Introduction
Drug overdose is one of the common events
encountered in the emergency department (ED). In 2018, 67,367 drug
overdose-related deaths were reported in the United States, and the
age-adjusted rate of drug overdose deaths was 20.7 per 100,000
population according to the data from the United States Centre for
Disease Control and Prevention. The rates were higher in men than
in women. In 2018, the age-adjusted rate of drug overdose deaths
was 27.9 in men, while that in women was 13.6(1).
The incidence of overdose in Taiwan is 0.16-0.22 per
1,000 population according to the Taiwan National Poison Centre
(2). In addition, the mortality
rate associated with poisoning is relatively high, which ranks
fourth among unintentional injuries, of which the top three causes
are automobile injuries, unintentional falls, and drowning
(3). Even though drug
overdose-related deaths have garnered considerable public
attention, the complications of nonfatal overdose including
cognitive impairment, cardiac and muscular problems, renal failure,
hearing loss, and other injuries should also be taken into
consideration (4,5). The average hospital cost of overdosed
patients who were treated and admitted is also notably high
(6).
Qin et al reported that although several
studies have sought to interpret the sex gap in suicidal behavior,
where unemployment, retirement, being single, and interpersonal
conflicts were all significant risk factors for suicide in men, no
significant risk factors other than mental illness were reported in
women (7,8). However, having a child aged <2
years was a significant protective factor against suicide in women
(8).
Therefore, the predisposing factors for drug
overdose should be recognized. In addition, the sex difference and
predisposing factors of overdose occurring in the ED should be
investigated.
Materials and methods
Patients and drugs
Data of patients with self-poisoning admitted to the
ED from January 2018 to August 2019 were retrospectively analyzed.
This project was approved by the Ethics Committee of Mackay
Memorial Hospital (Taipei, Taiwan), while the study was approved
(approval no. 19MMHIS288e) by the Institutional Review Board of
Mackay Memorial Hospital. The study cases were selected using the
following International Statistical Classification of Diseases and
Related Health Problems, 10th Revision, (ICD-10) coding system
(9): poisoning by, adverse effect
of and underdosing of systemic antibiotics (T36); other systemic
anti-infectives and antiparasitics (T37); hormones and their
synthetic substitutes and antagonists (T38); nonopioid analgesics,
antipyretics, and antirheumatics (T39); narcotics and
psychodysleptics (hallucinogens) (T40); anesthetics and therapeutic
gases (T41), antiepileptic, sedative-hypnotics, and
antiparkinsonism drugs (T42); psychotropic drugs (T43); drugs
primarily affecting the autonomic nervous system (T44); primarily
systemic and hematological agents (T45); agents primarily affecting
the cardiovascular system (T46); agents primarily affecting the
gastrointestinal system (T47); agents primarily acting on the
smooth and skeletal muscles and the respiratory system (T48);
topical agents primarily affecting the skin and mucous membrane and
ophthalmological, otorhinolaryngological, and dental drugs (T49);
and diuretics and other and unspecified drugs, medicaments, and
biological substances (T50).
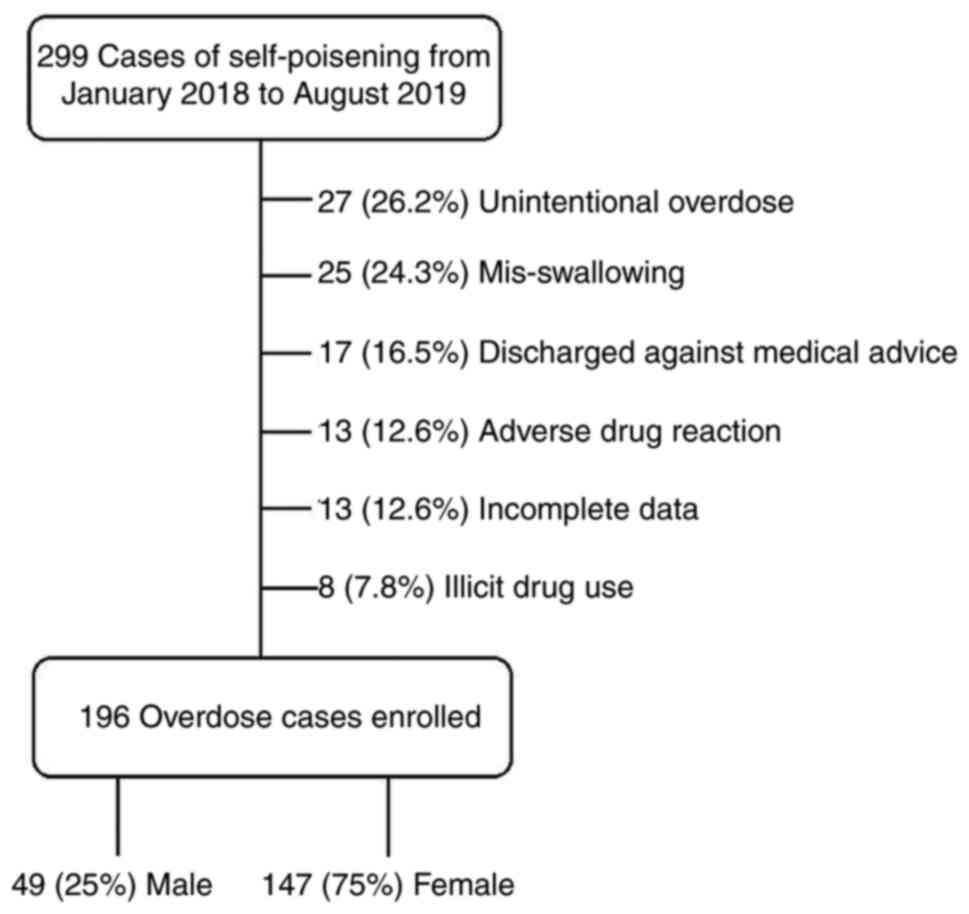
Data of 299 patients with self-poisoning were
collected from January 2018 to August 2019. A total of 196
intentional overdose patients were enrolled, while 103 patients
were excluded (Fig. 1). The
exclusion criteria were as follows: Patients who had unintentional
overdose, experienced mis-swallowing, developed an accidental
adverse drug reaction (ADR), were discharged from the ED without
complete treatment, and with incomplete data (Fig. 1). The following data were collected
and analyzed: Glasgow Coma Scale (GCS) scores and vital signs upon
arrival (including body temperature, heart rate, systolic blood
pressure (SBP), and diastolic blood pressure (DBP), sex, age,
marital status, arrival time, season on admission, previous suicide
attempts, psychiatric history, related comorbidities, recent
arguments, categories of overdose with or without concurrent
ethanol use, length of hospital stay, and survival to
discharge.
Statistical analysis
A statistical software (IBM SPSS Statistics for
Windows, version 20.0; IBM Corp.) was used to perform all data
analyses. Both unpaired Student's t-test and chi-square test
were used in the statistical analyses, and a P-value of <0.05
was considered to indicate a statistically significant
difference.
Results
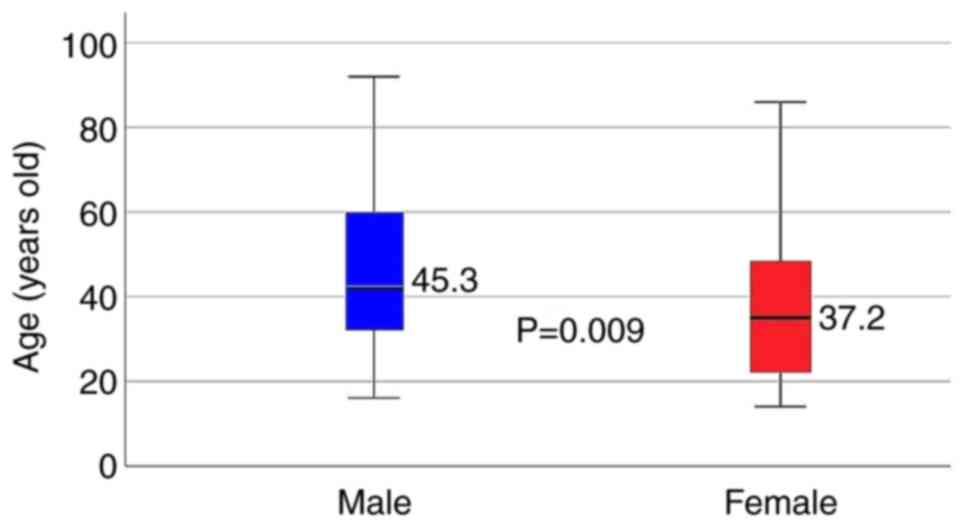
The 196 enrolled patients were aged 14-92 years
[mean ± standard deviation (SD)]: 39.2±18.3), and the male to
female ratio was 1:3 (men, n=49; women, n=147). The data revealed
that male intentional overdose patients were 8.1 years older than
their female counterparts (45.3±19.5 vs. 37.2±17.5, respectively;
P=0.009) (Fig. 2 and Table I). In comparison with female
patients, 6.1% (3/49) of the male patients tended to have
premeditated drug overdose after arguing with a girlfriend, which
had a significant difference (P<0.05). Moreover, more than half
of the overdose patients were single (n=117, 59.2%; Table I), which was considered as one of
the risk factors of overdose.
 | Table IDifferences between male and females
patients in 196 cases of intentional overdose from January 2018 to
August 2019. |
Table I
Differences between male and females
patients in 196 cases of intentional overdose from January 2018 to
August 2019.
| Intentional
overdose | All | Male | Female | P-value
(two-tailed) |
|---|
| n (%) | 196(100) | 49(25) | 147(75) | |
| Age (years old) | 39.2±18.3 | 45.3±19.5 | 37.2±17.5 | 0.009a |
| Times of
overdose | 1.2±0.7 | 1.1±0.3 | 1.2±0.8 | 0.339 |
| Seasons (n, %) | | | |
<0.001a |
|
Spring | 63 (32.1) | 28 (57.1) | 35 (23.8) | |
|
Summer | 43 (21.9) | 5 (10.2) | 38 (25.9) | |
|
Autumn | 45 (23.0) | 6 (12.2) | 39 (26.5) | |
|
Winter | 45 (32.0) | 10 (20.5) | 35 (23.8) | |
| Arrival time | | | | 0.127 |
|
Day | 55 (28.1) | 16 (32.7) | 39 (26.5) | |
|
Evening | 78 (39.8) | 23 (46.9) | 55 (37.4) | |
|
Night | 63 (32.1) | 10 (20.4) | 53 (36.5) | |
| History of prior
overdose | 63 (32.1) | 13 (26.5) | 50(34) | 0.331 |
| Marriage status | | | | |
|
Single | 117 (59.2) | 27 (55.1) | 90 (61.2) | 0.507 |
|
Marriage | 60 (30.6) | 19 (38.8) | 41 (27.9) | 0.157 |
|
Divorced | 19 (9.7) | 3 (6.1) | 16 (10.9) | 0.329 |
|
Alcohol-drinking | 54 (27.6) | 19 (38.8) | 35 (23.8) | 0.113 |
| Body temperature
(˚C) | 36.6±0.6 | 36.5±0.5 | 36.7±0.6 | 0.026a |
| Heart rate (beats
per min) | 88.9±19.9 | 89.1±16.9 | 88.9±20.9 | 0.583 |
| Systolic blood
pressure (mmHg) | 116.9±21.2 | 123.1±20.1 | 114.9±21.3 | 0.014a |
| Diastolic blood
pressure (mmHg) | 68.7±14.4 | 75.1±15.6 | 66.6±13.4 | 0.001a |
| Glasgow Coma
Scale | 12.9±3.6 | 13.1±3.4 | 12.8±3.7 | 0.676 |
| Hypertension | 21 (10.7) | 6 (12.2) | 15 (10.2) | 0.689 |
| Diabetes
mellitus | 14 (7.1) | 5 (10.2) | 9 (6.1) | 0.337 |
| Uremia | 3 (1.5) | 1(2) | 2 (1.4) | 0.737 |
| Depression | 96(50) | 23 (46.9) | 73 (49.7) | 0.741 |
| Personality
disorder | 75 (38.3) | 23 (46.9) | 52 (35.4) | 0.149 |
| Bipolar affective
disorder | 25 (12.8) | 4 (8.2) | 21 (14.3) | 0.266 |
| Schizophrenia | 10 (5.1) | 1(2) | 9 (6.1) | 0.261 |
| Argument with
family members | 62 (31.6) | 17 (34.7) | 45 (30.6) | 0.595 |
| Argument with
father | 10 (5.1) | 4 (8.2) | 6 (4.1) | 0.261 |
| Argument with
mother | 13 (6.6) | 1 (2.0) | 12 (8.2) | 0.136 |
| Argument with
friends | 43 (21.9) | 8 (16.3) | 35 (23.8) | 0.273 |
| Argument with
boyfriend | 4 (2.0) | 0 (0) | 4 (2.7) | 0.243 |
| Argument with
girlfriend | 3 (1.5) | 3 (6.1) | 0 (0) | 0.003a |
| Conflict with
co-workers | 10 (5.1) | 4 (8.2) | 6 (4.1) | 0.454 |
| Suffering from
insomnia | 79 (40.3) | 20 (40.8) | 59 (40.1) | 0.933 |
| Hospitalization in
the Toxicology ward | 22 (11.2) | 4 (8.2) | 18 (12.2) | 0.433 |
| Intensive care unit
admission | 4(2) | 1(2) | 3(2) | 1.000 |
| Length of stay
(days) | 2.0±4.1 | 2.1±4.2 | 2.0±4.1 | 0.183 |
Most intentional overdose cases occurred during the
spring season (n=63, 32.1%), especially in male patients (n=28,
57.1%; P<0.001). The majority of patients (n=78, 39.8%) were
sent to our ED in the evening (from 15:00 to 23:00 p.m.). In 31.6%
(62/196) of overdose patients, an argument with a family member
motivated them to commit a premeditated drug suicide attempt
(Table I).
Benzodiazepines (n=96, 49%; P=0.004) were the most
common drugs used in intentional overdose. In addition,
approximately 8.2% of female patients (12/147) committed
self-poisoning using acetaminophen (Table II). A great number of intentional
overdose patients had a history of depression (n=96, 49%) and
insomnia problems (n=79, 40.3%) (Table
I). Only 27.6% of the patients (54/196) reported concurrent use
of alcohol (Table I).
 | Table IISubstances involved in intentional
overdose. |
Table II
Substances involved in intentional
overdose.
| Substance of
overdose n, (%) | N=196, (100%) | Males, n=49
(25%) | Females, n=147
(75%) |
|---|
|
Benzodiazepinesa | 62 (31.6) | 20 (41.0) | 42 (28.5) |
| Flunitrazepam | 10 (5.1) | 3 (6.2) | 7 (4.7) |
| Estazolam | 7 (3.6) | 2(4) | 5 (3.4) |
| Alprazolam | 4 (2.1) | 1(2) | 3(2) |
| Lorazepam | 3 (1.6) | 2(4) | 1 (0.7) |
| Bromazepam | 1 (0.5) | 0 (0) | 1 (0.7) |
| Clonazepam | 1 (0.5) | 1(2) | 0 (0) |
| Mixed
medications | 63 (32.1) | 9 (18.8) | 54 (36.6) |
| Acetaminophen | 12 (6.1) | 0 (0) | 12 (8.2) |
| Non-benzodiazepine
hypnotics | 6 (3.1) | 2(4) | 4 (2.7) |
| Zolpidem | 5 (2.6) | 0 (0) | 5 (3.4) |
| Stilnox | 4 (2.1) | 2(4) | 2 (1.4) |
|
Anti-depressants | 2(1) | 0 (0) | 2 (1.4) |
|
Diphenhydramine | 2(1) | 0 (0) | 2 (1.4) |
| Amphetamine | 2(1) | 2(4) | 0 (0) |
| Baclofen | 1 (0.5) | 0 (0) | 1 (0.7) |
| Bromadiolone | 1 (0.5) | 0 (0) | 1 (0.7) |
| Bupropion | 1 (0.5) | 0 (0) | 1 (0.7) |
| Gasoline | 1 (0.5) | 1(2) | 0 (0) |
| Humalog Mix
(Insulin) | 1 (0.5) | 1(2) | 0 (0) |
| Iron | 1 (0.5) | 1(2) | 0 (0) |
| Ketamine | 1 (0.5) | 0 (0) | 1 (0.7) |
| Norvasc | 1 (0.5) | 0 (0) | 1 (0.7) |
| Quetiapine
(anti-psychotics) | 1 (0.5) | 1(2) | 0 (0) |
| Sertraline | 1 (0.5) | 0 (0) | 1 (0.7) |
| Valsartan | 1 (0.5) | 0 (0) | 1 (0.7) |
| Zolpiclone | 1 (0.5) | 1(2) | 0 (0) |
| Total | 196 | 49 | 147 |
Body temperature (in ˚C) was slightly higher in
female patients than in male patients (mean ± SD, 36.7±0.6 vs.
36.5±0.5, respectively; P=0.026). Our study also revealed
significantly higher levels of systolic and diastolic blood
pressure in male patients compared with female patients. No
significant differences were found in the marital status,
comorbidities, and concurrent psychiatric diseases between the two
sex groups (Table I).
Approximately 11.2% (22/196) and 2% (4/196) of total
patients were admitted to the Toxicology ward and intensive care
units, respectively (Table I). The
length of hospital stay was 2±4.1 days, and none of the patients in
our study succumbed to intentional drug overdose.
Discussion
Comparison in the rate of drug
overdose between men and women during the spring season
One of our interesting results indicated that
intentional drug overdose mostly occurred during the spring season.
Numerous studies also revealed that suicide rates peaked during the
spring season (10). The sudden
increase in the duration and amount of sunlight is a conceivable
reason for these phenomena. Hakko et al reported a 9%
increase in the suicide rates in spring and an 8% increase in fall
within the non-violent (i.e., ingestion of poisons, drugs, gases,
or vapors) subgroup (11). This
finding is compatible with the present data; notably, the overdose
rate increased during the spring season, in both sex groups (32.1%)
and particularly in men (57.1%) with statistical significance. A
study conducted in Iran revealed that seasonal peaks and troughs
were also observed in medication use and self-poisoning rates
during spring and winter (12). In
the present study, 57.1% of male patients tended to commit suicide
by drug overdose during the spring season. Rocchi et al
indicated that suicide cases had a seasonal peak distribution in
both men and women during the spring season (13). A study conducted in Greece revealed
that suicide attempts in men increased during spring and summer and
significantly decreased in September (14). A previous study reported that the
rates of suicide attempts among men only peaked during spring,
while cases in women peaked during spring and fall (15). A study by Mann reported that
seasonal variance in suicide rates depends on an underlying
seasonal biological variance, which affects the control of
impulses. Such variance was mostly related to the serotonergic
(5-HT) circuits since the brain levels of serotonin are sensitive
to climate change; a clear seasonal rhythm is evident in
serotonergic functions. Abnormalities in the number of serotonergic
neurons, serotonin transportation, receptor binding, and serotonin
levels in key brain areas have all been linked to suicide (16). Functional imaging studies have
demonstrated decreased serotonin transporter binding in patients
who attempted suicide (17). Thus,
low levels of serotonin are often associated with impulsive and
aggressive behavior.
Sex difference in overdose by
physiology
The body temperatures of self-poisoned women were
slightly higher (0.2˚C) than those of male patients. Several
factors cause variations in body temperature including sex-based
variation, thus indicating that women have a higher body
temperature than men (18). Body
temperature is also sensitive to changes in hormone levels, and
women exhibit elevation in body temperature of ~0.9˚ Fahrenheit (F)
during ovulation (19). By
contrast, the blood pressure of overdosed male patients was higher
than that of female patients. A previous study reported that the
blood pressure, measured through 24-h ambulatory blood pressure
monitoring, is higher in men than in women at similar ages
(20). Increased body temperature
and blood pressure mostly related to overdose from stimulants
(i.e., cocaine, amphetamine, and methamphetamine). In our study,
most patients were intentionally overdosed with benzodiazepines,
which would not significantly increase the body temperature and
blood pressure. Therefore, the elevated body temperature in women
and blood pressure in men might be a physiological effect rather
than a manifestation of a drug overdose.
Age distribution between drug overdose
male and female patients
Notably, in the present study, women had a threefold
increased risk for premeditated drug overdose than men. Veisani
et al indicated that the majority of non-violent suicide
victims were women (21). Another
study showed that poisoning was the most common non-violent
suicidal method of women (22). In
addition, the WHO/EURO Multicenter study on parasuicides indicated
that the seasonal pattern of suicide attempts in women showed a
peak in spring and nadir in winter (23). However, no significant difference
was noted in the incidence of self-poisoning among the four
seasons. In the present study, older male patients had a greater
tendency to self-poison compared with older women (P<=0.009, for
the pooled sample and men and women) despite the increased risk of
intentional overdose among women. A study in Taiwan revealed that
the mean age of suicidal victims was 49.4 (±18.3) years, and more
than half of non-violent (54.9%) suicidal victims were aged between
35 to 64 years (24). In the
present study, the mean age of male overdose patients was 8.1 years
older than that of female overdose patients with statistical
significance.
Comparison of the drug overdose rate
between men and women facing conflicts
Male patients had an obvious tendency to have
premeditated drug overdose after arguing with their girlfriends.
Although relationship breakdown is a known risk factor for suicide,
men and women may not be equally susceptible (25,26).
In a previous study by Kposowa, it was reported that divorced men
had an 8-fold increased risk of committing suicide than divorced
women (27). A study in Korea
indicated that interpersonal conflict is the most common
precipitating factor for committing suicide in adolescents, whereas
family conflict is one of main risk factors in older people
(28). People with unsettled
conflicts have a higher level of suicidal ideation, hopelessness,
and depression than those who could deal with their partner
harmoniously (29). Furthermore,
men have been taught to live independent lives and act decisively
without approaching others in time of need (30). The expression of suicidal ideation
in men may be deemed as a sign of weakness. Thus, men are
particularly vulnerable and avoid seeking help as an impact of
hegemonic masculinity (31),
whereas women are more likely to seek help (32). A study by Pollack in 2006, implied
that boys are imbued with hiding their emotions between the ages of
3 and 5 years by enforcing a ‘boy code’, which rewards toughness
and enforces prohibition against emotional expression or
vulnerability (33). Although
depression is a well-known risk factor for suicide (34), men do not realize this when they are
depressed because men are expected to be in control at all times of
their emotions and actions (35).
This explains in part how the dynamics of male suicide continue to
be underestimated and poorly understood.
Overdose is commonly observed in daily emergency
practice. To prevent patients from engaging in intentional
overdose, determining the epidemiology and predisposing factors is
of utmost importance. The top three types of substances commonly
ingested in overdose amounts are benzodiazepine (42.9%), mixed
medications (32.1%), and acetaminophen (6.1%). In the present
study, 11.2% of overdosed patients required hospitalization, while
2% were admitted to the intensive care unit. The length of stay was
2±4.1 days.
Male drug overdose patients were 8.1 years older
than female patients, and drug overdose was 2.4-fold higher in men
than in women during the spring season. Men had a 2.3-fold
increased risk of drug overdose while facing conflicts than women.
Hence, physicians should notify the suicide prevention centers to
be on alert for middle-aged men, facing conflicts, especially
during the spring season.
At present, drug overdose is a frequent occurrence
in clinical practice. Investigations, such as the present study,
with the potential to reduce the risk of death due to a drug
overdose, are invaluable.
In addition, although various factors can influence
the drug overdose rate, the tendency to engage in such act varies.
In addition, men and women may overdose on drugs depending on the
factors such as age and season; hence, in the future, continuous
and strengthened follow-up investigations are expected to be
undertaken from the authors of the present study.
Acknowledgements
Not applicable.
Funding
Funding: This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit
sectors.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
STT collected the data, wrote the draft, and
discussed the manuscript. CHLo and CHLi collected the data and
wrote the draft. YJS designed the study, collected the data,
performed the statistical analyses, and discussed the manuscript.
All authors confirm the authenticity of all the raw data. All
authors have read and approved the final version of the manuscript
to be published.
Ethics approval and consent to
participate
The present study was approved (approval no.
19MMHIS288e) by the Institutional Review Board of Mackay Memorial
Hospital (Taipei, Taiwan).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hedegaard H, Miniño AM and Warner M: Drug
Overdose Deaths in the United States, 1999-2018. NCHS Data Brief.
National Center for Health Statistics, Hyattsville, MD, 2020.
|
|
2
|
Yang CC, Wu JF, Ong HC, Hung SC, Kuo YP,
Sa CH, Chen SS and Deng JF: Taiwan National Poison Center:
Epidemiologic data 1985-1993. J Toxicol Clin Toxicol. 34:651–663.
1996.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chien WC, Lin JD, Lai CH, Chung CH and
Hung YC: Trends in poisoning hospitalization and mortality in
Taiwan, 1999-2008: a retrospective analysis. BMC Public Health.
11(703)2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Darke S, Williamson A, Ross J, Mills KL,
Havard A and Teesson M: Patterns of nonfatal heroin overdose over a
3-year period: Findings from the Australian treatment outcome
study. J Urban Health. 84:283–291. 2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Schweitzer VG, Darrat I, Stach BA and Gray
E: Sudden bilateral sensorineural hearing loss following
polysubstance narcotic overdose. J Am Acad Audiol. 22:208–214.
2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Pattanaik S, Dhamija P, Malhotra S, Sharma
N and Pandhi P: Evaluation of cost of treatment of drug-related
events in a tertiary care public sector hospital in Northern India:
A prospective study. Br J Clin Pharmacol. 67:363–369.
2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Qin P, Agerbo E, Westergård-Nielsen N,
Eriksson T and Mortensen PB: Gender differences in risk factors for
suicide in Denmark. Br J Psychiatry. 177:546–550. 2000.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tóth MD, Ádám S, Birkás E, Székely A,
Stauder A and Purebl G: Gender differences in deliberate
self-poisoning in Hungary: Analyzing the effect of precipitating
factors and their relation to depression. Crisis. 35:145–153.
2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
International Statistical Classification
of Diseases and Related Health Problems, 10th revision, 5th
edition. Vol 2, 2010. WHO Library Cataloguing-in-Publication Data,
2010.
|
|
10
|
Jee HJ, Cho CH, Lee YJ, Choi N, An H and
Lee HJ: Solar radiation increases suicide rate after adjusting for
other climate factors in South Korea. Acta Psychiatr Scand.
135:219–227. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hakko H, Räsänen P and Tiihonen J:
Seasonal variation in suicide occurrence in Finland. Acta Psychiatr
Scand. 98:92–97. 1998.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Amiri B, Pourreza A, Rahimi Foroushani A,
Hosseini SM and Poorolajal J: Suicide and associated risk factors
in Hamadan province, west of Iran, in 2008 and 2009. J Res Health
Sci. 12:88–92. 2012.PubMed/NCBI
|
|
13
|
Rocchi MB, Sisti D, Cascio MT and Preti A:
Seasonality and suicide in Italy: Amplitude is positively related
to suicide rates. J Affect Disord. 100:129–136. 2007.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Vougiouklakis T, Boumba VA, Mitselou A,
Peschos D and Gerontopoulos K: Trends in suicide mortality in the
deprived region of Epirus (north-west Greece) during the period
1998-2002. Med Sci Law. 45:39–46. 2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Preti A, Miotto P and De Coppi M: Season
and suicide: Recent findings from Italy. Crisis. 21:59–70.
2000.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Mann JJ: The serotonergic system in mood
disorders and suicidal behaviour. Philos Trans R Soc Lond B Biol
Sci. 368(20120537)2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Miller JM, Hesselgrave N, Ogden RT,
Sullivan GM, Oquendo MA, Mann JJ and Parsey RV: Positron emission
tomography quantification of serotonin transporter in suicide
attempters with major depressive disorder. Biol Psychiatry.
74:287–295. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sund-Levander M, Forsberg C and Wahren LK:
Normal oral, rectal, tympanic and axillary body temperature in
adult men and women: A systematic literature review. Scand J Caring
Sci. 16:122–128. 2002.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mackowiak PA: Temperature regulation and
pathogenesis of fever. In: Douglas and Bennett's Principles and
Practice of Infectious Diseases. Mandell GL, Bennett's JE and Dolin
R (eds). 6th edition. Elsevier-Churchill Livingstone, pp703-717,
2005.
|
|
20
|
Wiinberg N, Høegholm A, Christensen HR,
Bang LE, Mikkelsen KL, Nielsen PE, Svendsen TL, Kampmann JP, Madsen
NH and Bentzon MW: 24-h Ambulatory blood pressure in 352 normal
Danish subjects, related to age and gender. Am J Hypertens.
8:978–986. 1995.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Veisani Y, Delpisheh A, Sayehmiri K,
Moradi G and Hassanzadeh J: Seasonality in violent and nonviolent
methods of suicide attempts: A CrossSectional study on systematic
registry data. Acta Med Iran. 55:507–513. 2017.PubMed/NCBI
|
|
22
|
Bando DH, Brunoni AR, Fernandes TG,
Benseñor IM and Lotufo PA: Suicide rates and trends in São Paulo,
Brazil, according to gender, age, and demographic aspects: A
joinpoint regression analysis. Braz J Psychiatry. 34:286–293.
2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Jessen G, Andersen K, Arensman E,
Bille-Brahe U, Crepet P, De Leo D, Hawton K, Haring C, Hjelmeland
H, Michel K, et al: Temporal fluctuations and seasonality in
attempted suicide in Europe. Arch Suicide Res. 5:57–69. 1999.
|
|
24
|
Chung KH, Lee HC, Kao S and Lin HC:
Urbanicity and methods of suicide: A nationwide population-based
study. J Urban Health. 85:136–145. 2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Corcoran P and Nagar A: Suicide and
marital status in Northern Ireland. Soc Psychiatry Psychiatr
Epidemiol. 45:795–800. 2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ide N, Wyder M, Kõlves K and De Leo D:
Separation as an important risk factor for suicide: A systematic
review. J Fam Issues. 31:1689–1716. 2010.
|
|
27
|
Kposowa AJ: Divorce and suicide risk. J
Epidemiol Commun Health. 57(993)2003.
|
|
28
|
Kweon YS, Hwang S, Yeon B, Choi KH, Oh Y,
Lee HK, Lee CT and Lee KU: Characteristics of drug overdose in
young suicide attempters. Clin Psychopharmacol Neurosci.
10:180–184. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Clapperton A, Newstead S, Bugeja L and
Pirkis J: Relative risk of suicide following exposure to recent
stressors, Victoria, Australia. Aust N Z J Public Health.
43:254–260. 2019.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Murphy GE: Why women are less likely than
men to commit suicide. Compr Psychiatry. 39:165–175.
1998.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Cohen D: ‘The American National
Conversation about (Everything but) Shame.’. Soc Res. 70:1073–1108.
2003.
|
|
32
|
Thoits PA: ‘Self, identity, and mental
health’. In: Handbook of the Sociology of Mental Health. Aneshenel
CS, Phelan JC and Avinson WR (eds). Springer, New York, NY,
pp357-377, 2013.
|
|
33
|
Pollack WS: The ‘war’ for boys: Hearing
‘real boys’ voices, healing their pain. Professional Psychology.
37:190–195. 2006.
|
|
34
|
Borges G, Orozco R and Medina Mora ME:
Risk index for attempted suicide in Mexico. Salud Publica Mex.
54:595–606. 2012.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
35
|
Rasmussen ML, Hjelmeland H and Dieserud G:
Barriers toward help-seeking among young men prior to suicide.
Death Stud. 42:96–103. 2018.PubMed/NCBI View Article : Google Scholar
|