Introduction
Obstructive sleep apnea (OSA) is a common disease in
clinical practice. The average prevalence of OSA was 56% (1). Its prevalence may be high as 85% in
adults and elderly individuals. The prevalence of OSA may be varied
among countries with the highest prevalence in Mongolia (93%).
Untreated or unrecognized OSA may lead to several cardiovascular
diseases such as coronary artery disease or hypertension. The
prevalence of OSA in patients with these cardiovascular diseases
can be as high as 80% (2).
Additionally, OSA may result in several neuropsychological diseases
if left untreated including cognitive impairment, or depression
(3,4). Patients with OSA are at risk for
depression with odds ratio of 2.18 (95% confidence interval of
1.47, 2.88) by longitudinal studies (5).
Dizziness is a bothersome symptom and may cause by
several diseases such as hypertensive emergency (6,7). The
prevalence of dizziness in general population is ~30% (8-10).
Even though there are several causes of dizziness such as upper
respiratory tract infection, anemia, hypoglycemia, anxiety,
depression, postural hypotension, or hypertensive emergency, up to
80% of patients with dizziness are unexplained (11). One possible cause of dizziness OSA
reported by a national database from Korea (12). Patients with OSA had higher
incidence rate of dizziness than the non-OSA patients (149.86 vs.
23.88 per 10,000 individuals) with the incidence rate ratio of 6.28
(95% confidence interval of 4.89, 8.08). Even though the national
database study showed the positive correlation between OSA and
dizziness, there is limited data on risk factors of OSA in patients
with dizziness. The national database study provided only the
incidence and the correlation of both conditions. Additionally,
other causes of dizziness were not adjusted in the national
database study. A real-world study or pragmatic study can provide
the prevalence and risk factors of OSA in patients with dizziness.
Previously, two studies found that OSA was related with dizziness
(13,14). Being OSA had odds ratio of 1.69
(P=0.022) to be associated with OSA. However, both studies were
conducted by using the STOPBang questionnaire, not polysomnography.
Therefore, the present study aimed to evaluate the prevalence and
risk factors of OSA in patients with dizziness in real-world
clinical practice using home sleep apnea test.
Materials and methods
This was a retrospective cohort study conducted at
the outpatient department, University Hospital of Khon Kaen
University, Thailand. The inclusion criteria were adult patients
(aged ≥18 years) who had unexplained dizziness and underwent
overnight home sleep apnea test. Those who were pregnant or had
identifiable cause of dizziness such as upper respiratory tract
infection, anemia, hypoglycemia, anxiety, depression, postural
hypotension, or hypertensive emergency were excluded. These
excluded conditions were recorded from medical charts or history
taking. The study period was between November 2022 and November
2024.
Eligible patients were evaluated for OSA by baseline
characteristics, comorbidities, STOPBang score (15), and physical examination. The
overnight home sleep apnea test (Alice PDX®, Phillips
Respironics) was performed in all eligible patients. Overnight home
sleep apnea test comprised of nasal pressure transducer, pulse
oximeter, and chest belt to record chest movement body position
(16). The total sleep time for
overnight sleep apnea test was at least 4 h. Sleep tracings were
scored manually for apnea and hypopnea based on the criteria of
AASM (17). The device had
agreement with in-laboratory polysomnography of 96.4% (18). Diagnosis of OSA was made if an
apnea-hypopnea index (AHI) was five or more events/h.
Sample size calculation
The previous study reported that the incidence of
OSA in patients with dizziness by the national database study was
7.78% (12). The estimated
prevalence of OSA in patients with dizziness in clinical practice
was higher at 20% as previously reported (14). Based on the power of 80% and
confidence of 95%, the required sample size was 50 subjects.
Statistical analyses
Prevalence of OSA in patients with dizziness was
calculated. Patients were categorized into two groups: With and
without OSA. Results of studied variables of both groups were
reported as the mean (SD) or median (interquartile range) for
numerical variables according to normal distribution of studied
variables. For normally distributed variables, mean ± SD was
reported, while median (interquartile range) was reported for not
normally distributed variables. Number (proportion) was shown for
categorical variables. The differences of each studied variable
between the OSA and non-OSA group were computed by inferential
statistics. For numerical variables, the student t test or Wilcoxon
rank sum test was used to compare the differences between both
groups for normally distributed variables and non-normally
distributed variables, respectively. Fisher-Exact test was used to
compare the differences between two proportions.
Predictors OSA in patients with dizziness were
executed by stepwise method of multivariable logistic regression
analysis. Studied variables were computed for a P-value by
univariable logistic regression analysis. Those with P<0.20 or
clinically significant were included in the stepwise, multivariable
logistic regression analysis (19,20).
The model was tested for a goodness of fit by the Hosmer-Lemeshow
method. A P-value by the Hosmer-Lemeshow Chi square of more than
0.05 indicated a goodness of fit. A numerical predictor for being
OSA was computed for appropriate diagnostic cut off point by a
receiver operating characteristic (ROC) curve. Sensitivity and
specificity for the best cut-off point for OSA diagnosis were
reported. Studied variables with missing data of more than 50% were
not included in the analysis (21).
All statistical analyses were performed using STATA software
version 10.1 (StataCorp LP).
Results
During the study period, there were 81 patients met
the study criteria. Of those, 76 patients (93.83%) had OSA with a
median AHI of 23 events/h (IQR of 11.5-33.5), while the non-OSA
group had a median AHI of 4 events/h (IQR 3.9-4.0). Regarding
baseline characteristics, comorbidities and symptoms of OSA
(Table I), STOPBang score was
significantly different between both groups. The OSA group had
higher average of STOPBang score than the non-OSA group (3.95 vs.
2.40; P=0.026). The proportion of atrial fibrillation was
significantly higher in the non-OSA group than the OSA group (20.00
vs. 0%; P=0.005). For physical signs, the OSA group had significant
larger neck circumference than the non-OSA group: 37.63 vs. 33.25
cm (P=0.029) as shown in Table
II.
 | Table IBaseline characteristics,
comorbidities, and symptoms of patients with unexplained dizziness
categorized by presence of OSA. |
Table I
Baseline characteristics,
comorbidities, and symptoms of patients with unexplained dizziness
categorized by presence of OSA.
| Factors | Non-OSA (n=5) | OSA (n=76) | P-value |
|---|
| Mean (SD) age,
years | 59.00
(52.0-61.0) | 59.00
(47.5-65.0) | 0.523 |
| Male sex | 1 (20.0) | 33 (44.0) | 0.293 |
| Comorbidities | | | |
|
Hypertension | 2 (40.0) | 42 (56.8) | 0.465 |
|
Diabetes | 0 (0.0) | 18 (25.0) | 0.200 |
|
Coronary
artery disease | 0 (0.0) | 3 (4.0) | 0.646 |
|
Atrial
fibrillation | 1 (20.0) | 0 (0.0) | 0.005 |
|
Heart
failure | 0 (0.0) | 2 (2.7) | 0.710 |
|
Allergic
rhinitis | 0 (0.0) | 11 (14.8) | 0.353 |
| Symptoms | | | |
|
Snoring | 2 (40.0) | 57 (76.0) | 0.076 |
|
Stop
breathing | 0 (0.0) | 25 (33.3) | 0.119 |
|
Fatigue | 3 (60.0) | 35 (46.7) | 0.563 |
|
Dyspnea | 2 (40.0) | 13 (17.3) | 0.209 |
|
GERD | 2 (40.0) | 34 (45.3) | 0.855 |
|
Nocturia | 3 (60.0) | 56 (75.7) | 0.435 |
|
Light
sleeper | 3 (60.0) | 44 (58.7) | 0.953 |
|
Dizziness | 5 (100.0) | 100 (100.0) | 0.712 |
|
Sleepiness | 2 (40.0) | 49 (66.2) | 0.507 |
| Mean (SD)
STOPBANG | 2.40±1.52 | 3.95±1.48 | 0.026 |
 | Table IIPhysical signs of patients with
unexplained dizziness categorized by presence of OSA. |
Table II
Physical signs of patients with
unexplained dizziness categorized by presence of OSA.
| Factors | Non-OSA (n=5) | OSA (n=76) | P-value |
|---|
| Body mass index,
kg/m2 | 21.40
(16.80-25.65) | 26.75
(23.60-30.85) | 0.057 |
| Systolic blood
pressure, mmHg | 124.20±8.84 | 130.43±1.58 | 0.342 |
| Diastolic blood
pressure, mmHg | 73.00±4.66 | 74.32±1.21 | 0.786 |
| Neck circumference,
cm | 33.25±2.18 | 37.63±0.48 | 0.042 |
| Retrognathia | 1 (20.0) | 20 (27.4) | 0.718 |
| Torus
palatinus | 2 (40.0) | 19 (25.7) | 0.483 |
| Torus
mandibularis | 2 (40.0) | 15 (20.0) | 0.029 |
| Macroglossia | 1 (20.0) | 45 (60.8) | 0.073 |
| Friedman
classification | | | 0.059 |
|
1 | 0 (0.0) | 11 (14.9) | |
|
2 | 0 (0.0) | 14 (18.9) | |
|
3 | 4 (80.0) | 18 (24.3) | |
|
4 | 1 (20.0) | 31 (41.9) | |
|
Denture | 0 (0.0) | 12 (16.4) | 0.324 |
|
Tonsillectomy | 0 (0.0) | 0 (0.0) | - |
|
Thyromegaly | 0 (0.0) | 0 (0.0) | - |
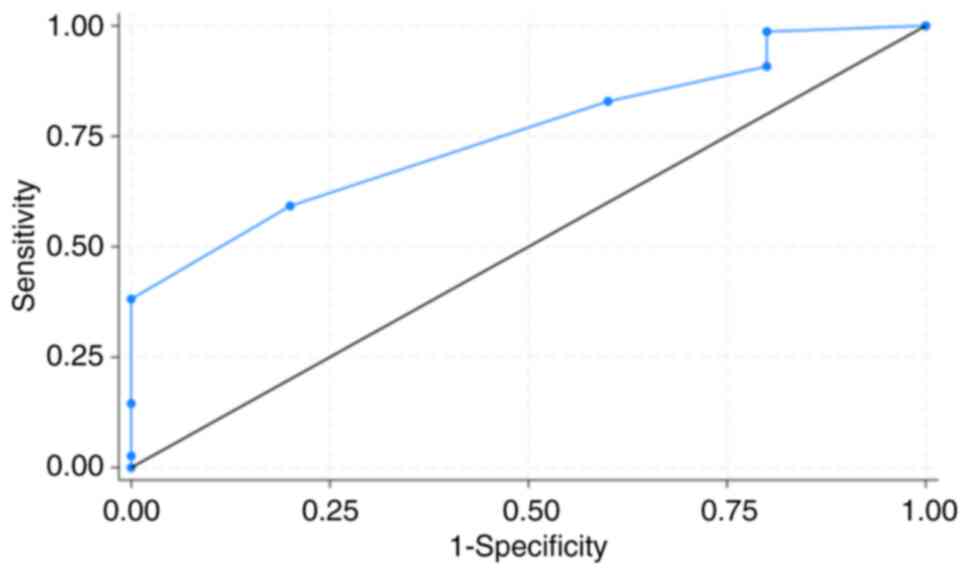
There were seven factors included in the predictive
model for OSA: Age, sex, snoring, nocturia, gastroesophageal reflux
disease, diabetes and STOPBang score. There were four factors
remaining in the model by stepwise logistic regression analysis
(Table III). Only STOPBang score
was independently associated with OSA with an adjusted odds ratio
of 2.115 (95% confidence interval of 1.048, 4.268). The
Hosmer-Lemeshow Chi square of the model was 3.24 (P=0.919)
indicating a goodness of fit of the model. The cut point of
STOPBang score of 3 or over had sensitivity of 82.89% and
specificity of 40.00% for OSA. The area under ROC curve of STOPBang
score on OSA was 75.39% (95% confidence interval of 57.50-93.29%)
as shown in Fig. 1.
 | Table IIIFactors predictive of obstructive
sleep apnea by multivariable logistic regression analysis in
patients with unexplained dizziness. |
Table III
Factors predictive of obstructive
sleep apnea by multivariable logistic regression analysis in
patients with unexplained dizziness.
| Factors | Unadjusted odds
ratio (95% confidence interval) | Adjusted odds ratio
(95% confidence interval) |
|---|
| STOPBang | 1.798 (0.982,
3.293) | 2.115 (1.048,
4.268) |
| Dyspnea | 0.314 (0.047,
2.074) | 0.127 (0.012,
1.243) |
| Nocturia | 2.074 (0.320,
13.408) | 2.609 (0.312,
21.779) |
| Torus
mandibularis | 0.375 (0.057,
2.449) | 0.383 (0.046,
3.170) |
Discussion
The present study showed that the prevalence of OSA
in patients with unexplained dizziness was notably high at 93.83%.
This prevalence was markedly higher than the previous national
study at 7.76% (12). This high
prevalence of OSA in the present study may be due to the different
study population from the previous study. The current study
enrolled only patients with unexplained dizziness, while the
national database study may enroll patients with dizziness from any
causes. These differences in study population may result in
different prevalence of OSA in patients with dizziness. A previous
study found that psychogenic dizziness or other causes of dizziness
were closely related to poor sleep (22). Both psychogenic dizziness and other
causes of dizziness had coefficients of 1.820 (P<0.05) and2.262
(P<0.01) to Pittsburg sleep quality index (PSQI), while only
other causes of dizziness were related to insomnia severity index
with a coefficient of 3.237 (P<0.05). These results showed poor
sleep quality and insomnia were found in these two types of
dizziness. Those with psychogenic and other causes of dizziness may
be similar to those with unexplained dizziness in the present
study. OSA is a condition leading to poor sleep quality and
insomnia. Patients with OSA had higher global score of PSQI than
those without OSA (8.62 vs. 5.36; P<0.001) as well as the C1
subscore of sleep quality (1.7 vs. 0.79; P<0.001) (23). Additionally, up to 50% of patients
with OSA reported symptoms of insomnia (24,25).
These data showed a close relationship between OSA and dizziness.
Even though the exact mechanisms of OSA associated with dizziness
remain unclear, there are several proposed mechanisms (13,26,27).
These mechanisms included brainstem and cerebellar damage,
imbalance of autonomic function, white matter damage, and
hippocampal degeneration in the areas associated with vestibular
function. These abnormalities were associated with intermittent
hypoxemia from OSA.
Among several studied variables, only STOPBang score
was a predictor of OSA in patients with unexplained dizziness. As
previously reported, the STOPBang score was a sensitive screening
tool for OSA in various settings across the world (15,28).
According to the adjusted odds ratio of 2.115 in the present study,
this finding may indicate moderate effect (29) of the STOPBang score as a screening
tool for OSA in patients with unexplained dizziness in clinical
setting of outpatient department. A systematic review showed that
STOPBang score of 3 or more had sensitivity of 91.4% to detect OSA
(28). Originally, the STOPBang was
used to screen for OSA in patients with perioperative setting.
Several studies showed that the STOPBang score can be used for OSA
detection in patients underwent bariatric surgery, or obese
patients (30-32).
Most studies found that the STOPBang score of 3 or more associated
with OSA as in the present study with patients with unexplained
dizziness (13,27). The original study for STOPBang score
in patients underwent surgery had sensitivity of 72%, while another
study showed the sensitivity of 87.9% in OSA detection with the
STOPBang questionnaire in obese patients. Similarly, the present
study showed the STOPBang score of 3 for OSA detection had
comparable sensitivity of 82.89% (Fig.
1). Note that low specificity of the STOPBang score of 40% may
result in false positive issue.
There are certain limitations to the present study.
First, the results may apply to only those without causes of
dizziness. Even though STOPBang was the statistically significant
factor, clinical significance was not evaluated in the present
study (33). As the outcome was the
diagnosis of OSA, not the effectiveness or efficacy of treatment
modality, clinical significance may not be able to be evaluated.
Second, no intervention such as a continuous positive airway
pressure machine was applied to the patients. Further studies to
evaluate CPAP treatment effects on dizziness as a treatment option.
Finally, the predictive model comprised only baseline clinical
parameter; no laboratory tests were included. Further cohort
studies including patients with other causes of dizziness with
laboratory tests may advance the knowledge provided by the current
study.
In conclusion, OSA was markedly prevalent in
patients with unexplained dizziness. The STOPBang questionnaire may
be used as a screening tool to detect OSA in this setting with high
sensitivity.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
NL, SK and KS conceived and designed the study. SS
collected data and interpreted data. WB interpreted data. KS
performed statistical analysis. All authors read and approved the
final version of the manuscript. NL, SK and KS confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
The study protocol was approved (approval no.
HE641504) by the ethics committee in human research of Khon Kaen
University (Khon Kaen, Thailand) and all methods were conducted
following the principles of the Declaration of Helsinki. The
requirement for informed consent was waived due to the
retrospective nature of the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
de Araujo Dantas AB, Gonçalves FM, Martins
AA, Alves GÂ, Stechman-Neto J, Corrêa CC, Santos RS, Nascimento WV,
de Araujo CM and Taveira KVM: Worldwide prevalence and associated
risk factors of obstructive sleep apnea: A meta-analysis and
meta-regression. Sleep Breath. 27:2083–2109. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Yeghiazarians Y, Jneid H, Tietjens JR,
Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE
and Somers VK: Obstructive sleep apnea and cardiovascular disease:
A scientific statement from the american heart association.
Circulation. 144:e56–e67. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chang WP, Liu ME, Chang WC, Yang AC, Ku
YC, Pai JT, Huang HL and Tsai SJ: Sleep apnea and the risk of
dementia: A population-based 5-year follow-up study in Taiwan. PLoS
One. 8(e78655)2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lajoie AC, Lafontaine AL, Kimoff RJ and
Kaminska M: Obstructive sleep apnea in neurodegenerative disorders:
Current evidence in support of benefit from sleep apnea treatment.
J Clin Med. 9(297)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Edwards C, Almeida OP and Ford AH:
Obstructive sleep apnea and depression: A systematic review and
meta-analysis. Maturitas. 142:45–54. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Alsharif A, Aljohani A, Ashour S, Zahim A
and Alsulimani L: Clinical outcomes of discharged patients with
high blood pressure in the emergency department. Cureus.
16(e76654)2024.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Newman-Toker DE, Dy FJ, Stanton VA, Zee
DS, Calkins H and Robinson KA: How often is dizziness from primary
cardiovascular disease true vertigo? A systematic review. J Gen
Intern Med. 23:2087–2094. 2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Chan Y: Differential diagnosis of
dizziness. Curr Opin Otolaryngol Head Neck Surg. 17:200–203.
2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Karatas M: Central vertigo and dizziness:
Epidemiology, differential diagnosis, and common causes.
Neurologist. 14:355–364. 2008.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lasisi AO and Gureje O: Prevalence and
correlates of dizziness in the Ibadan Study of Ageing. Ear Nose
Throat J. 93:E37–E44. 2014.PubMed/NCBI
|
|
11
|
van Leeuwen RB, Schermer TR and Bienfait
HP: The relationship between dizziness and sleep: A review of the
literature. Front Neurol. 15(1443827)2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Byun H, Chung JH, Jeong JH, Ryu J and Lee
SH: Incidence of peripheral vestibular disorders in individuals
with obstructive sleep apnea. J Vestib Res. 32:155–162.
2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kim E, Lee M and Park I: Risk of
obstructive sleep apnea, chronic dizziness, and sleep duration.
Nurs Res. 73:313–319. 2024.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Maas BDPJ, Bruintjes TD, van der
Zaag-Loonen HJ and van Leeuwen RB: The relation between dizziness
and suspected obstructive sleep apnoea. Eur Arch Otorhinolaryngol.
277:1537–1543. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chung F, Abdullah HR and Liao P: STOP-bang
questionnaire: A practical approach to screen for obstructive sleep
apnea. Chest. 149:631–638. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tran-Thi BT, Quach-Thieu M, Le-Tran BN,
Nguyen-Duc D, Tran-Hiep N, Nguyen-Thi T, Nguyen-Ngoc YL,
Nguyen-Tuan A, Tang-Thi-Thao T, Nguyen-Van T and Duong-Quy S: Study
of the agreement of the apnea-hypopnea index measured
simultaneously by pressure transducer via respiratory polygraphy
and by thermistor via polysomnography in real time with the same
individuals. J Otorhinolaryngol Hear Balance Med. 3(4)2022.
|
|
17
|
Berry RB, Brooks R, Gamaldo C, Harding SM,
Lloyd RM, Quan SF, Troester MT and Vaughn BV: AASM scoring manual
updates for 2017 (version 2.4). J Clin Sleep Med. 13:665–666.
2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nilius G, Domanski U, Schroeder M, Franke
KJ, Hogrebe A, Margarit L, Stoica M and d'Ortho MP: A randomized
controlled trial to validate the Alice PDX ambulatory device. Nat
Sci Sleep. 9:171–180. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mickey RM and Greenland S: The impact of
confounder selection criteria on effect estimation. Am J Epidemiol.
129:125–137. 1989.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Sun GW, Shook TL and Kay GL: Inappropriate
use of bivariable analysis to screen risk factors for use in
multivariable analysis. J Clin Epidemiol. 49:907–916.
1996.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Madley-Dowd P, Hughes R, Tilling K and
Heron J: The proportion of missing data should not be used to guide
decisions on multiple imputation. J Clin Epidemiol. 110:63–73.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kim SK, Kim JH, Jeon SS and Hong SM:
Relationship between sleep quality and dizziness. PLoS One.
13(e0192705)2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lusic Kalcina L, Valic M, Pecotic R,
Pavlinac Dodig I and Dogas Z: Good and poor sleepers among OSA
patients: Sleep quality and overnight polysomnography findings.
Neurol Sci. 38:1299–1306. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Mendes MS and dos Santos JM: Insomnia as
an expression of obstructive sleep apnea syndrome-the effect of
treatment with nocturnal ventilatory support. Rev Port Pneumol
(2006). 21:203–208. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wickwire EM and Collop NA: Insomnia and
sleep-related breathing disorders. Chest. 137:1449–1463.
2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Torabi-Nami M, Mehrabi S, Borhani-Haghighi
A and Derman S: Withstanding the obstructive sleep apnea syndrome
at the expense of arousal instability, altered cerebral
autoregulation and neurocognitive decline. J Integr Neurosci.
14:169–193. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Akiyama N, Suzuki Y, Tanaka T, Ito H and
Ichibayashi R: Obstructive sleep apnea as a hidden cause of
dizziness: A report of two non-obese patients. Cureus.
17(e84779)2025.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Pivetta B, Chen L, Nagappa M, Saripella A,
Waseem R, Englesakis M and Chung F: Use and Performance of the
STOP-Bang Questionnaire for Obstructive Sleep Apnea Screening
Across Geographic Regions: A systematic review and meta-analysis.
JAMA Netw Open. 4(e211009)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Chen H, Cohen P and Chen S: How big is a
big odds ratio? Interpreting the magnitudes of odds ratios in
epidemiological studies. Commun Stat Simul Comput. 39:860–864.
2010.
|
|
30
|
Matarredona-Quiles S, Carrasco-Llatas M,
Martínez-Ruíz de Apodaca P, Díez-Ares JÁ, González-Turienzo E and
Dalmau-Galofre J: Analysis of possible predictors of moderate and
severe obstructive sleep apnea in obese patients. Indian J
Otolaryngol Head Neck Surg. 76:5126–5132. 2024.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Turbati MS, Kindel TL and Higgins RM:
Identifying the optimal STOP-Bang screening score for obstructive
sleep apnea among bariatric surgery patients. Surg Obes Relat Dis.
20:1154–1162. 2024.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Mergen H, Altındağ B, Zeren Uçar Z and
Karasu Kılıçaslan I: The predictive performance of the STOP-bang
questionnaire in obstructive sleep apnea screening of obese
population at sleep clinical setting. Cureus.
11(e6498)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Sharma H: Statistical significance or
clinical significance? A researcher's dilemma for appropriate
interpretation of research results. Saudi J Anaesth. 15:431–434.
2021.PubMed/NCBI View Article : Google Scholar
|