | |
Study design
The results of the medical examination were provided
to each individual in a sealed letter from the medical institution.
Anonymized data, including the age, sex, occupation (dentist or
other employee) and presence/proportion of hepatitis virus markers,
were collected and analyzed. The data collected for this study was
anonymized by the Dental National Health Insurance Society in the
Oita Prefecture.
Screening for viral hepatitis
(anti-HCV, HBsAg and anti-HBs)
The serum antibody to HCV (anti-HCV) levels were
measured using a fully automated chemiluminescent enzyme
immunoassay (CLEIA) kit (Lumipulse II HCV; Fujirebio, Inc.; cat.
no. 295977); samples with a cut-off index (C.O.I.) of >1.0 were
considered positive for the anti-HCV antibody.
HBsAg was detected using a Lumipulse HBsAg-HQ assay
(Fujirebio Inc.; cat. no. 291153; C.O.I., 0.005 IU/ml) and HBsAg
antibody (anti-HBs) levels were determined using a Lumipulse
HBsAb-N (Fujirebio Inc.; cat. no. 296493; C.O.I. 10 mIU/ml).
Measurements were performed using a fully automated CLEIA system
(Lumipulse G1200; Fujirebio Inc.), according to the manufacturer's
protocols (21,22).
Comparison of the results of the
present study with previously published data (5)
Regarding the HCV and HBV infection rates, 1,753
(18-69 years) out of 1,834 subjects were compared with the results
of 2,727,727 Japanese blood donors (16-69 years) in the study by
Tanaka et al (5).
Statistical analysis
All data are expressed as the mean ± standard
deviation. Differences between the two groups were analyzed using a
Mann-Whitney U test, Wilcoxon signed-rank test and a Fisher's exact
test. The adjusted odds ratios were calculated using univariate and
multivariate logistical regression analysis. All statistical
analyses were performed using JMP version 13 (SAS Institute, Inc.).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Univariate analysis of hepatitis virus
infection
The number of subjects who were positive for HBsAg,
anti-HBs and anti-HCV were 11 (0.6%), 809 (44.1%) and 9 (0.5%),
respectively (Table I). The positive
rate for anti-HBs was significantly higher in dentists than in the
employees (56.4 vs. 39.6%, respectively; P<0.0001).
Univariate analysis demonstrated significant
associations between the positive and negative markers of viral
hepatitis amongst the subjects (Table
II). A significant difference in mean age was observed between
the HBsAg-positive and negative subjects (P=0.0135). Furthermore, a
significantly higher number of HBsAg-negative subjects were
positive for anti-HBs (P=0.0283; Table
II). Significant differences in sex (P=0.0207) and mean age
(P=0.0034) were observed between the anti-HCV-positive and
-negative subjects. Similarly, significant differences in sex
(P=0.0001) and occupation (P<0.0001) were observed between the
anti-HBs-positive and negative subjects, and there was a
significantly higher number of anti-HBs-negative subjects who were
positive for HBsAg (P=0.0283).
 | Table IIDistribution of HBsAg, anti-HCV and
anti-HBs in positive and negative subjects. |
Table II
Distribution of HBsAg, anti-HCV and
anti-HBs in positive and negative subjects.
| A, HBsAg |
|---|
| Number of
individuals | Positive, n=11 | Negative,
n=1,823 | P-value |
|---|
| Sex, male/female, n
(%) | 4/7
(36.4/63.6) | 526/1,297
(28.9/71.1) | NS |
| Age, mean ± SD,
years | 54.3±11.4 | 43.6±14.8 | 0.0135a |
| Occupation,
dentist/employee, n (%) | 4/7
(36.4/63.6) | 489/1,334
(26.8/73.2) | NS |
| Anti-HBs,
positive/negative, n (%) | 1/10
(9.1/90.9) | 808/1,015
(44.3/55.7) | 0.0283a |
| Anti-HCV,
positive/negative, n (%) | 0/11 (0/100) | 9/1,814
(0.5/99.5%) | NS |
| B, Anti-HCV |
| Number of
individuals | Positive, n=9 | Negative,
n=1,825 | P-value |
| Sex, male/female, n
(%) | 6/3
(66.7/33.3) | 524/1,301
(28.7/71.3) | 0.0207 |
| Age, mean ± SD,
years | 58.4±13.2 | 43.6±14.7 | 0.0034b |
| Occupation,
dentist/employee, n (%) | 4/5
(44.4/55.6) | 489/1,336
(26.8/73.2) | NS |
| HBsAg,
positive/negative, n (%) | 0/9 (0/100) | 11/1,814
(0.6/99.4) | NS |
| Anti-HBs,
positive/negative, n (%) | 3/6
(33.3/66.7) | 806/1,019
(44.2/55.8) | NS |
| C, Anti-HBs |
| Number of
individuals | Positive,
n=809 | Negative,
n=1,025 | P-value |
| Sex, male/female, n
(%) | 271/538
(33.5/66.5) | 259/766
(25.3/74.7) | 0.0001c |
| Age, mean ± SD,
years | 43.6±14.9 | 43.8±14.7 | NS |
| Occupation,
dentist/employee, n (%) | 278/531
(56.4/39.6) | 215/1,336
(43.6/60.4) |
<0.0001c |
| HBsAg,
positive/negative, n (%) | 1/808
(0.1/99.9) | 10/1,015
(1.0/99.0) | 0.0283a |
| Anti-HCV,
positive/negative, n (%) | 3/806
(0.4/99.6) | 6/1,019
(0.6/99.4) | NS |
Age-specific prevalence of HBsAg and
anti-HCV
The age-specific prevalence of the markers of HBV
and HCV infection are shown in Table
III. The positive rates of HBsAg and anti-HCV increased with
age. The positive rates of HBsAg and anti-HCV were compared between
1,753 out of 1,834 subjects (18-69 years of age) in the present
study and 2,727,727 blood donors (<70 years of age) in a study
by Tanaka et al (5); the
positive rate of HBsAg was significantly higher amongst subjects
aged 50-59 years old than amongst the age-matched blood donors
(P=0.0177). The positive rate was highest among dentists aged 50-59
(1.7%) and 70-79 (1.7%), and other dental employees aged 60-69
(2.2%).
 | Table IIIAge-specific prevalence of HBsAg and
anti-HCV. |
Table III
Age-specific prevalence of HBsAg and
anti-HCV.
| A, HBsAg |
|---|
| | Subjects in the
present study | First-time blood
donors between 2007 and 2011 | |
|---|
| | Total | Dentist | Employee | Total | |
|---|
| Age, years | n | HBsAg-positive, n
(%) | n | HBsAg-positive, n
(%) | n | HBsAg-positive, n
(%) | n | HBsAg-positive, n
(%) | P-value |
|---|
| 18-19 | 7 | 0 (0) | 0 | - | 7 | 0 (0) | 275,907 | 233 (0.1) | NS |
| 20-29 | 388 | 0 (0) | 4 | 0 (0) | 384 | 0 (0) | 1,301,790 | 1,205 (0.1) | NS |
| 30-39 | 384 | 1 (0.3) | 74 | 0 (0) | 310 | 1 (0.3) | 513,237 | 1,305 (0.3) | NS |
| 40-49 | 391 | 2 (0.5) | 97 | 1 (1.0) | 294 | 1 (0.3) | 351,162 | 1,217 (0.3) | NS |
| 50-59 | 359 | 5 (1.4) | 115 | 2 (1.7) | 244 | 3 (1.2) | 195,819 | 987 (0.5) | 0.0177a |
| 60-69 | 224 | 2 (0.9) | 135 | 0 (0) | 89 | 2 (2.2) | 82,812 | 522 (0.6) | NS |
| 70-79 | 71 | 1 (1.4) | 58 | 1 (1.7) | 13 | 0 (0) | - | - | - |
| ≥80 | 10 | 0 (0) | 10 | 0 (0) | 0 | - | - | - | - |
| Total | 1,834 | 11 (0.6) | 493 | 4 (0.8) | 1,341 | 7 (0.5) | 2,720,727 | 5,469 (0.2) | |
| B, Anti-HCV |
| | Subjects in the
present study | First-time blood
donors between 2007 and 2011 | |
| | Total | Dentist | Employee | Total | |
| Age, years | n | Anti-HCV positive,
n (%) | n | Anti-HCV positive,
n (%) | n | Anti-HCV positive,
n (%) | n | Anti-HCV positive,
n (%) | P-value |
| 18-19 | 7 | 0 (0) | 0 | - | 7 | 0 (0) | 275,907 | 115 (0) | NS |
| 20-29 | 388 | 1 (0.3) | 4 | 0 (0) | 384 | 1 (0.3) | 1,301,790 | 754 (0.1) | NS |
| 30-39 | 384 | 0 (0) | 74 | 0 (0) | 310 | 0 (0) | 513,237 | 961 (0.2) | NS |
| 40-49 | 391 | 1 (0.3) | 97 | 0 (0) | 294 | 1 (0.3) | 351,162 | 1,125 (0.3) | NS |
| 50-59 | 359 | 1 (0.3) | 115 | 0 (0) | 244 | 1 (0.4) | 195,819 | 981 (0.5) | NS |
| 60-69 | 224 | 5 (2.2) | 135 | 3 (2.2) | 89 | 2 (2.2) | 82,812 | 504 (0.6) | 0.0019a |
| 70-79 | 71 | 1 (1.4) | 58 | 1 (1.7) | 13 | 0 (0) | - | - | - |
| ≥80 | 10 | 0 (0) | 10 | 0 (0) | 0 | - | - | - | - |
| Total | 1,834 | 9 (0.5) | 493 | 4 (0.8) | 1,341 | 5 (0.4) | 2,720,727 | 4,440 (0.2) | |
Similarly, the positive rate of anti-HCV was
significantly higher among subjects who were in their 60s in the
present study when compared with the blood donors (P=0.0019). The
highest rates were observed in dentists and employees who were in
their 60-69 (2.2%).
Age-specific prevalence of
anti-HBs
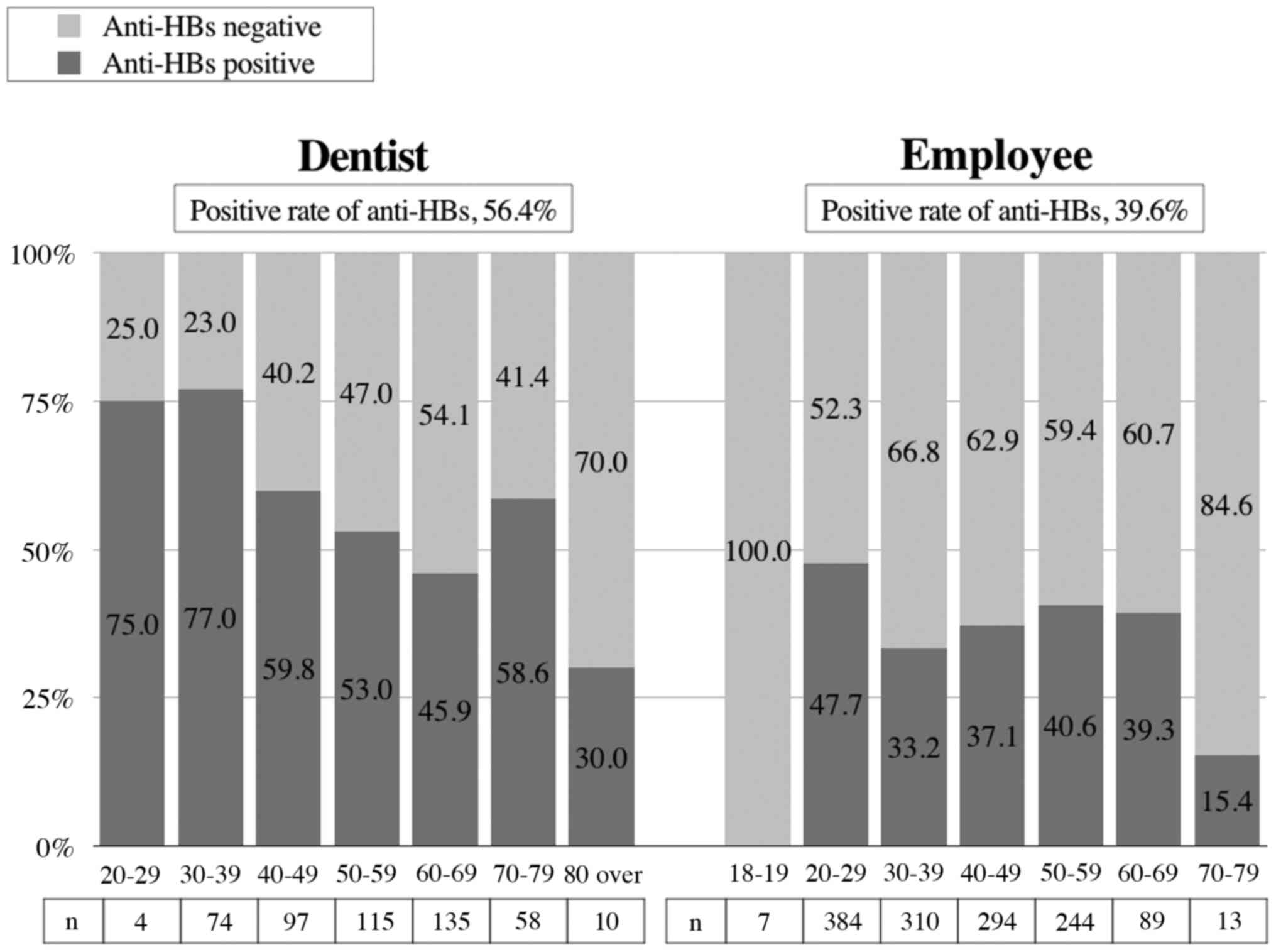
The age-specific prevalence of the anti-HBs marker
is shown in Fig. 2. The presence or
absence of vaccination amongst the subjects in the present study
could not be investigated. The rate of anti-HBs positivity amongst
dentists decreased with age from 75.0% in subjects aged 20-29 years
old to 30% in those aged 80 years old and over (Fig. 2). Alternatively, the rate of anti-HBs
positivity amongst the employees was low at all ages, particularly
in those who were <20 years of age (Fig. 2).
Multivariate analysis of anti-HBs
positivity
All variables in the univariate analysis were
included in the multivariate analysis (Table IV). Based on the multivariate
analysis, three factors [HBsAg negativity, occupation (dentist) and
age (20-29 years old)] were found to be associated with anti-HBs
positivity with adjusted odds ratios of 8.29, 2.27 and 1.59,
respectively (P<0.05).
 | Table IVMultivariate analysis of factors
associated with anti-HBs-positivity. |
Table IV
Multivariate analysis of factors
associated with anti-HBs-positivity.
| Factor | Odds ratio | 95% Confidence
interval | P-value |
|---|
| HBsAg negative | 8.29 | 1.55-153.38 | 0.0098a |
| Occupation,
dentist | 2.27 | 1.82-2.83 |
<0.0001b |
| Age group,
20-29 | 1.59 | 1.25-2.01 | 0.0002b |
Discussion
HBV, HCV and HIV are some of the most common and
dangerous pathogens that spread through blood in medical
institutions (15). HBV is the most
infectious type of virus that causes blood-borne infections, and it
can survive on dry environmental surfaces for >7 days (23). Dental workers are at increased risk
of needle-stick injuries resulting in exposure to the blood and
body fluids of potentially infected patients. In a previous study,
exposure to needle-stick injuries was reported in 70.3% of dentists
and 77.2% of dental hygienists and assistants in Japan (24). In Canada, an average of 1.5 mucous
membrane exposures and 3 percutaneous injuries per a dentist were
reported per year (25). The rate of
acquiring an HBV infection through HBV-contaminated needles is
high, 12% (26) to 60% (27), in unvaccinated individuals.
Dentists have been reported to present with the
highest rates of HBV infection amongst health care workers
(28). The prevalence of HBsAg
amongst dentists was reported to be significantly higher (45%) than
that amongst doctors (35.8%) and blood donors (20%) (28). Furthermore, the seroprevalence of HBV
infections amongst dentists was 12.1% in Japan (17), 2.4% in Malaysia (29), 13% in Korea (29), 10.8% in Brazil (30), 9-14% in the USA (31) and 7% in Germany (32). In a previous study consisting of
1,628 Iranian DHWs, the positive rates of HBsAg, anti-hepatitis B
virus core antigen (anti-HBc), anti-HBs, anti-HCV and anti-HIV were
found to be 0.42, 4.97, 88.53, 0.06 and 0%, respectively; 94.28% of
the subjects were reported to be vaccinated against HBV (33). The authors emphasized that prevalence
of HBV infection among DHWs was lower than that in the general
population, but permanent vigilance and educational programs
addressing blood-borne viruses infection among dentists are
necessary (33).
In one of our previous studies conducted in 2007,
141 DHWs in the Fukuoka Prefecture (northern Kyushu in Japan) were
screened for the presence of HBV and HCV infections; amongst them,
17 subjects (12.1%) were anti-HBc positive (17). The positive rate of anti-HBc
increased with age from 2.9% for individuals aged 30-39 to 100% in
individuals aged 70-79 (5.6% in individuals aged 40-49, 29.4% in
individuals aged 50-59 and 85.7% in individuals aged 60-69) in the
previous study (17). Furthermore,
less than half (48.2%) of the participants had been vaccinated
against hepatitis B; 16 (25.4%) out of the 63 unvaccinated DHWs
were found to be anti-HBc positive (17).
In our 2017 study, an anonymous online survey and
interview with members of the Japanese Society of Dental Practice
Administration was performed in order to evaluate the recognition
of the problems associated with hepatitis amongst dentists, and
found that 26.8% of the subjects had not been immunized against
hepatitis B. Additionally, male dentists had a significantly higher
risk and knowledge deficits scores than female dentists, and the
directors of the dental clinics presented with significantly higher
risk and knowledge deficits scores than dentists working at
university hospitals (18).
In the United States, a case of HBV transmission
from one patient to another during tooth extraction was reported in
2007(34). It was identified as a
nosocomial infection due to the matching of the HBV nucleotide
sequence between the two patients. Similarly, a case of acute
hepatitis C following dental treatment was suspected in Japan in
2017(35). Only 59.8% of patients
with HBV- and HCV-infected liver disease declared the presence of a
hepatitis virus infection whilst undergoing dental treatment
(36). The most common reason for
not declaring the presence of a hepatitis viral infection at a
dental clinic was because the dentist had not enquired regarding
the possibility of an underlying disease (71.2%).
The Japanese Society for Infection Prevention and
Control recommends that hepatitis B vaccination must be given to
all medical personnel who are sensitive to hepatitis B in a medical
institution, if there is a possibility of their coming in contact
with a patient (or the blood or body fluids of a potentially
infected patient) (37,38). Unfortunately, it is not legally
required for DHWs to be tested for the hepatitis virus or be
vaccinated against hepatitis B in Japan. Furthermore, there is a
dearth of recent epidemiological data on hepatitis virus infections
amongst Japanese DHWs.
In the present study, the examination of hepatitis
virus markers as health check items was first introduced by the
Dental National Health Insurance Society in the Oita Prefecture,
which includes dentists and employees. A total of 20 (11
HBsAg-positive and 9 anti-HCV-positive subjects) were found to be
HBV and HCV-infected. In addition, the infection rate was
particularly high amongst those aged 50-79. The positive rate of
anti-HBs was 44.1% (dentists vs. employees, 56.4 vs. 39.6%). This
ratio was lower than that observed in our survey conducted in the
Fukuoka Prefecture in 2007 (51.8%) (17). It was estimated that the vaccination
rate was lower amongst dental employees than dentists, although the
presence or absence of HB vaccination in the current study could
not be confirmed.
HCV RNA has been detected in 6.1% (39) to 18% (40) of the dental instruments and in the
saliva of patients with hepatitis C (41,42). HCV
transmission in dental healthcare settings is preventable using
standard precautions, including injection safety, although no
vaccine for the prevention of HCV infection is available thus far.
Dentists should receive vaccinations against hepatitis B to avoid
the risk of HBV infection. Unvaccinated dentists have been reported
to be 5x more likely to be infected with HBV than vaccinated
dentists (31). In the present
study, the anti-HBs-positive DHWs were nearly 8.3 times more likely
to be HBsAg negative than the anti-HBs-negative DHWs. According to
Banatvala and Van Damme (43), the
primary objective of vaccination against hepatitis B is to prevent
infection and thereby reduce the incidence of persistent HBV
infections and chronic liver diseases; in addition, the elimination
of the pool of chronic carriers limits the transmission of the
infection to susceptible contacts. A previous survey reported that
8.8% of a total of 283 dentists were not vaccinated, primarily due
to a lack of information, thus indicating that educational
campaigns are required to assist in reducing the transmission of
HBV (44).
As of December 31, 2018, there were 104,908 dentists
in Japan, and the majority of these (90,105 dentists) worked as
dentists in clinics (45). However,
information disclosure and education about hepatitis is not
sufficient, as it is estimated that several Japanese dentists have
not yet been tested for hepatitis virus (17,18).
Therefore, it is important to increase HCV and HBV testing rates
and HBV vaccination rates for dentists (46). This can be achieved by educating
dental workers about hepatitis. The method used to test for
assessing hepatitis infection in the present study may prove useful
in the future. In addition, the Dental National Health Insurance
Society has a ‘Hepatitis B vaccination subsidy system’, which
subsidizes the cost of the HBV vaccinations, and it is recommended
that awareness of this system amongst DHWs should be increased.
The present study has several limitations. First, it
was not possible to determine if a DHW had been vaccinated against
hepatitis B, and data on the antibody titers were not available.
Second, the outcomes of 11 HBsAg-positive and 9 anti-HCV-positive
subjects were not evaluated.
In conclusion the rate of hepatitis virus infection
amongst the 1,834 DHWs in the Oita Prefecture of Japan was
determined in the present study. The positive rates of HBsAg,
anti-HBs and anti-HCV were 0.6, 44.1 and 0.5%, respectively;
furthermore, the rates were higher amongst dentists than among the
other associated employees. These findings highlight the importance
of identifying untreated hepatitis individuals amongst DHWs who
have not yet been tested for HBV or HCV in order to prevent and
provide early treatment for the disease.
Acknowledgements
We would like to thank Dr Haruhiko Wakita (Dental
National Health Insurance Society) for their support during data
collection.
Funding
This study was supported in part by a Grant-in-Aid
for Scientific Research (grant no. 17K12012) from the Ministry of
Education, Culture, Sports, Science, and Technology of Japan.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YN interpreted data, performed the statistical
analysis and wrote the manuscript. TK collected data from
participants. HN made a substantial contribution to the conception
and design of the study, and made critical revisions to the
manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee of Oita Dental Association (approval no. 2020-1) and was
performed in accordance with the Declaration of Helsinki. Written
informed consent regarding the submission of the results of the
medical examination to a third party for health management and
effective use was obtained from each subject.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
WHO: Hepatitis B. July 27, 2019.
urihttp://www.who.int/mediacentre/factsheets/fs204/en/simplehttp://www.who.int/mediacentre/factsheets/fs204/en/.
|
|
2
|
WHO: Hepatitis C. July 27, 2019.
urihttp://www.who.int/mediacentre/factsheets/fs164/en/simplehttp://www.who.int/mediacentre/factsheets/fs164/en/.
|
|
3
|
Umemura T, Ichijo T, Yoshizawa K, Tanaka E
and Kiyosawa K: Epidemiology of hepatocellular carcinoma in Japan.
J Gastroenterol. 44 (Suppl 19):S102–S107. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Omata M, Kanda T, Wei L, Yu ML, Chuang WL,
Ibrahim A, Lesmana CR, Sollano J, Kumar M, Jindal A, et al: APASL
consensus statements and recommendations for hepatitis C
prevention, epidemiology, and laboratory testing. Hepatol Int.
10:681–701. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tanaka J, Akita T, Ohisa M, Sakamune K, Ko
K, Uchida S and Satake M: Trends in the total numbers of HBV and
HCV carriers in Japan from 2000 to 2011. J Viral Hepat. 25:363–372.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tanaka J, Akita T, Ko K, Miura Y and
Satake M: Countermeasures against viral hepatitis B and C in Japan:
An epidemiological point of view. Hepatol Res. 49:990–1002.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Omata M, Nishiguchi S, Ueno Y, Mochizuki
H, Izumi N, Ikeda F, Toyoda H, Yokosuka O, Nirei K, Genda T, et al:
Sofosbuvir plus ribavirin in Japanese patients with chronic
genotype 2 HCV infection: An open-label, phase 3 trial. J Viral
Hepat. 21:762–768. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kumada H, Suzuki Y, Ikeda K, Toyota J,
Karino Y, Chayama K, Kawakami Y, Ido A, Yamamoto K, Takaguchi K, et
al: Daclatasvir plus asunaprevir for chronic HCV genotype 1b
infection. Hepatology. 59:2083–2091. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mizokami M, Yokosuka O, Takehara T,
Sakamoto N, Korenaga M, Mochizuki H, Nakane K, Enomoto H, Ikeda F,
Yanase M, et al: Ledipasvir and sofosbuvir fixed-dose combination
with and without ribavirin for 12 weeks in treatment-naive and
previously treated Japanese patients with genotype 1 hepatitis C:
An open-label, randomised, phase 3 trial. Lancet Infect Dis.
15:645–653. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chayama K, Suzuki F, Karino Y, Kawakami Y,
Sato K, Atarashi T, Naganuma A, Watanabe T, Eguchi Y, Yoshiji H, et
al: Efficacy and safety of glecaprevir/pibrentasvir in Japanese
patients with chronic genotype 1 hepatitis C virus infection with
and without cirrhosis. J Gastroenterol. 53:557–565. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Liaw YF, Sung JJ, Chow WC, Farrell G, Lee
CZ, Yuen H, Tanwandee T, Tao QM, Shue K, Keene ON, et al:
Lamivudine for patients with chronic hepatitis B and advanced liver
disease. N Engl J Med. 351:1521–1531. 2004.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chang TT, Gish RG, de Man R, Gadano A,
Sollano J, Chao YC, Lok AS, Han KH, Goodman Z, Zhu J, et al: A
comparison of entecavir and lamivudine for HBeAg-positive chronic
hepatitis B. N Engl J Med. 354:1001–1010. 2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
European Association for the Study of the
Liver. Electronic address: simpleeasloffice@easloffice.eu
and European Association for the Study of the Liver. EASL 2017
Clinical Practice Guidelines on the management of hepatitis B virus
infection. J Hepatol. 67:370–398. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Japanese low translation (Ministry of
Justice). Industrial Safety and Health Act. urihttp://www.japaneselawtranslation.go.jp/law/detail/?id=1926&vm=&resimplehttp://www.japaneselawtranslation.go.jp/law/detail/?id=1926&vm=&re.
|
|
15
|
Gerberding JL: Management of occupational
exposures to blood-borne viruses. N Engl J Med. 332:444–451.
1995.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nagao Y, Chiba I and Sata M: Survey of
hepatitis B and C in students of faculty of dentistry and dental
hygienist school. Kansenshogaku Zasshi. 78:554–565. 2004.PubMed/NCBI View Article : Google Scholar : (In Japanese).
|
|
17
|
Nagao Y, Matsuoka H, Kawaguchi T, Ide T
and Sata M: HBV and HCV infection in Japanese dental care workers.
Int J Mol Med. 21:791–799. 2008.PubMed/NCBI
|
|
18
|
Nagao Y, Ozaki T, Kawaguchi A, Chiba I,
Harada K, Saito T and Shiratsuchi S: Survey of dental health care
workers regarding their knowledge of viral liver disease and
prevention of its transmission, using an online questionnaire. Adv
Res Gastroentero Hepatol. 10:95–108. 2018.
|
|
19
|
Nishijo T, Inoue R, Kurita T, Akita A,
Takano K and Kuroda H: A preliminary report of the vaccination of
hepatitis B vaccine to the medical stuff in Juntendo University
Hospital. Juntendo Med J. 34:232–235. 1988.
|
|
20
|
Okabe N, Arakawa S, Iwata S, Shiraishi T,
Taya K, Fujimoto T, Mikamo H and Yasuoka A: The first edition of
the vaccine guideline for nosocomial infections. Jap J
Environmental Infect. 24:S1–S11. 2009.(In Japanese).
|
|
21
|
Deguchi M, Kagita M, Yoshioka N, Tsukamoto
H, Takao M, Tahara K, Maeda I, Hidaka Y, Yamauchi S, Kaneko A, et
al: Evaluation of the highly sensitive chemiluminescent enzyme
immunoassay ‘Lumipulse HBsAg-HQ’ for hepatitis B virus screening. J
Clin Lab Anal. 32(e22334)2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Choi SJ, Park Y, Lee EY, Kim S and Kim HS:
Performance evaluation of LUMIPULSE G1200 autoimmunoanalyzer for
the detection of serum hepatitis B virus markers. J Clin Lab Anal.
27:204–206. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Bond WW, Favero MS, Petersen NJ, Gravelle
CR, Ebert JW and Maynard JE: Survival of hepatitis B virus after
drying and storage for one week. Lancet. 1:550–551. 1981.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kobayashi K: Questionnaire study of
needlestick injures and hepatitis B vaccination in general dental
practices. Jap J Environmental Infect. 30:348–353. 2015.(In
Japanese).
|
|
25
|
McCarthy GM, Koval JJ and MacDonald JK:
Occupational injuries and exposures among Canadian dentists: The
results of a national survey. Infect Control Hosp Epidemiol.
20:331–336. 1999.PubMed/NCBI View
Article : Google Scholar
|
|
26
|
Werner BG and Grady GF: Accidental
hepatitis-B-surface-antigen-positive inoculations Use of e antigen
to estimate infectivity. Ann Intern Med. 97:367–369.
1982.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Relation of e antigen to infectivity of
hBsAg-positive inoculations among medical personnel. Lancet.
1:492–494. 1976.PubMed/NCBI
|
|
28
|
Olubuyide IO, Ola SO, Aliyu B, Dosumu OO,
Arotiba JT, Olaleye OA, Odaibo GN, Odemuyiwa SO and Olawuyi F:
Hepatitis B and C in doctors and dentists in Nigeria. QJM.
90:417–422. 1997.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Vadivale M, Tan TC and Ong CN:
Sero-prevalence of hepatitis B infection among dental
professionals. Singapore Med J. 33:367–369. 1992.PubMed/NCBI
|
|
30
|
Batista SM, Andreasi MS, Borges AM,
Lindenberg AS, Silva AL, Fernandes TD, Pereira EF, Basmage EA and
Cardoso DD: Seropositivity for hepatitis B virus, vaccination
coverage, and vaccine response in dentists from Campo Grande, Mato
Grosso do Sul, Brazil. Mem Inst Oswaldo Cruz. 101:263–267.
2006.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Cleveland JL, Siew C, Lockwood SA,
Gruninger SE, Gooch BF and Shapiro CN: Hepatitis B vaccination and
infection among U.S. dentists, 1983-1992. J Am Dent Assoc.
127:1385–1390. 1996.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ammon A, Reichart PA, Pauli G and Petersen
LR: Hepatitis B and C among Berlin dental personnel: Incidence,
risk factors, and effectiveness of barrier prevention measures.
Epidemiol Infect. 125:407–413. 2000.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ahmad Akhoundi MS, Momeni N, Norouzi M,
Ghalichi L, Shamshiri AR, Alavian SM, Poortahmasebi V and Jazayeri
SM: Prevalence of blood-borne viruses among Iranian dentists:
Results of a national survey. Int J Occup Med Environ Health.
28:593–602. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Redd JT, Baumbach J, Kohn W, Nainan O,
Khristova M and Williams I: Patient-to-patient transmission of
hepatitis B virus associated with oral surgery. J Infect Dis.
195:1311–1314. 2007.PubMed/NCBI View
Article : Google Scholar
|
|
35
|
Seike M, Honda K, Endo M, Oribe J, Arakawa
M, Tokoro M, Iwao M, Otsu S and Murakami K: A case of acute
hepatitis C suspected to be infected by dental treatment. Kanzo. 58
(Suppl 3)(A880)2017.(In Japanese).
|
|
36
|
Nagao Y, Kawaguchi T, Ide T and Sata M:
HCV or HBV infection self-disclosure to dentists. Kansenshogaku
Zasshi. 82:213–219. 2008.PubMed/NCBI View Article : Google Scholar : (In Japanese).
|
|
37
|
Okabe N, Arakawa S, Iwata S, Ihara T,
Shiraishi T, Taya K, Fujimoto T, Mikamo H and Yasuoka A: The second
edition of the vaccine guideline for healthcare professionals. Jap
J Environmental Infec. 29 (Suppl 3):S1–S13. 2014.(In Japanese).
|
|
38
|
Mikamo H, Taya K, Ishiguro N, Iwata S,
Uchida M, Okada K, Kanai S, Toyokawa M, Nakano T, Fujimura S, et
al: The third edition of the vaccine guideline for healthcare
professionals. Jap J Environmental Infect. 35 (Suppl II):S1–S31.
2020.(In Japanese).
|
|
39
|
Piazza M, Borgia G, Picciotto L, Nappa S,
Cicciarello S and Orlando R: Detection of hepatitis C virus-RNA by
polymerase chain reaction in dental surgeries. J Med Virol.
45:40–42. 1995.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hashish MH, Selim HS, Elshazly SA, Diab HH
and Elsayed NM: Screening for the hepatitis C virus in some dental
clinics in Alexandria, Egypt. J Egypt Public Health Assoc.
87:109–115. 2012.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Nagao Y, Seki N, Tamatsukuri S and Sata M:
Detection of hepatitis C virus in saliva before and after scaling
of dental calculus. Kansenshogaku Zasshi. 74:961–965.
2000.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Wang CC, Morishima C, Chung M, Engelberg
R, Krantz E, Krows M, Sullivan DG, Gretch DR and Corey L: High
serum hepatitis C virus (HCV) RNA load predicts the presence of HCV
RNA in saliva from individuals with chronic and acute HCV
infection. J Infect Dis. 193:672–676. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
43
|
Banatvala JE and Van Damme P: Hepatitis B
vaccine-do we need boosters? J Viral Hepat. 10:1–6. 2003.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Ferreira RC, Guimaraes AL, Pereira RD,
Andrade RM, Xavier RP and Martins AM: Hepatitis B vaccination and
associated factors among dentists. Rev Bras Epidemiol. 15:315–323.
2012.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Survey of Physicians, Dentists and
Pharmacists. 2018, Ministry of Health, Labor and Welfare (In
Japanese). Accessed from: urihttps://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/index.htmlsimplehttps://www.mhlw.go.jp/toukei/saikin/hw/ishi/18/index.html.
|
|
46
|
Nagao Y: The role of dentists in
controlling hepatocellular carcinoma in Japan (Review). Exp Ther
Med: Dec 3, 2020 (Epub ahead of print). doi:
org/10.3892/etm.2020.9545.
|