Introduction
Appendiceal mucocele is a type I tumor of epithelial
origin that can be caused by a number of factors, such as chronic
inflammation or the presence of a bezoar, and it can make the
discharge of mucus difficult. As a result, mucus secreted by the
cells lining the appendix cannot be expelled and instead is
deposited into the abdominal cavity. As the amount of mucus
accumulates, the pressure in the appendiceal cavity increases, thus
leading to the atrophy of the mucosa and the disorder of secretory
function, eventually resulting in the formation of stable cysts.
Appendiceal mucocele does not have any known markers and is thus
often misdiagnosed as acute appendicitis, or can even be missed
completely. Patients often come to The First Hospital of Nanping
with pain and discomfort in the right lower abdomen and a mass in
the right lower abdomen, which is eventually confirmed by CT
examination or intraoperative and postoperative pathology as
appendiceal mucoceles (1-3).
In the patients diagnosed with acute appendicitis, appendiceal
mucoceles accounts for about 0.2-0.3% of cases They are most common
in patients >50 years old and can lead to ileus peritoneal
effusion or peritonitis (4). Due to
the continual improvement and frequent use of imaging methods,
especially the application of plain and enhanced CT, the
preoperative diagnosis rate of patients has been significantly
improved, but there remains differing opinions on its prognosis and
treatment methods (5,6). A few experts suggest appendiceal
mucous cysts are a benign disease with a tendency towards forming
malignant lesions, whereas others suggest that appendiceal mucous
cysts may also divide into benign and malignant lesions (7,8).
Certain patients may develop edema and inflammation, and possibly a
perforated appendix. Once the mucus leaks into the abdominal
cavity, it can lead to extensive implantation and eventually to the
development of secondary peritoneal pseudomyxoma, which drastically
reduces the survival rate of patients (9). In the present study, the clinical data
of 9 patients with appendiceal mucoceles were retrospectively
analyzed in order to improve our understanding of the disease.
Materials and methods
Patient data
There were 9 patients included in the analysis in
the present study including 3 males and 6 females, aged 39-86 years
old, with a median age 55 years old. The clinical manifestations
were: 4 patients were hospitalized with right lower abdominal pain
as the primary complaint, which was confirmed by color ultrasound
or CT examination; 3 cases complained of abdominal discomfort,
especially in the right lower abdomen, without obvious pain; 4 of
the 9 exhibited muscle guarding (44.4%) and 3 exhibited rebounding
pain (33.3%). Additionally, 1 patient exhibited hematochezia; and 2
patients were hospitalized due to a mass occupying the ileocecal
area that was serendipitously found in routine physical
examinations. This retrospective clinical study was approved by The
Nanping First Hospital's Ethics Committee (approval no.
NPSY2021120016) and written informed consent was obtained from all
patients. The clinicopathological information of the patients
obtained from their medical records are summarized in Table I.
 | Table IClinicopathological characteristics of
the patients. |
Table I
Clinicopathological characteristics of
the patients.
| Parameter | Value |
|---|
| Age, years | 59.8±13.6 |
| White blood cell
count, x109/l | 6.54±1.81 |
| Dimension, cm | 2.89±1.11 |
| Sex, n (%) | |
|
Male | 3 (33.3%) |
|
Female | 6 (66.7%) |
| Abdominal pain, n
(%) | |
|
Yes | 7 (77.8%) |
|
No | 2 (22.2%) |
| Muscle guarding, n
(%) | |
|
Yes | 4 (44.4%) |
|
No | 6 (55.6%) |
| Rebounding pain, n
(%) | |
|
Yes | 3 (33.3%) |
|
No | 6 (66.7%) |
| Pathological result,
n (%) | |
|
Low grade
mucinous neoplasm | 2 (22.2%) |
|
Appendiceal
mucocele | 7 (77.8%) |
Surgical methods
All patients analyzed received surgical treatment,
including laparoscopic appendectomy in 2 cases, exploratory
laparotomy + partial cecectomy + appendectomy in 3 cases,
laparoscopic partial cecectomy + appendectomy in 2 cases, and
laparoscopic right hemicolectomy in 2 cases (Table II).
 | Table IISurgical methods used to manage the
patients. |
Table II
Surgical methods used to manage the
patients.
| Surgical method | n (%) |
|---|
| Laparoscopic
appendectomy | 2 (22.2) |
| Exploratory
laparotomy + appendectomy + partial cecectomy | 3 (33.3) |
| Laparoscopic
appendectomy + partial cecectomy | 2 (22.2) |
| Right hemicolectomy
cecectomy | 2 (22.2) |
Pathological results and postoperative
follow-up
Among the reviewed appendiceal mucocele cases, the
diameter of the appendix was 1.2-5 cm, with an mean diameter of
2.89 cm. Among these, 2 cases were pathologically indicated as
low-grade appendiceal mucinous tumors, and 7 cases were appendiceal
mucinous cysts. The patients were followed up for between 3 months
to 5 years after operation.
Results
Entire cohort
Among the 3,071 patients with appendicitis, 9 cases
were appendiceal mucocele, with an incidence of 0.293%. Clinical
manifestations included discomfort in the right lower abdomen in 7
out of 9 cases, whereas the other 2 cases were accidentally
discovered. Additionally, 4 patients were misdiagnosed as
appendicitis prior to operation, and the misdiagnosis rate was as
high as 44.4%. In the preoperative imaging examination, 3 patients
were diagnosed with appendiceal mucocele, the accuracy rate of
imaging diagnosis was 33.3%.
Of note, two of these cases were misdiagnosed as
ascending colon tumors. All 9 patients underwent surgical
treatment, including laparoscopic surgery in 6 cases (2
laparoscopic appendectomy, 2 laparoscopic partial cecectomy plus
appendectomy, and 2 laparoscopic right hemicolectomy) and
laparotomy in 3 cases (partial cecectomy plus appendectomy).
Pathological examination was performed on the surgically resected
specimens of all patients. The results showed that 7 cases were
appendiceal mucoceles, and 2 cases were low-grade appendiceal
mucoceles. During the follow-up from 3 months to 5 years after
surgery, one patient with exploratory laparotomy plus partial
cecectomy and appendectomy was pathologically diagnosed with
low-grade appendiceal myxoma. The patient developed peritoneal
implants appeared 2 years later, and the remaining patients are
still alive, without any postoperative complications or obvious
signs of recurrence.
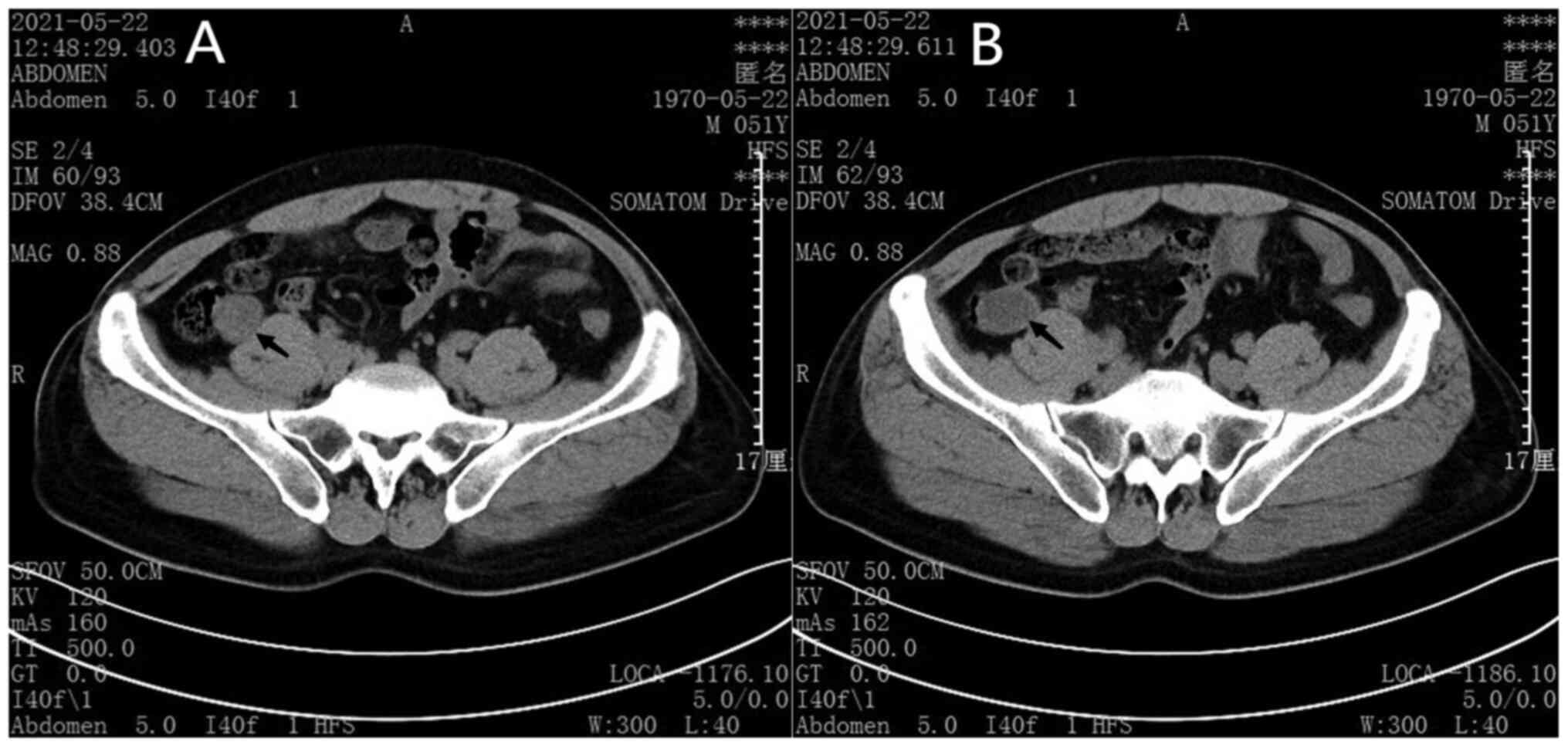
Typical case A patient who underwent
laparoscopic partial cecectomy + appendectomy
The patient came to the hospital complaining of
right lower abdominal pain for half a day. After admission,
abdominal CT examination was completed as shown in Fig. 1 (Appendix mucoceles is highlighted
by arrow).
CT findings of this case
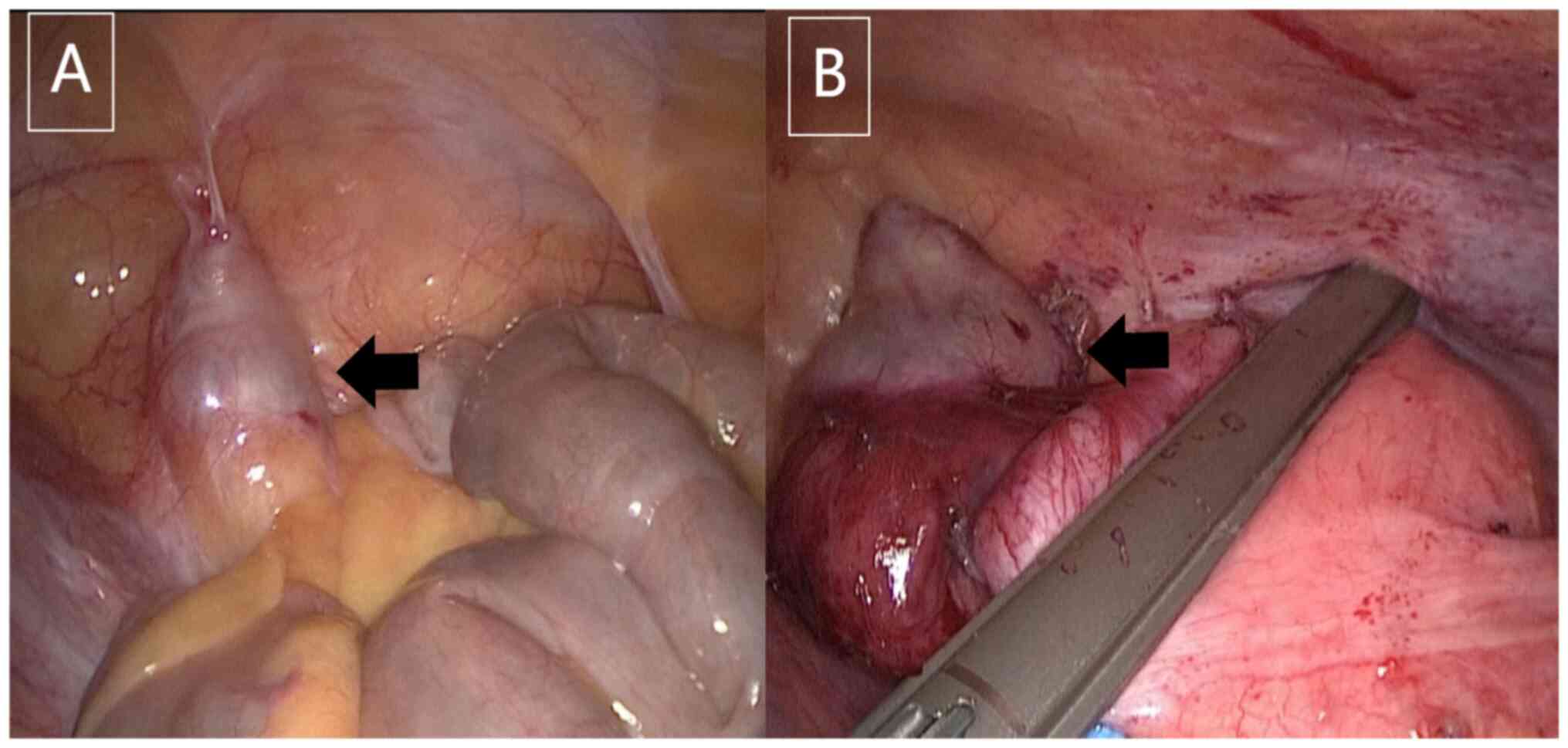
After the anesthesia had taken effect, the patient
was placed in the supine position, and the tissue was disinfected.
Then a curved incision ~10 mm in length was taken from the
umbilicus. After successful puncture, a 14 mmHg pneumoperitoneum
was established. One incision of 5 mm and one incision of 12 mm
were made on the McBurney (the point of outer third between the
navel and the right anterior superior iliac spine) and inverse
McBurney (the point of outer third between the navel and the left
anterior superior iliac spine) incisions (10), respectively. The corresponding
Trocar was inserted, and the greater omentum was explored to cover
the ileocecal region. When the greater omentum was opened, obvious
swelling was seen in the appendix, with a maximum diameter of 3 cm
and a length of 7 cm; obvious adhesion to the surrounding tissues,
notable mesangial edema, and no perforation or gangrene at the root
was observed. Additionally, ~10 ml of a milky exudation was found
in the abdominal cavity, which was considered to be an appendiceal
mucocele. The appendix was lifted using grasping forceps and the
hook was used to dissociate the appendix. The mesoappendix was
dissected, then the appendiceal artery was disassociated. The
appendiceal artery was clipped using a Hem-o-lock polymeric clips
and severed with a hook. On the cecum, 2 cm away from the root of
the appendix, the appendix and part of cecum were removed using
ENDOPATH Endoscopic Linear Cutters. The stump was reinforced with
4-0 absorbable thread, and the greater omentum was sutured onto the
stump. No active bleeding was observed on examination. The appendix
was taken out, and an abdominal drainage tube was placed which led
out from the right lower abdominal incision. After counting the
instruments and gauze, the abdomen was closed layer by layer, and
the specimens were sent for examination. The surgical procedure is
shown in Fig. 2.
The pathological results were acute onset of chronic
appendicitis with the formation of retention mucocele.
Discussion
Appendiceal mucocele is a type I tumor of epithelial
origin. Currently, appendiceal mucoceles are classified into four
pathological types: Simple retention cyst and mucocele with mucosal
hyperplasia (5-25% of cases), mucocythadenoma (63-84% of cases) and
mucocythadenocarcinoma (11-20% of cases) (1). However, the clinical understanding of
the pathological types of appendiceal mucoceles, especially the
differentiation from pseudomyxosis peritoneum, remains unclear. In
order to simplify the diagnosis of appendiceal mucocele,
gastrointestinal neoplasms were divided into two separate grade,
low grade and high grade, in the fourth edition of WHO
Classification, and some morphological features were clarified,
such as structure, cytology, presence of signet-ring cells and
mitotic images (11). The
International Peritoneal Surface Oncology Group extends the current
WHO diagnostic terminology on WHO Classification. Finally, the
classification of appendiceal mucoceles by the American Cancer
Federation 8th edition uses a three-grade classification method:
Low-grade tumor (G1), and high-grade tumors (G2 and G3) (12). In the present study, there were 2
cases of low grade appendiceal mucinous tumors, and 7 cases of
appendiceal mucinous cysts.
The clinical manifestations of appendiceal mucoceles
are atypical and lack specificity. Right lower abdominal pain or a
right lower abdominal mass is the primary manifestation, and 25-50%
of patients have no clinical symptoms and are found accidentally
during physical examination or other operations. One patient in the
present study presented with hematochezia, which was caused by the
compression of intestinal mucosa by the appendiceal mucocele.
Patients with appendiceal mucocele have a high rate
of preoperative misdiagnoses, and often postoperative pathological
diagnoses are required. In this group, four patients (44.4%) were
diagnosed with appendiceal cystic changes by preoperative CT,
confirming that CT-assisted examination of appendiceal mucoceles is
preferred, especially enhanced CT of the lower abdomen, such that
most appendiceal mucoceles can be diagnosed.
Once a diagnosis of an appendiceal mucocele is
confirmed, surgical treatment is necessary. The surgical methods
for its treatment can be appendectomy, appendectomy + partial
cecectomy ileocecectomy and right hemicolectomy. In this group,
laparoscopic appendectomy + partial cecectomy provided good
postoperative prognoses, and this highlights its preference as the
surgical method. When conditions permit, intraoperative rapid
cryotherapy can quickly identify the occurrence of malignant
tumors. If a malignant cancer is diagnosed, laparoscopic right
hemicolectomy is possible. The diameters of mucosal hyperplasia,
appendiceal mucinous cystadenoma and appendiceal mucinous
cystadenocarcinoma are typically >2 cm, and the specific
diameter can provide certain clues for surgeons during surgery
(13). However, there is no
correlation between the size of the appendix and how malignant the
appendiceal mucocele is (14). Even
though mucoceles of the appendix are benign, they have a malignant
tendency and can lead to implantation if the ruptured contents flow
into the abdominal cavity. A variety of factors can lead to mucosal
proliferation of cysts, including spontaneous perforation and
iatrogenic injury. It is hypothesized that iatrogenic factors lead
to one tenth of appendiceal mucoceles developing into pseudomyxoma
of the peritoneum (15).
In conclusion, on the cecum, 1.5-2 cm away from the
appendix root, patients with complete mucocele resection combined
with direct appendectomy and partial cecectomy had a better
prognosis than those with simple appendectomy and less peritoneal
implantation metastasis. Meanwhile, compared with ileocecal bowel
resection, the injury was less severe, and there were fewer
complications; direct appendectomy + partial cecal resection has a
smaller surgical scope and should be the first choice for
treatment, but it is necessary to protect against ileocecal valve
structure damage and cecum and ileum stenosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JG conceived the study, curated the data and wrote
the original draft of the manuscript. ZC contributed to the
acquisition of the data. JC performed the analysis. YZ revised the
work critically for important intellectual content. XH contributed
to the development and design of the methodology and the creation
of models. KH supervised the study, provided the resources and
wrote and reviewed the manuscript. JG and KH confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
This retrospective clinical study was approved by
The Nanping First Hospital's Ethics Committee (approval no.
NPSY2021120016) and written informed consent was obtained from all
patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Abuoglu H, Yıldız MK, Kaya B and Odabaşı
M: Clinicopathological analysis of patients operated for
appendiceal mucocele. Ulus Travma Acil Cerrahi Derg. 23:230–234.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
García Lozano A, Vázquez Tarrago A, Castro
García C, Richart Aznar J, Gómez Abril S and Martínez Abad M:
Mucocele of the appendix: Presentation of 31 cases. Cir Esp.
87:108–112. 2010.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
3
|
Carr NJ, McCarthy WF and Sobin LH:
Epithelial noncarcinoid tumors and tumor-like lesions of the
appendix: A clinicopathologic study of 184 patients with a
multivariate analysis of prognostic factors. Cancer. 75:757–768.
1995.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Marudanayagam R, Williams GT and Rees BI:
Review of the pathological results of 2660 appendecectomy
specimens. J Gastroenterol. 41:745–749. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Dixit A, Robertson JH, Mudan SS and Akle
C: Appendiceal mucocoeles and pseudomyxoma peritonei. World J
Gastroenterol. 13:2381–2384. 2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Rymer B, Forsythe RO and Husada G:
Mucocoele and mucinous tumours of the appendix: A review of the
literature. Int J Surg. 18:132–135. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ali SM, Al-Tarakji M, Shahid F, Qabani AS,
Shah AA, Ahmed K, Khan MB and Inamullah : From diagnosis to
management; mucocele of stump appendicitis, extremely rare finding
in an uncommon surgical disease: Literature review. Int J Surg
Oncol. 2021(8816643)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Scotté M, Laquerrière A, Riff Y, Majerus
B, Manouvrier JL, Leblanc I, Michot F, Hémet J and Ténière P:
Appendiceal mucoceles. Pathophysiology and therapeutic indications.
J Chir (Paris). 131:303–312. 1994.PubMed/NCBI(In French).
|
|
9
|
Rabie ME, Al Shraim M, Al Skaini MS,
Alqahtani S, El Hakeem I, Al Qahtani AS, Malatani T and Hummadi A:
Mucus containing cystic lesions ‘mucocele’ of the appendix: The
unresolved issues. Int J Surg Oncol. 2015(139461)2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pattanshetti VM and Krishna KL:
Conventional laparoscopic appendectomy versus double-incision,
three-port laparoscopic appendectomy: A 1-year randomized
controlled trial. Asian J Endosc Surg. 11:366–372. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Carr NS: Tumors of the appendix. In: World
Health Organization Classification of Tumours. Vol 3. Bosman FT,
Carneiro F, Hruban RH and Theise ND (eds). IARC Press, Lyon,
pp122-125, 2010.
|
|
12
|
Valasek MA and Pai RK: An update on the
diagnosis, grading, and staging of appendiceal mucinous neoplasma.
Adv Anat Pathol. 25:38–60. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pickhardt PJ, Levy AD, Rohrmann CA Jr and
Kende AI: Primary neoplasms of the appendix: Radiologic spectrum of
disease with pathologic correlation. Radiographics. 23:645–662.
2003.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Leonards LM, Pahwa A, Patel MK, Petersen
J, Nguyen MJ and Jude CM: Neoplasms of the Appendix: Pictorial
review with clinical and pathologic correlation. Radiographics.
37:1059–1083. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Virgilio E, Tallerini A, Addario Chieco P,
Castagnola G and Cavallini M: Appendiceal mucocele: The importance
of getting a preoperative diagnosis. ANZ J Surg. 87:E312–E313.
2017.PubMed/NCBI View Article : Google Scholar
|