Introduction
The conjunctiva is a thin and delicate mucous
membrane, lining the inner eyelid and the anterior surface of the
eyeball. Histologically, the conjunctival epithelium is composed of
two to five layers of columnar or cuboidal cells, mucin-secreting
goblet cells and melanocytes (1).
Since the ocular surface is exposed to numerous infectious and
noninfectious agents or allergens, hyperplastic changes can occur
due to nonspecific chronic inflammation of the conjunctiva
(2). Ohashi et al (3) reported of two cases of conjunctival
mucoepithelial hyperplasia amongst elderly patients. Specifically,
nodular lesions found on the internal canthus were presented in
both patients. Clinically, neoplasms were identified as
differential diagnoses in both cases; however the nodular lesions
were pathologically characterized by goblet cell hyperplasia and
chronic inflammation of the stroma. For neoplasms as differential
diagnoses, conjunctival squamous intraepithelial neoplasia (CSIN)
and squamous cell papilloma of the conjunctiva were more probable
diseases. CSIN shows dysplastic changes of the conjunctiva, located
at the limbus within the interpalpebral area, and is the most
common form of ocular surface neoplasia (4). Squamous cell papilloma of the
conjunctiva is a benign neoplasm characterized by an outgrowth of
epithelial and stromal elements of the conjunctiva; it is often
associated with human papilloma virus (HPV), and is more frequently
found in men and amongst patients aged 20-29 years (5). Although there are some case reports of
hyperplastic lesions in the conjunctiva, as a pathological entity,
conjunctival epithelial hyperplasia has not been sufficiently
established. Additionally, the immunohistochemical (IHC) features
of both the intact conjunctiva epithelium and conjunctival
epithelial hyperplasia have not been sufficiently evaluated. In the
present report, the case of a nodular lesion in the palpebral
conjunctiva is described. The component cells in the conjunctival
epithelium exhibited hyperplastic changes with minimal
inflammation, and showed squamous metaplasia in a segment of thick
conjunctiva. IHC analysis was performed to further characterize the
immunophenotype of the lesion and rule out differential diagnoses,
such as CSIN and squamous cell papilloma of the conjunctiva.
Case report
An 86-year-old man consulted with an ophthalmologist
for a 6-month-old nodular lesion on his left eye. Although the
nodular lesion had not grown during these 6 months, he started
feeling uncomfortable due to an increase in discharge from the eye
and blurring of vision. There were no other changes, such as
failing vision or limited eye movement. His past medical history
and family history were unremarkable. He had no allergies, did not
smoke and did not drink alcohol. The visual acuities [normal
>1.0(6)] of the right and left
eye were 0.8 and 1.2, respectively, indicating a mild decline in
the acuity of the right eye. Both intraocular pressures were 14
mmHg, which falls within the normal range [10-21 mmHg (7)]. Laboratory tests showed no
abnormalities, except for C-reactive protein (CRP) level, which was
0.15 mg/dl [0.00-0.14 mg/dl (8)].
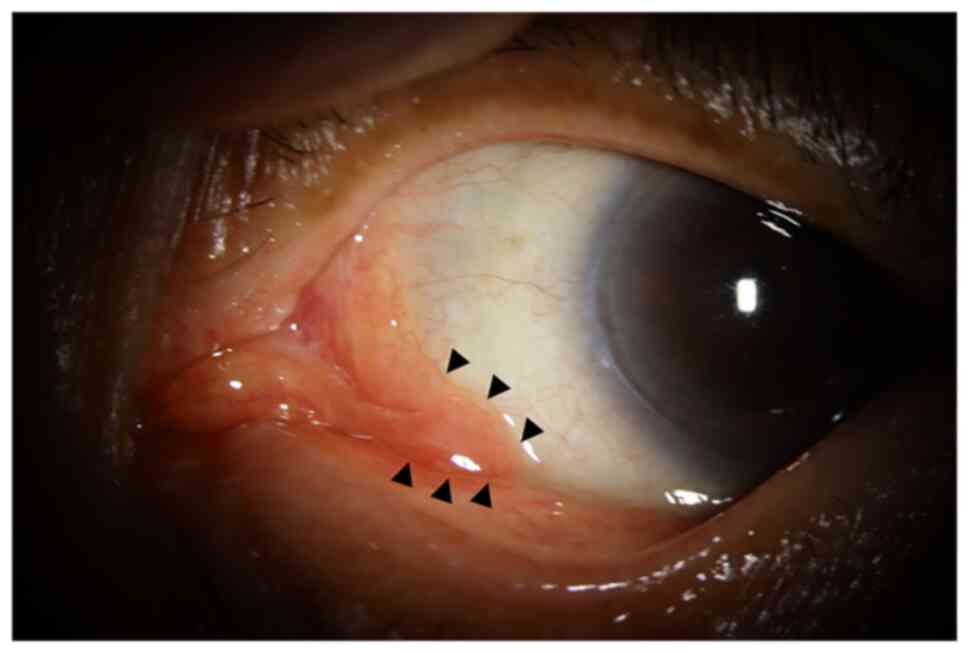
Located in the medial aspect of the left lower palpebral
conjunctiva, the lesion was slightly erythematous and smooth
(Fig. 1, black arrowhead). Although
CRP level was slightly elevated, based on the nodularity of the
lesion, hyperplasia rather than inflammation was a more probable
differential diagnosis. An excisional biopsy of the lesion was
performed to obtain a pathological diagnosis.
The tissue specimen was fixed in 10% neutral
buffered formalin, and then embedded in paraffin wax for
hematoxylin and eosin (H&E) staining. IHC analysis was
performed using Vectastain Elite ABC kits from Vector Laboratories,
Inc., according to the manufacturer's instructions for blocking,
secondary antibody dilution and labeling. The following primary
antibodies against cytokeratin (CK) markers were purchased: AE1/AE3
(clone AE1/AE3; Nichirei); CK5/6 (clone D5/16 B4), CK7 (clone OV-TL
12/30), and CK20 (Clone Ks20.8) all from Dako (Agilent
Technologies, Inc.); and anti p63 (clone 4A4; Nichirei) antibody, a
myoepithelial marker. The anti Ki-67 (clone MIB-1) antibody was
used to evaluate cell proliferation using a Dako system (Agilent
Technologies, Inc.). DAB (Sigma-Aldrich; Merck KGaA) was freshly
prepared from tablets for chromogenic staining at 20˚C for 10
min.
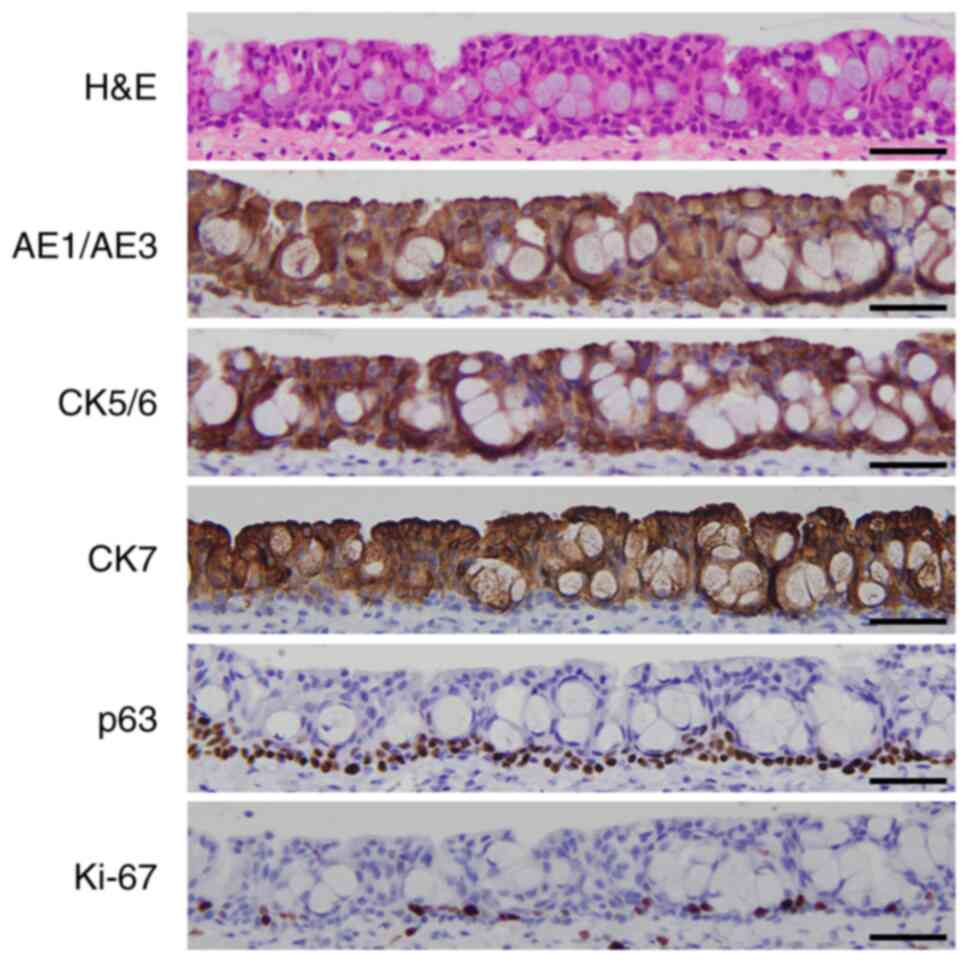
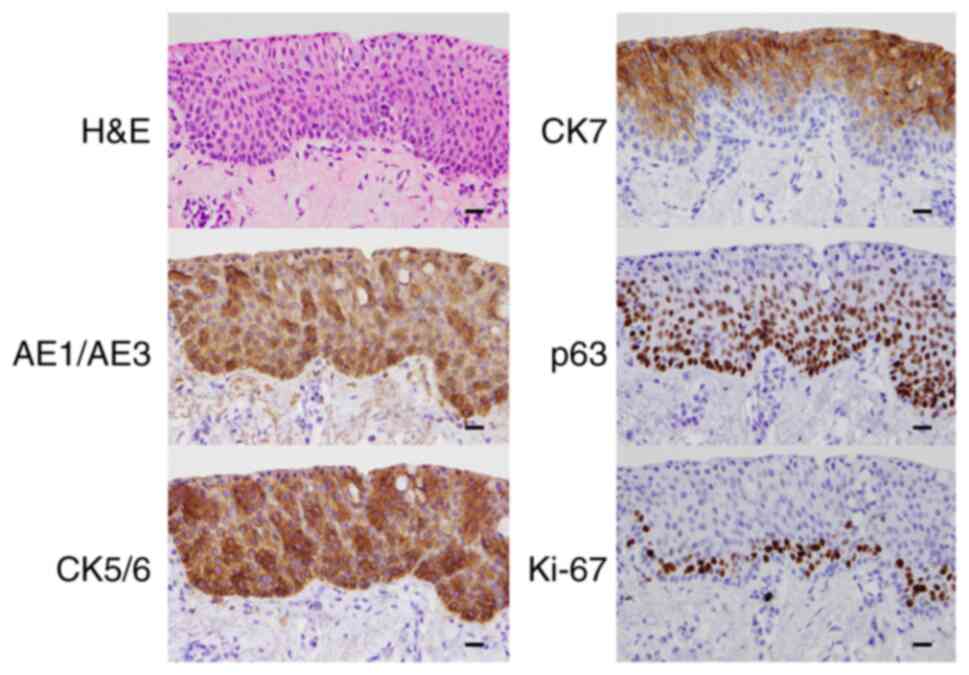
The H&E stained section of the intact part of
the palpebral conjunctiva showed a stratified epithelium composed
of two to seven layers of cuboidal cells with mucin-producing
goblet cells (Fig. 2). AE1/AE3
(intensity: +), CK5/6 (intensity: +) and CK7 (intensity: +) stained
positively in the epithelium (Fig.
2), whereas CK20 (intensity: -) was negative (data not shown).
p63-positive cells were detected in the basal and parabasal layers
(intensity: +). This indicated that the conjunctival epithelium had
basal cells similar to that of the respiratory epithelium.
Additionally, the proliferative zone of the epithelium was located
in the basal and parabasal layers, as indicated by Ki-67-positive
staining (Fig. 2).
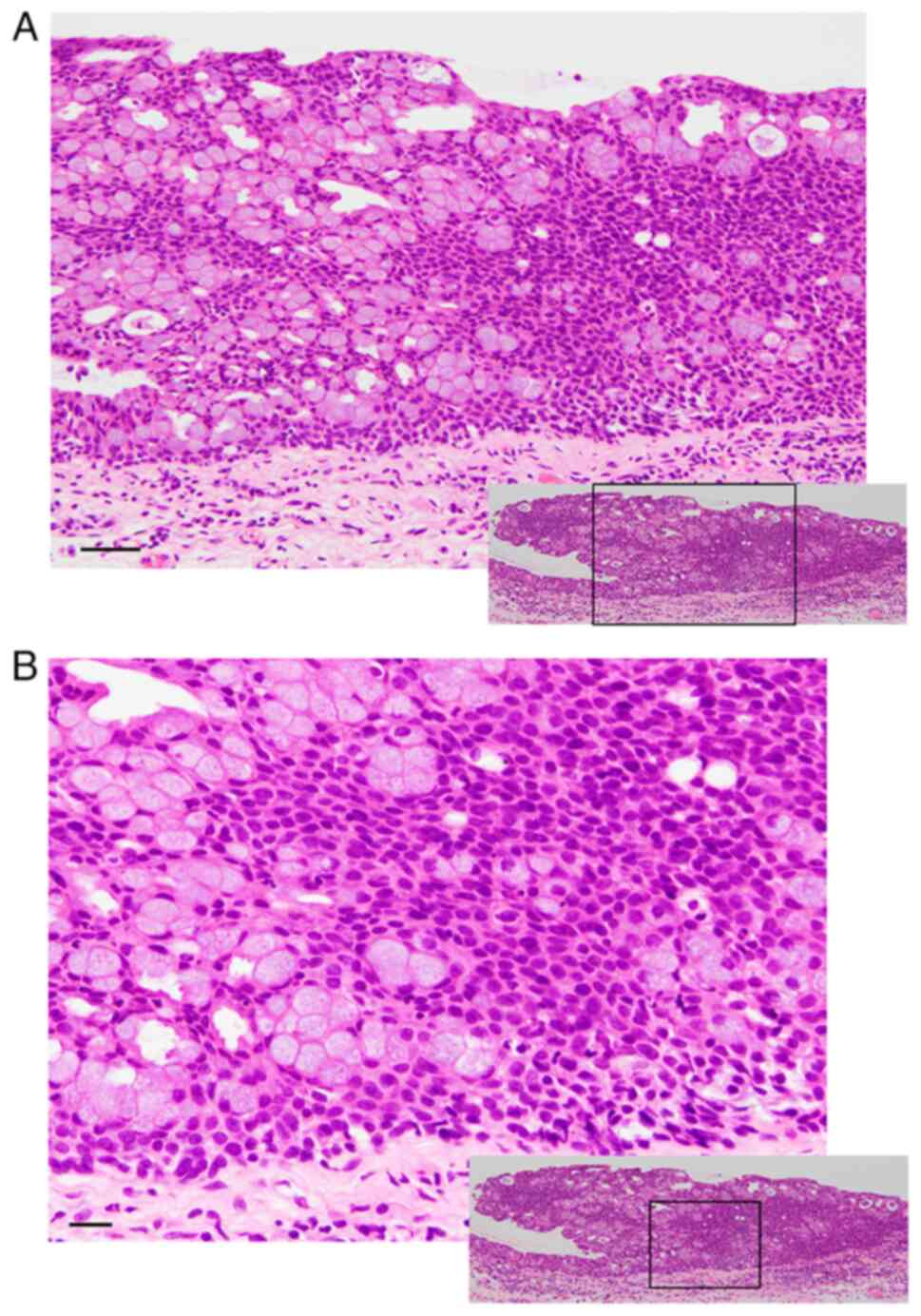
The H&E staining of the nodule revealed a
thickened conjunctival epithelium, composed of increased cuboidal
epithelial cells and goblet cells (Fig.
3A). Atypia and increased mitosis, indicative of neoplastic
changes, were not observed on high-magnification microscopy
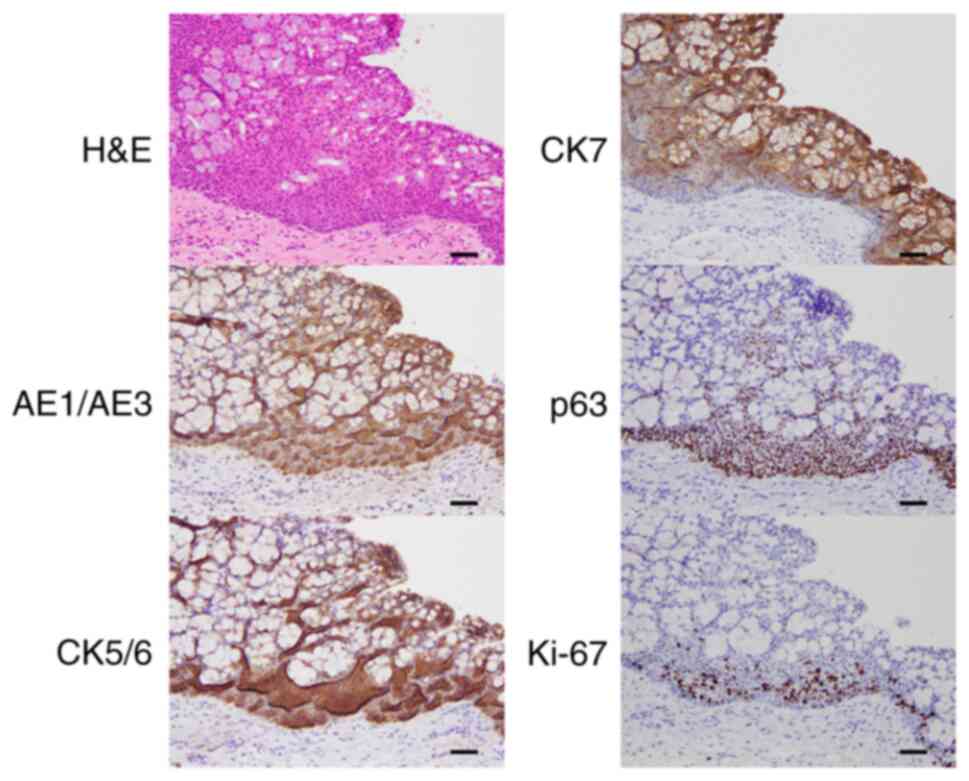
(Fig. 3B). As shown in Fig. 4, the thick conjunctival epithelium
consisted of epithelial cells that stained positive for CK [AE1/AE3
(intensity: +), CK5/6 (intensity: ++), and CK7 (intensity: +)] and
p63-positive basal cells (intensity: +). There were no large
sections of Ki-67-positive cells in the epithelium, so a tumorous
lesion was unlikely. These findings suggested hyperplasia of the
thick conjunctival epithelium. In Fig.
5, squamous metaplasia was detected in a segment of the thick
conjunctiva, the IHC features of which were similar to those of
hyperplasia (Fig. 4).
Discussion
Hyperplastic changes were detected in the cells
comprising the nodular lesion of the conjunctival epithelium. IHC
analysis was also performed. Ohashi et al (3) reported conjunctival mucoepithelial
hyperplasia amongst the elderly. These cases were characterized by
goblet cell hyperplasia with nonspecific chronic inflammation that
mimicked neoplastic lesions. In the present case, hyperplasia was
observed not only in the goblet cells but also in epithelial and
basal cells of the nodule. These findings led to the diagnosis of
conjunctival epithelial hyperplasia as a pathological entity, which
is a diagnosis that has not been sufficiently established yet.
As they are amongst the differential diagnoses for
the described lesion, CSIN and squamous cell papilloma of the
conjunctiva had to be ruled out. CSIN represents the in situ
precursor lesion of squamous cell carcinoma, which shows acanthosis
with loss of goblet cells, atypical keratinocytes and suprabasilar
mitotic figures. Immunophenotype of CSIN is AE1/AE3 positive, but
shows low expression of CK7. Usually, expression of p53 and Ki-67
is increased and appear in suprabasilar cells (4). In this described lesion, loss of
goblet cells, atypia, increased mitosis, decreased CK7 expression
and a broad distribution of Ki-67-positive cells were absent.
Additionally, expression of p53 was not increased, indicating
wild-type pattern (data not shown). Based on this data, CSIN was
excluded. Squamous cell papilloma of the conjunctiva is a benign
lesion caused by HPV and is typically an exophytic growth with
papillary proliferation of stratified squamous epithelium.
Koilocytosis (nuclear pyknosis and cytoplasmic clearing) is a
morphological hallmark of HPV infection (5). This lesion showed neither
papillomatous architecture nor koilocytosis, and squamous cell
papilloma was ruled out.
On immunohistochemistry, the epithelial cells in
both the intact conjunctiva and conjunctival epithelial hyperplasia
positively stained for AE1/AE3, CK5/6 and CK7, but not CK20.
AE1/AE3 antibody is a CK cocktail, referred to as a
‘pancytokeratin’. It detects both high (CK1-6, 10, 14, 15 and 16)
and low (CK7, 8, and 19) molecular weight keratins (9). CK5/6 (high molecular weight keratins)
antibody detects stratified and transitional epithelium,
proliferating squamous epithelium and mesothelial cells. The CK7
(low molecular weight keratin) antibody detects non-keratinizing
epithelia, except for those of the intestine, ectocervix, prostate,
and liver. CK20 is a low-molecular-weight keratin that identifies
the gastrointestinal and urothelial epithelia (10-12).
The IHC features of the intact conjunctiva and conjunctival
epithelial hyperplasia are similar to those of respiratory
epithelium in that both are CK7-positive and CK20-negative. CK5/6
was also positive in this case, indicating endogenous squamous
differentiation of the intact conjunctiva and conjunctival
epithelial hyperplasia.
Based on previous literature, the presence of basal
cells in the conjunctiva has received insufficient recognition. The
presence of p63, which is expressed in the basal epithelia of
multiple organs (13), was
evaluated in the intact conjunctiva. As shown in Fig. 2, the basal and parabasal layers
positively stained for p63. Ramalho et al (14) assessed the relationship between p63
and p16 expression in primary and recurrent pterygia and showed p63
positivity in the basal layer of the normal conjunctiva. The
results of the present case support the findings of Ramalho et
al (14), indicating the
presence of basal cells as well as respiratory epithelium (15).
In conclusion, the results of this investigation
suggest that ‘conjunctival epithelial hyperplasia’ should be
considered a pathological entity and indicate the presence of basal
cells in the conjunctiva. Further collection and analysis of other
cases of conjunctival epithelial hyperplasia can help elucidate its
characteristics, including prognostic data such as the recurrence
rate, and help in the development of prevention methods and
therapeutic drugs for this lesion.
Acknowledgements
The authors would like to thank Research Scientist
Yusuke Onishi (Department of Pathology, Faculty of Medicine, Osaka
Medical and Pharmaceutical University, Osaka, Japan) for technical
support with the IHC analyses.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SK designed this study, collected and analyzed data,
and wrote the manuscript; YY, KT and TK contributed to clinical
data acquisition and interpretation; YK and YH evaluated the
pathological findings and approved the final pathological
diagnosis. All authors have read approved the final manuscript. SK
and YK confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
Our institute does not require an approval for a
case report based on Ethical Guidelines for Medical and Health
Research Involving Human Subjects from the Japanese Ministry of
Health, Labour and Welfare. The patient provided written informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Proia AD and Cummings TJ: In: Mills SE
(ed). Histology for pathologists, 5th edition. Philadelphia,
Wolters Kluwer, pp335-361, 2020.
|
|
2
|
Eagle RC Jr: Conjunctiva. In: Eye
Pathology: An Atlas and Text, 3rd edition. Philadelphia, Wolters
Kluwer, pp90-133, 2016. Available from: https://www.proquest.com/legacydocview/EBC/5228949?accountid=38219.
|
|
3
|
Ohashi A, Elsayed AA, Yasuma T, Iijima T
and Nakamura S: Conjunctival mucoepithelial hyperplasia of the
elderly. Int Ophthalmol. 35:611–614. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Reese A and Margo CE: Conjunctival
squamous intraepithelial neoplasia and its differential diagnosis.
J Clin Pathol, Feb 22, 2021 (Epub ahead of print).
|
|
5
|
Kalogeropoulos C, Koumpoulis I, Papadiotis
E, Zioga A, Gkrepi K, Pappa C, Paschides C, Malamou-Mitsi V and
Aspiotis M: Squamous cell papilloma of the conjunctiva due to human
papillomavirus (HPV): Presentation of two cases and review of
literature. Clin Ophthalmol. 6:1553–1561. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huang L, Kawasaki H, Yasuda R and Sakai R:
Relationship between visual acuity and lifestyle: A cross-sectional
study in Japanese children. Hiroshima J Med Sci. 67:105–111.
2018.
|
|
7
|
Wang YX, Xu L, Wei WB and Jonas JB:
Intraocular pressure and its normal range adjusted for ocular and
systemic parameters. The Beijing eye study 2011. PLoS One.
13(e0196926)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ozaka S, Kodera T, Ariki S, Kobayashi T
and Murakami K: Acute pancreatitis soon after COVID-19 vaccination:
A case report. Medicine (Baltimore). 101(e28471)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Badzio A, Czapiewski P, Gorczyński A,
Szczepańska-Michalska K, Haybaeck J, Biernat W and Jassem J:
Prognostic value of broad-spectrum keratin clones AE1/AE3 and
CAM5.2 in small cell lung cancer patients undergoing pulmonary
resection. Acta Biochim Pol. 66:111–114. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Moll R, Franke WW, Schiller DL, Geiger B
and Krepler R: The catalog of human cytokeratins: Patterns of
expression in normal epithelia, tumors and cultured cells. Cell.
31:11–24. 1982.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bragulla HH and Homberger DG: Structure
and functions of keratin proteins in simple, stratified,
keratinized and cornified epithelia. J Anat. 214:516–559.
2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Karantza V: Keratins in health and cancer:
More than mere epithelial cell markers. Oncogene. 30:127–138.
2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Dewar R, Fadare O, Gilmore H and Gown AM:
Best practices in diagnostic immunohistochemistry: Myoepithelial
markers in breast pathology. Arch Pathol Lab Med. 135:422–429.
2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ramalho FS, Maestri C, Ramalho LNZ,
Ribeiro-Silva A and Romão E: Expression of p63 and p16 in primary
and recurrent pterygia. Graefe's Arch Clin Exp Ophthalmol.
244:1310–1314. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Steurer S, Riemann C, Büscheck F, Luebke
AM, Kluth M, Hube-Magg C, Hinsch A, Höflmayer D, Weidemann S,
Fraune C, et al: p63 expression in human tumors and normal tissues:
A tissue microarray study on 10,200 tumors. Biomark Res.
9(7)2021.PubMed/NCBI View Article : Google Scholar
|