Introduction
Mediastinitis, which is an inflammation of the chest
region between the lungs, develops mostly due to a deep wound
infection of the sternum, pneumonia, perforation of the esophagus,
or descending necrotizing mediastinitis resulting from
ear-nose-throat infections (1).
Very rarely, mediastinitis can occur from hematogenous spread, and
is usually a complication of the health care received (2).
Microorganisms frequently implicated in mediastinal
infections include anaerobes, Streptococcus species,
Corynebacterium species and members of the family
Enterobacteriaceae (3).
Methicillin-resistant Staphylococcus aureus (MRSA) continues
to emerge as a causative agent of serious infections, mostly skin
and soft tissue infections (4,5). MRSA
is more frequently related to mediastinal infections following
cardiothoracic surgery, intravenous drug use and retropharyngeal
abscesses (3).
Few cases of MRSA mediastinitis have been described.
Herein, the rare case of MRSA mediastinitis accompanied by
pulmonary consolidation, pleural effusion and sternal osteomyelitis
following facial skin infection in, an otherwise healthy,
41-year-old man is reported.
Case report
A 41-year-old male non-smoking patient presented to
Sismanogleio Hospital with fever and anterior thoracic pain over
the previous 7 days. He had a medical history of gastroesophageal
reflux, and was not receiving any medication. The patient had no
history of diabetes mellitus, intravenous drug abuse, chronic
obstructive pulmonary disease or other comorbidities, and no
history of hospitalization and antibiotic intake in the previous 90
days.
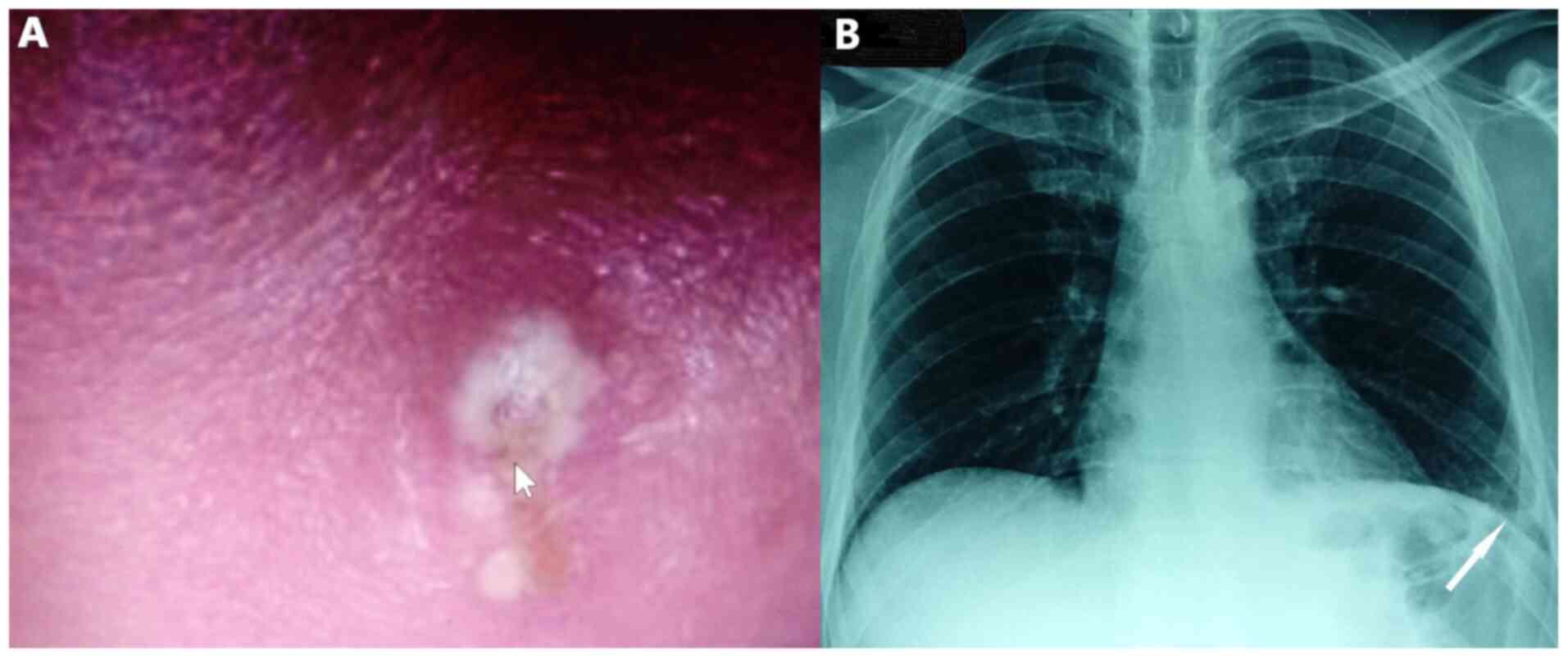
Clinical evaluation revealed a febrile patient with
dullness on percussion and crackles on auscultation at the base of
the left lung. He also had boils and carbuncles in his face, with a
pus-filled, 1 cm in greatest dimension, skin lesion on his
forehead. The skin over the infected area was red and swollen
(Fig. 1A). Physical examination of
the oropharyngeal region did not reveal abnormal findings. Clinical
examination did not also reveal neck lymph node enlargement or
obvious inflammation of neck skin and soft tissues.
Blood pressure was 150/85 mmHg, heart rate was 89
beats per minute, oxygen saturation was 96% on room air and body
temperature was 38.6˚C. Electrocardiography did not reveal abnormal
findings on admission. Chest X-ray revealed consolidation in the
left lower lobe with blunting of the left costophrenic angle
(Fig. 1B).
Laboratory investigation included complete blood
cell count, and standard biochemistry serum and urine parameters.
Laboratory findings included hemoglobin, 14.6 g/dl (normal range,
12-15 g/dl); white blood cell count, 13.37x103/µl
(normal range, 4-11x103/µl); platelet count,
167x103/µl (normal range, 150-400x103/µl);
serum glucose, 95 mg/dl (normal range, 60-100 mg/dl), C-reactive
protein (CRP), 96 mg/l (normal range, <6 mg/l) and D-dimers,
170.4 µg/l (normal range, <500 µg/l). Urinalysis and other blood
biochemistry parameters were normal.
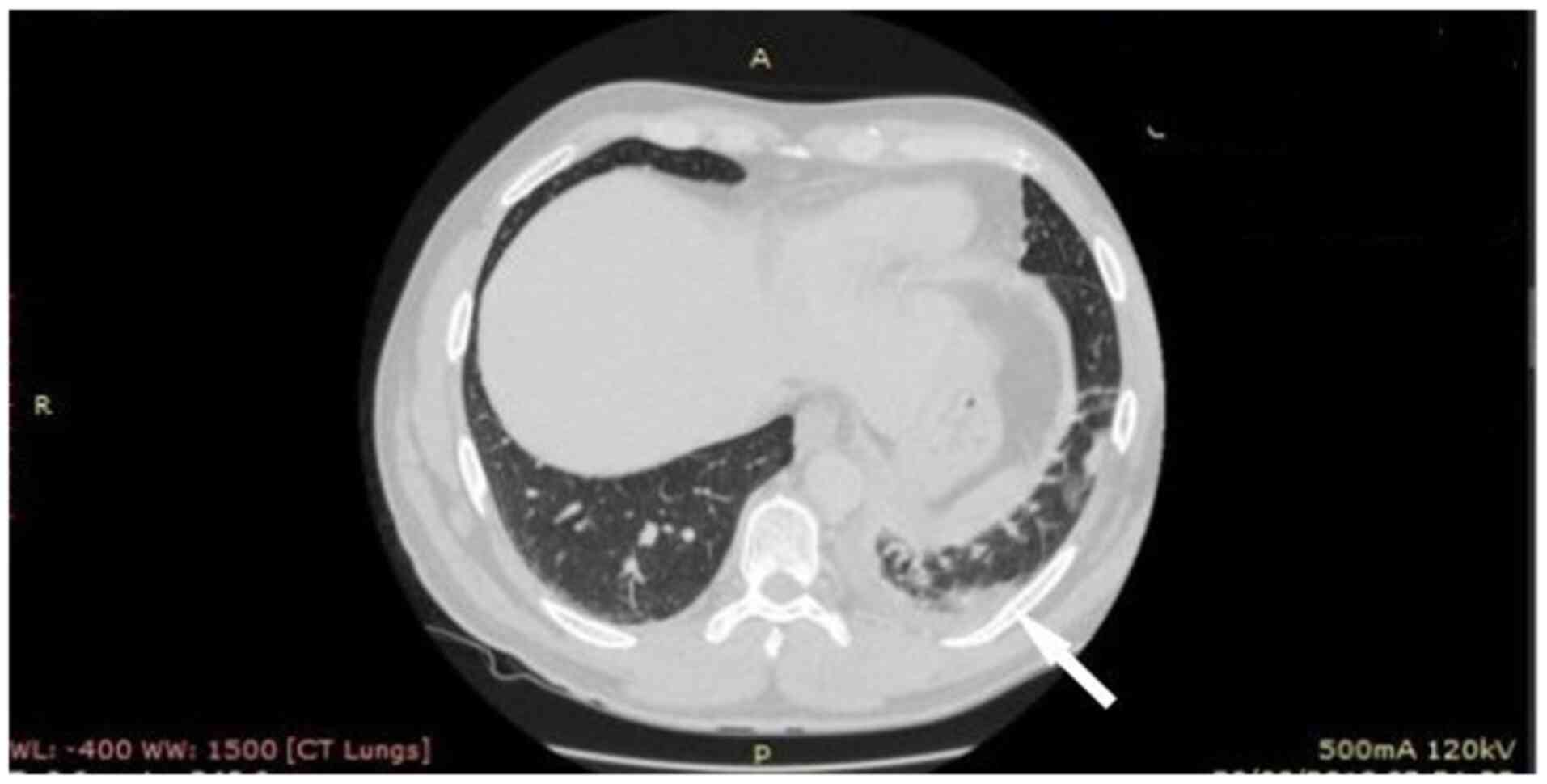
The patient underwent computed tomography (CT) of
the chest showing consolidation in the left lower lobe with left
pleural effusion, edema of the soft tissue adjacent to the first
sternocostal joint and heterogeneity, and invasion of the
retrosternal fat (Figs. 2 and
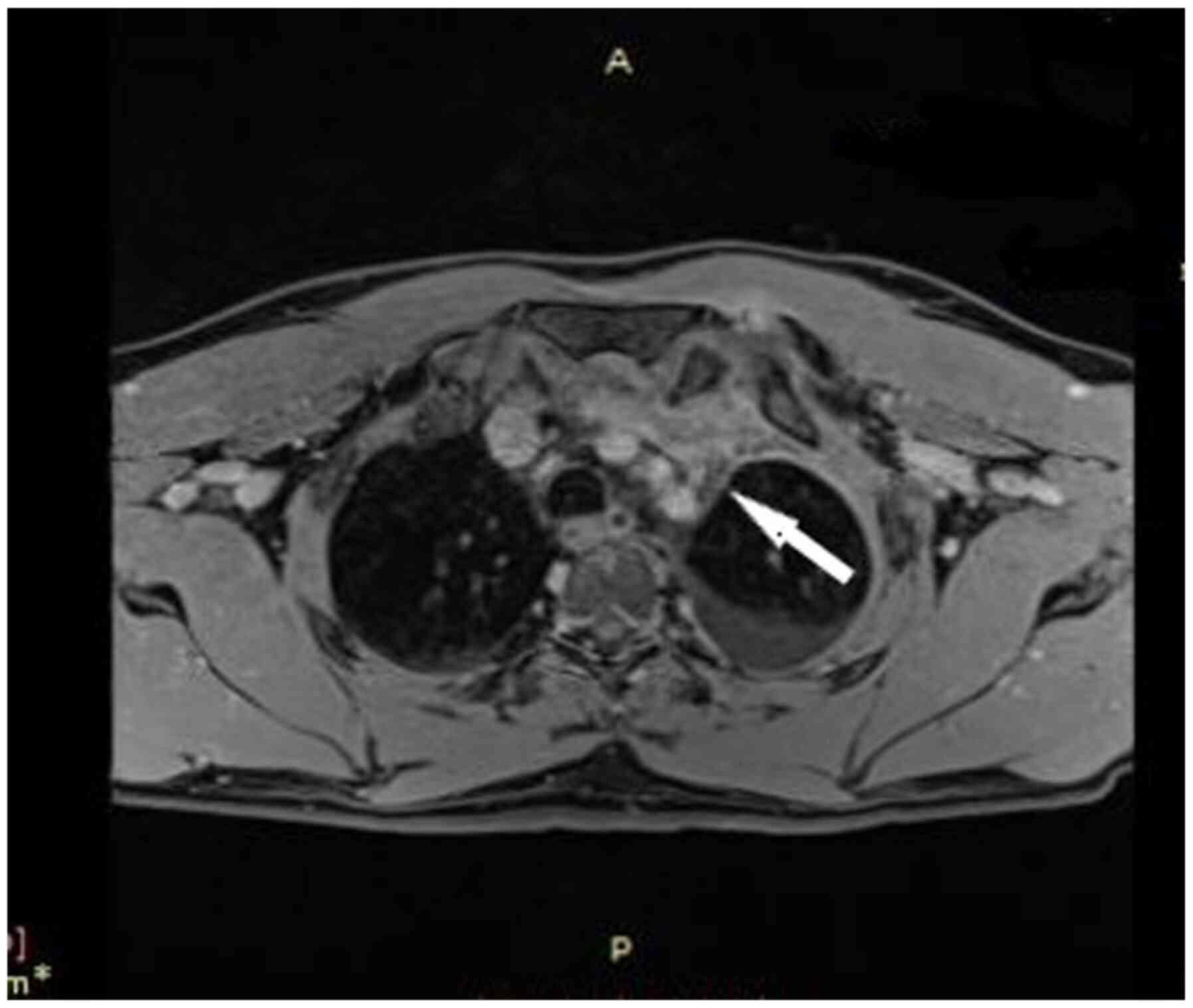
3). In addition, the patient
underwent magnetic resonance imaging (MRI) of the chest, to obtain
detailed information regarding the pleura and mediastinum, that
revealed abnormal soft tissue with dimensions at transverse level
7.0x1.3 cm, containing cystic lesions, adjacent to the first
sternocostal joint, indicating inflammation in sternocostal
cartilage. MRI also revealed contrast enhancement of the
ipsilateral mediastinal pleura, imaging compatible with
mediastinitis (Fig. 4).
Three blood cultures and culture of the pus from the
area of facial infection were obtained before administration of
antibiotics. The pleural effusion was assessed with pleural
ultrasound and was not tapped due to its small size. The patient
was treated with intravenous ceftriaxone (2 g single daily dose)
and intravenous vancomycin (1 g twice daily) for pneumonia and skin
infection, and metronidazole (500 mg three times daily) for
anaerobic coverage regarding the suspected pleural infection
empirically. MRSA, with susceptibility to ciprofloxacin,
trimethoprim-sulfamethoxazole, vancomycin and linezolid, and
resistance to clindamycin, was isolated both from blood cultures
and from pus culture. MRSA was considered the causative agent for
the mediastinal and lung lesions. A CT-guided aspiration of the
cystic lesions for culture and susceptibility testing was
performed, and this culture also revealed MRSA.
Transthoracic echocardiography was performed with
normal ejection fraction and valve function. The patient was
evaluated with an immunologic workup, with no immunodeficiency
being identified. Immunoglobulin panel and T cell subpopulations
were normal. Dihydrorhodamine testing for chronic granulomatous
disease was also performed in order to exclude another rare
etiology of severe MRSA infection. Human immunodeficiency virus
testing was also negative.
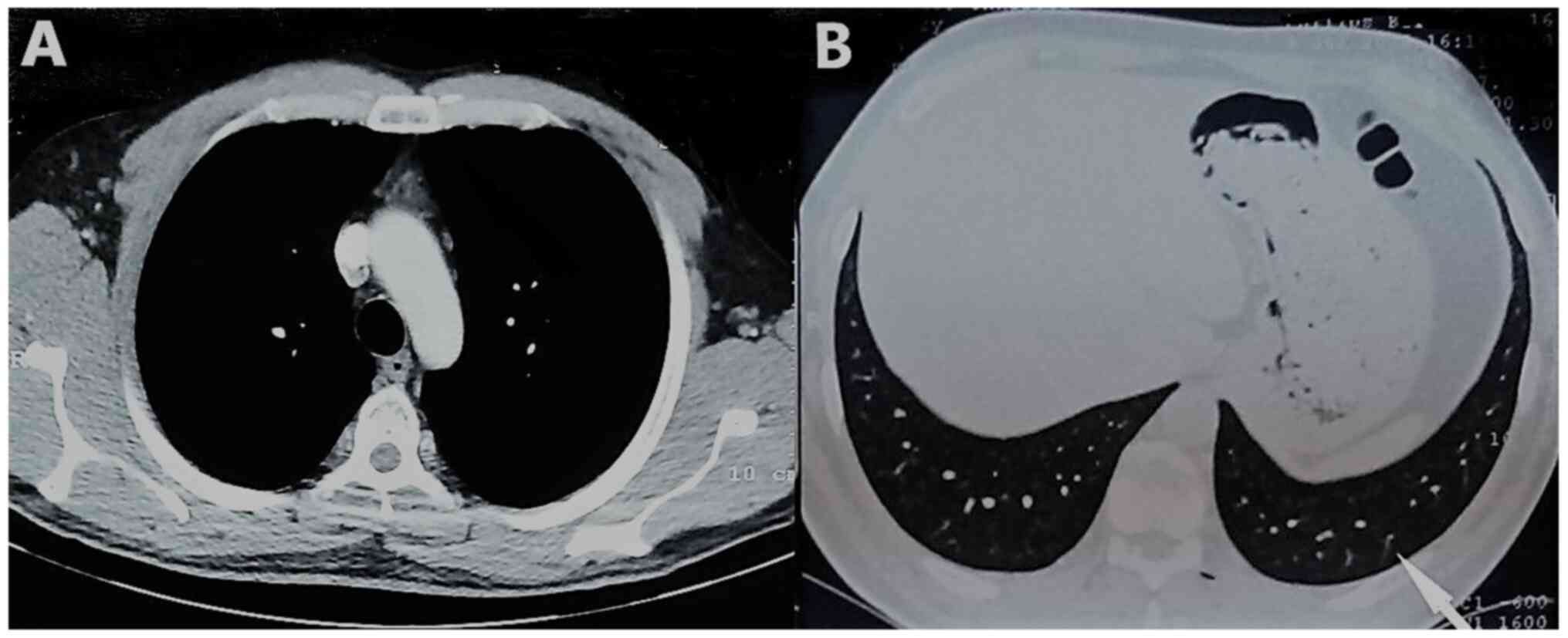
The patient presented with improvement in clinical
manifestations and blood inflammatory indices on the second day of
hospitalization, and the fever subsided on the fourth day of
hospitalization. There was no need for surgical procedure due to
the good clinical response to antibiotics. The patient received
intravenous vancomycin for 4 weeks and then there was a switch to
oral treatment with ciprofloxacin 500 mg twice daily for 2 weeks.
Table I shows the prescription
history and recovery flow of the patient. There was also complete
recovery observed in the imaging evaluation (Fig. 5).
 | Table IPrescription history and recovery
course of the patient. |
Table I
Prescription history and recovery
course of the patient.
| Day | Recovery course |
|---|
| Days 1-4 | Administration of
intravenous Ceftriaxone, Vancomycin and Metronidazole |
| Day 2 | Improvement in
clinical manifestations and blood inflammatory indices. |
| Day 4 | Fever
subsidence. |
| Day 4 | Positive cultures
from blood, pus and cystic lesions-isolation of Methicillin
-resistant -resistant Staphylococcus aureus. |
| Day 4-28 | Administration of
intravenous Vancomycin. |
| Days 29-42 | Administration of
oral Ciprofloxacin . |
| Day 43 | Complete recovery;
inflammatory indices within normal range. |
Discussion
The present report describes the rare case of a MRSA
mediastinitis and sternal osteomyelitis infection accompanied by
pulmonary consolidation and pleural effusion following skin
infection, which was caused by a hematogenous spread in an
immunocompetent host. Risk factors for MRSA infections include
intravenous drug use, immunodeficiency, prior therapy with
antibiotics and recent hospitalization. Young age, low
socioeconomic status, and minority ethnicity have also been
identified as emerging risk factors (3).
Moreover, MRSA mediastinitis is a particularly
infrequent infection, and it has previously been known to be
associated with complications of sternotomy and retropharyngeal
abscesses (3). However, the patient
described in the present case report did not have a retropharyngeal
infection or cardiothoracic surgery, nor established
immunodeficiency.
Common findings in mediastinitis are leukocytosis
and elevations in CRP levels (6,7). In
certain cases of acute mediastinitis, high levels of CRP are
associated with a greater risk of death (6,7). In
the present case report, the patient also presented with increased
levels of CRP. This biomarker was used to detect response to
therapy, and it was within the normal range at the end of the
treatment.
Although mediastinitis, as a result of hematogenous
spread is rare, it has been described previously. Smith and
Sinzobahamvya (8) reported an
interesting case of an 11-year-old child with septic arthritis due
to Staphylococcus aureus, complicated with anterior
mediastinal abscess through hematogenous spread. Mediastinitis
usually results from a wide range of etiologies, including
esophageal perforation, lung infection, infected lymph nodes of the
neck, an infected sternotomy wound, odontogenic infection,
peritonsillar or retropharyngeal abscess, trauma of the cervix,
epiglottitis, sinusitis and intravenous drug use (9). Mediastinitis as a result of
hematogenous spread was also described by Calvano et al
(3) in a case of an
immunocompromised 47-year-old female who presented with pneumonia
complicated with bacteremia and sepsis, and who developed multiple
neck and mediastinal abscesses due to Staphylococcus aureus.
Chang et al (2) reported a
case of mediastinitis in a hemodialysis patient as a complication
of Staphylococcus bacteremia, while Er et al (10) described a case of central venous
catheter-associated mediastinitis due to Candida
species.
In addition, mediastinitis as a complication of
primary skin infections is also a rare entity. Brisset et al
(1) reported a case of
Staphylococcus aureus mediastinitis in an immunocompetent
adult following back skin abscess. To the best of our knowledge,
the present case is the second report of such a case of
mediastinitis secondary to hematogenous spread following skin
infection.
Treatment of acute mediastinitis is based on
administration of antibiotics and control of the source of
inflammation with surgical debridement (11). Mediastinitis, developing as a
postoperative complication, usually requires rapid surgical
debridement. Generally, management with multiple surgical
procedures is needed in ~30% of patients. The surgical approach
depends on the extent of the disease and structures involved
(12). The usual duration of
therapy for mediastinitis is up to 4-6 weeks depending on the
extent of surgical debridement performed (13).
In conclusion, development of mediastinitis, with
hematogenous spread following skin infection, is a rare clinical
entity. With the increase of described MRSA infectious disease
cases, clinicians should remain alert for future cases of MRSA
mediastinitis and consider mediastinitis in the differential
diagnosis when a patient presents with respiratory symptoms, such
as thoracic pain and dyspnea, as well as signs of skin
infection.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
VEG, KM and DM conceptualized the study. AGk, PP,
PD, NG, NT and XT made substantial contributions to the
acquisition, analysis and interpretation of the data. CD and AGa
prepared the figures. All authors contributed to manuscript
revision and approved the final manuscript. PS and SC confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication.
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Brisset J, Daix T, Tricard J, Evrard B,
Vignon P, Barraud O and François B: Spontaneous community-acquired
PVL-producing Staphylococcus aureus mediastinitis in an
immunocompetent adult - a case report. BMC Infect Dis.
20(354)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chang CH, Huang JY, Lai PC and Yang CW:
Posterior mediastinal abscess in a hemodialysis patient - a rare
but life-threatening complication of Staphylococcus bacteremia.
Clin Nephrol. 71:92–95. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Calvano TP, Ferraro DM, Prakash V, Mende K
and Hospenthal DR: Community-associated methicillin-resistant
Staphylococcus aureus mediastinitis. J Clin Microbiol.
47:3367–3369. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gajdács M: The continuing threat of
methicillin-resistant Staphylococcus aureus. Antibiotics
(Basel). 8(52)2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Stefani S and Goglio A:
Methicillin-resistant Staphylococcus aureus: Related
infections and antibiotic resistance. Int J Infect Dis. 14 (Suppl
4):S19–S22. 2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Jabłoński S, Brocki M, Krzysztof K,
Wawrzycki M, Santorek-Strumiłło E, Łobos M and Kozakiewicz M:
Evaluation of prognostic value of selected biochemical markers in
surgically treated patients with acute mediastinitis. Med Sci
Monit. 18:CR308–CR315. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kimura A, Miyamoto S and Yamashita T:
Clinical predictors of descending necrotizing mediastinitis after
deep neck infections. Laryngoscope. 130:E567–E572. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Smith A and Sinzobahamvya N: Anterior
mediastinal abscess complicating septic arthritis. J Pediatr Surg.
27:101–102. 1992.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lin YY, Hsu CW, Chu SJ, Chen SC and Tsai
SH: Rapidly propagating descending necrotizing mediastinitis as a
consequence of intravenous drug use. Am J Med Sci. 334:499–502.
2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Er F, Nia AM, Caglayan E and Gassanov N:
Mediastinitis as a complication of central venous catheterization.
Infection. 38(509)2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Abu-Omar Y, Kocher GJ, Bosco P, Barbero C,
Waller D, Gudbjartsson T, Sousa-Uva M, Licht PB, Dunning J, Schmid
RA, et al: European Association for Cardio-Thoracic Surgery expert
consensus statement on the prevention and management of
mediastinitis. Eur J Cardiothorac Surg. 51:10–29. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Prado-Calleros HM, Jiménez-Fuentes E and
Jiménez-Escobar I: Descending necrotizing mediastinitis: Systematic
review on its treatment in the last 6 years, 75 years after its
description. Head Neck. 38 (Suppl 1):E2275–E2283. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
El Oakley RM and Wright JE: Postoperative
mediastinitis: Classification and management. Ann Thorac Surg.
61:1030–1036. 1996.PubMed/NCBI View Article : Google Scholar
|