|
1
|
Sarode G, Maniyar N, Sarode SC, Jafer M,
Patil S and Awan KH: Epidemiologic aspects of oral cancer. Dis Mon.
66(100988)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Health Promotion Administration: Cancer
registry annual report, 2020 Taiwan. Health Promotion
Administration, Ministry of Health and Welfare, Taiwan, 2022.
|
|
4
|
Cheng FC, Wang LH, Lin HP and Chiang CP:
Morbidity and mortality of oral cancer in Taiwan: Trends from 2000
to 2021. J Dent Sci. 18:1338–1346. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Guha N, Warnakulasuriya S, Vlaanderen J
and Straif K: Betel quid chewing and the risk of oral and
oropharyngeal cancers: A meta-analysis with implications for cancer
control. Int J Cancer. 135:1433–1443. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Herrero R, Castellsagué X, Pawlita M,
Lissowska J, Kee F, Balaram P, Rajkumar T, Sridhar H, Rose B,
Pintos J, et al: Human papillomavirus and oral cancer: The
international agency for research on cancer multicenter study. J
Nat Cancer Inst. 95:1772–1783. 2003.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ribeiro FA, Noguti J, Oshima CT and
Ribeiro DA: Effective targeting of the epidermal growth factor
receptor (EGFR) for treating oral cancer: A promising approach.
Anticancer Res. 34:1547–1552. 2014.PubMed/NCBI
|
|
8
|
Hyodo T, Kuribayashi N, Fukumoto C,
Komiyama Y, Shiraishi R, Kamimura R, Sawatani Y, Yaguchi E,
Hasegawa T, Izumi S, et al: The mutational spectrum in whole exon
of p53 in oral squamous cell carcinoma and its clinical
implications. Sci Rep. 12(21695)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Huang CC, Ou CY, Lee WT, Hsiao JR, Tsai ST
and Wang JD: Life expectancy and expected years of life lost to
oral cancer in Taiwan: A nation-wide analysis of 22,024 cases
followed for 10 years. Oral Oncol. 51:349–354. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ikawa H, Sato H, Takayama K, Takeda D,
Suzuki T, Yuasa H, Adachi M, Uzawa N and Kurita H: Is
chemoradiotherapy more effective than radiotherapy alone in
patients with primary unresectable locally advanced oral cancer
without distant metastases? Systematic review and meta-analysis
based on the GRADE approach. J Oral Maxillofac Surg Med Pathol.
36:259–265. 2024.
|
|
11
|
Naruse T, Yanamoto S, Matsushita Y,
Sakamoto Y, Morishita K, Ohba S, Shiraishi T, Yamada SI, Asahina I
and Umeda M: Cetuximab for the treatment of locally advanced and
recurrent/metastatic oral cancer: An investigation of distant
metastasis. Mol Clin Oncol. 5:246–252. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Balachander K and Paramasivam A: Anti-PD-1
agent: A promising immunotherapy drug for oral cancer? Oral Oncol.
132(105997)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Liu C, Wang M, Zhang H, Li C, Zhang T, Liu
H, Zhu S and Chen J: Tumor microenvironment and immunotherapy of
oral cancer. Eur J Med Res. 27(198)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cooper JS, Pajak TF, Forastiere AA, Jacobs
J, Campbell BH, Saxman SB, Kish JA, Kim HE, Cmelak AJ, Rotman M, et
al: Postoperative concurrent radiotherapy and chemotherapy for
high-risk squamous-cell carcinoma of the head and neck. N Engl J
Med. 350:1937–1944. 2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
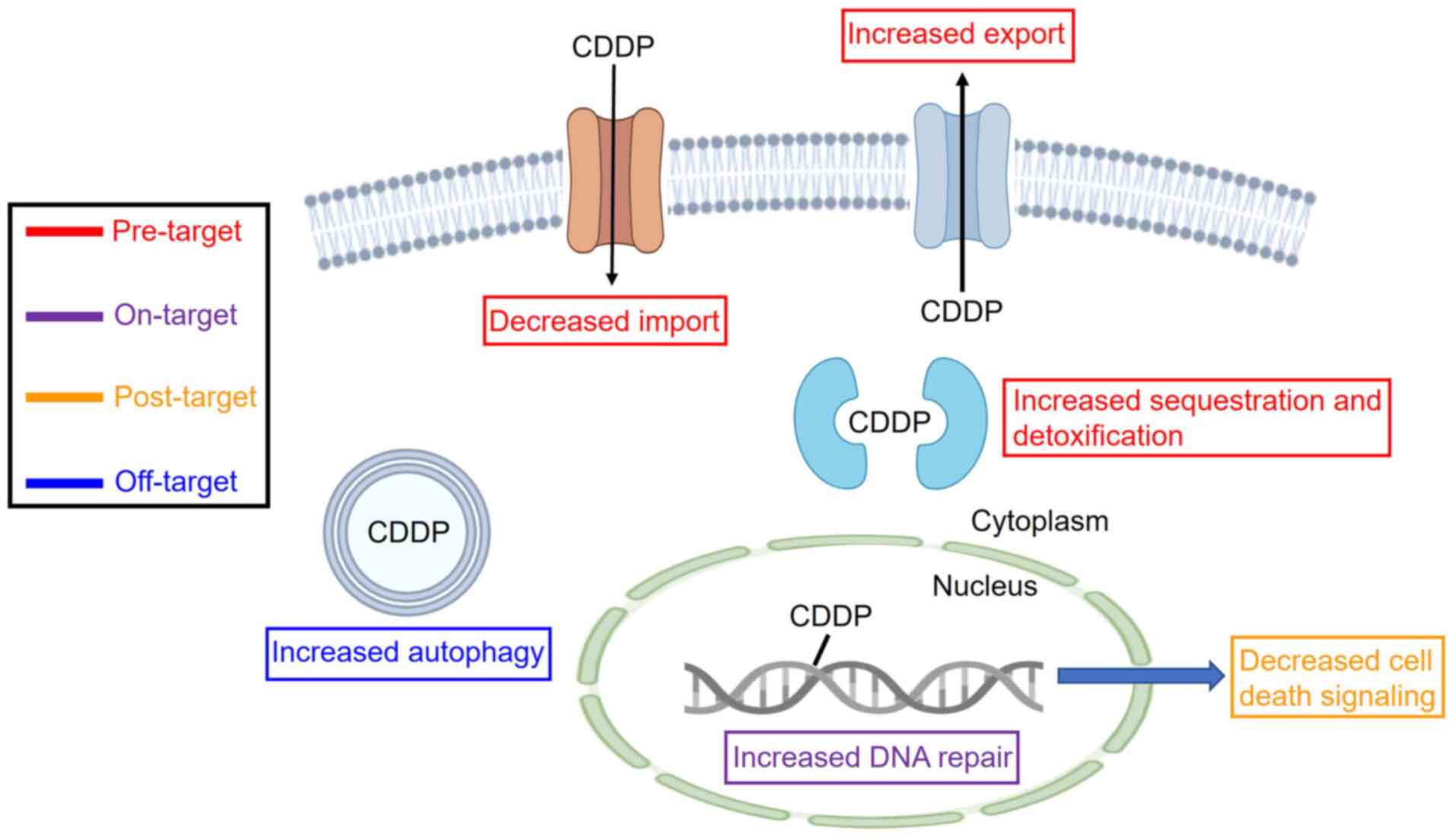
Cheng Y, Li S, Gao L, Zhi K and Ren W: The
molecular basis and therapeutic aspects of cisplatin resistance in
oral squamous cell carcinoma. Front Oncol.
11(761379)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Biswal S, Panda M, Sahoo RK, Tripathi SK
and Biswal BK: Tumour microenvironment and aberrant signaling
pathways in cisplatin resistance and strategies to overcome in oral
cancer. Arch Oral Biol. 151(105697)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
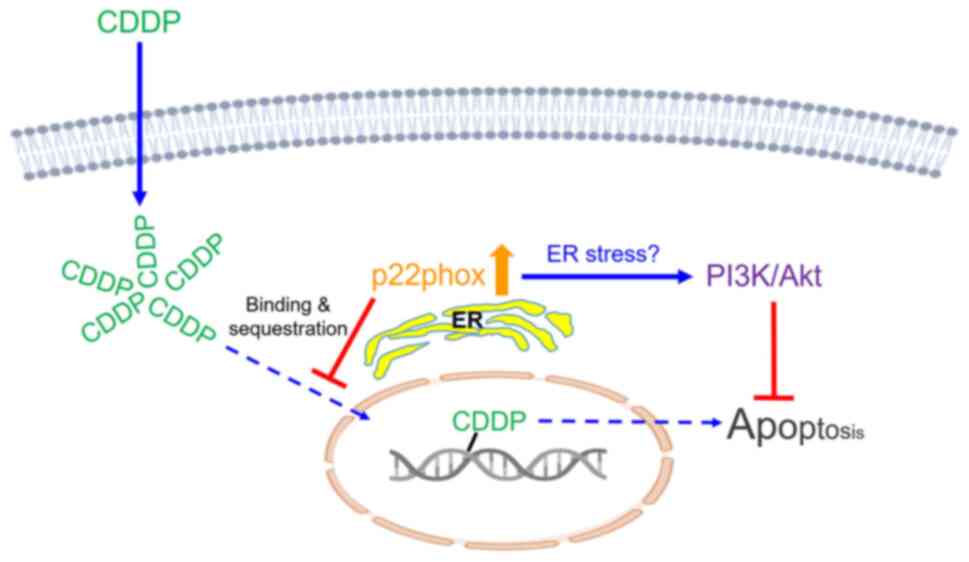
Hung CC, Li FA, Liang SS, Wang LF, Lin IL,
Chiu CC, Lee CH and Chen JY: Direct binding of cisplatin to
p22phox, an endoplasmic reticulum (ER) membrane protein,
contributes to cisplatin resistance in oral squamous cell carcinoma
(OSCC) cells. Molecules. 25(3815)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hung CC, Chien CY, Chiang WF, Lin CS, Hour
TC, Chen HR, Wang LF, Ko JY, Chang CH and Chen JY: p22phox confers
resistance to cisplatin, by blocking its entry into the nucleus.
Oncotarget. 6:4110–4125. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hung CC, Chien CY, Chu PY, Wu YJ, Lin CS,
Huang CJ, Chan LP, Wang YY, Yuan SF, Hour TC, et al: Differential
resistance to platinum-based drugs and 5-Fluorouracil in
p22phox-overexpressing oral squamous cell carcinoma: Implications
of alternative treatment strategies. Head Neck. 39:1621–1630.
2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bedard K and Krause KH: The NOX family of
ROS-generating NADPH oxidases: Physiology and pathophysiology.
Physiol Rev. 87:245–313. 2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Parkos CA, Allen RA, Cochrane CG and
Jesaitiset AJ: Purified cytochrome b from human granulocyte plasma
membrane is comprised of two polypeptides with relative molecular
weights of 91,000 and 22,000. J Clin Invest. 80:732–742.
1987.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kawahara T, Ritsick D, Cheng G and
Lambethet JD: Point mutations in the proline-rich region of p22phox
are dominant inhibitors of Nox1- and Nox2-dependent reactive oxygen
generation. J Biol Chem. 280:31859–31869. 2005.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Martyn KD, Frederick LM, von Loehneysen K,
Dinauer MC and Knaus UG: Functional analysis of Nox4 reveals unique
characteristics compared to other NADPH oxidases. Cell Signal.
18:69–82. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Nakano Y, Banfi B, Jesaitis AJ, Dinauer
MC, Allen LA and Nauseef WM: Critical roles for p22phox in the
structural maturation and subcellular targeting of Nox3. Biochem J.
403:97–108. 2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
von Löhneysen K, Noack D, Wood MR,
Friedman JS and Knaus UG: Structural insights into Nox4 and Nox2:
Motifs involved in function and cellular localization. Mol Cell
Bio. 30:961–975. 2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Petry A, Zhang Z, Trautz B, Rieß F and
Görlach A: Cross talk between p22phox and ATF4 in the endothelial
unfolded protein response. Antioxid Redox Signal. 30:40–55.
2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Li Q, Feng X, Niu F, Yang J, Xu Y, Pu X,
Chen J, Fan X, Jiang B and Huang Q: Inhibition of
p22phox suppresses epithelial ovarian cancer cell
proliferation and tumorigenesis. J Cancer. 12:4277–4287.
2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Block K, Gorin Y, New DD, Eid A, Chelmicki
T, Reed A, Choudhury GG, Parekh DJ and Abboud HE: The NADPH oxidase
subunit p22phox inhibits the function of the tumor suppressor
protein tuberin. Am J Pathol. 176:2447–2455. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Edderkaoui M, Nitsche C, Zheng L, Pandol
SJ, Gukovsky I and Gukovskaya AS: NADPH oxidase activation in
pancreatic cancer cells is mediated through Akt-dependent
up-regulation of p22phox. J Biol Chem. 286:7779–7787.
2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Li Q, Fu GB, Zheng JT, He J, Niu XB, Chen
QD, Yin Y, Qian X, Xu Q, Wang M, et al: NADPH oxidase subunit
p22(phox)-mediated reactive oxygen species contribute to
angiogenesis and tumor growth through AKT and ERK1/2 signaling
pathways in prostate cancer. Biochim Biophys Acta. 1833:3375–3385.
2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kobayashi M, Saito R, Miki Y, Nanamiya R,
Inoue C, Abe J, Sato I, Okada Y and Sasano H: The correlation of
p22phox and chemosensitivity in EGFR-TKI resistant lung
adenocarcinoma. Oncotarget. 10:1119–1131. 2019.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Tian H, Gao Z, Li H, Zhang B, Wang G,
Zhang Q, Pei D and Zheng J: DNA damage response-a double-edged
sword in cancer prevention and cancer therapy. Cancer Lett.
358:8–16. 2015.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Romani AMP: Cisplatin in cancer treatment.
Biochem Pharmacol. 206(115323)2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Azuma M, Harada K, Supriatno Tamatani T,
Motegi K, Ashida Y and Sato M: Potentiation of induction of
apoptosis by sequential treatment with cisplatin followed by
5-fluorouracil in human oral cancer cells. Int J Oncol.
24:1449–1455. 2004.PubMed/NCBI
|
|
35
|
Andreadis C, Vahtsevanos K, Sidiras T,
Thomaidis I, Antoniadis K and Mouratidou D: 5-Fluorouracil and
cisplatin in the treatment of advanced oral cancer. Oral Oncol.
39:380–385. 2003.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hartner L: Chemotherapy for oral cancer.
Dent Clin North Am. 62:87–97. 2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Hiraishi Y, Wada T, Nakatani K, Tojyo I,
Matsumoto T, Kiga N, Negoro K and Fujita S: EGFR inhibitor enhances
cisplatin sensitivity of oral squamous cell carcinoma cell lines.
Pathol Oncol Res. 14:39–43. 2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Takaoka S, Iwase M, Uchida M, Yoshiba S,
Kondo G, Watanabe H, Ohashi M, Nagumo M and Shintani S: Effect of
combining epidermal growth factor receptor inhibitors and cisplatin
on proliferation and apoptosis of oral squamous cell carcinoma
cells. Int J Oncol. 30:1469–1476. 2007.PubMed/NCBI
|
|
39
|
Galluzzi L, Vitale I, Michels J, Brenner
C, Szabadkai G, Harel-Bellan A, Castedo M and Kroemer G: Systems
biology of cisplatin resistance: Past, present and future. Cell
Death Dis. 5(e1257)2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Komatsu M, Sumizawa T, Mutoh M, Chen ZS,
Terada K, Furukawa T, Yang XL, Gao H, Miura N, Sugiyama T and
Akiyama S: Copper-transporting P-type adenosine triphosphatase
(ATP7B) is associated with cisplatin resistance. Cancer Res.
60:1312–1316. 2000.PubMed/NCBI
|
|
41
|
Liedert B, Materna V, Schadendorf D,
Thomale J and Lage H: Overexpression of Cmoat (MRP2/ABCC2) is
associated with decreased formation of platinum-DNA adducts and
decreased G2-arrest in melanoma cells resistant to cisplatin. J
Invest Dermatol. 121:172–176. 2003.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Chen HH and Kuo MT: Role of glutathione in
the regulation of cisplatin resistance in cancer chemotherapy. Met
Based Drugs. 2010(430939)2010.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Kasahara K, Fujiwara Y, Nishio K, Ohmori
T, Sugimoto Y, Komiya K, Matsuda T and Saijo N: Metallothionein
content correlates with the sensitivity of human small cell lung
cancer cell lines to cisplatin. Cancer Res. 51:3237–3242.
1991.PubMed/NCBI
|
|
44
|
Jun HJ, Ahn MJ, Kim HS, Yi SY, Han J, Lee
SK, Ahn YC, Jeong HS, Son YI, Baek JH and Park K: ERCC1 expression
as a predictive marker of squamous cell carcinoma of the head and
neck treated with cisplatin-based concurrent chemoradiation. Br J
Cancer. 99:167–172. 2008.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Olaussen KA: A new step ahead for the
consideration of ERCC1 as a candidate biomarker to select NSCLC
patients for the treatment of cetuximab in combination with
cisplatin. Cancer Biol Ther. 8:1922–1923. 2009.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Branch P, Masson M, Aquilina G, Bignami M
and Karran P: Spontaneous development of drug resistance: Mismatch
repair and p53 defects in resistance to cisplatin in human tumor
cells. Oncogene. 19:3138–3145. 2000.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Brozovic A, Fritz G, Christmann M,
Zisowsky J, Jaehde U, Osmak M and Kaina B: Long-term activation of
SAPK/JNK, p38 kinase and fas-L expression by cisplatin is
attenuated in human carcinoma cells that acquired drug resistance.
Int J Cancer. 112:974–985. 2004.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Wu T, Wang MC, Jing L, Liu ZY, Guo H, Liu
Y, Bai YY, Cheng YZ, Nan KJ and Liang X: Autophagy facilitates lung
adenocarcinoma resistance to cisplatin treatment by activation of
AMPK/mTOR signaling pathway. Drug Des Devel Ther. 9:6421–6431.
2015.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Chiu TJ, Chen CH, Chien CY, Li SH, Tsai HT
and Chen YJ: High ERCC1 Expression predicts cisplatin-based
chemotherapy resistance and poor outcome in unresectable squamous
cell carcinoma of head and neck in a betel-chewing area. J Trans
Med. 9(31)2011.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Hsu DS, Lan HY, Huang CH, Tai SK, Chang
SY, Tsai TL, Chang CC, Tzeng CH, Wu KJ, Kao JY and Yang MH:
Regulation of excision repair cross-complementation group 1 by
snail contributes to cisplatin resistance in head and neck cancer.
Clin Cancer Res. 16:4561–4571. 2010.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Amable L: Cisplatin resistance and
opportunities for precision medicine. Pharmacol Res. 106:27–36.
2016.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Gao F, Han J, Wang Y, Jia L, Luo W and
Zeng Y: Circ_0109291 promotes cisplatin resistance of oral squamous
cell carcinoma by sponging miR-188-3p to increase ABCB1 expression.
Cancer Biother Radiopharm. 37:233–245. 2022.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Sasabe E, Zhou X, Li D, Oku N, Yamamoto T
and Osaki T: The involvement of hypoxia-inducible factor-1alpha in
the susceptibility to gamma-rays and chemotherapeutic drugs of oral
squamous cell carcinoma cells. Int J Cancer. 120:268–277.
2007.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Li S, Wu Y, Ding Y, Yu M and Ai Z: CerS6
regulates cisplatin resistance in oral squamous cell carcinoma by
altering mitochondrial fission and autophagy. J Cell Physiol.
233:9416–925. 2018.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Hellberg V, Wallin I, Eriksson S, Hernlund
E, Jerremalm E, Berndtsson M, Eksborg S, Arnér ES, Shoshan M,
Ehrsson H and Laurell G: Cisplatin and oxaliplatin toxicity:
Importance of cochlear kinetics as a determinant for ototoxicity. J
Natl Cancer Inst. 101:37–47. 2009.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Cassidy J and Misset JL:
Oxaliplatin-related side effects: Characteristics and management.
Semin Oncol. 29 (5 Suppl 15):S11–S20. 2002.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Wheate NJ, Walker S, Craig GE and Oun R:
The status of platinum anticancer drugs in the clinic and in
clinical trials. Dalton Trans. 39:8113–8127. 2010.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Li D, Kou Y, Gao Y, Liu S, Yang P,
Hasegawa T, Su R, Guo J and Li M: Oxaliplatin induces the
PARP1-mediated parthanatos in oral squamous cell carcinoma by
increasing production of ROS. Aging (Albany NY). 13:4242–4257.
2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Alcindor T and Beauger N: Oxaliplatin: A
review in the era of molecularly targeted therapy. Curr Oncol.
18:18–25. 2011.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Okamura M, Kobayashi M, Suzuki F, Shimada
J and Sakagami H: Induction of cell death by combination treatment
with cisplatin and 5-fluorouracil in a human oral squamous cell
carcinoma cell line. Anticancer Res. 27:3331–3337. 2007.PubMed/NCBI
|
|
61
|
Downward J: PI 3-kinase, Akt and cell
survival. Semin Cell Dev Biol. 15:177–182. 2004.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Song G, Ouyang G and Bao S: The activation
of Akt/PKB signaling pathway and cell survival. J Cell Mol Med.
9:59–71. 2005.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Wang M, Liu ZM, Li XC, Yao YT and Yin ZX:
Activation of ERK1/2 and Akt is associated with cisplatin
resistance in human lung cancer cells. J Chemother. 25:162–169.
2013.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Wang Y, Chen L, Huang G, He D, He J, Xu W,
Zou C, Zong F, Li Y, Chen B, et al: Klotho sensitizes human lung
cancer cell line to cisplatin via PI3k/Akt pathway. PLoS One.
8(e57391)2013.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Zhang LL, Zhang J, Shen L, Xu XM and Yu
HG: Overexpression of AKT decreases the chemosensitivity of gastric
cancer cells to cisplatin in vitro and in vivo. Mol Med Rep.
7:1387–1390. 2013.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Fan L, Song B, Sun G, Ma T, Zhong F and
Wei W: Endoplasmic reticulum stress-induced resistance to
Doxorubicin is reversed by paeonol treatment in human
hepatocellular carcinoma cells. PLoS One. 8(e62627)2013.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Lin Y, Wang Z, Liu L and Chen L: Akt is
the downstream target of GRP78 in mediating cisplatin resistance in
ER stress-tolerant human lung cancer cells. Lung Cancer.
71:291–297. 2011.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Pabla N, Huang S, Mi QS, Daniel R and Dong
Z: ATR-Chk2 signaling in p53 activation and DNA damage response
during cisplatin-induced apoptosis. J Biol Chem. 283:6572–6583.
2008.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Shieh SY, Ahn J, Tamai K, Taya Y and
Prives C: The human homologs of checkpoint kinases Chk1 and Cds1
(Chk2) phosphorylate p53 at multiple DNA damage-inducible sites.
Genes Dev. 14:289–300. 2000.PubMed/NCBI
|
|
70
|
Zhao H and Piwnica-Worms H: ATR-mediated
checkpoint pathways regulate phosphorylation and activation of
human Chk1. Mol Cell Biol. 21:4129–4139. 2001.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Arnesano F, Nardella MI and Natile G:
Platinum drugs, copper transporters and copper chelators. Coord
Chem Rev. 374:254–260. 2018.
|
|
72
|
Karasawa T, Sibrian-Vazquez M, Strongin RM
and Steyger PS: Identification of cisplatin-binding proteins using
agarose conjugates of platinum compounds. PLoS One.
8(e66220)2013.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Zhao T and King FL: Direct determination
of the primary binding site of cisplatin on cytochrome c by mass
spectrometry. J Am Soc Mass Spectrom. 20:1141–1147. 2009.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Li H, Zhao Y, Phillips HI, Qi Y, Lin TY,
Sadler PJ and O'Connor PB: Mass spectrometry evidence for cisplatin
as a cross-linking reagent. Anal Chem. 83:5369–5376.
2011.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Tanley SW and Helliwell JR: Structural
dynamics of cisplatin binding to histidine in a protein. Struct
Dyn. 1(034701)2014.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Seflova J, Cechova P, Stenclova T, Sebela
M and Kubala M: Identification of cisplatin-binding sites on the
large cytoplasmic loop of the Na+/K+-ATPase.
J Enzym Inhib Med Chem. 33:701–706. 2018.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Wu Z, Lou Y, Jin W, Liu Y, Lu L, Chen Q,
Xie Y and Lu G: Relationship of the p22phox (CYBA) gene
polymorphism C242T with risk of coronary artery disease: A
meta-analysis. PLoS One. 8(e70885)2013.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Mehranpour P, Wang SS, Blanco RR, Li W,
Song Q, Lassegue B, Dikalov SI, Austin H and Zafari AM: The C242T
CYBA polymorphism as a major determinant of NADPH oxidase activity
in patients with cardiovascular disease. Cardiovasc Hematol Agents
Med Chem. 7:251–259. 2009.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Moltgen S, Piumatti E, Massafra GM,
Metzger S, Jaehde U and Kalayda GV: Cisplatin protein binding
partners and their relevance for platinum drug sensitivity. Cells.
9(1322)2020.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Hirano T, Kato H, Maeda M, Gong Y, Shou Y,
Nakamura M, Maeda J, Yashima K, Kato Y and Akimoto S: , et
al: Identification of postoperative adjuvant chemotherapy
responders in non-small cell lung cancer by novel biomarker. Int J
Cancer. 117:460–468. 2005.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Surowiak P, Materna V, Kaplenko I,
Spaczýnski M, Dietel M, Lage H and Zabel M: Augmented expression of
metallothionein and glutathione S-transferase pi as unfavourable
prognostic factors in cisplatin-treated ovarian cancer patients.
Virchows Arch. 447:626–633. 2005.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Hishikawa Y, Abe S, Kinugasa S, Yoshimura
H, Monden N, Igarashi M, Tachibana M and Nagasue N: Overexpression
of metallothionein correlates with chemoresistance to cisplatin and
prognosis in esophageal cancer. Oncology. 54:342–347.
1997.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Kelley SL, Basu A, Teicher BA, Hacker MP,
Hamer DH and Lazo JS: Overexpression of metallothionein confers
resistance to anticancer drugs. Science. 241:1813–1815.
1988.PubMed/NCBI View Article : Google Scholar
|
|
84
|
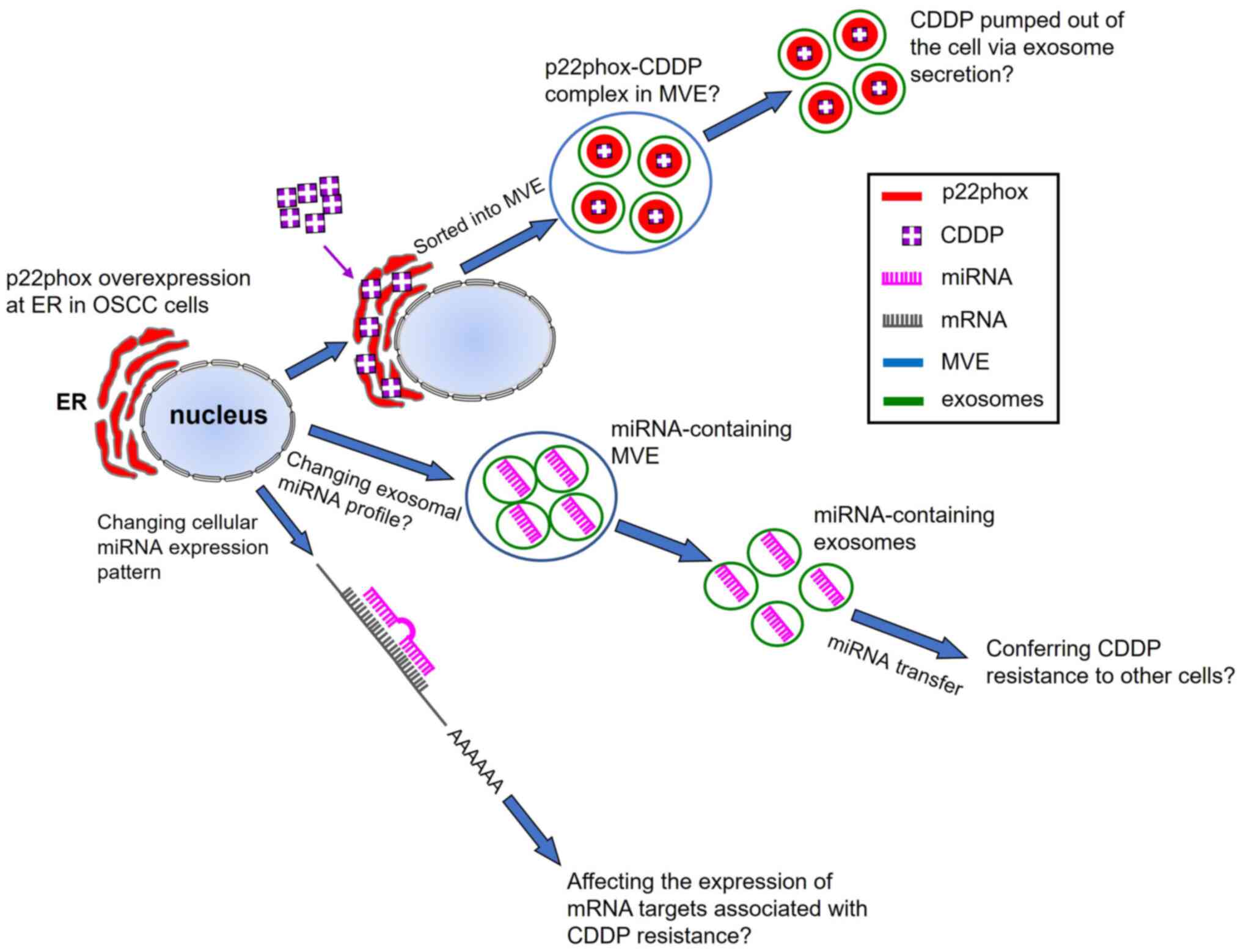
Khoo XH, Paterson IC, Goh BH and Lee WL:
Cisplatin-resistance in oral squamous cell carcinoma: Regulation by
tumor cell-derived extracellular vesicles. Cancers.
11(1166)2019.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Safaei R, Larson BJ, Cheng TC, Gibson MA,
Otani S, Naerdemann W and Howell SB: Abnormal lysosomal trafficking
and enhanced exosomal export of cisplatin in drug-resistant human
ovarian carcinoma cells. Mol Cancer Ther. 4:1595–1604.
2005.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Liu T, Chen G, Sun D, Lei M, Li Y, Zhou C,
Li X, Xue W, Wang H, Liu C and Xu J: Exosomes containing miR-21
transfer the characteristic of cisplatin resistance by targeting
PTEN and PDCD4 in oral squamous cell carcinoma. Acta Biochim
Biophys Sin (Shanghai). 49:808–816. 2017.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Chen WX, Liu XM, Lv MM, Chen L, Zhao JH,
Zhong SL, Ji MH, Hu Q, Luo Z, Wu JZ and Tang JH: Exosomes from
drug-resistant breast cancer cells transmit chemoresistance by a
horizontal transfer of microRNAs. PLoS One.
9(e95240)2014.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Zhang T, Zhang P and Li HX: CAFs-derived
exosomal miRNA-130a confers cisplatin resistance of NSCLC cells
through PUM2-dependent packaging. Int J Nanomedicine. 16:561–577.
2021.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Liu H, Huang Y, Huang M, Huang Z, Wang Q,
Qing L, Li L, Xu S and Jia B: Current status, opportunities, and
challenges of exosomes in oral cancer diagnosis and treatment. Int
J Nanomedicine. 17:2679–2705. 2022.PubMed/NCBI View Article : Google Scholar
|