Introduction
Chronic rhinosinusitis (CRS) is a multifactorial
condition characterized by persistent inflammation of the sinonasal
mucosa, affecting -16% of the global population (1,2).
Symptoms such as nasal congestion, increased nasal discharge,
facial pain or pressure, and olfactory dysfunction persist for
>12 weeks, significantly impairing quality of life and
contributing to psychological distress (3). The high prevalence and recurrent
nature of CRS poses a substantial healthcare burden.
Sinonasal computed tomography (CT) is the most
commonly used imaging modality in CRS diagnosis and management
(4-6);
it provides detailed anatomical visualization, aiding in disease
assessment, surgical planning and postoperative evaluation
(7,8). The technique helps assess the presence
of fluid, mucosal thickening, bone fractures, osteitis and
sinonasal anatomical variations (9-11).
For example, CT imaging can highlight surgical indications, such as
severe osteomeatal complex (OMC) obstruction or extensive
soft-tissue disease within the sinuses. By combining CT-derived
Lund-Mackay (LM) scores (12,13)
with symptom scores, clinicians can tailor treatment plans to
individual patient's needs (14,15).
Furthermore, CT serves as an essential tool for postoperative
evaluation, enabling direct comparison of preoperative and
postoperative LM scores to assess the effectiveness of surgical
interventions in resolving sinonasal pathology (16-18).
While numerous studies have explored the association between CT
scoring at a single time point and treatment outcomes (19,20),
limited research has focused on longitudinal imaging changes in
CRS, particularly in untreated patients. The natural progression of
the disease over time remains inadequately explored. Therefore,
analyzing the temporal trends of CRS using CT scoring is of
considerable significance. Such an analysis not only reflects the
dynamic characteristics of the disease but also provides insights
into potential factors influencing disease progression or
resolution, such as advancements in medical technology, changes in
environmental factors, or shifts in the healthcare-seeking
behaviors of patients.
Building on this context, the present study compared
CT imaging data of patients with CRS from 2017 and 2023, using the
LM scoring system to assess changes in disease severity. Given
ongoing changes in diagnostic strategies, clinical management and
public health awareness, such a comparison may provide insight into
how CRS presentations may have shifted in recent years. These
findings offer valuable data to inform the future of precision
medicine and personalized management strategies for CRS.
Materials and methods
Study design and population
The present study employed a retrospective analysis
conducted at The Department of Otorhinolaryngology of The Second
Hospital of Shanxi Medical University (Taiyuan, China), involving
120 patients diagnosed with CRS in 2017 and 2023. The 2017 group
included 60 patients (41 males and 19 females; median age, 31
years; range, 9-64 years), and the 2023 group included 60 patients
(35 males and 25 females; median age, 24 years; range, 7-50 years).
The present study was approved by The Institutional Review Board of
the Second Hospital of Shanxi Medical University (approval no.
2025.YX059) and conducted in full compliance with the Declaration
of Helsinki and institutional ethical guidelines. All clinical and
imaging data were retrospectively obtained from routine care and
fully anonymized prior to analysis. Given the retrospective design
and use of de-identified data, the requirement for informed consent
was waived by the ethics committee. All patients met the diagnostic
criteria for CRS with nasal polyps as defined in The European
Position Paper on Rhinosinusitis and Nasal Polyps 2020(4). Each patient underwent standardized CT
scans and completed LM score evaluations.
The inclusion criteria required participants to have
a confirmed CRS diagnosis (with or without nasal polyps) in 2017 or
2023 and to have undergone both standardized CT imaging and symptom
scoring. Exclusion criteria were established to ensure data
reliability and minimize confounding factors, and were as follows:
i) Severe systemic diseases (such as uncontrolled diabetes,
autoimmune disorders or malignancies) that could influence CRS
severity or treatment response; ii) history of sinus-related
surgery, as prior surgical intervention could alter sinonasal
anatomy and inflammation, confounding comparisons between the two
time points; and iii) incomplete data or poor-quality CT images,
which could compromise the accuracy of the LM scoring and limit the
validity of the findings. To mitigate potential selection bias,
patient recruitment was based solely on predefined inclusion and
exclusion criteria, without influence from disease severity or
treatment history. Additionally, the two study groups (2017 and
2023) were matched for age and sex distribution to enhance
comparability.
The study population was divided into two groups: i)
The 2017 group, consisting of 60 patients diagnosed with CRS (with
or without nasal polyps) who completed CT scans and ii) the 2023
group, consisting of 60 patients meeting identical diagnostic
criteria. For both groups, demographic data and disease history
were recorded. Importantly, neither group received major
therapeutic interventions before or during the study period,
ensuring comparable disease status for robust analysis.
CT imaging evaluation
All patients underwent preoperative CT scans using a
64-slice multislice scanner (GE Healthcare). The scanning
parameters were as follows: Slice thickness of 0.6-1.0 mm, 120 kV
and 80-160 mAs. Sagittal and coronal reconstructions were obtained
for each scan. CT findings were evaluated and staged according to
the LM scoring system (12,13) by two experienced radiologists, with
the final score representing the average of the independent
assessments to minimize subjective bias.
The LM staging system assigns a score of 0 for no
opacification, 1 for partial opacification and 2 for complete
opacification of each sinus (maxillary, anterior ethmoid, posterior
ethmoid, sphenoid and frontal). For the OMC region, the score is
either 0 (not occluded) or 2 (occluded). The total score ranges
from 0 (no abnormalities) to 24 (complete opacification of all
sinuses and OMC). The total LM score (maximum of 24) represents the
sum of scores from both sides, with each of the five sinuses scored
from 0 to 2, and the OMC scored as 0 or 2 per side.
Statistical analysis
Statistical analyses were performed using IBM SPSS
Statistics for Windows, version 23.0 (IBM Corp.). Continuous
variables, such as age, are expressed as the mean ± standard
deviation (SD) and were compared between the 2017 and 2023 groups
using unpaired (independent samples) t-test. Sex distribution was
analyzed using the χ2 test. LM scores, which did not
follow a normal distribution, were compared using the Mann-Whitney
U test. All statistical tests were two-tailed, with P<0.05
considered to indicate a statistically significant difference.
Results
Participants and CRS clinical
features
A total of 294 patients diagnosed with CRS were
initially considered for inclusion in the present study. After
excluding 174 patients due to incomplete data or presentations
unrelated to nasal symptoms, the final analysis included 120
participants (n=60, 2017; n=60, 2023). The mean age of the 2017
cohort was 31 years (SD, 15 years; range, 9-64 years), with 31.7%
women and 68.3% men. The 2023 cohort had a mean age of 24 years
(SD, 10 years; range: 7-50 years), with 41.6% women and 58.4% man.
Table I provides a detailed summary
of the demographic and clinical characteristics of the study
participants.
 | Table ISubjects' characteristics. |
Table I
Subjects' characteristics.
| Characteristic | 2017 | 2023 |
|---|
| Mean age (SD),
years | 31(15) | 24(10) |
| Female sex, n/total n
(%) | 19/60 (31.7) | 25/60 (41.6) |
| LM score, n left/n
right | | |
|
Osteomeatal
complex | | |
|
0 | 17/22 | 39/39 |
|
1 | 0/0 | 0 |
|
2 | 43/38 | 21/21 |
|
Frontal
sinus | | |
|
0 | 11/19 | 36/32 |
|
1 | 25/18 | 18/19 |
|
2 | 24/23 | 6/9 |
|
Sphenoid
sinus | | |
|
0 | 14/14 | 31/24 |
|
1 | 36/35 | 23/30 |
|
2 | 10/11 | 6/6 |
|
Anterior
ethmoid sinus | | |
|
0 | 2/9 | 3/0 |
|
1 | 25/21 | 43/46 |
|
2 | 33/30 | 14/14 |
|
Posterior
ethmoid sinus | | |
|
0 | 8/8 | 14/17 |
|
1 | 24/33 | 40/36 |
|
2 | 28/19 | 6/7 |
|
Maxillary
sinus | | |
|
0 | 4/3 | 6/5 |
|
1 | 28/32 | 42/40 |
|
2 | 28/25 | 12/15 |
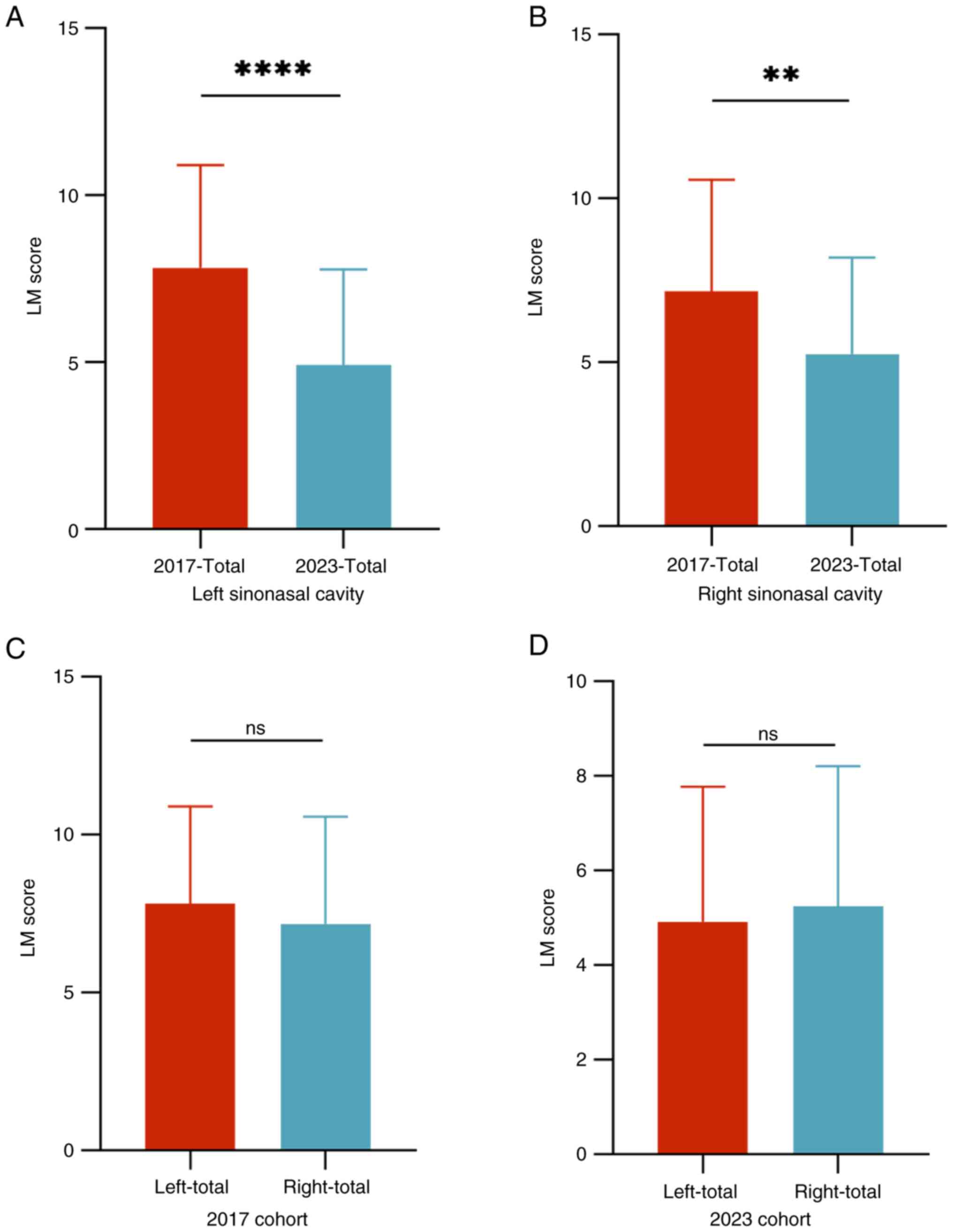
Changes in sinonasal LM scores
The LM scores were analyzed to evaluate changes in
disease severity as assessed by CT imaging among patients with CRS
between 2017 and 2023. The findings revealed a significant
reduction in total LM scores in 2023 compared with those in 2017,
as shown in Fig. 1A for the left
sinonasal cavity and Fig. 1B for
the right side. Both left and right sinonasal scores demonstrated a
decreasing trend, with the left-sided scores showing a slightly
more pronounced reduction. However, the differences between left
and right sinonasal LM scores were assessed separately for the 2017
and 2023 cohorts. No statistically significant differences were
found between sides in either group. These results are shown in
Fig. 1C for the 2017 cohort and
Fig. 1D for the 2023 cohort. These
results indicated a general decline in the radiological severity of
CRS over the 5-year period.
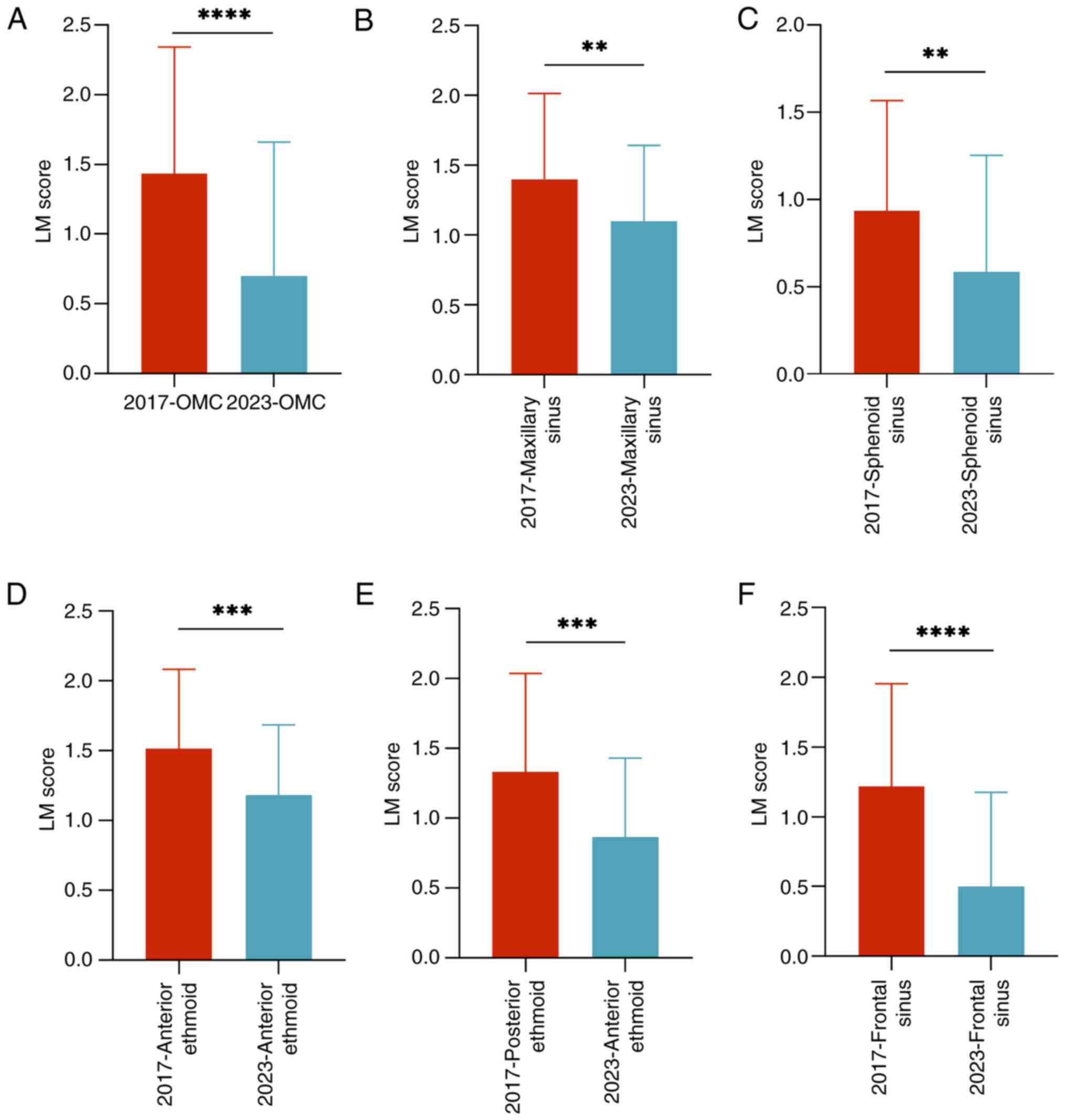
Left-sided OMC and individual sinus
scores
The analysis of the left-sided OMC and individual
sinuses, including the frontal, ethmoid, sphenoid and maxillary
sinuses, revealed significant reductions in CT scores over time
(Fig. 2). Both the OMC and frontal
sinus demonstrated the most substantial improvements, with marked
reductions in CT scores compared with those in 2017 (Fig. 2A and F). Similarly, the ethmoid sinus,
encompassing both the anterior and posterior regions, exhibited a
consistent downward trend with significant score decreases in 2023
compared with those in 2017 (Fig.
2D and E). The sphenoid and
maxillary sinuses exhibited significant reduction but these were
less pronounced, potentially due to their unique anatomical and
pathological features (Fig. 2B and
C). These results highlighted a
notable decrease in inflammation in the left frontal sinus and OMC,
reflecting considerable improvements in these regions over the
5-year period.
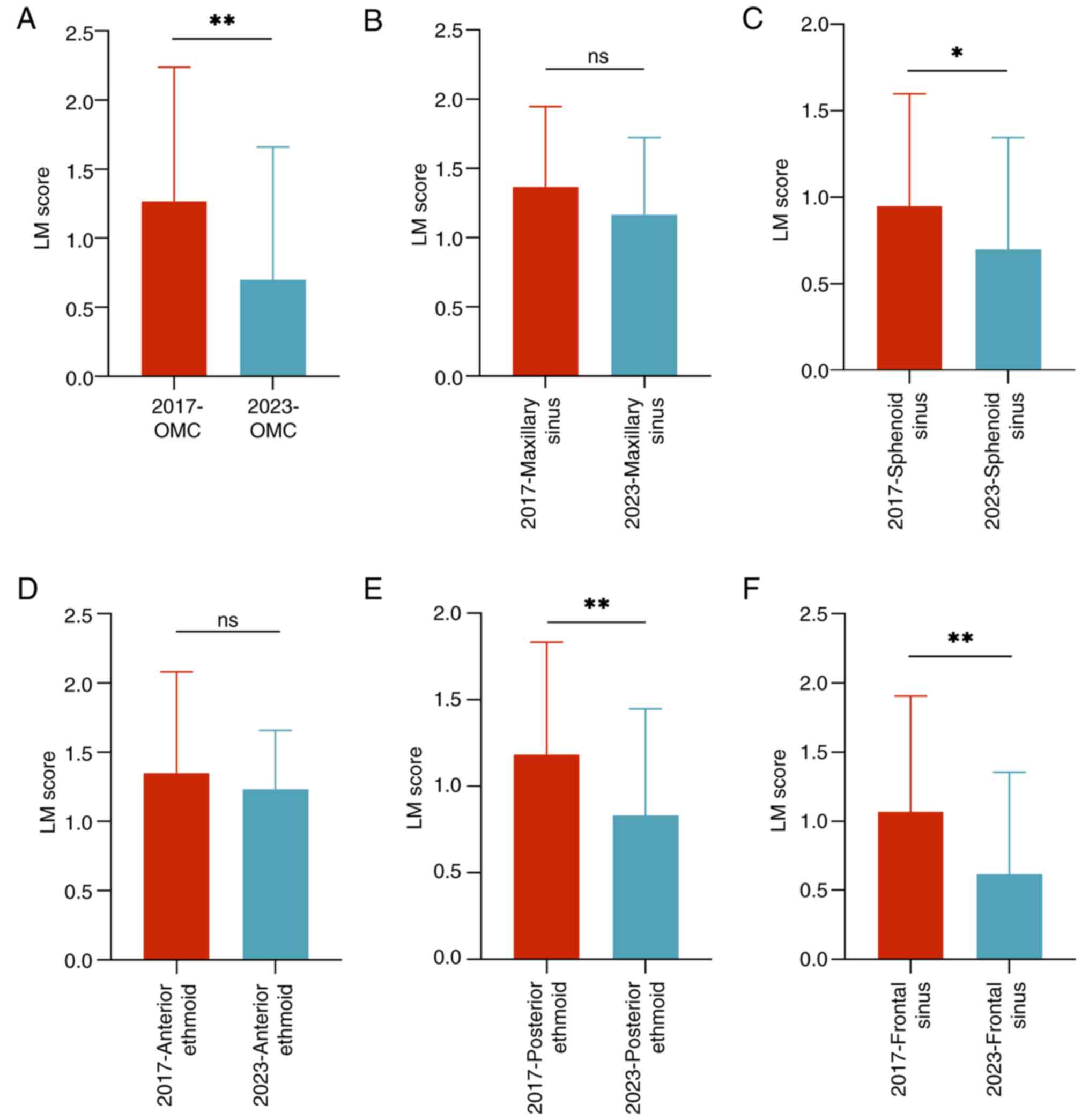
Right-sided OMC and individual sinus
scores
Analysis of the right-sided OMC and individual
sinuses (Fig. 3) revealed trends
similar, but not identical, to those observed on the left side.
Significant reductions in CT scores were noted in the right OMC,
sphenoid sinus, posterior ethmoid sinus and frontal sinus, with
statistically significant improvements in these areas between 2017
and 2023 (Fig. 3A, C, E and
F). By contrast, the reductions in
the maxillary sinus and anterior ethmoid sinus scores were less
pronounced and did not reach statistical significance (Fig. 3B and D). These results suggested asymmetrical
changes between the two sides, with more substantial improvements
observed in the right OMC and frontal sinus. Overall, the present
study highlighted a notable reduction in sinonasal inflammation
severity over the 5-year period, with the most significant
improvements in the left-sided OMC and frontal sinus, while the
maxillary and sphenoid sinuses exhibited relatively smaller
changes.
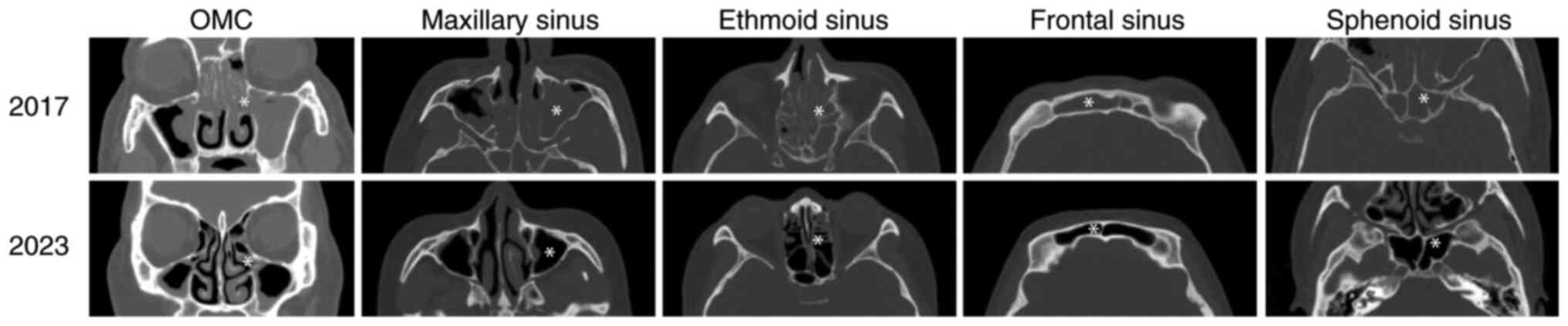
Changes in OMC and individual sinus CT
features
A comparative analysis of representative CT images
from 2017 and 2023 revealed significant differences in sinonasal
inflammation features (Fig. 4A-F).
Patients from 2023 exhibited notably less mucosal thickening, with
some sinuses showing no obvious signs of inflammation.
Additionally, submucosal bone thickening attributed to osteitis was
markedly reduced, reflecting a decrease in chronic inflammatory
remodeling and an overall improvement in sinonasal CT features over
the 5-year period. The ethmoid and frontal sinuses demonstrated the
most notable improvements, characterized by thinner mucosal layers
and increased aeration of the sinus cavities, indicating improved
ventilation and drainage. Importantly, no significant increase in
anatomical variations was observed in patients with normal sinus
development during this period.
Patterns of mucosal thickening also differed between
the two cohorts. In the 2017 group, CRS predominantly manifested as
diffuse mucosal thickening involving the OMC and other sinuses,
with frequent fluid accumulations and obstructions caused by
soft-tissue density lesions, such as polyps. CT features included
localized bone sclerosis and hypertrophy. By contrast, the 2023
group more frequently exhibited mild or localized mucosal
thickening with reduced fluid accumulation and fewer radiological
signs suggestive of chronic osteitis. These findings were based on
qualitative assessments of CT images by radiological review and are
presented descriptively in the text. A shift toward milder
radiological presentations of CRS was observed in the 2023 cohort,
as evidenced by improved aeration, reduced mucosal and submucosal
thickening, and decreased chronic remodeling.
Discussion
CT provides a comprehensive view of sinonasal
anatomy, inflammation and anatomical variations, thus offering
valuable insights into disease classification and staging (21). The present study explored temporal
changes in the clinical presentation of CRS by comparing CT
findings from two cohorts diagnosed in 2017 and 2023. Unlike
longitudinal studies that track disease progression in individuals
(7,10,13),
the present cross-sectional analysis focuses on disease severity at
the time of diagnosis, offering a unique perspective on broader
shifts in CRS awareness, diagnostic strategies and clinical
management.
Over the past 5 years, a notable reduction in the
severity of CRS, particularly in the OMC and frontal sinuses, was
observed. This trend likely reflects earlier disease identification
and intervention, influenced by improved public awareness,
advancements in imaging technology and clinical practices. The
observed reduction in LM scores, particularly in regions critical
for sinus ventilation and drainage, supports the hypothesis that
early intervention and personalized treatment approaches contribute
to improved disease control. These findings indicate a paradigm
shift in CRS management, with the disease increasingly being
addressed at milder stages, thereby reducing the risk of advanced
complications. This observation aligns with the study by Wang et
al (22), which noted a similar
trend toward less severe CRS when analyzing clinical and
pathological characteristics over an 11-year period.
This inter-sinus asymmetry in disease severity may
stem from several factors, including anatomical variations such as
middle turbinate pneumatization, nasal septum deviation and
variations in frontal sinus drainage pathway attachment points
(23-25),
which have been associated with CRS development. The distribution
and frequency of these variations may be influenced by genetic and
environmental factors. Such anatomical differences could
potentially alter sinus ventilation and drainage, contributing to
the observed laterality in LM scores (26,27)
such as differences in sinus drainage pathways or ventilation,
which could influence disease severity. Physiological factors
(28,29), such as regional immune responses or
airflow dynamics, may also contribute to the observed variability
in inflammation patterns. Understanding these asymmetries is
crucial for developing targeted treatment strategies that address
the unique sinus involvement of each patient.
Qualitative analysis revealed improvements in
imaging features, including reductions in mucosal thickening,
submucosal bony changes and improved sinus aeration. These findings
suggest a shift towards milder CRS phenotypes at the time of
diagnosis, likely reflecting earlier and more effective
interventions. The reduced incidence of chronic inflammatory
remodeling (30,31), such as osteitis (32) or fibrosis (33), further supports this trend. Notably,
the absence of marked changes in sinonasal anatomical variations
indicates that these improvements are more likely due to
advancements in clinical care rather than inherent patient
characteristics. Understanding these imaging trends underscores the
impact of evolving diagnostic and therapeutic strategies on CRS
management.
The present study highlights several key areas where
clinical practice can be adapted to improve the management of CRS.
First, the significant reduction in CRS severity over time,
particularly in the OMC and frontal sinuses, suggests that earlier
detection of symptoms is crucial. Clinicians should consider
incorporating routine CT evaluations for patients with early
sinonasal complaints to identify and intervene in milder stages of
the disease before it progresses to more severe complications.
Second, the observed asymmetry in CT scores indicates that CRS may
present differently on each side of the sinonasal cavity. The
finding supports a personalized approach where treatment plans are
tailored not only to severity but also to the specific regions
affected. For example, targeted therapies, such as localized
topical treatments or refined surgical approaches, may be
beneficial for patients with predominant disease in one sinus
region. Third, given the evolving landscape of diagnostic tools,
the integration of advanced imaging techniques along with biomarker
assessments can further refine disease stratification. This would
allow clinicians to more accurately predict disease trajectory and
optimize treatment strategies, moving towards precision medicine in
CRS care. Fourth, increasing public awareness of CRS symptoms and
the benefits of early treatment is essential. Clinicians should
also be updated on the latest imaging techniques and treatment
protocols to ensure that improvements in diagnostic and therapeutic
strategies translate into improved patient outcomes. Fifth, as
regional variability in CRS persists, continuous monitoring of CT
findings and patient responses should inform treatment
modifications. Prospective studies integrating molecular profiling
and environmental assessments could further enhance understanding,
enabling clinicians to refine treatment algorithms over time.
The retrospective cross-sectional design of the
current study presented inherent limitations, particularly in
establishing causal relationships or evaluating the long-term
effects of specific therapies. Additionally, reliance on CT
scoring, while robust, may not entirely capture the complex and
dynamic inflammatory processes underlying CRS. The selection of
only two timepoints (2017 and 2023) provides a snapshot of changes
in CRS severity but does not account for potential year-to-year
variability between 2018 and 2022. While these time points were
chosen due to data availability and noticeable shifts in clinical
practice, future studies incorporating annual or more frequent data
points would help establish a clearer trajectory of change. The
sample size and limited diversity of the cohort also constrained
the generalizability of the findings, underscoring the need for
broader patient populations in future analyses. Moving forward,
prospective longitudinal studies incorporating advanced imaging
techniques, molecular profiling and environmental assessments are
essential to achieve a more comprehensive understanding of CRS
progression and to refine management strategies.
In conclusion, the present study revealed a
significant reduction in the severity of CRS at diagnosis over a
5-year period with the most pronounced improvements observed in the
OMC and frontal sinuses. These trends reflect advancements in
disease awareness, early diagnostic strategies and management
practices. However, the observed changes were not uniform across
all sinuses or between the left and right sides, emphasizing the
asymmetry in disease progression and resolution. These findings
highlight the necessity of further research into the distinct
characteristics and underlying mechanisms influencing each sinus
region. Additionally, they underscore the critical need for
continued efforts to refine diagnostic tools, develop enhanced
therapeutic options and promote public education. By addressing the
unique clinical features of CRS in individual patients, healthcare
providers can optimize treatment outcomes and significantly reduce
the overall disease burden.
Acknowledgements
The authors express their gratitude to Mr. Tao
Zhang, radiological technologist at the Second Hospital of Shanxi
Medical University (Shanxi, China), for their skilled technical
support in acquiring and processing the imaging data, which was
crucial for the present study. The authors also wish to thank
Professor Ningning Li from the Seventh Affiliated Hospital of Sun
Yat-sen University (Shenzhen, China) for academic guidance on study
design and manuscript revision.
Funding
Funding: The present study was supported in part by The Sanming
Project of Medicine in Shenzhen (grant no. SZSM202111005), The
Shenzhen Science and Technology Program (grant no.
JCYJ20240813150209013) and The Sun Yat-sen University Higher
Education Teaching Research and Reform Project (grant no. 2021
A1032 1030).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
YG conceptualized the study. JW and SX performed the
study methodology and data curation. JW wrote and prepared the
original draft. JW, SX and YF were responsible for software
application, and performed study visualization and investigation.
JW, SX, YF and YG wrote, reviewed and edited the manuscript. YG
acquired the funding. JW and YG confirm the authenticity of all the
raw data. All authors read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Given the retrospective nature of the present study,
the requirement for informed consent was waived by the
institutional review board. The present study was approved by The
Institutional Review Board of the Second Hospital of Shanxi Medical
University (Taiyuan, China; approval no. 2025.YX059) and conducted
in full compliance with the Declaration of Helsinki and
institutional ethical guidelines.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liu Z, Chen J, Cheng L, Li H, Liu S, Lou
H, Shi J, Sun Y, Wang D, Wang C, et al: Chinese society of allergy
and Chinese society of otorhinolaryngology-head and neck surgery
guideline for chronic rhinosinusitis. Allergy Asthma Immunol Res.
12:176–237. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Shi JB, Fu QL, Zhang H, Cheng L, Wang YJ,
Zhu DD, Lv W, Liu SX, Li PZ, Ou CQ and Xu G: Epidemiology of
chronic rhinosinusitis: Results from a cross-sectional survey in
seven Chinese cities. Allergy. 70:533–539. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hamilos DL: Chronic rhinosinusitis:
Epidemiology and medical management. J Allergy Clin Immunol.
128:693–707; quiz 708-709. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fokkens WJ, Lund VJ, Hopkins C, Hellings
PW, Kern R, Reitsma S, Toppila-Salmi S, Bernal-Sprekelsen M, Mullol
J, Alobid I, et al: European position paper on rhinosinusitis and
nasal polyps 2020. Rhinology. 58 (Suppl 29):S1–S464.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hirsch AG, Nordberg C, Bandeen-Roche K,
Tan BK, Schleimer RP, Kern RC, Sundaresan A, Pinto JM, Kennedy TL,
Greene JS, et al: Radiologic sinus inflammation and symptoms of
chronic rhinosinusitis in a population-based sample. Allergy.
75:911–920. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Orlandi RR, Kingdom TT, Smith TL, Bleier
B, DeConde A, Luong AU, Poetker DM, Soler Z, Welch KC, Wise SK, et
al: International consensus statement on allergy and rhinology:
Rhinosinusitis 2021. Int Forum Allergy Rhinol. 11:213–739.
2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Brescia G, Contro G, Ruaro A, Frigo AC,
Barion U and Marioni G: Preoperative sinonasal computed tomography
score in chronic rhinosinusitis with nasal polyps. Tomography.
8:77–88. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hua HL, Li S, Xu Y, Chen SM, Kong YG, Yang
R, Deng YQ and Tao ZZ: Differentiation of eosinophilic and
non-eosinophilic chronic rhinosinusitis on preoperative computed
tomography using deep learning. Clin Otolaryngol. 48:330–338.
2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gufran K, Alsakr AM, Alqahtani AS,
Alqhtani NR, Alasmari D, Alzamil FF, Alotaibi NM, Alhamid HM and
Aldafiri AS: Association between periodontitis and chronic
rhinosinusitis involving maxillary sinus measured by lund mackay
staging system. Healthcare (Basel). 10(1961)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Huang BY, Senior BA and Castillo M:
Current trends in sinonasal imaging. Neuroimaging Clin N Am.
25:507–525. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sedaghat AR and Bhattacharyya N: Chronic
rhinosinusitis symptoms and computed tomography staging: Improved
correlation by incorporating radiographic density. Int Forum
Allergy Rhinol. 2:386–391. 2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lund VJ and Mackay IS: Staging in
rhinosinusitus. Rhinology. 31:183–184. 1993.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Subspecialty Group of Rhinology, Editorial
Board of Chinese Journal of Otorhinolaryngology Head and Neck
Surgery; Subspecialty Group of Rhinology, Society of
Otorhinolaryngology Head and Neck Surgery, Chinese Medical
Association. Chinese guidelines for diagnosis and treatment of
chronic rhinosinusitis (2018). Zhonghua Er Bi Yan Hou Tou Jing Wai
Ke Za Zhi. 54:81–100. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
14
|
Marino MJ, Riley CA, Patel AS, Pou JD,
Kessler RH and McCoul ED: Paranasal sinus
opacification-to-pneumatization ratio applied as a rapid and
validated clinician assessment. Int Forum Allergy Rhinol. 7:24–29.
2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Roland LT, Marcus S, Schertzer JS, Wise
SK, Levy JM and DelGaudio JM: Computed tomography findings can help
identify different chronic rhinosinusitis with nasal polyp
phenotypes. Am J Rhinol Allergy. 34:679–685. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kuo CJ, Liao YS, Barman J and Liu SC:
Semi-supervised deep learning semantic segmentation for 3D
volumetric computed tomographic scoring of chronic rhinosinusitis:
Clinical correlations and comparison with lund-mackay scoring.
Tomography. 8:718–729. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Li C, Zhang B, Yan M, Li Y, Chen J, Nie Z,
Guo Y, Shi J and Chen F: Cluster analysis of patients with chronic
rhinosinusitis and asthma after endoscopic sinus surgery. Ann
Allergy Asthma Immunol. 130:325–332 e7. 2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Samargandy S, Grose E, Yip J and Lee JM:
Endoscopic sinus surgery outcomes in patients with chronic
rhinosinusitis and immunoglobulin deficiencies. J Otolaryngol Head
Neck Surg. 52(43)2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Arancibia C, Langdon C, Mullol J and
Alobid I: Twelve-year long-term postoperative outcomes in patients
with chronic rhinosinusitis with nasal polyps. Rhinology.
60:261–269. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Gata A, Raduly L, Budisan L, Ursu TM,
Chira C, Dioșan L, Berindan-Neagoe I and Albu S: Machine learning
model predicts postoperative outcomes in chronic rhinosinusitis
with nasal polyps. Clin Otolaryngol. 49:776–784. 2024.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wu AW, Borrelli M, Raskin J, Hopp ML,
Mirocha J and Tang DM: Correlation of chronic
rhinosinusitis-related symptoms with computed tomography subsite.
Int Forum Allergy Rhinol. 12:791–794. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wang W, Gao Y, Zhu Z, Zha Y, Wang X, Qi F,
Zhou L, Pang J, Gao Z and Lv W: Changes in the clinical and
histological characteristics of Chinese chronic rhinosinusitis with
nasal polyps over 11 years. Int Forum Allergy Rhinol. 9:149–157.
2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cho JH, Park MS, Chung YS, Hong SC, Kwon
KH and Kim JK: Do anatomic variations of the middle turbinate have
an effect on nasal septal deviation or paranasal sinusitis? Ann
Otol Rhinol Laryngol. 120:569–574. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Alsowey AM, Abdulmonaem G, Elsammak A and
Fouad Y: Diagnostic performance of multidetector computed
tomography (MDCT) in diagnosis of sinus variations. Pol J Radiol.
82:713–725. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Eviatar E, Golan Y and Gavriel H:
Fronto-septal rostrum: Prevalence, classification and clinical
implications. J Laryngol Otol. 132:423–428. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wu J, Jain R and Douglas R: Effect of
paranasal anatomical variants on outcomes in patients with limited
and diffuse chronic rhinosinusitis. Auris Nasus Larynx. 44:417–421.
2017.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zhou F, Cao C, Fan W, Tan L, Liu P, Lv H
and Xu Y: The imaging anatomy of ethmomaxillary sinus and its
impact on chronic rhinosinusitis. Eur Arch Otorhinolaryngol.
278:719–726. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Choi A, Xu S, Luong AU and Wise SK:
Current review of comorbidities in chronic rhinosinusitis. Curr
Allergy Asthma Rep. 25(4)2024.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lin L, Lan J, Dai F, Wei J and Chen Z:
Effect of local corticosteroid administration on CD8+CD25+Foxp3+
tregs in neutrophilic CRSwNP. ORL J Otorhinolaryngol Relat Spec.
84:396–405. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Huang ZQ, Liu J, Sun LY, Ong HH, Ye J, Xu
Y and Wang DY: Updated epithelial barrier dysfunction in chronic
rhinosinusitis: Targeting pathophysiology and treatment response of
tight junctions. Allergy. 79:1146–1165. 2024.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Wang X, Sima Y, Zhao Y, Zhang N, Zheng M,
Du K, Wang M, Wang Y, Hao Y, Li Y, et al: Endotypes of chronic
rhinosinusitis based on inflammatory and remodeling factors. J
Allergy Clin Immunol. 151:458–468. 2023.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Snidvongs K, Sacks R and Harvey RJ:
Osteitis in chronic rhinosinusitis. Curr Allergy Asthma Rep.
19(24)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Schwartz BS, Al-Sayouri SA, Pollak JS,
Hirsch AG, Kern R, Tan B, Kato A, Schleimer RP and Peters AT:
Strong and consistent associations of precedent chronic
rhinosinusitis with risk of non-cystic fibrosis bronchiectasis. J
Allergy Clin Immunol. 150:701–708.e4. 2022.PubMed/NCBI View Article : Google Scholar
|