Introduction
Chagas disease is due to infection with the
protozoan Trypanosoma cruzi. It is estimated that 6 to 7
million people are infected by the protozoan worldwide, with a
predominance in Latin America, mainly in Argentina, Brazil and
Mexico (1-3).
Chronic chagasic cardiomyopathy is the most common
clinical complication in patients with Chagas disease; it is
characterized by severe myocarditis, infiltration of the
lymphomononuclear cells, interstitial fibrosis and cardiomyocyte
hypertrophy, which may lead to dilated cardiomyopathy, end-stage
heart failure (HF) and death (4).
Congestive heart failure, a characteristic of
chagasic patients, is also associated with significant impairment
of cardiac function and decreased inspiratory muscle strength
(5,6), in addition to a restriction in
pulmonary expandability, airway obstruction, increased dead space
and respiratory rate, gas diffusion abnormalities and expiratory
muscle weakness (7,8).
The interstitial congestion present in HF prevents
alveolar distension, which contributes to the inefficiency of
respiratory muscle function, a reduction in oxygen supply and
pulmonary complacency. This set of changes results in a restrictive
respiratory pattern that contributes to respiratory muscle overload
and an uncontrolled breathing regulation mechanism (8).
Among the symptoms presented by affected patients,
the sensation of exertion fatigue and dyspnea are notable, both of
which restrict the activities of daily living (ADLs). The intensity
of the dyspnea is disproportionate to the physical activity
performed, which directly affects the quality of life and prognosis
of the affected patient, thus having an important impact on the
functional capacity of the individual (3,9).
In view of the aforementioned respiratory
complications, the measurement of respiratory flows and volumes
through spirometry becomes an important additional tool for a
comprehensive evaluation of chagasic patients. The decrease in
these parameters has an impact on the physical restriction, in
addition to being associated with clinical outcomes of the chagasic
patient, such as the risk of cardiovascular events in a short
period and the risk of death (10).
As the characteristics of the disease can lead to
dysfunction and restriction of lung volumes, spirometric values
become essential to assess the dysfunction present in patients with
Chagas disease. Functional complications are already known to be
associated with spirometric values in patients with Chagas disease.
In the present study, the associations between pulmonary functional
capacity values are expanded, and to the best of our knowledge,
this is the first study to evaluate and compare the pulmonary flows
and volumes of patients with Chagas disease according to their
clinical characteristics, verifying the differences between the
different risk groups of death and stroke, as well as different
clinical forms of the disease.
Materials and methods
Study population
This study was a descriptive, cross-sectional study
that included 72 individuals with Chagas disease, confirmed by a
positive result in enzyme-linked immunoassays, indirect
immunofluorescence assays and indirect hemagglutination assays.
These individuals were treated clinically at the Chagas Disease
Ambulatory Service of the Health Sciences College of the University
of Rio Grande do Norte State (FACS-UERN; Mossoró, Brazil).
Inclusion and exclusion criteria
Patients with good cognition and understanding,
those who were >18 years of age and those who agreed to
participate in the survey were included in the study. Those
patients who dropped out of the test protocol when already in
progress, those who, due to physical limitation, were unable to
complete one of the functional tests and those who had previously
used bronchodilators were excluded.
Ethical considerations
The patients were initially informed about the
objectives of the study and the methods to be applied, and were
later questioned about their willingness to participate. After
agreeing to participate, the patients were asked to sign an
informed consent form. The research followed the criteria of the
Declaration of Helsinki (1997) and respected the ethical principles
of Resolution 466/2012 of the National Health Council in Brazil,
which supports research involving human beings. The ethical aspects
of the study were approved by the Research Ethics Committee of the
University of Rio Grande do Norte State (approval nos. 1.510.620
and CAAE 53362316.8.0000.5294).
Data collection
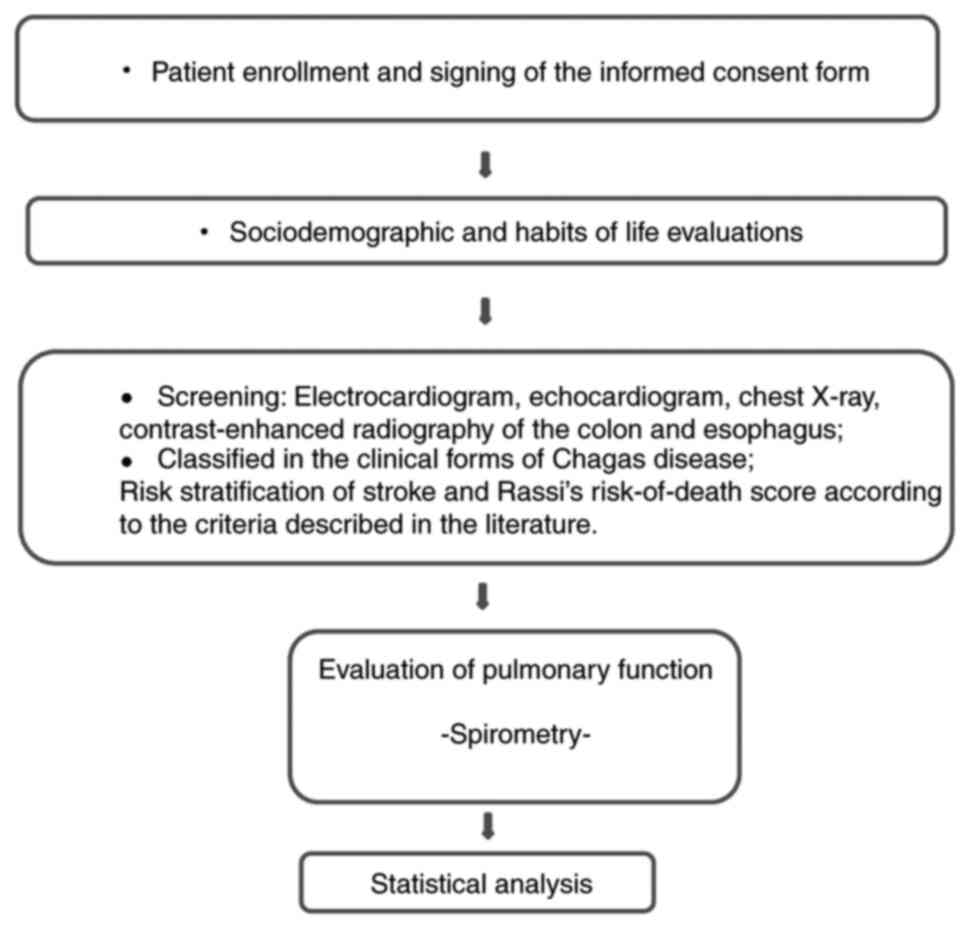
An initial evaluation was performed at the FACS-UERN
Chagas Disease Ambulatory Service, where the medical history and
sociodemographic data of the patients were collected and a life
habits assessment was performed through an evaluation form prepared
for the study. Echocardiography, chest X-ray, contrast-enhanced
radiography of the colon and esophagus, and subsequent
classification of the clinical forms of Chagas disease were
performed. Risk stratification of stroke and Rassi's risk-of-death
were also analyzed, according to the criteria described in the
literature (9,11). Finally, spirometry was performed.
The sequence of actions performed from enrollment to statistical
analysis is described in Fig.
1.
The pulmonary function evaluation was performed by
spirometry, using a USB digital spirometer from the
CareFusion® brand (Becton, Dickinson and Company), to
characterize the degree of obstructive pulmonary disorder as an
evaluation parameter.
The entire procedure was performed as described by
Pereira et al (12,13) and Miller et al (14). For spirometry, the volunteer was
sitting, with the head kept in a neutral position and hips flexed
at 90˚, with a minimum of 5-10 min of rest before the exam. Three
to eight maneuvers were performed, so that in the end, three blows
were obtained that passed the criteria, with at least 6 sec of
exhalation, and the last blow could not be the best. The patients
received visual and auditory feedback, and all the disposable
nozzles were changed and used individually for each patient.
The values that were obtained from the patients were
compared to predicted values adequate for the population evaluated,
and the percentages were adjusted for sex, height, weight and age
(14). Obstructive or restrictive
diseases were identified, evaluating the following variables:
Forced expiratory volume in 1 sec (FEV1), forced vital
capacity (FVC), peak expiratory flow rate (PEFR) and
FEV1/FVC (Tiffeneau index) (12).
Statistical analysis
All data were tabulated and organized into
worksheets using Microsoft Excel (version 16.0.9226.2156; Microsoft
Corporation) and IBM SPSS Statistics (version 20; IBM Corp.)
software. The normality of the data obtained was verified using the
Kolmogorov-Smirnoff and Shapiro-Wilk tests.
The comparison of the test values obtained between
the groups of patients stratified according to their clinical form
and risk of death and stroke was performed using the t-test for
independent samples when there was a normal distribution, and the
Mann-Whitney when there was a non-normal distribution. P<0.05
was considered to indicate a statistically significant
difference.
Results
The percentages recorded are values obtained
relative to predicted values for the population evaluated, adjusted
for sex, height, weight and age (14). It was not specifically observed
whether there were respiratory disorders, i.e. values below the
limits of normality, but rather if the worsening of the respiratory
flow and volume values accompanied the risks of clinical
aggravation and complications in the chagasic patients.
Blood was initially collected from 82 patients who
went to the FACS-UERN Chagas Disease Ambulatory Service to undergo
laboratory and clinical examinations and periodic medical
consultations. After applying the inclusion and exclusion criteria,
10 subjects were eliminated from the study and 72 patients (33
women and 39 men) remained; however, not all patients had a full
set of clinical characteristics available, so when divided into the
groups, there were 42 patients in the death risk group, 62 in the
stroke risk group and 67 patients classified into different
clinical forms. All patients were from the West Potiguar mesoregion
of Rio Grande do Norte in Brazil, mainly from the city of Mossoró
(25 patients). The majority (55.6%) of the patients lived in the
urban area of these municipalities. The patient ages ranged from 26
to 69 years, with a mean [± standard deviation (SD)] of 48.3±10.9
years. The mean (± SD) weight was 70.1±13.7 kg, the mean (± SD)
height was 1.60±0.09 m and the mean (± SD) BMI was 27.0±4.4.
It was observed that 4.2% of patients were reported
with diabetes, 33.3% with hypertension, 5.6% with dyslipidemia and
34.3% with musculoskeletal disorders. It was also observed that
56.9% of the cohort used some form of medication, mainly
antihypertensive drugs (30.6% of the total patients). With regard
to lifestyle, only 18 (25%) patients performed regular physical
activities and 21 (29.2%) were smokers or former smokers (data not
shown).
The distribution of patients according to Rassi's
risk-of-death score (11) revealed
that 24 patients (33.3%) were at a low risk of death, 11 (15.3%)
were at intermediate risk and 7 (9.7%) were at high risk. A total
of 11 patients (15.3%) had not yet been classified and 19 (25.4%)
did not meet the criteria for determining the risk of death. For
comparison purposes, the patients were divided into two groups
according to the scores, namely the group with a low risk of death
and the group with an intermediate/high risk of death, as shown in
Table I.
 | Table IComparison of the spirometric values
in patients with a low and intermediate/high risk of death. |
Table I
Comparison of the spirometric values
in patients with a low and intermediate/high risk of death.
| | Rassi's risk of death
score | |
|---|
| Parameter | Low risk-group
(n=24) |
Intermediate/high-group (n=18) | P-value |
|---|
| Spirometry | | | |
|
FVC | 3.04±0.84 | 3.47±1.05 | 0.148a |
|
FVC
percentage | 85.70±12.48 | 87.33±12.48 | 0.733a |
|
FEV1 | 2.63±0.69 | 2.84±0.89 | 0.390a |
|
FEV1
percentage | 90.75±11.55 | 87.83±18.65 | 0.536a |
|
Tiffeneau
index | 88.79±7.44 | 82.27±7.41 | 0.008a,b |
Regarding stroke risk scores (9), 49 patients (68.1%) had a low risk of
developing a stroke, 6 (8.3%) had a moderate risk, 7 (9.7%) had a
high risk and 10 (13.9%) had not yet been classified. For
comparison purposes, the patients were divided into two groups,
according to the scores, namely the group with a low risk of stroke
and the group with an intermediate/high risk of stroke, as shown in
Table II.
 | Table IIComparison of the spirometric values
in patients with a low and intermediate/high risk of stroke. |
Table II
Comparison of the spirometric values
in patients with a low and intermediate/high risk of stroke.
| | Stroke risk
score | |
|---|
| Parameter | Low-risk group
((n=50) |
Intermediate/high-risk group (n=12) | P-value |
|---|
| Spirometry | | | |
|
FVC | 3.38±0.95 | 3.19±0.82 | 0.533a |
|
FVC
percentage | 91.64±13.43 | 81.16±17.56 | 0.026a,b |
|
FEV1 | 2.87±0.78 | 2.65±0.66 | 0.372a |
|
FEV1
percentage | 94.98±12.12 | 82.66±18.78 | 0.007a,b |
|
Tiffeneau
index | 86.26±7.77 | 83.66±9.10 | 0.320a |
In the clinical forms classification, 30 patients
(41.7%) had an undetermined clinical form, while 18 (25.0%) had a
cardiac form, 8 (11.1%) had a digestive form and 11 (15.3%) had a
cardiodigestive form. In addition, 5 (6.9%) still needed to undergo
complementary tests to determine their clinical form. For
comparison purposes, the patients were divided into two groups,
namely the cardiac group, with cardiac or cardiodigestive clinical
forms, and the non-cardiac group, with undetermined and digestive
clinical forms, as shown in Table
III.
 | Table IIIComparison of the spirometric values
in patients with the cardiac form and the non-cardiac form. |
Table III
Comparison of the spirometric values
in patients with the cardiac form and the non-cardiac form.
| | Clinical forms | |
|---|
| Parameter | Cardiac group
(n=29) | Non-cardiac group
(n=38) | P-value |
|---|
| Spirometry | | | |
|
FVC | 3.25±0.87 | 3.47±0.98 | 0.594a |
|
FVC
percentage | 82.89±13.83 | 94.16±14.79 | 0.005a,b |
|
FEV1 | 2.75±0.73 | 2.92±0.80 | 0.380a |
|
FEV1
percentage | 86.26±15.76 | 96.27±13.01 | 0.001a,b |
|
Tiffeneau
index | 86.0(27) | 87.0(41) | 0.217c |
The comparison of the respiratory and functional
parameters of the patients, taking into account the risk of death
scores, showed that the group with low risk (scores 0 to 2) had
significantly higher values for the Tiffeneau index (Table I). The evaluation of
cardiorespiratory capacity according to the risk of stroke, on the
other hand, showed that patients with low risk had significantly
higher percentage values for FVC and FEV1 (Table II).
When comparing the respiratory and functional
parameters among the patients with the undetermined or digestive
clinical form (non-cardiac group) and those with the cardiac or
cardiodigestive forms (cardiac group), the percentage values of FVC
and FEV1 were significantly higher in the non-cardiac
group (Table III).
Discussion
In the present study, the Tiffeneau index was
significantly different between the groups with a high and a low
risk of death in the chagasic patients. The index represents the
association between FEV1 and FVC (FEV1/FVC),
and has normal values between 0.70 and 0.80(15), or 0.70, so that lower values suggest
a limitation of air flow. The present results suggest that patients
at a high risk of death presented with more obstructive
characteristics than those at a low risk. Although there have been
no previous studies with chagasic patients, this association has
been reported in patients with heart failure, among whom those with
restrictive or obstructive ventilation had a higher mortality rate
and the lower limit of the Tiffeneau Index was an independent
variable for this outcome (16).
Physical activities and ADLs increase ventilatory
demand, and airway obstruction in these efforts generates dynamic
pulmonary hyperinflation. This imprisonment generates increasing
difficulty for the aforementioned activities by the impairment of
function and pulmonary mobility. Thus, a patient with poor
pulmonary function tends to decrease the amount of activity
undertaken, compromising their independence and functionality, and
this set of factors is known to be associated with higher mortality
(17,18).
In the present study, when the groups were divided
according to the stroke risk score (9), the patients who had a lower risk had
significantly higher mean percentage values for FVC and
FEV1. Despite the existence of other factors, such as
hypercoagulability, in the majority of cases, stroke in the
chagasic patient is associated with cardioembolism (9). In a cardioembolism, emboli are formed
in the cardiac cavities that leave the heart through the left
ventricle through the aortic artery and reach the cerebral
irrigation arteries, obstructing the blood flow and causing
consequent ischemia and neuronal tissue hypoxia (19). The cause of the formation of these
emboli is mainly dysfunction of cardiac contractility, function and
rhythm, in which inefficient pumping leads to stasis and blood
coagulation, with subsequent embolization of the heart to the brain
(20). Thus, it has been observed
that the simple presence of systolic dysfunction in chagasic heart
disease, regardless of the degree of myocardial involvement, is
associated with the high incidence of ischemic stroke (9).
Georgiopoulou et al (21) found a correlation between the FVC
and FEV1 percentages and the risk of developing HF in
the elderly, concluding that abnormal findings in the spirometry
were associated with an increased risk of this dysfunction. Barr
et al (22) found that the
percentage values for emphysema and the FEV1/FVC ratio
were associated with left ventricular filling, which reinforces the
correlation between lung volumes and flows and cardiac function.
Considering that the stroke has a direct causal relationship with
HF in the chagasic patient, reduced percentages of FVC and
FEV1 have a positive association with the risk of
developing this clinical complication, as shown in the present
study. This relationship can be explained by the high oxidative
stress characteristic of impaired gas exchange in abnormal
pulmonary function, which directly affects myocardial function
(23), and by changes in
respiratory mechanics and intrathoracic pressure, which may reduce
cardiac output by interference with the preload, as there is a
mechanical relationship between the respiratory and cardiovascular
systems, since the two are closely accommodated in the thoracic
region (24).
A significant difference was also observed in the
mean percentages of FVC and FEV1 among cardiac and
non-cardiac patients. The same results cited previously in the
studies by Georgiopoulou et al (21) and Barr et al (22) explain this difference, since these
studies correlated the abnormal values in spirometry with cardiac
dysfunction.
A previous review has shown significant differences
in functional capacity (maximum oxygen consumption values) among
cardiac and non-cardiac chagasic patients (24), but no studies have shown specific
differences in pulmonary function in these patients. By contrast,
Baião et al (25) found that
cardiac chagasic patients have lower FVC values than cardiopaths of
other etiologies. However, other studies have found no significant
differences in pulmonary flow and volumes when cardiac chagasic
patients were compared with healthy individuals, as well as in the
comparison of those indeterminate patients, who are asymptomatic,
and their pairs with pulmonary hypertension (26,27).
In addition to the chronic oxidative stress caused
by the pulmonary volume deficit previously mentioned (23), restrictive physiological findings
have been reported in patients with heart disease and are mainly
attributed to subclinical interstitial and alveolar pulmonary
edema, in addition to cardiomegaly, increased central blood volume
and fibrotic stiffening of the lung parenchyma. All this leads to a
reduction in pulmonary complacency and an increased difficulty to
breathe in these patients, which explains the significant
difference found in the present study (28,29).
However, despite the differences between the groups, the mean
values of the cardiac patients were within the limits of normality,
>80% of that expected, so preventative maintenance of values
using physical exercises is recommended to avoid a decline in these
values. In addition to the interference of cardiac dysfunction in
the functioning of the respiratory system, there is also the
hypothesis of an inverse interaction in which the inefficient
respiratory system can interfere chronically in the cardiovascular
system. These dysfunctions may be added continuously and cause
deterioration of physical and functional cardiopulmonary system
capacity (30,31). The dysfunction of one of these
systems requires early follow-up so that the injury does not
develop in the other.
The decrease in pulmonary volumes and capacities
accompanied a higher risk of death and stroke related to the
cardiac form of Chagas disease in the present study, which confirms
previous discussions in the literature that associate the higher
risk of clinical worsening with worse respiratory function
(32).
Spirometry proved to be a good analytical tool in
the present study and showed a good association with clinical forms
and risk of death and stroke scores in patients with Chagas
disease. Therefore, it is suggested that the spirometric parameters
of Tiffeneau index, FVC value and FEV1 value may give
indications that the patient is suffering from a clinical worsening
of their condition.
To the best of our knowledge, this is the first
study to find significant differences in the stratifications cited
in chagasic patients, as some of these associations were only
studied in other categories of patients.
Chagas disease is a pathology that can have a
heterogeneous course. The condition is widely studied and the
different clinical forms and prognostic instruments for the risk of
stroke and death are already known. Thus, data that correlate with
these disease progression variables are important to guide
therapeutic approaches and predict injuries. The present study
concluded that spirometry is a relatively simple yet important
clinical tool that correlates with the risk of death and stroke,
and the development of the most severe form of the disease. In view
of the data, these patients should also be challenged to avoid a
sedentary lifestyle and be physically active, as these are
attitudes that directly influence lung function assessed by
spirometry.
Acknowledgements
The authors offer their deepest thanks to the
professionals at the Chagas Disease Ambulatory Service of the
Health Sciences College of the University of Rio Grande do Norte
State (Mossoró, Brazil) and Artmedica Clinic (Mossoró, Brazil) who
provided technical support for the development of this study.
Funding
Funding: This research was funded in part by Coordenação de
Aperfeiçoamento de Pessoal de Nível Superior-Brazil (grant no.
001).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NMM and TAAMF were responsible for the conception
and design of the study. NMM, VDA and LCCML collected the data, and
NMM, MFA, CMA, CMB, EGCN, JVF and TAAMF performed the data analysis
and interpretation. MFA and VDA contributed to the statistical
analysis. NMM was primarily responsible for writing the manuscript,
with contributions from LCCML, TAAMF, CMA, CMB, EGCN and JVF. CMA,
CMB, EGCN and JVF also made a critical review and approved the
final version for publication. NMM and TAAMF confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The research followed the criteria of the
Declaration of Helsinki (1997) and respected the ethical principles
of Resolution 466/2012 of the National Health Council from Brazil.
The ethical aspects were approved by the Research Ethics Committee
of the University of Rio Grande do Norte State (grant nos.
1.510.620 and CAAE 53362316.8.0000.5294). Written informed consent
was obtained from all participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
No authors listed. Chagas disease in Latin
America: An epidemiological update based on 2010 estimates. Wkly
Epidemiol Rec. 90:33–44. 2015.PubMed/NCBI(In English, French).
|
|
2
|
Guhl F and Lazdins-Helds JK: OPAS,
Organization Pan American Health. Report on the Chagas disease.
Scientific Organization working group on the Chagas disease.
Technical Meeting, Buenos Aires, Argentina: Special Program
Research and Teaching on tropical diseases. Special Research and
Teaching Program on Tropical Diseases (TDR)/GTC/09, update at 2007:
p. 266.
|
|
3
|
Dias JC, Ramos AN Jr, Gontijo ED, Luquetti
A, Shikanai-Yasuda MA, Coura JR, Torres RM, Melo JR, Almeida EA,
Oliveira W Jr, et al: Brazilian Consensus on Chagas disease, 2015.
Epidemiol Serv Saúde. 25(esp):7–86. 2016.PubMed/NCBI View Article : Google Scholar : (In Portuguese).
|
|
4
|
Marin-Neto JA, Simoes MV and Sarabanda AV:
Chagas heart disease. Arq Bras Cardiol. 72:247–280. 1999.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nishimura Y, Maeda H, Tanaka K, Nakamura
H, Hashimoto Y and Yokovama M: Respiratory muscle strenght and
hemodynamics in chronic heart failure. Chest. 105:355–359.
1994.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ribeiro AL, Nunes MP, Teixeira MM and
Rocha MO: Diagnosis and management of Chagas disease and
cardiomyopathy. Nat Rev Cardiol. 9:576–589. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Chua TP, Anker SD, Harrington D and Costa
AJ: Inspiratory muscle strength is a determinant of maximum oxygen
consumption in chronic heart failure. Br Heart J. 74:381–385.
1995.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Daganou M, Dimopoulou I, Alivizatos PA and
Tzelepis GE: Pulmonary function and respiratory muscle strenght in
chronic heart failure: Comparison between ischemic and idiopathic
dilated cardiomyopathy. Heart. 81:618–620. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sousa AS, Xavier SS, Freitas GR and
Hasslocher-Moreno A: Prevention strategies of cardioembolic
ischemic stroke in Chagas' disease. Arq Bras Cardiol. 91:306–310.
2008.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
10
|
Rassi A Jr, Rassi SG and Rassi AG: Sudden
death in Chagas disease. Arq Bras Cardiol. 76:75–96.
2001.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
11
|
Rassi A Jr, Rassi A, Little WC, Xavier SS,
Rassi SG, Rassi AG, Rassi GG, Hasslocher-Moreno A, Sousa AS and
Scanavacca MI: Development and validation of a risk score for
predicting death in Chagas' heart disease. N Engl J Med.
355:799–808. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pereira CA, Duarte AA, Gimenez A and
Soares MR: Comparison between reference values for FVC, FEV1, and
FEV1/FVC ratio in White adults in Brazil and those suggested by the
Global lung function initiative 2012. J Bras Pneumol. 40:397–402.
2014.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
13
|
Pereira CA, Sato T and Rodrigues SC: New
reference values for forced spirometry in white adults in Brazil. J
Bras Pneumol. 33:397–406. 2007.PubMed/NCBI View Article : Google Scholar : (In English,
Portuguese).
|
|
14
|
Miller MR, Hankinson J, Brusasco V, Burgos
F, Casaburi R, Coates A, Crapo R, Enright P, van der Griten CP,
Gustafsson P, et al: Standardisation of spirometry. Eur Respir J.
26:319–338. 2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bateman ED, Hurd SS, Barnes PJ, Bousquet
J, Drazen JM, FitzGerald JM, Gibson P, Ohta K, O'Byrne P, Pedersen
SE, et al: Global strategy for asthma management and prevention:
GINA executive summary. Eur Respir J. 31:143–178. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Plesner LL, Dalsgaard M, Schou M, Køber L,
Vestbo J, Kjøller E and Iversen K: The prognostic significance of
lung function in stable heart failure outpatients. Clin Cardiol.
40:1145–1151. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Vogelmeier CF, Criner GJ, Martinez FJ,
Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M,
Fabbri LM, et al: Global strategy for the diagnosis, management,
and prevention of chronic obstructive lung disease 2017 report.
GOLD executive summary. Am J Respir Crit Care Med. 195:557–582.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
O'Donnell DE, Revill SM and Webb KA:
Dynamic Hyperinflation and exercise intolerance in Chronic
obstructive pulmonary disease. Am J Respir Crit Care Med.
164:770–777. 2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Arboix A and Alió J: Cardioembolic stroke:
Clinical features, specific cardiac disorders and prognosis. Curr
Cardiol Rev. 6:150–161. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Weir NU: An update on cardioembolic
stroke. Postgrad Med J. 84:133–142. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Georgiopoulou VV, Kalogeropoulos AP, Psaty
BM, Rodondi N, Bauer DC, Butler AB, Koster A, Smith AL, Harris TB,
Newman AB, et al: Lung function and risk for heart failure among
older adults: The health ABC study. Am J Med. 124:334–341.
2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Barr RG, Bluemke DA, Ahmed FS, Carr JJ,
Enright PL, Hoffman EA, Jiang R, Kawut SM, Kronmal RA, Lima JAC, et
al: Percent emphysema, airflow obstruction, and impaired left
ventricular filling. N Engl J Med. 362:217–227. 2010.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dhalla AK, Hill MF and Singal PK: Role of
oxidative stress in transition of hypertrophy to heart failure. J
Am Coll Cardiol. 28:506–514. 1996.PubMed/NCBI View Article : Google Scholar
|
|
24
|
van den Hout RJ, Lamb HJ, van den Aardweg
JG, Schot R, Steendijk P, van der Wall EE, Bax JJ and de Ross A:
Real-time MR imaging of aortic flow: Influence of breathing on left
ventricular stroke volume in chronic obstructive pulmonary disease.
Radiology. 229:513–519. 2003.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Baião EA, Costa Rocha MO, Lima MM, Beloti
FR, Pereira DA, Parreira VF, Ribeiro AL and Britto RR: Respiratory
function and functional capacity in Chagas cardiomyopathy. Int J
Cardiol. 168:5059–5061. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Montes de Oca M, Torres SH, Loyo JG,
Vazquez F, Hernández N, Anchustegui B and Puigbó JJ: Exercise
performance and skeletal muscles in patients with advanced Chagas
disease. Chest. 125:1306–1314. 2004.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Suman AC, Costa EAPND, Bazan SGZ, Hueb JC,
Carvalho FC, Martin LC and Yoo HHB: Evaluating respiratory
musculature, quality of life, anxiety, and depression among
patients with indeterminate chronic Chagas disease and symptoms of
pulmonary hypertension. Rev Soc Bras Med Trop. 50:194–198.
2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hauge A, Bo G and Waaler BA:
Interrelations between pulmonary liquid volumes and lung
compliance. J Appl Physiol. 38:608–614. 1975.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Evans SA, Watson L, Cowley AJ, Johnston ID
and Kinnear WJ: Static lung compliance in chronic heart failure:
Relation with dyspnea and exercise capacity. Thorax. 50:245–248.
1995.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Mortara A, Sleight P, Pinna GD, Mastri R,
Capomolla S, Febo O, La Rovere MT and Cobelli F: Association
between hemodynamic impairment and cheyne-stokes respiration and
periodic breathing in chronic stable congestive heart failure
secondary to ischemic or idiopathic dilated cardiomyopathy. Am J
Cardiol. 84:900–904. 1999.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Schettino CDS, Deus FCC, Gonçalves AAV and
Wallace E: Relationship between COPD and cardiovascular disease.
Pulmao RJ. 22:19–23. 2013.
|
|
32
|
Vargas FS, Cukier A, Tsanaclis A, Pereira
JR, Barrero AC and Romeiro Neto MM: Respiratory mechanics in
patients with Chagas disease without cardiac insufficiency. Rev
Inst Med Trop Sao Paulo. 23:264–273. 1981.PubMed/NCBI
|