|
1
|
Morgan E, Soerjomataram I, Rumgay H,
Coleman HG, Thrift AP, Vignat J, Laversanne M, Ferlay J and Arnold
M: The global landscape of esophageal squamous cell carcinoma and
esophageal adenocarcinoma incidence and mortality in 2020 and
projections to 2040: New estimates from GLOBOCAN 2020.
Gastroenterology. 163:649–658.e2. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mattiuzzi C and Lippi G: Current cancer
epidemiology. J Epidemiol Glob Health. 9:217–222. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
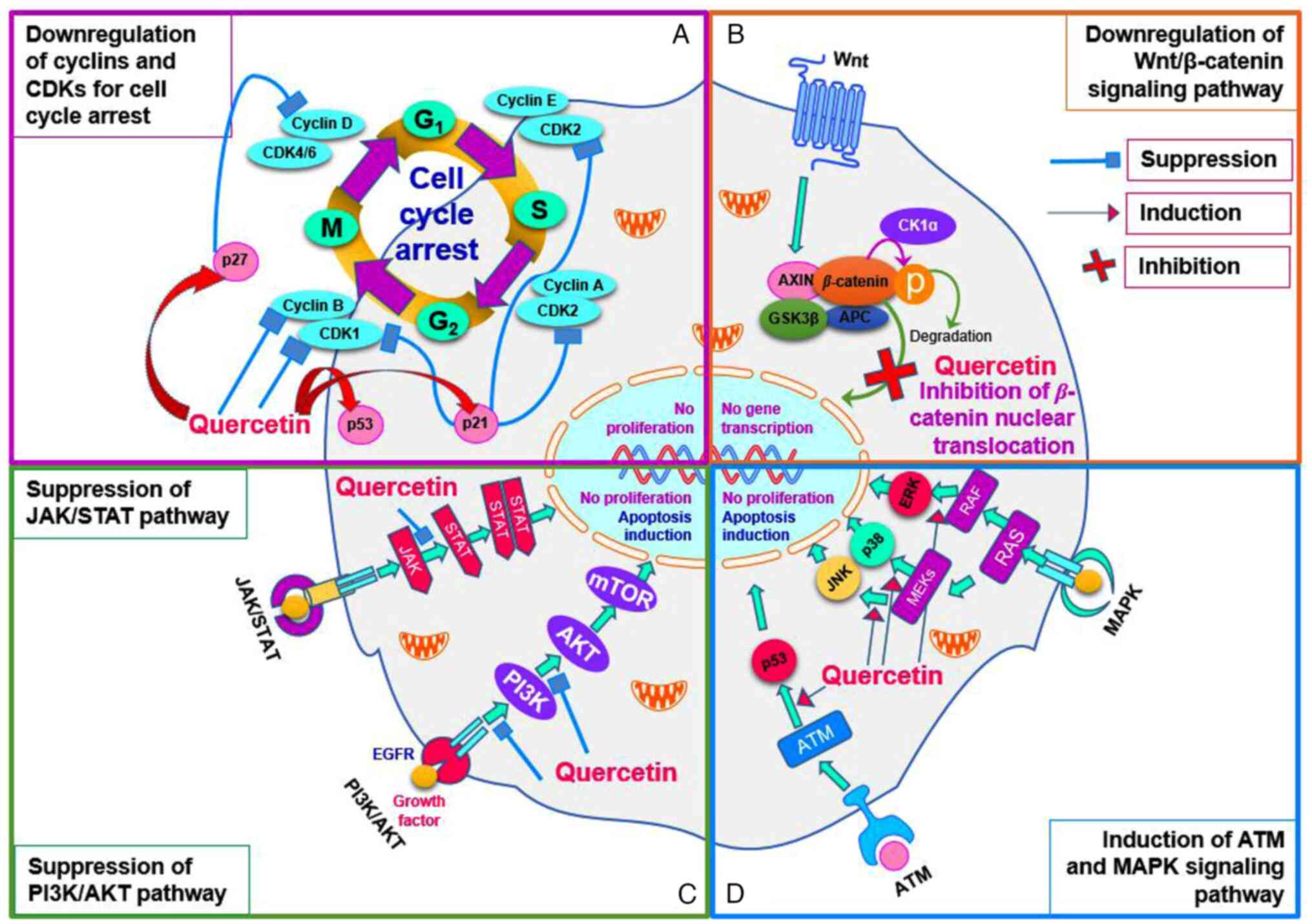
Sayiner M, Golabi P and Younossi ZM:
Disease burden of hepatocellular carcinoma: A global Dig Dis. Sci.
64:910–917. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
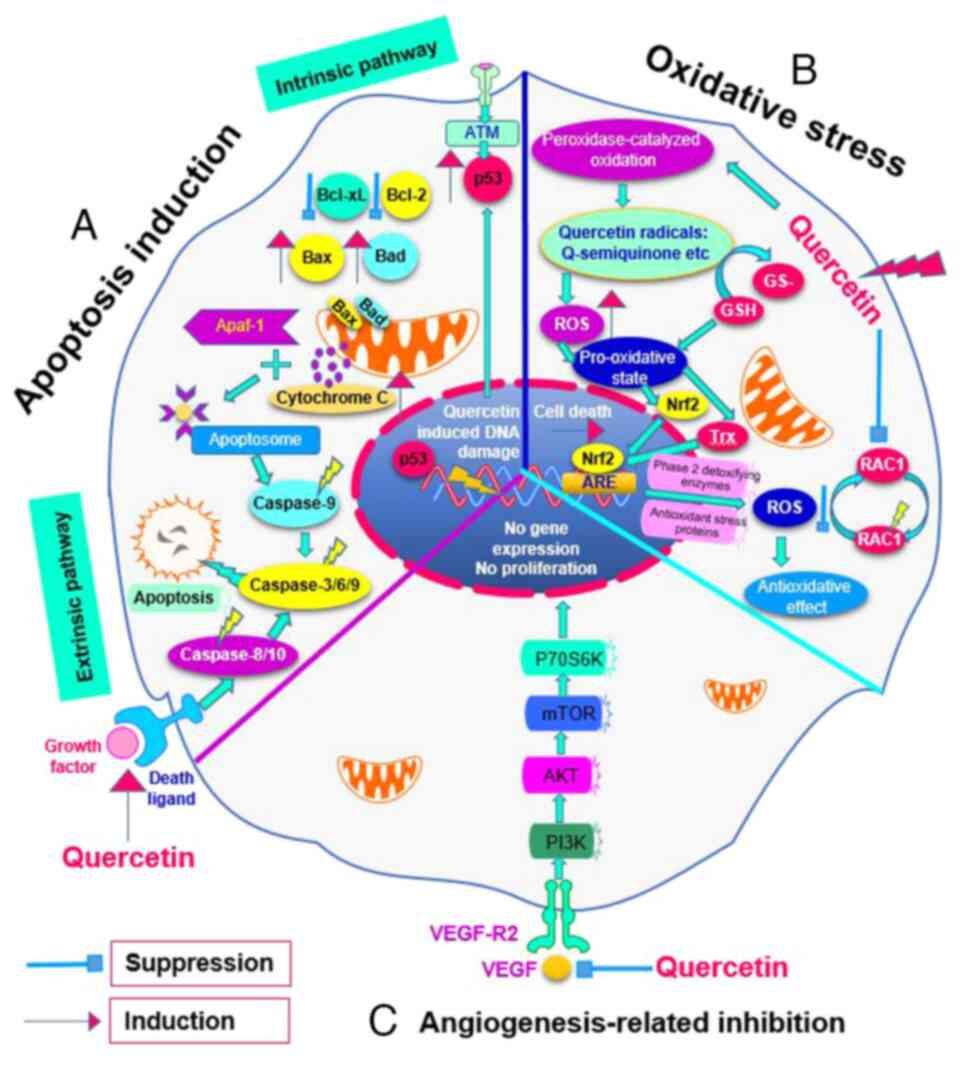
|
Joyce H, McCann A, Clynes M and Larkin A:
Influence of multidrug resistance and drug transport proteins on
chemotherapy drug metabolism. Expert Opin Drug Metab Toxicol.
11:795–809. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lundqvist EÅ, Fujiwara K and Seoud M:
Principles of chemotherapy. Int J Gynaecol Obstet. 131 (Suppl
2):S146–S149. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wu H, Wei M, Xu Y, Li Y, Zhai X, Su P, Ma
Q and Zhang H: PDA-based drug delivery nanosystems: A potential
approach for glioma treatment. Int J Nanomedicine. 17:3751–3775.
2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ding Y, Li W, Zhang F, Liu Z, Zanjanizadeh
Ezazi N, Liu D and Santos HA: Electrospun fibrous architectures for
drug delivery, tissue engineering and cancer therapy. Adv Funct
Mater. 29(1802852)2019.
|
|
9
|
Ali I, Nadeem Lone M, Suhail M, Danish
Mukhtar S and Asnin L: Advances in nanocarriers for anticancer
drugs delivery. Curr Med Chem. 23:2159–2187. 2016.PubMed/NCBI View Article : Google Scholar
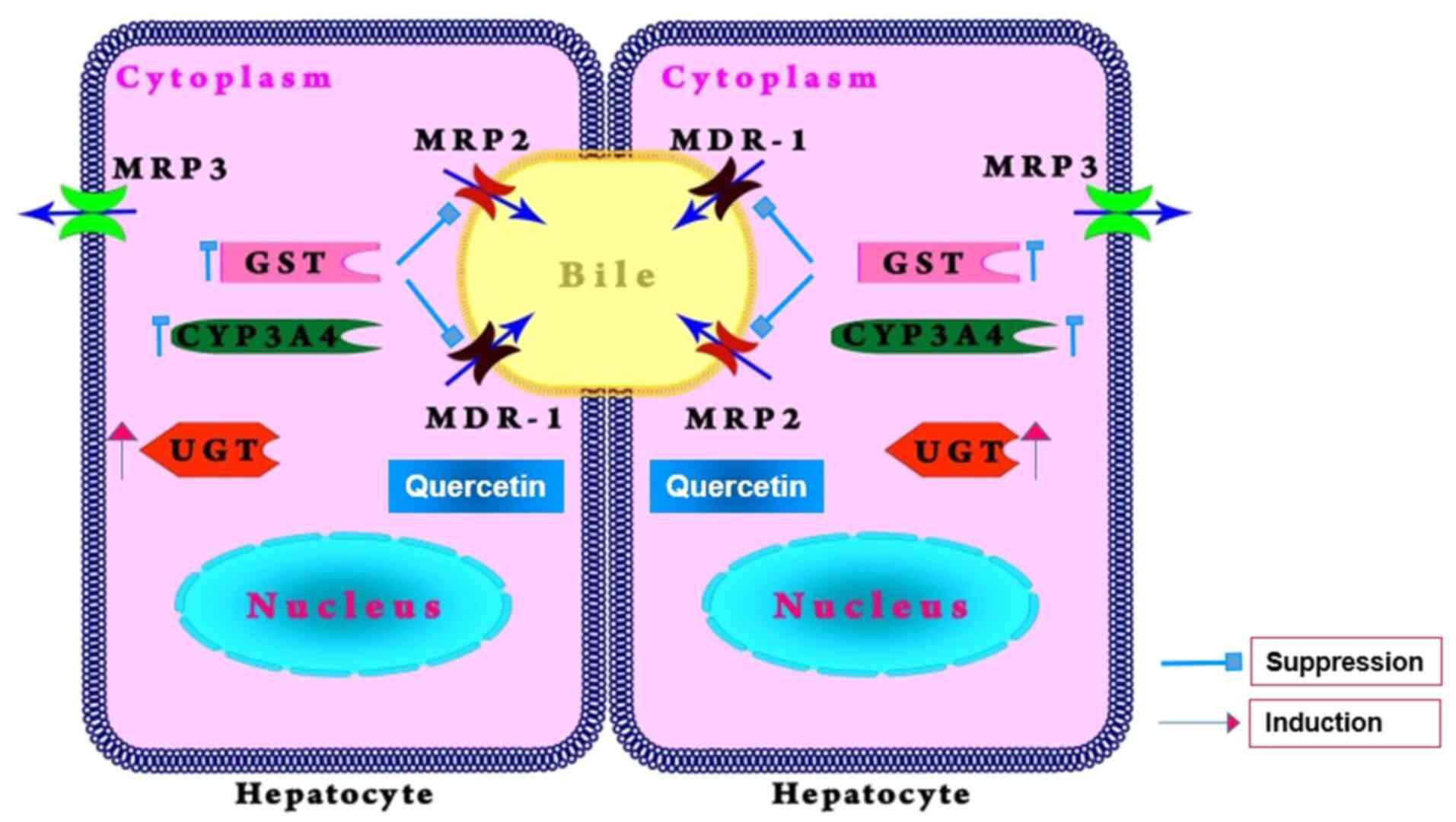
|
|
10
|
Sun Y, Su J, Liu G, Chen J, Zhang X, Zhang
R, Jiang M and Qiu M: Advances of blood cell-based drug delivery
systems. Eur J Pharm Sci. 96:115–128. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Upadhyay RK: Therapeutic and
pharmaceutical potential of Cinnamomum tamala. Res Rev Pharm
Pharm Sci. 6:18–28. 2017.
|
|
12
|
Sultana S, Munir N, Mahmood Z, Riaz M,
Akram M, Rebezov M, Kuderinova N, Moldabayeva Z, Shariati MA, Rauf
A and Rengasamy KRR: Molecular targets for the management of cancer
using Curcuma longa Linn. phytoconstituents: A review.
Biomed Pharmacother. 135(111078)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Taleghani A, Emami SA and Tayarani-Najaran
Z: Artemisia: A promising plant for the treatment of cancer.
Bioorg Med Chem. 28(115180)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ji S, Li Z, Song W, Wang Y, Liang W, Li K,
Tang S, Wang Q, Qiao X, Zhou D, et al: Bioactive constituents of
Glycyrrhiza uralensis (Licorice): Discovery of the effective
components of a traditional herbal medicine. J Nat Prod.
79:281–292. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Makia R, Al-Sammarrae K, Al-Halbosiy M and
Al-Mashhadani M: In vitro cytotoxic activity of total flavonoid
from Equisetum arvense extract. Rep Biochem Mol Biol.
11:487–492. 2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lee D, Park S, Choi S, Kim SH and Kang KS:
In vitro estrogenic and breast cancer inhibitory activities of
chemical constituents isolated from Rheum undulatum L.
Molecules. 23(1215)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cheng CS, Chen J, Tan HY, Wang N, Chen Z
and Feng Y: Scutellaria baicalensis and cancer treatment:
Recent progress and perspectives in biomedical and clinical
studies. Am J Chin Med. 46:25–54. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Men K, Duan X, Wei XW, Gou ML, Huang MJ,
Chen LJ, Qian ZY and Wei YQ: Nanoparticle-delivered quercetin for
cancer therapy. Anticancer Agents Med Chem. 14:826–832.
2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
An T, Yin H, Lu Y and Liu F: The emerging
potential of parthenolide nanoformulations in tumor therapy. Drug
Des Devel Ther. 16:1255–1272. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Dang X, Cho S, Wang H, Seok WJ, Ha JH and
Kim IH: Quercetin extracted from Sophora japonica flower improves
growth performance, nutrient digestibility, cecal microbiota, organ
indexes, and breast quality in broiler chicks. Anim Biosci.
35:577–586. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lekar AV, Borisenko SN, Vetrova EV,
Sushkova SN and Borisenko NI: Extraction of quercetin from
Polygonum hydropiper L. by subcritical water. Am J Agric
Biol Sci. 9:1–5. 2014.
|
|
22
|
Yang HH, Hwangbo K, Zheng MS, Cho JH, Son
JK, Kim HY, Baek SH, Choi HC, Park SY and Kim JR:
Quercetin-3-O-β-D-glucuronide isolated from Polygonum
aviculare inhibits cellular senescence in human primary cells.
Arch Pharm Res. 37:1219–1233. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Anand David AV, Arulmoli R and Parasuraman
S: Overviews of Biological importance of quercetin: A bioactive
flavonoid. Pharmacogn Rev. 10:84–89. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Michala AS and Pritsa A: Quercetin: A
molecule of great biochemical and clinical value and its beneficial
effect on diabetes and cancer. Diseases. 10(37)2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang SY, Duan KM, Li Y, Mei Y, Sheng H,
Liu H, Mei X, Ouyang W, Zhou HH and Liu ZQ: Effect of quercetin on
P-glycoprotein transport ability in Chinese healthy subjects. Eur J
Clin Nutr. 67:390–394. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Davoodvandi A, Shabani Varkani M, Clark
CCT and Jafarnejad S: Quercetin as an anticancer agent: Focus on
esophageal cancer. J Food Biochem. 44(e13374)2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Vafadar A, Shabaninejad Z, Movahedpour A,
Fallahi F, Taghavipour M, Ghasemi Y, Akbari M, Shafiee A,
Hajighadimi S, Moradizarmehri S, et al: Quercetin and cancer: New
insights into its therapeutic effects on ovarian cancer cells. Cell
Biosci. 10(31)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Jeong JH, An JY, Kwon YT, Rhee JG and Lee
YJ: Effects of low dose quercetin: Cancer cell-specific inhibition
of cell cycle progression. J Cell Biochem. 106:73–82.
2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ganthala PD, Alavala S, Chella N,
andugulapati SB, Bathini NB and Sistla R: Co-encapsulated
nanoparticles of erlotinib and quercetin for targeting lung cancer
through nuclear EGFR and PI3K/AKT inhibition. Colloids Surf B
Biointerfaces. 211(112305)2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Safi A, Heidarian E and Ahmadi R:
Quercetin synergistically enhances the anticancer efficacy of
docetaxel through induction of apoptosis and modulation of
PI3K/AKT, MAPK/ERK and JAK/STAT3 signaling pathways in MDA-MB-231
breast cancer cell line. Int J Mol Cell Med. 10:11–22.
2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Guo T, Wu C, Zhang J, Yu J, Li G, Jiang H,
Zhang X, Yu R and Liu X: Dual blockade of EGFR and PI3K signaling
pathways offers a therapeutic strategy for glioblastoma. Cell
Commun Signal. 21(363)2023.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Li Y, Han N, Hou P, Zhao FQ and Liu H:
Roles of MAPK and Nrf2 signaling pathways in quercetin alleviating
redox imbalance induced by hydrogen peroxide in mammary epithelial
cells. Anim Nutr. 1(e1)2024.
|
|
33
|
Liu W, Chen D, Su J, Zheng R, Kong R, Zhu
B, Dong H and Li Y: Quercetin induced HepG2 cells apoptosis through
ATM/JNK/STAT3 signaling pathways. Biocell. 47:187–194. 2023.
|
|
34
|
Wang ZX, Ma J, Li XY, Wu Y, Shi H, Chen Y,
Lu G, Shen HM, Lu GD and Zhou J: Quercetin induces p53-independent
cancer cell death through lysosome activation by the transcription
factor EB and reactive oxygen species-dependent ferroptosis. Br J
Pharmacol. 178:1133–1148. 2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chan ST, Yang NC, Huang CS, Liao JW and
Yeh SL: Quercetin enhances the antitumor activity of trichostatin A
through upregulation of p53 protein expression in vitro and in
vivo. PLoS One. 8(e54255)2013.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Granado-Serrano AB, Martín MA, Bravo L,
Goya L and Ramos S: Quercetin induces apoptosis via caspase
activation, regulation of Bcl-2, and inhibition of PI-3-kinase/Akt
and ERK pathways in a human hepatoma cell line (HepG2). J Nutr.
136:2715–2721. 2006.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Lee DH, Szczepanski M and Lee YJ: Role of
Bax in quercetin-induced apoptosis in human prostate cancer cells.
Biochem Pharmacol. 75:2345–2355. 2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Huang CF, Liu SH, Ho TJ, Lee KI, Fang KM,
Lo WC, Liu JM, Wu CC and Su CC: Quercetin induces tongue squamous
cell carcinoma cell apoptosis via the JNK activation-regulated
ERK/GSK-3α/β-mediated mitochondria-dependent apoptotic signaling
pathway. Oncol Lett. 23(78)2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Xu D, Hu MJ, Wang YQ and Cui YL:
Antioxidant activities of quercetin and its complexes for medicinal
application. Molecules. 24(1123)2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Lee YJ, Lee DM and Lee SH: Nrf2 expression
and apoptosis in quercetin-treated malignant mesothelioma cells.
Mol Cells. 38:416–425. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Rashidi Z, Aleyasin A, Eslami M, Nekoonam
S, Zendedel A, Bahramrezaie M and Amidi F: Quercetin protects human
granulosa cells against oxidative stress via thioredoxin system.
Reprod Biol. 19:245–254. 2019.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Baba RA, Mir HA, Mokhdomi TA, Bhat HF,
Ahmad A and Khanday FA: Quercetin suppresses ROS production and
migration by specifically targeting Rac1 activation in gliomas.
Front Pharmacol. 15(1318797)2024.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Biswas P, Dey D, Biswas PK, Rahaman TI,
Saha S, Parvez A, Khan DA, Lily NJ, Saha K, Sohel M, et al: A
comprehensive analysis and anti-cancer activities of quercetin in
ROS-mediated cancer and cancer stem cells. Int J Mol Sci.
23(11746)2022.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Zhang Q, Cheng G, Qiu H, Zhu L, Ren Z,
Zhao W, Zhang T and Liu L: The p53-inducible gene 3 involved in
flavonoid-induced cytotoxicity through the reactive oxygen
species-mediated mitochondrial apoptotic pathway in human hepatoma
cells. Food Funct. 6:1518–1525. 2015.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Pratheeshkumar P, Budhraja A, Son YO, Wang
X, Zhang Z, Ding S, Wang L, Hitron A, Lee JC, Xu M, et al:
Quercetin inhibits angiogenesis mediated human prostate tumor
growth by targeting VEGFR-2 regulated AKT/mTOR/P70S6K signaling
pathways. PLoS One. 7(e47516)2012.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Igura K, Ohta T, Kuroda Y and Kaji K:
Resveratrol and quercetin inhibit angiogenesis in vitro. Cancer
Lett. 171:11–16. 2001.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Okumo T, Furuta A, Kimura T, Yusa K, Asano
K and Sunagawa M: Inhibition of angiogenic factor productions by
quercetin in vitro and in vivo. Medicines (Basel).
8(22)2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Ren KW, Li YH, Wu G, Ren JZ, Lu HB, Li ZM
and Han XW: Quercetin nanoparticles display antitumor activity via
proliferation inhibition and apoptosis induction in liver cancer
cells. Int J Oncol. 50:1299–1311. 2017.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Guan X, Gao M, Xu H, Zhang C, Liu H, Lv L,
Deng S, Gao D and Tian Y: Quercetin-loaded poly (lactic-co-glycolic
acid)-d-α-tocopheryl polyethylene glycol 1000 succinate
nanoparticles for the targeted treatment of liver cancer. Drug
Deliv. 23:3307–3318. 2016.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Srisa-Nga K, Mankhetkorn S, Okonogi S and
Khonkarn R: Delivery of superparamagnetic polymeric micelles loaded
with quercetin to hepatocellular carcinoma cells. J Pharm Sci.
108:996–1006. 2019.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Wang C, Su L, Wu C, Wu J, Zhu C and Yuan
G: RGD peptide targeted lipid-coated nanoparticles for
combinatorial delivery of sorafenib and quercetin against
hepatocellular carcinoma. Drug Dev Ind Pharm. 42:1938–1944.
2016.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Deng Q, Huang Y, Zeng J, Li X, Zheng X,
Guo L, Shi J and Bai L: Recent advancements in the small-molecule
drugs for hepatocellular carcinoma (HCC): Structure-activity
relationships, pharmacological activities, and the clinical trials.
Biomed Pharmacother. 179(117343)2024.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Tang W, Chen Z, Zhang W, Cheng Y, Zhang B,
Wu F, Wang Q, Wang S, Rong D, Reiter FP, et al: The mechanisms of
sorafenib resistance in hepatocellular carcinoma: Theoretical basis
and therapeutic aspects. Signal Transduct Target Ther.
5(87)2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Pradhan A, Kumari A, Srivastava R and
Panda D: Quercetin encapsulated biodegradable plasmonic
nanoparticles for photothermal therapy of hepatocellular carcinoma
cells. ACS Appl Bio Mater. 2:5727–5738. 2019.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Varshosaz J, Jafarian A, Salehi G and
Zolfaghari B: Comparing different sterol containing solid lipid
nanoparticles for targeted delivery of quercetin in hepatocellular
carcinoma. J Liposome Res. 24:191–203. 2014.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Koulouris A, Tsagkaris C, Spyrou V, Pappa
E, Troullinou A and Nikolaou M: Hepatocellular carcinoma: An
overview of the changing landscape of treatment options. J
Hepatocell Carcinoma. 8:387–401. 2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Bukowski K, Kciuk M and Kontek R:
Mechanisms of multidrug resistance in cancer chemotherapy. Int J
Mol Sci. 21(3233)2020.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Talib WH, Alsayed AR, Barakat M, Abu-Taha
MI and Mahmod AI: Targeting drug chemo-resistance in cancer using
natural products. Biomedicines. 9(1353)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Al Saihati HA and Rabaan AA: Cellular
resistance mechanisms in cancer and the new approaches to overcome
resistance mechanisms chemotherapy. Saudi Med J. 44:329–344.
2023.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Halder J, Pradhan D, Kar B, Ghosh G and
Rath G: Nanotherapeutics approaches to overcome
P-glycoprotein-mediated multi-drug resistance in cancer.
Nanomedicine. 40(102494)2022.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Waghray D and Zhang Q: Inhibit or evade
multidrug resistance P-glycoprotein in cancer treatment:
Miniperspective. J Med Chem. 61:5108–5121. 2017.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Li S, Zhao Q, Wang B, Yuan S, Wang X and
Li K: Quercetin reversed MDR in breast cancer cells through
down-regulating P-gp expression and eliminating cancer stem cells
mediated by YB-1 nuclear translocation. Phytother Res.
32:1530–1536. 2018.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Ganesan M, Kanimozhi G, Pradhapsingh B,
Khan HA, Alhomida AS, Ekhzaimy A, Brindha GR and Prasad NR:
Phytochemicals reverse P-glycoprotein mediated multidrug resistance
via signal transduction pathways. Biomed Pharmacother.
139(111632)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Suroowan S, Abdallah HH and Mahomoodally
MF: Herb-drug interactions and toxicity: Underscoring potential
mechanisms and forecasting clinically relevant interactions induced
by common phytoconstituents via data mining and computational
approaches. Food Chem Toxicol. 156(112432)2021.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Palmeira A, Sousa E, Vasconcelos MH and
Pinto MM: Three decades of P-gp inhibitors: Skimming through
several generations and scaffolds. Curr Med Chem. 19:1946–2025.
2012.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Gurunath S, Nanjwade BK and Patil PA: Oral
bioavailability and intestinal absorption of candesartan cilexetil:
Role of naringin as P-glycoprotein inhibitor. Drug Dev Ind Pharm.
41:170–176. 2015.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Di Sotto A, Irannejad H, Eufemi M,
Mancinelli R, Abete L, Mammola CL, Altieri F, Mazzanti G and Di
Giacomo S: Potentiation of low-dose doxorubicin cytotoxicity by
affecting P-glycoprotein through caryophyllane sesquiterpenes in
hepG2 cells: An in vitro and in silico study. Int J Mol Sci.
21(633)2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Dewanjee S, Dua TK, Bhattacharjee N, Das
A, Gangopadhyay M, Khanra R, Joardar S, Riaz M, Feo V and
Zia-Ul-Haq M: Natural products as alternative choices for
P-glycoprotein (P-gp) inhibition. Molecules. 22(871)2017.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Mohos V, Fliszár-Nyúl E, Ungvári O, Kuffa
K, Needs PW, Kroon PA, Telbisz Á, Özvegy-Laczka C and Poór M:
Inhibitory effects of quercetin and its main methyl, sulfate, and
glucuronic acid conjugates on cytochrome p450 enzymes, and on OATP,
BCRP and MRP2 transporters. Nutrients. 12(2306)2020.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Arinç E, Yilmaz D and Bozcaarmutlu A:
Mechanism of inhibition of CYP1A1 and glutathione S-transferase
activities in fish liver by quercetin, resveratrol, naringenin,
hesperidin, and rutin. Nutr Cancer. 67:137–144. 2015.PubMed/NCBI View Article : Google Scholar
|
|
71
|
van Zanden JJ, Ben Hamman O, van Iersel
ML, Boeren S, Cnubben NH, Lo Bello M, Vervoort J, van Bladeren PJ
and Rietjens IM: Inhibition of human glutathione S-transferase P1-1
by the flavonoid quercetin. Chem Biol Interact. 145:139–148.
2003.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Choi JS, Piao YJ and Kang KW: Effects of
quercetin on the bioavailability of doxorubicin in rats: role of
CYP3A4 and P-gp inhibition by quercetin. Arch Pharm Res.
34:607–613. 2011.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Borska S, Sopel M, Chmielewska M, Zabel M
and Dziegiel P: Quercetin as a potential modulator of
P-glycoprotein expression and function in cells of human pancreatic
carcinoma line resistant to daunorubicin. Molecules. 15:857–870.
2010.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Singh A, Patel SK, Kumar P, Das KC, Verma
D, Sharma R, Tripathi T, Giri R, Martins N and Garg N: Quercetin
acts as a P-gp modulator via impeding signal transduction from
nucleotide-binding domain to transmembrane domain. J Biomol Struct
Dyn. 40:4507–4515. 2020.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Mu Y, Fu Y, Li J, Yu X, Li Y, Wang Y, Wu
X, Zhang K, Kong M, Feng C and Chen X: Multifunctional quercetin
conjugated chitosan nano-micelles with P-gp inhibition and
permeation enhancement of anticancer drug. Carbohydr Polym.
203:10–18. 2019.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Guo Y, Liu S, Luo F, Tang D, Yang T, Yang
X and Xie Y: A nanosized codelivery system based on intracellular
stimuli-triggered dual-drug release for multilevel chemotherapy
amplification in drug-resistant breast cancer. Pharmaceutics.
14(422)2022.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Yu J, Chen H, Jiang L and Wang J, Dai J
and Wang J: Codelivery of adriamycin and P-gp inhibitor quercetin
using PEGylated liposomes to overcome cancer drug resistance. J
Pharm Sci. 108:1788–1799. 2019.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Wang X, Chen Y, Dahmani FZ, Yin L, Zhou J
and Yao J: Amphiphilic carboxymethyl chitosan-quercetin conjugate
with P-gp inhibitory properties for oral delivery of paclitaxel.
Biomaterials. 35:7654–7665. 2014.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Khonkarn R, Daowtak K and Okonogi S:
Chemotherapeutic efficacy enhancement in P-gp-overexpressing cancer
cells by flavonoid-loaded polymeric micelles. AAPS PharmSciTech.
21(121)2020.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Mu Y, Wu G, Su C, Dong Y, Zhang K, Li J,
Sun X, Li Y, Chen X and Feng C: pH-sensitive amphiphilic
chitosan-quercetin conjugate for intracellular delivery of
doxorubicin enhancement. Carbohydr Polym.
223(115072)2019.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Kumar M, Sharma G, Misra C, Kumar R, Singh
B, Katare OP and Raza K: N-desmethyl tamoxifen and quercetin-loaded
multiwalled CNTs: A synergistic approach to overcome MDR in cancer
cells. Mater Sci Eng C Mater Biol Appl. 89:274–282. 2018.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Qian J, Liu S, Yang T, Xiao Y, Sun J, Zhao
J, Zhang Z and Xie Y: Polyethyleneimine-tocopherol hydrogen
succinate/hyaluronic acid-quercetin (PEI-TOS/HA-QU) core-shell
micelles delivering paclitaxel for combinatorial treatment of MDR
breast cancer. J Biomed Nanotechnol. 17:382–398. 2021.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Dallavalle S, Dobričić V, Lazzarato L,
Gazzano E, Machuqueiro M, Pajeva I, Tsakovska I, Zidar N and
Fruttero R: Improvement of conventional anti-cancer drugs as new
tools against multidrug resistant tumors. Drug Resist Updat.
50(100682)2020.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Deshmukh R, Prajapati M and Harwansh RK:
Management of colorectal cancer using nanocarriers-based drug
delivery for herbal bioactives: Current and emerging approaches.
Curr Pharm Biotechnol. 25:599–622. 2024.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Kenchegowda M, Rahamathulla M, Hani U,
Begum MY, Guruswamy S, Osmani RAM, Gowrav MP, Alshehri S, Ghoneim
MM, Alshlowi A and Gowda DV: Smart nanocarriers as an emerging
platform for cancer therapy: A review. Molecules.
27(146)2021.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Tang L, Li J, Zhao Q, Pan T, Zhong H and
Wang W: Advanced and innovative nano-systems for anticancer
targeted drug delivery. Pharmaceutics. 13(1151)2021.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Kumar V, Rahman M, Gahtori P, Al-Abbasi F,
Anwar F and Kim HS: Current status and future directions of
hepatocellular carcinoma-targeted nanoparticles and nanomedicine.
Expert Opin Drug Deliv. 18:673–694. 2021.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Mishra AK, Pandey M, Dewangan HK, Sl N and
Sahoo PK: A comprehensive review on liver targeting: Emphasis on
nanotechnology-based molecular targets and receptors mediated
approaches. Curr Drug Targets. 23:1381–1405. 2022.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Dutta R and Mahato RI: Recent advances in
hepatocellular carcinoma therapy. Pharmacol Ther. 173:106–117.
2017.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Aghababaei F and Hadidi M: Recent advances
in potential health benefits of quercetin. Pharmaceuticals (Basel).
16(1020)2023.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Manzoor MF, Hussain A, Sameen A, Sahar A,
Khan S, Siddique R, Aadil RM and Xu B: Novel extraction, rapid
assessment and bioavailability improvement of quercetin: A review.
Ultrason Sonochem. 78(105686)2021.PubMed/NCBI View Article : Google Scholar
|