Introduction
Stroke remains one of the leading causes of death
and long-term disability worldwide, with large vessel occlusion
(LVO) representing one of the most severe subtypes due to the
extensive brain regions affected (1). Mechanical thrombectomy (MT) has
transformed the management of acute ischemic stroke by enabling
rapid reperfusion and significant functional recovery in patients
with LVO (2,3). Current guidelines recommend MT based
on several criteria: The location of occlusion (typically proximal
anterior circulation, such as the internal carotid artery or middle
cerebral artery), the time from stroke onset (within 6-24 h), and
acceptable infarct burden commonly assessed by an Alberta Stroke
Program Early CT Score [ASPECTS]≥6 or infarct volume <50 ml)
(4).
MT involves the physical removal of a thrombus using
stent retrievers or aspiration devices to restore cerebral
perfusion (5). Although MT has been
major advance in stroke therapy, clinical outcomes vary, and not
all patients benefit equally from the procedure (6). Vascular risk factors such as
hypertension, diabetes, hyperlipidemia and smoking are
well-established contributors to cerebrovascular pathology and may
influence the efficacy and safety of thrombectomy procedures
(7). The present study aims to
evaluate the impact of these pre-existing vascular conditions on
clinical outcomes following MT in patients with LVO, thereby
contributing to more personalized and effective treatment
strategies. However, functional outcomes following MT vary
significantly and are influenced by pretreatment factors such as
age and comorbidities (8,9). Numerous pre- and intra-procedural
variables have been identified as predictors of clinical outcomes
(10).
Although vascular risk factors such as hypertension
and diabetes mellitus are widely recognized to influence MT
outcomes, their independent prognostic roles remain debated. For
instance, the role of diabetes mellitus in predicting poorer
recanalization success is controversial, with conflicting evidence
in the literature (11). Moreover,
the impact of glycemic variability-beyond absolute
hyperglycemia-remains underexplored. Existing thresholds for
glycemic control (for example, <180 mg/dl.) are derived from
heterogeneous clinical protocols, further complicating
standardization (11). These
ongoing controversies emphasize the need for improved risk
stratification and standardized peri-procedural management
strategies.
Factor such as hyperglycemia, advanced age, higher
baseline NIHSS score, and failed recanalization increase the risk
of unfavorable outcomes at 90 days in patients with acute ischemic
stroke treated with MT (12). In
addition to preventing complications, optimizing of blood pressure,
glucose levels and hemoglobin concentrations represent potentially
modifiable factors that merit further investigation (9).
Post-stroke seizures are another frequent
complication and are associated with poorer functional outcomes. A
systematic review in 2022 reported that 5.8% of patients with
stroke undergoing MT developed seizures. However, the relationship
between MT and post-stroke seizures remains inconclusive, and the
mechanisms linking LVO-related stroke and seizure activity are not
yet fully understood (13), Saver
et al (14) were the first
to confirm the significant benefit of MT in patients with LVO,
providing the foundational evidence for current clinical
guidelines.
Regarding glycemic management during MT, recent
studies have clarified the clinical relevance of maintaining
intraoperative glucose levels below 180 mg/dl. For example, the
study by Janelidze et al (15) demonstrated improved outcomes with
strict glycemic control, highlighting the importance of real-time
glucose monitoring during MT to enhance prognosis.
The present study aims to investigate the impact of
vascular risk factors on the clinical outcomes of MT in patients
with stroke with LVO. Additionally, it seeks to determine the
prevalence of structural epilepsy in this population, a
complication that can profoundly affect quality of life and
long-term prognosis. By examining this prevalence, the study aims
to contribute to more comprehensive post-stroke management
strategies, addressing both acute intervention, and long-term
complication. Understanding and managing modifiable vascular risk
factors will be critical for optimizing MT outcomes and improving
patient care.
Patients and methods
Study design
The present study utilizes a retrospective cohort
design, focusing on patients who experienced ischemic stroke due to
LVO and subsequently underwent endovascular MT.
Study duration and setting
The study was conducted at a single tertiary care
center and included medical records reviewed from 2018 to 2023.
Data collection began in June 2023 and was completed in December
2023.
Participants
A total of 56 patients (25 women and 31 men) with
stroke aged between 20 and 80 years, who underwent MT for LVO
during the study period, were included. Patients were identified
through hospital medical records. Only those who received MT were
eligible; patients who did not undergo the procedure were
excluded.
Diagnosis
Post-stroke epilepsy was diagnosed based on the
International League Against Epilepsy criteria, requiring at least
one unprovoked seizure occurring >24 h after stroke onset, with
corroborative electroencephalogram (EEG) or clinical
documentation.
Data collection method
Data were collected retrospectively by electronic
medical records. The variables gathered included demographic
details, vascular comorbidities (for example, hypertension,
diabetes), clinical outcomes post-MT, and the incidence of
post-stroke (structural) epilepsy.
Outcome assessment
The primary clinical outcome was assessed using the
Modified Thrombolysis in Cerebral Infarction (mTICI) scoring
system, which measures the degree of reperfusion post-MT.
Sample size justification
A sample size of 56 patients was determined based on
the available eligible cases during the study period. While
relatively small, this sample was deemed sufficient to provide
preliminary insights into the relationship between vascular risk
factors and MT outcomes, as well as to estimate the prevalence of
post-stroke epilepsy in this population.
Data analysis
Statistical analysis was performed using Stata BE 18
software (2023; StataCorp LLC). Continuous variables were expressed
as the mean ± standard deviation, while categorical variables were
expressed as percentages. A t-test and a Chi-square test were used.
Statistical significance was set at a P-value of less than 0.05.
Differences in demographic characteristics and the prevalence of
vascular risk factors were examined. Descriptive statistics were
calculated for all variables. Pearson's Chi-square test or Fisher's
exact test was used to test differences in proportions between
groups, where appropriate. Regression analysis was used to
determine the extent to which vascular risk factors predict the
outcomes of endovascular MT in patients with stroke, considering
other patient characteristics and comorbidities.
Ethical considerations
The Institutional Review Board (IRB) of King Fahad
Specialist Hospital, approved the study (approval no. NEU0397;
Dammam, Saudi Arabia). As an observational, non-interventional
study, it posed minimal risk to participants. All patient data were
anonymized, and identifying information was removed to ensure
confidentiality. The requirement for consent was waived due to the
retrospective nature of the data analysis.
Results
A total of 56 individuals with LVO stroke who
underwent endovascular MT were included in the study to evaluate
the impact of vascular risk factors on MT outcome and to estimate
the prevalence of epilepsy.
An overview of participant characteristics of the
participants is presented in Table
I. Hypertension was the most prevalent comorbidity, identified
in 33 (59.0%) followed by diabetes mellitus in 29 patients (51.8%).
An additional 29 individuals (51.8%) had other unspecified comorbid
conditions. Atrial fibrillation was observed in 15 patients
(26.9%), while both smoking and dyslipidemia were reported in 10
patients each (17.9%). Heart failure was present in 7 individuals
(12.5%), and a history of previous stroke was noted in 6 cases
(10.7%). Cardiac thrombus and prior transient ischemic attack (TIA)
were the least common, each reported in 1 patient (1.79%).
 | Table IPatient characteristics and vascular
risk factors among patients with stroke (n=56). |
Table I
Patient characteristics and vascular
risk factors among patients with stroke (n=56).
| Risk factors | Frequency | Percentage, % |
|---|
| Hypertension | 33 | 59.0 |
| Diabetes
mellitus | 29 | 51.8 |
| Other
comorbidities | 29 | 51.8 |
| Atrial
fibrillation | 15 | 26.9 |
| Smoking | 10 | 17.9 |
| Dyslipidemia | 10 | 17.9 |
| Heart failure | 7 | 12.50 |
| Old stroke | 6 | 10.71 |
| Cardiac thrombus | 1 | 1.79 |
| Previous TIA | 1 | 1.79 |
| Body mass index | Mean ± SD | 27.2±5.3 |
| Age | Mean ± SD | 62±15.2 |
The mean body mass index (BMI) of the study
population was 27.2±5.3, indicating a leaning towards the
overweight category. The average age was 62 years (SD ± 15.2),
showing a wide age distribution among patients with stroke. These
findings suggest that hypertension and diabetes are significant
risk factors for stroke in this population, and the presence of
multiple comorbidities is common among patients with stroke. The
results underscore the need to address a broad spectrum of vascular
risk factors in both acute management and long-term prevention
strategies for ischemic stroke.
Stroke location distribution
Among the 56 patients, the most common site of
stroke was the right middle cerebral artery (Rt MCA) territory,
accounting for 28 cases (50%). This was followed by the Left MCA
territory 22 patients (39.3%). The remaining stroke locations were
less frequent. The data indicates a clear predominance of strokes
in the MCA territories, particularly on the right side, with rare
occurrences in other specified areas.
Thrombectomy techniques
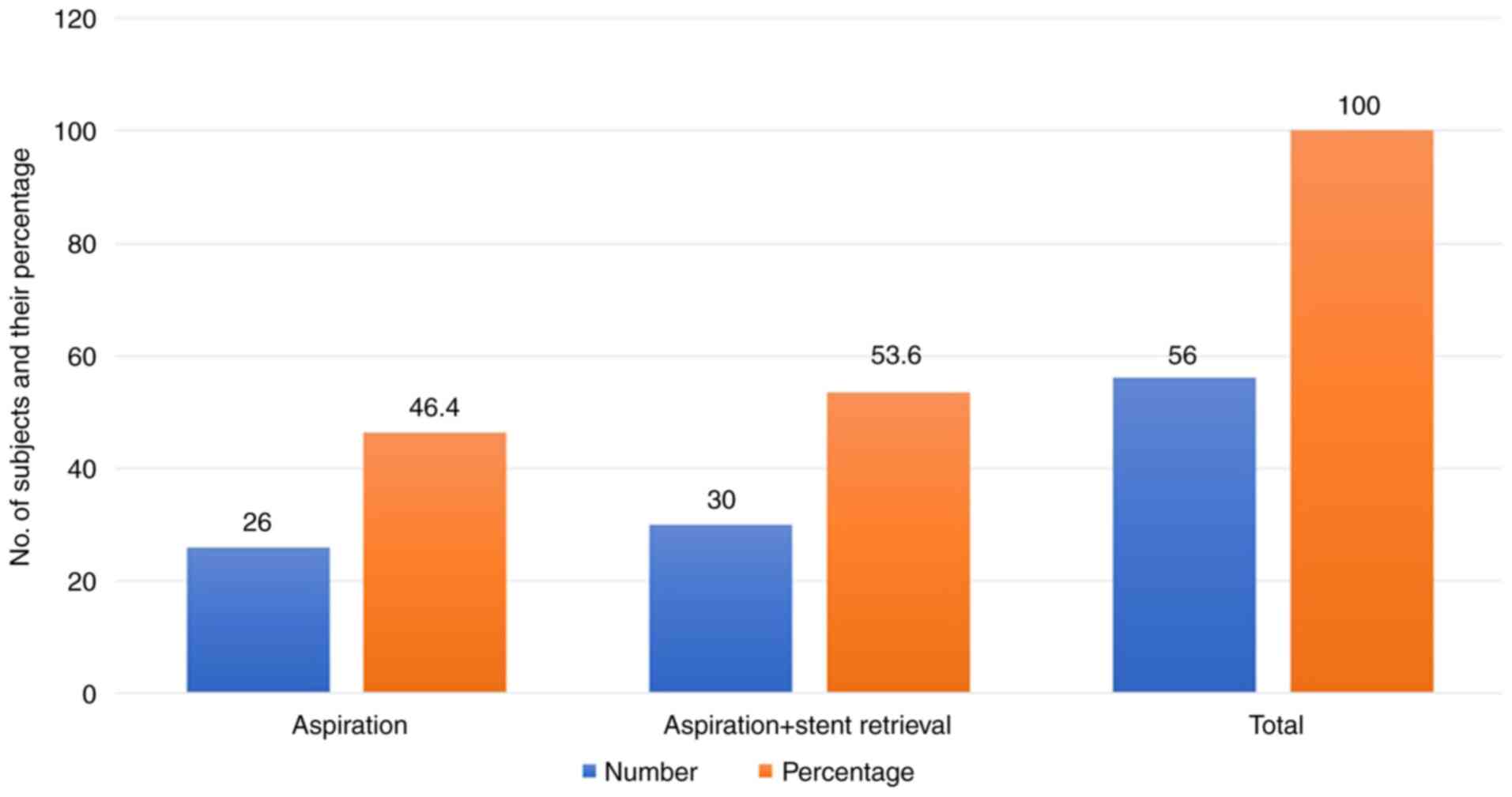
As illustrated in Fig.
1, aspiration in combination with stent retrieval was the most
commonly employed technique, used in 30 patients (53.6%).
Aspiration alone was performed in 26 cases (46.4%), indicating a
clear preference for aspiration-based approaches, either alone or
in combination.
Reperfusion outcomes (mTICI
score)
The distribution of mTICI scores following
thrombectomy is shown in Table II.
Complete reperfusion (Grade 3) was achieved in 17 patients (30.4%),
while partial reperfusion (Grade 2B) occurred in 31 cases (55.4%).
No patients were classified as Grade 2A. Minimal perfusion (Grade
1) and no perfusion (Grade 0) were each observed in 4 patients
(7.1%). Overall, 85.8% of patients (Grades 3 and 2B combined)
achieved substantial reperfusion, while 14.2% (Grades 0 and 1) had
poor outcomes, underscoring the variability in response to MT.
 | Table IIDistribution of outcomes based on
post-treatment mTICI scores. |
Table II
Distribution of outcomes based on
post-treatment mTICI scores.
| mTICI Grade | Frequency (%) |
|---|
| Grade 3 | 17 (30.4) |
| Grade 2B | 31 (55.4) |
| Grade 1 | 4 (7.1) |
| Grade 0 | 4 (7.1) |
| Total | 56(100) |
Effect of TPA on recanalization
outcomes
mTICI outcomes between patients who received
intravenous tissue plasminogen activator (TPA) and those who did
not are compared in Table III. Of
the 56 patients, 21 received TPA and 35 did not. Among TPA
recipients, 8 (38.1%) achieved Grade 3 and 11 (52.4%) achieved
Grade 2B reperfusion. By contrast, 9 (25.7%) non-TPA patients
achieved Grade 3 and 20 (57.1%) achieved Grade 2B. Statistical
analysis revealed a significant association between TPA
administration and higher mTICI scores (Fisher's exact test,
P=0.03; likelihood-ratio chi-square, P=0.041). These findings
support the beneficial role of TPA in enhancing recanalization
outcomes when used adjunctively with MT.
 | Table IIIComparison of mTICI outcomes between
patients who received and did not receive TPA (n=56). |
Table III
Comparison of mTICI outcomes between
patients who received and did not receive TPA (n=56).
| | Received TPA | |
|---|
| TICI score | Yes | No | Total |
|---|
| Grade 3 | 8 | 9 | 17 |
| Grade 2B | 11 | 20 | 31 |
| Grade 1 | 1 | 3 | 4 |
| Grade 0 | 1 | 3 | 4 |
| Total | 21 | 35 | 56 |
Risk factors for hemorrhagic
transformation
Clinical risk factors associated with hemorrhagic
transformation are presented in Table
IV. Significant predictors included: Age was identified as a
crucial risk factor, with individuals aged 65 and younger having an
odds ratio (OR) of 2.5 (95% CI: 1.8-3.6) and a P=0.001. This
indicates a significant increase in the risk of hemorrhagic
transformation among older patients.
 | Table IVLogistic regression analysis of risk
factors associated with hemorrhagic transformation. |
Table IV
Logistic regression analysis of risk
factors associated with hemorrhagic transformation.
| Risk factor | Odds ratio | 95% confidence
interval | P-value |
|---|
| Age (less than 65
years) | 2.5 | 1.8-3.6 | 0.001 |
| Hypertension | 3.0 | 2.2-4.1 | <0.001 |
| Diabetes
mellitus | 1.8 | 1.2-2.7 | 0.008 |
| Dyslipidemia | 1.2 | 0.8-1.9 | 0.300 |
| Smoking | 1.0 | 0.7-1.4 | 0.900 |
| Sex | 1.1 | 0.8-1.6 | 0.450 |
| Atrial
fibrillation | 1.3 | 0.9-1.9 | 0.200 |
| Old stroke | 1.4 | 0.9-2.2 | 0.150 |
| Previous TIA | 1.0 | 0.7-1.5 | 0.900 |
| Heart Failure | 1.5 | 1.0-2.2 | 0.050 |
| Cardiac
thrombus | 2.0 | 1.3-3.1 | 0.005 |
| Body mass
index | 1.1 | 0.9-1.3 | 0.450 |
| -cons | 0.3 | 0.08-1.5 | 0.17 |
Hypertension emerged as the most notable risk factor
(OR, 3.0; 95% CI: 2.2-4.1) with a highly significant P<0.001.
This suggests that patients with hypertension are three times more
likely to experience hemorrhagic transformation compared to those
without hypertension.
Diabetes mellitus also showed a significant
association with hemorrhagic transformation, with an OR of 1.8 (95%
CI: 1.2-2.7) and a P=0.008. This indicates that diabetic patients
have an increased risk of hemorrhagic transformation.
Additionally, heart failure was approaching
significance with an OR of 1.5 (95% CI: 1.0-2.2) and a P=0.05,
while cardiac thrombus showed a strong significant association with
an OR of 2.0 (95% CI: 1.3-3.1) and a P=0.005, suggesting that
patients with cardiac thrombi have double the odds of hemorrhagic
transformation.
By contrast, dyslipidemia (P=0.300), smoking
(P=0.900), sex (P=0.450), atrial fibrillation (P=0.200), old stroke
(P=0.150), previous TIA (P=0.900) and BMI (P=0.450) did not show
significant associations with hemorrhagic transformation. Their ORs
were close to 1.0, indicating that they may not substantially
influence the risk of this complication.
The significant risk factors for hemorrhagic
transformation include age, hypertension, diabetes, heart failure
and cardiac thrombus. This emphasizes the critical need for
thorough monitoring and management of these conditions in patients
with stroke after endovascular MT, as they are vulnerable to
hemorrhagic transformation. Further research is recommended to
elucidate the mechanism of these associations and evaluate
potential preventive strategies.
Predictors of thrombectomy
outcomes
In Table V, logistic
regression identified age ≤65 years as a significant predictor of
favorable MT outcomes (OR, 2.3; 95% CI: 1.5-3.5; P=0.002). No
significant associations were observed with hypertension, diabetes,
dyslipidemia, smoking, atrial fibrillation, old stroke, TIA, heart
failure, cardiac thrombus, or BMI. For example, hypertension showed
no predictive value (OR, 1.0; 95% CI: 0.6-1.6; P=0.900). These
findings highlight age as a critical determinant of MT success in
this cohort.
 | Table VPredictors of mechanical thrombectomy
outcomes in patients with stroke (n=56). |
Table V
Predictors of mechanical thrombectomy
outcomes in patients with stroke (n=56).
| Predictor | Odds ratio | 95% confidence
interval | P-value |
|---|
| Age (≥65
years) | 2.3 | 1.5-3.5 | 0.002 |
| Hypertension | 1.0 | 0.6-1.6 | 0.900 |
| Diabetes
mellitus | 0.9 | 0.5-1.5 | 0.700 |
| Dyslipidemia | 1.1 | 0.7-1.8 | 0.400 |
| Smoking | 1.2 | 0.8-1.9 | 0.600 |
| Sex | 1.0 | 0.6-1.5 | 0.950 |
| Atrial
fibrillation | 0.9 | 0.5-1.4 | 0.600 |
| Old stroke | 1.0 | 0.6-1.6 | 0.800 |
| Previous TIA | 1.1 | 0.7-1.8 | 0.500 |
| Heart failure | 1.3 | 0.8-2.1 | 0.250 |
| Cardiac
thrombus | 1.4 | 0.9-2.2 | 0.150 |
| Body mass
index | 1.0 | 0.9-1.1 | 0.800 |
Prevalence of post-stroke
epilepsy
Of the 56 patients studied, 8 (14.29%) developed
post-stroke seizures, while 48 (85.71%) did not. This indicates a
seizure prevalence of 14.29% in patients with LVO stroke treated
with MT.
Effect of TPA on seizure
incidence
The relationship between TPA administration and
seizure occurrence is analyzed in Table VI. Among 21 TPA recipients, only 2
(9.5%) developed seizures, while 6 (17.1%) of the 35 non-TPA
patients experienced seizures. Statistical analysis revealed a
significant association between TPA use and reduced seizure
incidence (likelihood-ratio chi-square test, P=0.0419; Fisher's
exact test, P=0.046). These results suggest that TPA could benefit
patients with stroke with LVO who undergo endovascular MT by
reducing the incidence of seizures. However, the evidence could be
more substantial, and further research is needed to confirm this
finding.
 | Table VIAssociation between seizure
occurrence and TPA administration among patients with stroke
(n=56). |
Table VI
Association between seizure
occurrence and TPA administration among patients with stroke
(n=56).
| | Received TPA | |
|---|
| Seizures | Not received TPA, N
(%) | Revived TPA N
(%) | Total | P-value |
|---|
| No seizures | 29 (51.8) | 19 (33.9) | 48 (85.7) | 0.041 |
| Seizures | 6 (10.7) | 8 (3.6) | 8 (14.3) | 0.041 |
| Total | 35 (62.5) | 21 (37.5) | 56(100) | 0.046 |
Discussion
The present study examined the impact of vascular
risk factors on outcomes following endovascular MT in patients with
stroke with LVO and yielded several key findings.
A notable finding was the prevalence of post-stroke
epilepsy, observed in 14.29% of patients who underwent MT. This
rate is higher than that reported in a 2022 systematic review,
which found a cumulative incidence of 9% among patients with stroke
treated with MT (13). The
increased prevalence in our cohort may reflect the specific focus
on LVO strokes, which are associated with more extensive brain
tissue damage and, consequently, a higher risk of seizures. This
underscores the importance of post-stroke seizure monitoring and
early intervention to improve patient quality of life and reduce
long-term neurological complications.
Our findings also suggest a potential benefit of TPA
in reducing seizure incidence among patients with MT. While prior
studies have reported mixed results (14-17),
our data support a statistically significant association between
TPA administration and reduced seizure risk. Given the potential
clinical significance of this finding, further research is
warranted to confirm the potential benefit of TPA in reducing
seizures. A more extensive, prospective study with a more diverse
patient cohort could provide more definitive evidence.
Additionally, exploring the mechanisms by which TPA might exert
this protective effect could offer insights into the
pathophysiology of post-stroke seizures and lead to targeted
prevention strategies.
A substantial proportion of patients (85.8%)
achieved successful reperfusion (mTICI Grades 2B-3), reinforcing
the effectiveness of MT in restoring cerebral perfusion. This
aligns with existing evidence from clinical trials and
meta-analyses demonstrating MT's efficacy in improving outcomes for
LVO stroke (18-21).
Future research should focus on identifying predictors of
reperfusion success and exploring novel adjunctive therapies that
could enhance the efficacy of endovascular MT. Additionally,
efforts should be made to optimize patient selection and treatment
timing to maximize the chances of successful reperfusion.
TPA administration within the recommended window
(3-4.5 h) was associated with improved recanalization outcomes,
consistent with current guideline-supported bridging therapy
protocols (22-25).
This supports the continued use of TPA, both systemically and
intra-arterially, as a complement to MT in eligible patients to
enhance both short- and long-term recovery.
In terms of complications, hemorrhagic
transformation was significantly associated with age, hypertension,
diabetes mellitus, heart failure and cardiac thrombus. These
results are consistent with previous studies (26-30)
and emphasize the need for personalized risk assessment and
vigilant monitoring in patients undergoing MT. The consistency of
these findings across studies underscores the importance of these
risk factors in the clinical management of patients with stroke.
These findings emphasize the need for personalized stroke
management strategies that consider individual patient risk
profiles.
Age was a significant predictor of MT outcomes, with
patients ≤65 years demonstrating higher odds of favorable recovery.
This is consistent with previous studies (31-33)
showing that younger patients tend to have improved physiological
resilience and post-intervention recovery. This finding suggests
that younger patients should be actively considered for
endovascular MT when they present with LVO strokes. The potential
for favorable outcomes in this age group underscores the importance
of timely intervention and access to specialized stroke care
(34-36).
The age is both statistically robust and clinically significant,
reinforcing age as a pivotal factor in MT outcomes. These findings
advocate for age-tailored protocols in acute stroke management
while highlighting the need for further research to optimize
outcomes in older populations.
Additionally, our results suggest that TPA may exert
neuroprotective effects beyond its thrombolytic action. Preclinical
studies have proposed mechanisms such as modulation of NMDA
receptor trafficking and reduced excitotoxicity (31), which may explain its potential
anti-epileptogenic effects. While our study used the standard 0.9
mg/kg dose, emerging evidence suggests that lower doses may be
effective in certain populations with reduced bleeding risk.
Moreover, the benefit of adjunctive TPA in extended time windows
(for example, per DAWN/DEFUSE-3 criteria) remains an area of active
investigation, particularly given varying ischemic tolerances and
endothelial vulnerability.
To enhance the innovation and clinical applicability
of the discussion section, we recommend integrating three key
improvements: i) a deeper exploration of the mechanistic links
between vascular risk factors and thrombectomy outcomes, including
potential biological pathways (for example, endothelial
dysfunction, clot composition); ii) the incorporation of predictive
modeling approaches (for example, nomograms or machine learning
tools) to stratify patients by individualized risk profiles; and
iii) a clear translational roadmap outlining how these findings
could inform clinical protocols, such as tailored peri-procedural
management for high-risk subgroups. These refinements would bridge
the gap between observational data and actionable clinical
insights. These findings advocate for more personalized protocols,
incorporating risk stratification tools (for example, glycemic and
BP thresholds) and evaluating novel adjunctive therapies in
high-risk patients.
The present study has several limitations. Its
retrospective design introduces the potential for selection and
information bias due to reliance on medical record documentation.
The sample size, though sufficient to detect moderate effect sizes,
may limit the statistical power to detect smaller associations.
Additionally, being a single-center study, the findings may not be
generalizable to broader or more diverse populations. Future
research should employ prospective, multicenter designs with larger
cohorts to validate and expand upon these findings.
Further research is needed to elucidate the
mechanisms underlying this age-dependent effect and to develop
targeted strategies for optimizing outcomes in older populations.
Future studies should quantify the magnitude of this benefit in
real-world clinical settings and explore adjunctive therapies to
mitigate age-related disparities.
In conclusion, the present study provides important
insights into the impact of vascular risk factors on MT outcomes in
patients with stroke with LVO. It highlights the effectiveness of
MT in achieving successful reperfusion and suggests potential
benefits of adjunctive TPA administration in improving
recanalization and reducing seizure risk. The findings reinforce
the importance of personalized, risk-based management strategies,
especially with regard to age, comorbidities, and hemorrhagic
complications. Comprehensive post-stroke care should integrate
seizure surveillance and address modifiable vascular risk factors
to optimize both acute outcomes and long-term recovery across
patient demographics.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the King Salman
center For Disability Research (grant no. KSRG-2024-307).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
WAA contributed to study conception and design, data
collection, analysis and interpretation, drafting, and critical
revision of the manuscript. SB contributed to study design, data
interpretation, manuscript drafting and critical revision for
intellectual content. EMA contributed to data collection, data
analysis, and initial manuscript drafting. BA contributed to data
interpretation, supervision, manuscript review and editing for
important intellectual content, and approved the final version. WAA
and SB confirm the authenticity of all the raw data. All authors
read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the local ethic
committee (approval no. NEU0397) of King Fahad Specialist Hospital
Dammam. The requirement for consent was waived due to the
retrospective nature of the data analysis.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript or to generate images, and subsequently,
the authors revised and edited the content produced by the
artificial intelligence tools as necessary, taking full
responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Saini V, Guada L and Yavagal DR: Global
epidemiology of stroke and access to acute ischemic stroke
interventions. Neurology. 97 (20 Suppl 2):S6–S16. 2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Widimsky P, Snyder K, Sulzenko J, Hopkins
LN and Stetkarova I: Acute ischaemic stroke: Recent advances in
reperfusion treatment. Eur Heart J. 44:1205–1215. 2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Balami JS, White PM, McMeekin PJ, Ford GA
and Buchan AM: Complications of endovascular treatment for acute
ischemic stroke: Prevention and management. Int J Stroke.
13:348–361. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jadhav AP, Desai SM and Jovin TG:
Indications for mechanical thrombectomy for acute ischemic stroke:
Current guidelines and beyond. Neurology. 97 (20 Suppl
2):S126–S136. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhu Y, Zhang H, Zhang Y, Wu H, Wei L, Zhou
G, Zhang Y, Deng L, Cheng Y, Li M, et al: Endovascular metal
devices for the treatment of cerebrovascular diseases. Adv Mater.
31(e1805452)2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Anagnostakou V, Epshtein M, Kühn AL, King
RM, Puri A and Gounis MJ: Preclinical modeling of mechanical
thrombectomy. J Biomech. 130(110894)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ząbczyk M, Ariëns RAS and Undas A: Fibrin
clot properties in cardiovascular disease: From basic mechanisms to
clinical practice. Cardiovasc Res. 119:94–111. 2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Almallouhi E, Al Kasab S, Hubbard Z, Bass
EC, Porto G, Alawieh A, Chalhoub R, Jabbour PM, Starke RM, Wolfe
SQ, et al: Outcomes of mechanical thrombectomy for patients with
stroke presenting with low alberta stroke program early computed
tomography score in the early and extended window. JAMA Netw Open.
4(e2137708)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ganesh A, Ospel JM, Menon BK, Demchuk AM,
McTaggart RA, Nogueira RG, Poppe AY, Almekhlafi MA, Hanel RA,
Thomalla G, et al: Assessment of discrepancies between follow-up
infarct volume and 90-day outcomes among patients with ischemic
stroke who received endovascular therapy. JAMA Netw Open.
4(e2132376)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jiang S, Fei A, Peng Y, Zhang J, Lu YR,
Wang HR, Chen M and Pan S: Predictors of outcome and hemorrhage in
patients undergoing endovascular therapy with solitaire stent for
acute ischemic stroke. PLoS One. 10(e0144452)2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Karamchandani RR, Satyanarayana S, Yang H,
Rhoten JB, Strong D, Clemente JD, Defilipp G, Patel NM, Bernard JD,
Stetler WR, et al: Predictors of devastating functional outcome
despite successful basilar thrombectomy. Interv Neuroradiol:
November 21, 2023 (Epub ahead of print).
|
|
12
|
Wnuk M, Popiela T, Drabik L, Brzegowy P,
Lasocha B, Wloch-Kopec D, Pulyk R, Jagiella J, Wiacek M,
Kaczorowski R, et al: Fasting hyperglycemia and long-term outcome
in patients with acute ischemic stroke treated with mechanical
thrombectomy. J Stroke Cerebrovasc Dis. 29(104774)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Liu F, Chen D, Fu Y, Wang H and Liu L:
Incidence and association of seizures in stroke patients following
endovascular treatment: A systematic review and meta-analysis. Eur
J Neurol. 30:134–143. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Saver JL, Goyal M, Bonafe A, Diener HC,
Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, et
al: Stent-retriever thrombectomy after intravenous t-PA vs t-PA
alone in stroke. N Engl J Med. 372:2285–2295. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Janelidze S, Berron D, Smith R, Strandberg
O, Proctor NK, Dage JL, Stomrud E, Palmqvist S, Mattsson-Carlgren N
and Hansson O: Associations of plasma phospho-tau217 levels with
tau positron emission tomography in early Alzheimer disease. JAMA
Neurol. 78:149–156. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gruber J, Gattringer T, Mayr G,
Schwarzenhofer D, Kneihsl M, Wagner J, Sonnberger M, Deutschmann H,
Haidegger M, Fandler-Höfler S, et al: Frequency and predictors of
poststroke epilepsy after mechanical thrombectomy for large vessel
occlusion stroke: Results from a multicenter cohort study. J
Neurol. 270:6064–6070. 2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Naylor J, Thevathasan A, Churilov L, Guo
R, Xiong Y, Koome M, Chen Z, Chen Z, Liu X, Kwan P and Campbell
BCV: Association between different acute stroke therapies and
development of post stroke seizures. BMC Neurol.
18(61)2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nesselroth D, Gilad R, Namneh M, Avishay S
and Eilam A: Estimation of seizures prevalence in ischemic strokes
after thrombolytic therapy. Seizure. 62:91–94. 2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lekoubou A, Awoumou JJ and Kengne AP:
Incidence of seizure in stroke patients treated with recombinant
tissue plasminogen activator: A systematic review and
meta-analysis. Int J Stroke. 12:923–931. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Brigo F, Schneider M, Wagenpfeil G,
Ragoschke-Schumm A, Fousse M, Holzhoffer C, Nardone R, Faßbender K
and Lochner P: Intravenous thrombolysis with tPA and cortical
involvement increase the risk of early poststroke seizures: Results
of a case-control study. Epilepsy Behav. 104(106312)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhao W, Ma P, Zhao W, Yang B, Zhang Y,
Song J, Zhang P and Yue X: The safety and efficacy of mechanical
thrombectomy in posterior vs anterior emergent large vessel
occlusion: A systematic review and meta-analysis. J Stroke
Cerebrovasc Dis. 29(104545)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Dargazanli C, Arquizan C, Gory B, Consoli
A, Labreuche J, Redjem H, Eker O, Decroix JP, Corlobé A, Mourand I,
et al: Mechanical thrombectomy for minor and mild stroke patients
harboring large vessel occlusion in the anterior circulation: A
multicenter cohort study. Stroke. 48:3274–3281. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Alexandre AM, Valente I, Pedicelli A,
Pezzullo AM, Colò F, Scarcia L, Romi A, Piano M, Macera A, Gabrieli
JD, et al: Mechanical thrombectomy in acute ischemic stroke due to
large vessel occlusion in the anterior circulation and low baseline
national institute of health stroke scale score: A multicenter
retrospective matched analysis. Neurol Sci. 43:3105–3112.
2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Nagel S, Bouslama M, Krause LU, Küpper C,
Messer M, Petersen M, Lowens S, Herzberg M, Ringleb PA, Möhlenbruch
MA, et al: Mechanical thrombectomy in patients with milder strokes
and large vessel occlusions. Stroke. 49:2391–2397. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Cheng NT and Kim AS: Intravenous
thrombolysis for acute ischemic stroke within 3 h versus between 3
and 4.5 h of symptom onset. Neurohospitalist. 5:101–109.
2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Song S: Hyperacute management of ischemic
stroke. Semin Neurol. 33:427–435. 2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Del Zoppo GJ, Saver JL, Jauch EC and Adams
HP Jr: American Heart Association Stroke Council. Expansion of the
time window for treatment of acute ischemic stroke with intravenous
tissue plasminogen activator: A science advisory from the American
heart association/American stroke association. Stroke.
40:2945–2948. 2009.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Nguyen TQ, Truong AL, Phan HT, Nguyen DD,
Nguyen KV, Nguyen HTB, Nguyen ATT, Hoang DCB, Tran VT, Nguyen TQ,
et al: Bridging therapy and direct thrombectomy for acute ischemic
stroke: A prospective cohort study. J Stroke Med. 3:124–130.
2020.
|
|
29
|
Kablau M, Kreisel SH, Sauer T, Binder J,
Szabo K, Hennerici MG and Kern R: Predictors and early outcome of
hemorrhagic transformation after acute ischemic stroke. Cerebrovasc
Dis. 32:334–341. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Thomas SE, Plumber N, Venkatapathappa P
and Gorantla V: A review of risk factors and predictors for
hemorrhagic transformation in patients with acute ischemic stroke.
Int J Vasc Med. 2021(4244267)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kunte H, Busch MA, Trostdorf K, Vollnberg
B, Harms L, Mehta RI, Castellani RJ, Mandava P, Kent TA and Simard
JM: Hemorrhagic transformation of ischemic stroke in diabetics on
sulfonylureas. Ann Neurol. 72:799–806. 2012.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Tan S, Wang D, Liu M, Zhang S, Wu B and
Liu B: Frequency and predictors of spontaneous hemorrhagic
transformation in ischemic stroke and its association with
prognosis. J Neurol. 261:905–912. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yu G, Kim YJ, Jeon SB and Kim WY:
Thromboelastography for prediction of hemorrhagic transformation in
patients with acute ischemic stroke. Am J Emerg Med. 38:1772–1777.
2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Bagg S, Pombo AP and Hopman W: Effect of
age on functional outcomes after stroke rehabilitation. Stroke.
33:179–185. 2002.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Emberson J, Lees KR, Lyden P, Blackwell L,
Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, et al:
Effect of treatment delay, age, and stroke severity on the effects
of intravenous thrombolysis with alteplase for acute ischaemic
stroke: A meta-analysis of individual patient data from randomised
trials. Lancet. 384:1929–1935. 2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Adcock AK, Schwamm LH, Smith EE, Fonarow
GC, Reeves MJ, Xu H, Matsouaka RA, Xian Y and Saver JL: Trends in
use, outcomes, and disparities in endovascular thrombectomy in US
patients with stroke aged 80 years and older compared with younger
patients. JAMA Netw Open. 5(e2215869)2022.PubMed/NCBI View Article : Google Scholar
|