Introduction
Prostate cancer (PCa) is the second leading cause of
cancer-associated mortalities worldwide and the most commonly
diagnosed cancer among men in 2025(1). Despite its high prevalence,
prostate-specific antigen (PSA) testing remains the most widely
used screening method due to its cost-effectiveness and
practicality (2). However, numerous
studies demonstrate that PSA levels can be influenced by various
non-cancer-associated factors, including benign prostatic
hyperplasia (3), prostatitis
(4), antibiotic use (5) and body mass index (BMI) (6). These confounding factors can lead to
diagnostic inaccuracies, increasing the risk of a false-positive or
-negative diagnosis, which may result in unnecessary or
inappropriate treatment (7).
Therefore, relying solely on PSA levels for the screening of PCa
presents notable challenges that warrant further investigation and
improvement (8).
Growing evidence suggests that immune inflammation
and nutritional status serve critical roles in the development and
progression of PCa (9,10). A previous study reveals a potential
association between abnormal immune-inflammatory responses,
nutritional imbalances and elevated serum PSA levels in men
(11). C-reactive protein (CRP), an
acute-phase reactant with levels that increase in response to acute
inflammation, infection or tissue damage, is linked to poor
clinical outcomes in patients with PCa (12). For example, a previous meta-analysis
demonstrates that increased CRP levels are notably associated with
a reduced overall survival (OS), cancer-specific survival and
progression-free survival (PFS) in patients with PCa (13). The systemic immune-inflammation
index (SII), which is calculated as: (Platelets x
neutrophils)/lymphocytes, serves as a simple yet effective
prognostic biomarker. Elevated pre-treatment SII values are
associated with reduced OS and PFS outcomes in patients with PCa
(14). Compared with normal
tissues, the levels of tumor necrosis factor are increased in
various tumors and are associated with inflammatory cell
infiltration and increased vascularization within the tumor
microenvironment (15). Other
inflammatory markers, such as the neutrophil-to-lymphocyte ratio
(NLR) and platelet-to-lymphocyte ratio (PLR), may also help
differentiate benign prostatic hyperplasia from PCa and serve as
potential diagnostic tools (16-18).
Serum albumin, a readily available and cost-effective indicator of
nutritional status, is also linked to PSA levels. It is reported
that lower serum albumin levels in middle-aged men are associated
with higher PSA concentrations (19). However, a cross-sectional analysis
reveals that a dietary protein intake of >181.8 g/day is
positively associated with elevated PSA levels (20).
Previous studies report associations between
individual inflammatory or nutritional markers (such as CRP,
albumin and NLR) and the PSA levels or prognosis of PCa (21-24).
However, to the best of our knowledge, the CRP-albumin-lymphocyte
(CALLY) index, a composite score integrating inflammation (such as
the CRP levels), nutritional status (such as the albumin levels)
and immunity (such as the lymphocyte count), is yet to be evaluated
in association with the PSA levels in a general population without
PCa (25). Previous retrospective
studies demonstrate that the CALLY index is an independent
prognostic factor of OS and PFS in various types of cancer,
including gastric (26),
non-small-cell lung (27),
colorectal cancer (28) and
hepatocellular carcinoma (29).
However, previous research on the association between the CALLY
index and PCa is limited. Accurate interpretation of PSA values,
accounting for potential confounding effects from subclinical
inflammation and nutritional status, is essential to increase the
reliability of the screening for PCa.
Therefore, using data from the 2003-2010 national
health and nutrition examination survey (NHANES) cycles, the
present study investigated the association between the CALLY index
and the PSA levels in a population of American men aged ≥40 years
without known prostate conditions.
Subjects and methods
Study description and population
A NHANES (https://www.cdc.gov/nchs/nhanes/) is a cross-sectional
study designed to assess the health and nutritional status of
adults and children in the United States of America and is
stipulated by a Code of Federal Regulations (45 CFR 46.101). It is
conducted by the National Center for Health Statistics (NCHS), a
part of the Centers for Disease Control and Prevention (CDC)
(30). All NHANES protocols were
approved by the NCHS research ethics review board, and written
informed consent was obtained from all participants. The present
study received an exemption of ethics approval from the Huai'an No.
1 People's Hospital institutional review board. The present study
involved a secondary analysis of NHANES data and adhered to the
reporting guidelines outlined in the strengthening the reporting of
observational studies in epidemiology statement for cross-sectional
studies.
The present study used data from four NHANES cycles
between 2003-2010 (https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2003;
https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2005;
https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2007;
https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2009),
as these were the only cycles that included comprehensive PSA
information. Participants were included if there was complete data
for PSA and all components of the CALLY index. The following
exclusion criteria were applied: i) Age, <40 years; ii) missing
data for PSA, CRP, albumin or lymphocyte counts; iii) missing
information regarding BMI, comorbidities, lifestyle factors or
education level; iv) conditions or treatments known to affect PSA
levels, including the use of 5-α reductase inhibitors, diagnosis of
benign prostatic hyperplasia or prostatitis, prostate biopsy within
the past week, urological surgery within the past month, or the
diagnosis of PCa.
Definitions of PSA and the CALLY
index
Serum samples were stored at 2-8˚C and analyzed by
Collaborative Laboratory Services LLC. Total PSA concentrations
were measured using the Hybritech method (31) and validated using a chemiluminescent
immunoassay platform with the Beckman Access®
Immunoassay System (Beckman Coulter, Inc.). Testing was carried out
according to standardized NHANES protocols (https://www.cdc.gov/nchs/nhanes/about/erb.html).
Each sample was analyzed once without replication. Rigorous quality
control procedures, including internal calibration and commercial
controls (bench quality controls; https://wwwn.cdc.gov/nchs/data/nhanes/public/2009/labmethods/PSA_F_met_complex.pdf),
were carried out to ensure measurement accuracy. PSA concentrations
were reported in ng/ml. A total of 5,320 serum samples from men
aged ≥40 years were included in the final analysis.
The CALLY index was calculated using the following
formula: CALLY index=[albumin concentration (g/l) x lymphocyte
count (109/l)]/[CRP concentration (mg/l) x 10]. CRP
concentrations were quantified using latex-enhanced nephelometry on
a Behring Nephelometer (Siemens Healthineers). Lymphocyte counts
were analyzed using the Beckman Coulter MAXM Instrument. Serum
albumin levels were measured using the Beckman Synchron LX20 and
Beckman UniCel DxC800 Synchron systems. Due to the skewed
distribution of the CALLY index, a logarithmic transformation was
applied prior to statistical analyses.
Covariates
A range of covariates that could influence the
association between the CALLY index and PSA levels were included in
the analysis. These covariates included demographic characteristics
(such as age, ethnicity, education level, BMI, smoking status and
alcohol consumption), laboratory indices [such as the levels of
blood urea nitrogen (mmol/l), cholesterol (mg/dl), glucose (mg/dl),
serum lactate dehydrogenase (LDH; U/l), total bilirubin (mg/dl),
triglycerides (mmol/l), serum uric acid (mg/dl), serum creatinine
(mg/dl), aspartate aminotransferase (U/l) and alanine
aminotransferase (U/l)] and clinical history (such as the presence
or absence of chronic diseases including hypertension, diabetes,
coronary artery disease, angina pectoris and history of neoplastic
diseases).
Statistical analysis
All statistical analyses were carried out using R
version 4.3 (https://www.r-project.org) and EmpowerStats version
2.0 (http://www.empowerstats.net/en/),
incorporating the complex sampling design of NHANES in accordance
with CDC analytical guidelines. Participants were stratified into
quartiles based on their CALLY index values: Q1, <1.91; Q2,
1.91-4.27; Q3, 4.28-9.68; and Q4, >9.68. Continuous variables
are presented as the mean ± standard deviation, while categorical
variables are presented as counts and percentages. Differences
between groups across CALLY quartiles were analyzed using one-way
analysis of variance with Tukey's honestly significant difference
post hoc test for continuous variables and Pearson's chi-square
test for categorical variables.
To investigate the association between the CALLY
index and PSA levels, both weighted univariate and multivariate
linear regression models were used, with β coefficients (β) and 95%
confidence intervals (CIs) reported. Three models were constructed:
i) Model 1 was unadjusted; ii) model 2 was adjusted for age,
ethnicity and BMI; and iii) model 3 was fully adjusted for a
comprehensive set of covariates selected based on biological
plausibility, prior literature and data availability in NHANES
(32). These variables may affect
the PSA levels and/or components of the CALLY index, including
comorbidities (such as the presence or absence of hypertension,
diabetes, coronary heart disease, angina, tumor history and BMI),
lifestyle factors (such as smoking status, alcohol intake, age,
ethnicity and level of education) and laboratory markers [such as
the levels of CRP, albumin, alanine aminotransferase (ALT),
aspartate aminotransferase (AST), cholesterol, bilirubin,
triglycerides, monocytes, neutrophils, platelets, creatinine, LDH,
uric acid and glucose]. Variables such as globulin, testosterone
and physical activity were not included due to incomplete data,
limited availability across NHANES cycles and lack of consistent
associations with PSA or CALLY components in the population without
cancer.
To investigate potential non-linear associations,
restricted cubic spline (RCS) regression was used. Additionally,
subgroup analyses were conducted to assess whether the association
between the CALLY index and PSA varied by demographic or clinical
characteristics. P<0.05 was considered to indicate a
statistically significant difference.
Results
Baseline characteristics of
participants
The present study initially included 41,156
participants. However, a number of participants were excluded due
to incomplete information on key variables. Specifically,
exclusions were made due to missing data regarding PSA levels
(n=35,138), factors known to influence PSA levels (n=232), albumin
levels (n=11), CRP levels (n=1), lymphocyte counts (n=29), BMI
(n=86), chronic health conditions or tumor history (n=21),
education level (n=1) and alcohol consumption history (n=265).
After applying these criteria, a total of 5,320 eligible
participants were included in the final analysis. The mean age of
participants was 59.44±12.51 years. Participants were divided into
quartiles based on their CALLY index values (Q1-Q4, Table I). The mean total serum PSA level
was 1.82±3.20, with a statistically significant decreasing trend
observed across increasing CALLY quartiles. Compared with
participants with low CALLY index values, those with increased
values tended to be younger and had lower levels of blood glucose,
uric acid, LDH, creatinine, globulin and BMI as well as reduced
counts of monocytes, neutrophils and platelets. Additionally,
compared with participants with low CALLY index values, those with
increased values were associated with a reduced prevalence of
hypertension, diabetes, coronary heart disease, history of cancer
and cigarette smoking. However, no significant differences were
observed in the levels of ALT, AST, alcohol consumption or
incidence of angina.
 | Table IBaseline characteristics of
participants sorted by CALLY index quartiles (n=5,320). |
Table I
Baseline characteristics of
participants sorted by CALLY index quartiles (n=5,320).
| | CALLY index
quartiles | |
|---|
| Variables | Total
(n=5,320) | 1 (n=1,330) | 2 (n=1,330) | 3 (n=1,328) | 4 (n=1,332) | Statistic | P-value |
|---|
| ALTa | 28.61±20.66 | 27.63±29.14 | 29.15±18.23 | 29.40±17.38 | 28.25±14.92 | F=2.07 | 0.102 |
| ASTa | 28.02±15.39 | 28.19±19.94 | 28.03±14.49 | 27.78±12.65 | 28.10±13.42 | F=0.17 | 0.916 |
|
Cholesterola | 5.13±1.10 | 5.00±1.11 | 5.16±1.13 | 5.23±1.10 | 5.12±1.04 | F=10.13 | <0.001 |
|
Glucosea | 5.98±2.31 | 6.41±2.78 | 6.02±2.39 | 5.79±1.95 | 5.71±1.94 | F=24.86 | <0.001 |
| Lactate
dehydrogenasea | 133.87±33.42 | 139.33±45.50 | 134.20±31.79 | 132.10±26.05 | 129.84±25.73 | F=19.68 | <0.001 |
|
Bilirubina | 14.25±5.21 | 13.65±5.28 | 14.11±5.04 | 14.49±5.34 | 14.76±5.10 | F=11.61 | <0.001 |
|
Triglyceridesa | 1.95±1.49 | 1.82±1.24 | 2.06±1.57 | 2.04±1.64 | 1.87±1.47 | F=8.31 | <0.001 |
| Uric
acida | 362.14±80.04 | 378.38±91.79 | 369.99±77.30 | 356.53±72.61 | 343.72±72.57 | F=49.52 | <0.001 |
|
Creatininea | 94.10±48.59 | 101.14±65.41 | 94.58±42.21 | 90.45±34.83 | 90.22±45.77 | F=14.81 | <0.001 |
|
Globulina | 29.36±4.97 | 31.29±5.82 | 29.38±4.64 | 28.84±4.39 | 27.92±4.26 | F=116.29 | <0.001 |
| PSAa | 1.82±3.20 | 2.10±3.97 | 1.93±3.29 | 1.64±2.64 | 1.62±2.73 | F=7.14 | <0.001 |
|
Monocytea | 0.58±0.20 | 0.60±0.23 | 0.58±0.19 | 0.57±0.18 | 0.56±0.21 | F=13.29 | <0.001 |
|
Neutrophila | 4.30±2.14 | 4.85±2.87 | 4.37±2.31 | 4.14±1.52 | 3.83±1.38 | F=55.64 | <0.001 |
| Age,
yearsa | 59.44±12.51 | 62.37±12.54 | 59.98±12.52 | 58.20±12.29 | 57.20±12.07 | F=44.97 | <0.001 |
|
Plateleta | 238.90±63.85 | 246.41±75.68 | 238.10±58.52 | 237.64±61.65 | 233.48±57.26 | F=9.62 | <0.001 |
| BMIa | 28.87±5.68 | 30.49±7.08 | 29.69±5.35 | 28.53±4.92 | 26.77±4.29 | F=114.48 | <0.001 |
| Ethnicity, N
(%) | | | | | | χ²=42.50 | <0.001 |
|
Non-Hispanic
White | 935 (17.58) | 192 (14.44) | 247 (18.57) | 255 (19.20) | 241 (18.09) | | |
|
Non-Hispanic
Black | 342 (6.43) | 67 (5.04) | 92 (6.92) | 96 (7.23) | 87 (6.53) | | |
|
Mexican
American | 2,923 (54.94) | 749 (56.32) | 724 (54.44) | 724 (54.52) | 726 (54.50) | | |
|
Other
ethnicity | 949 (17.84) | 288 (21.65) | 234 (17.59) | 207 (15.59) | 220 (16.52) | | |
|
Other
Hispanic ethnicity | 171 (3.21) | 34 (2.56) | 33 (2.48) | 46 (3.46) | 58 (4.35) | | |
| Education level, N
(%) | | | | | | χ²=46.63 | <0.001 |
|
<9th
grade | 855 (16.07) | 231 (17.37) | 224 (16.84) | 210 (15.81) | 190 (14.26) | | |
|
9-11th
grade | 767 (14.42) | 214 (16.09) | 186 (13.98) | 195 (14.68) | 172 (12.91) | | |
|
High school
grade | 1,255 (23.59) | 329 (24.74) | 324 (24.36) | 323 (24.32) | 279 (20.95) | | |
|
University
attendance or associate of arts degree | 1,307 (24.57) | 324 (24.36) | 334 (25.11) | 318 (23.95) | 331 (24.85) | | |
|
University
graduate or postgraduate education | 1,136 (21.35) | 232 (17.44) | 262 (19.70) | 282 (21.23) | 360 (27.03) | | |
| Alcohol use, N | | | | | | χ²=4.94 | 0.176 |
|
(%) | | | | | | | |
|
Yes | 4,375 (82.24) | 1,092 (82.11) | 1,070 (80.45) | 1,099 (82.76) | 1,114 (83.63) | | |
|
No | 945 (17.76) | 238 (17.89) | 260 (19.55) | 229 (17.24) | 218 (16.37) | | |
| Hypertension, N
(%) | | | | | | χ²=99.76 | <0.001 |
|
Yes | 2,352 (44.21) | 715 (53.76) | 615 (46.24) | 555 (41.79) | 467 (35.06) | | |
|
No | 2,968 (55.79) | 615 (46.24) | 715 (53.76) | 773 (58.21) | 865 (64.94) | | |
| Diabetes, N
(%) | | | | | | χ²=26.44 | <0.001 |
|
Yes | 845 (15.88) | 263 (19.77) | 202 (15.19) | 193 (14.53) | 187 (14.04) | | |
|
No | 4,344 (81.65) | 1,025 (77.07) | 1,095 (82.33) | 1,109 (83.51) | 1,115 (83.71) | | |
|
Borderline | 131 (2.46) | 42 (3.16) | 33 (2.48) | 26 (1.96) | 30 (2.25) | | |
| Coronary heart
disease, N (%) | | | | | | χ²=26.48 | <0.001 |
|
Yes | 471 (8.85) | 150 (11.28) | 138 (10.38) | 94 (7.08) | 89 (6.68) | | |
|
No | 4,849 (91.15) | 1,180 (88.72) | 1,192 (89.62) | 1,234 (92.92) | 1,243 (93.32) | | |
| Angina, N (%) | | | | | | χ²=5.98 | 0.113 |
|
Yes | 245 (4.61) | 77 (5.79) | 59 (4.44) | 56 (4.22) | 53 (3.98) | | |
|
No | 5,075 (95.39) | 1,253 (94.21) | 1,271 (95.56) | 1,272 (95.78) | 1,279 (96.02) | | |
| Tumor history, N
(%) | | | | | | χ²=16.24 | 0.001 |
|
Yes | 461 (8.67) | 151 (11.35) | 105 (7.89) | 103 (7.76) | 102 (7.66) | | |
|
No | 4,859 (91.33) | 1,179 (88.65) | 1,225 (92.11) | 1,225 (92.24) | 1,230 (92.34) | | |
| Smoking status, N
(%) | | | | | | χ²=38.25 | <0.001 |
|
Yes | 3,295 (61.94) | 903 (67.89) | 843 (63.38) | 789 (59.41) | 760 (57.06) | | |
|
No | 2,025 (38.06) | 427 (32.11) | 487 (36.62) | 539 (40.59) | 572 (42.94) | | |
Association between the CALLY index
and PSA levels
In the unadjusted model (model 1), there was a
significant inverse association between the CALLY index and serum
total PSA. Each one-unit increase in the CALLY index corresponded
to a 0.17 ng/ml decrease in the PSA levels (β=-0.17; 95% CI, -0.24
to -0.10). Sensitivity analysis using CALLY quartiles revealed that
participants in Q4 had a 48% reduced PSA level compared with those
in Q1 (β=-0.48; 95% CI, -0.73 to -0.24). In model 2, which was
adjusted for age, ethnicity and BMI, each one-unit increase in the
CALLY index corresponded to a 0.10 ng/ml decrease in the PSA levels
(β=-0.10; 95% CI, -0.17 to -0.03). In a fully adjusted model, model
3, controlling for all relevant covariates, the association
remained significant in which PSA levels decreased by 0.09 ng/ml
for each one-unit increase in the CALLY index (β=-0.09; 95% CI,
-0.16 to -0.02) (Table II).
 | Table IIAssociations between the CALLY index
and serum prostate-specific antigen levels across three regression
models. |
Table II
Associations between the CALLY index
and serum prostate-specific antigen levels across three regression
models.
| | Models |
|---|
| | 1 | 2 | 3 |
|---|
| CALLY index | β (95% CI) | P-value | β (95% CI) | P-value | β (95% CI) | P-value |
|---|
|
Continuousa | -0.17
(-0.24-0.10) | <0.001 | -0.10
(-0.17-0.03) | 0.006 | -0.09
(-0.16-0.02) | 0.017 |
| Quartiles | | | | | | |
|
1 | Reference | - | Reference | - | Reference | - |
|
2 | -0.18
(-0.42-0.07) | 0.156 | -0.03
(-0.27-0.20) | 0.795 | -0.01
(-0.25-0.22) | 0.903 |
|
3 | -0.46
(-0.71-0.22) | <0.001 | -0.22
(-0.46-0.01) | 0.065 | -0.20
(-0.45-0.04) | 0.105 |
|
4 | -0.48
(-0.73-0.24) | <0.001 | -0.23
(-0.47-0.01) | 0.066 | -0.20
(-0.45-0.06) | 0.126 |
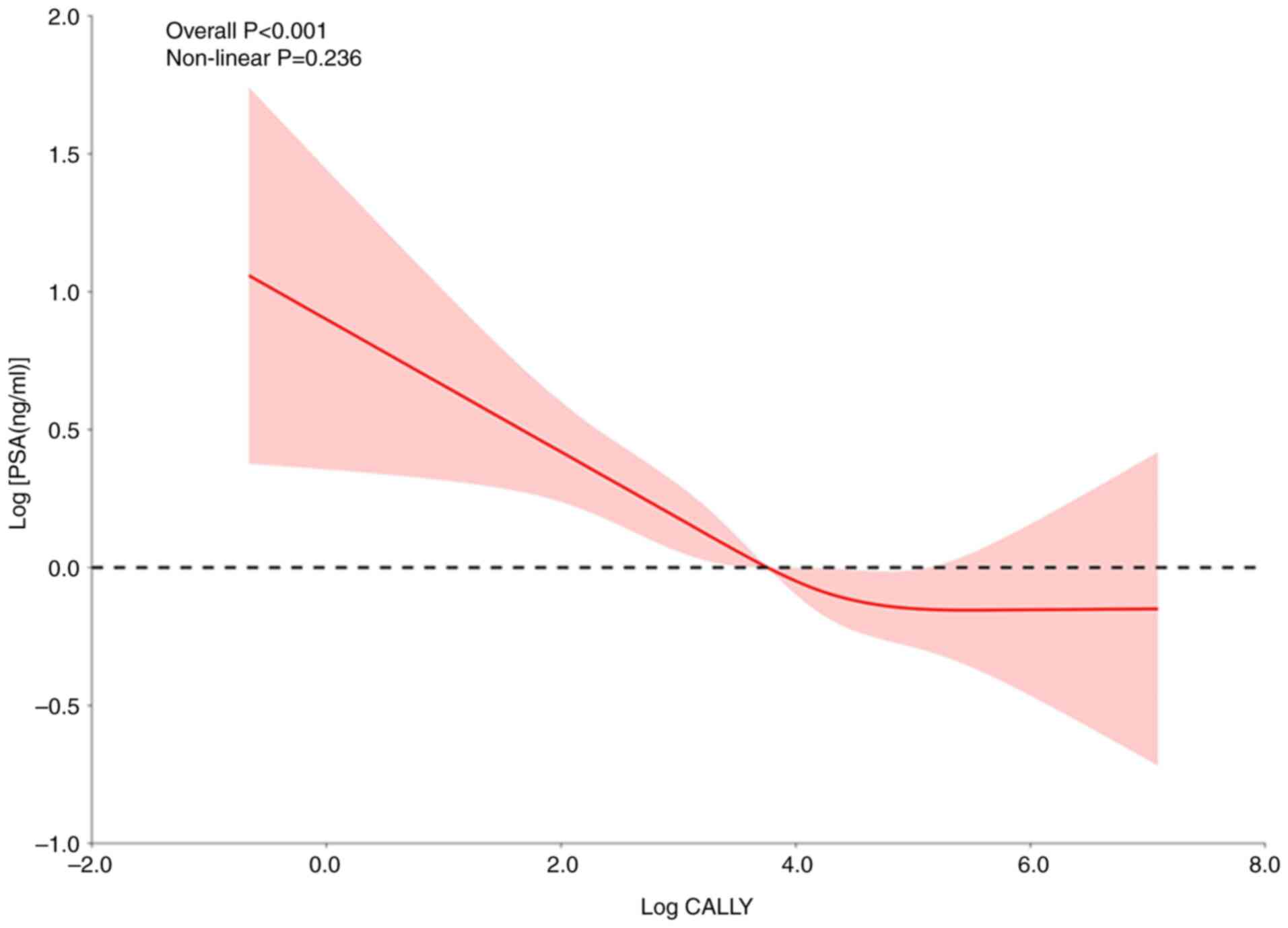
There is not a non-linear association
between CALLY index and PSA
Due to the skewed distribution of PSA and CALLY
index values, both variables were log-transformed to achieve
normality prior to modeling. The RCS regression was then performed
using the fully adjusted model (model 3) to assess potential
non-linear associations. The results indicated that there was no
significant evidence of a non-linear association between the
log-transformed CALLY index and PSA levels (Fig. 1).
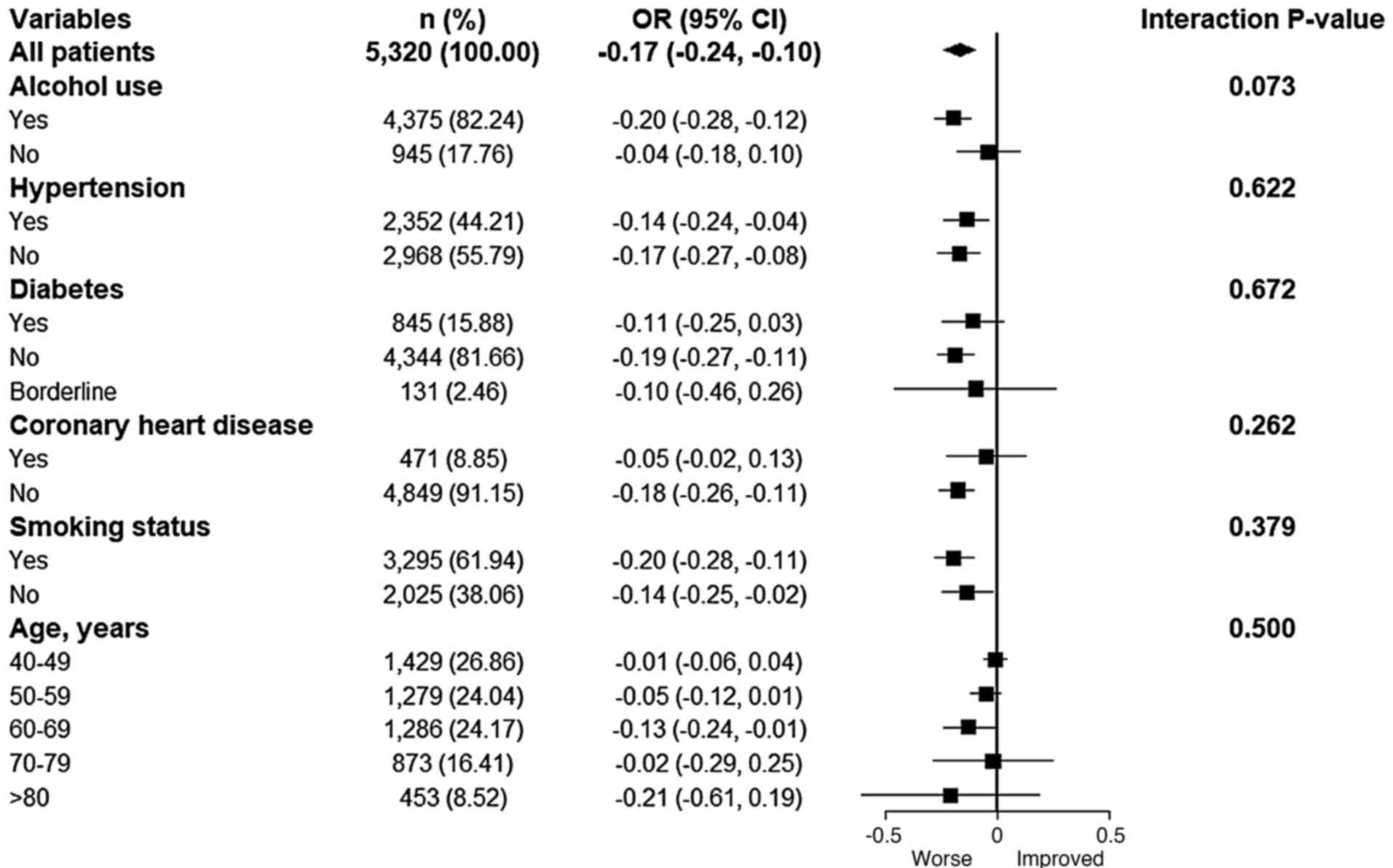
Subgroup analysis
To assess the consistency of the association across
various subpopulations, subgroup analyses were carried out after
the population was stratified by age, smoking status, alcohol
consumption, and the presence or absence of hypertension, diabetes
and coronary heart disease. As shown in Fig. 2, interaction tests did not yield
statistically significant results, indicating that the inverse
association between the CALLY index and PSA levels was not
significantly modified by any of the stratified variables tested.
Therefore, this suggested that the observed association was robust
across different demographic and clinical subgroups.
Discussion
The present study was, to the best of our knowledge,
the first to investigate the association between the CALLY index
and PSA levels in a population without PCa in the United States of
America. Using cross-sectional data from 5,320 participants in the
NHANES database, the present study identified a significant linear
association between the CALLY index and PSA concentrations, with
PSA levels decreasing as the CALLY index increased. Furthermore,
this inverse association was consistent across multiple subgroups,
including those stratified by age, smoking status, alcohol
consumption, hypertension, diabetes and coronary heart disease.
Specifically, each one-unit increase in the CALLY index was
associated with a 0.09 ng/ml reduction in the PSA levels. Although
the association between increased CALLY index values and reduced
PSA levels was statistically significant, the absolute effect size
was relatively small and may have limited clinical impact at the
individual level. However, in population-level screening, even
modest reductions in PSA, particularly when consistently observed,
may contribute to increased specificity and help mitigate
overdiagnosis due to subclinical inflammation. Sensitivity analyses
confirmed the robustness of this association, supporting its
reliability and validity. These findings suggest that an increased
CALLY index may serve as an independent predictor of reduced PSA
levels.
The CALLY index, calculated from levels of CRP,
serum albumin and lymphocyte counts, represents a composite
indicator of systemic inflammation, nutritional status and immune
function (33). It is used as a
prognostic biomarker in various malignancies of the digestive
system such as gastric and colorectal cancer. Previous studies
demonstrate that a reduced CALLY index score is associated with a
reduced OS in patients with non-small cell lung cancer (34), gastric cancer (35), esophageal cancer (36), breast cancer (37) and renal cell carcinoma (38). In addition, data from NHANES
indicates that, compared with reduced CALLY indices, an increased
CALLY index is associated with a reduced risk of all-cause and
cause-specific mortality in patients with cancer (39). Specifically, after comprehensive
adjustment for variables (such as sex, age, ethnicity, poverty
income ratio, smoking status, alcohol consumption, BMI, total
cholesterol, ALT, serum creatinine, serum total bilirubin, types of
cancer, prevalences of diabetes mellitus, cardiovascular disease,
chronic kidney disease and hypertension), each one-unit increase in
the natural logarithm of the CALLY index was associated with an 18%
reduction in the risk of all-cause mortality among cancer patients
(39). However, the association
between the CALLY index and PCa is yet to be elucidated.
The present study identified a negative association
between the CALLY index and PSA levels. Although, to the best of
our knowledge, this specific association has not been previously
reported, previous studies examine the individual components of the
CALLY index in association with PSA levels and PCa. For example, a
previous study reveals a non-linear association between serum
albumin and PSA levels, highlighting an inverse association when
albumin concentrations exceed 41 g/l (21). Furthermore, a previous study by Gao
et al (32) reveals that
among men >40 years of age without prostate diseases, the
albumin-globulin ratio (AGR) demonstrates a non-linear association
with PSA, with a negative association when the AGR is <1.32. Low
levels of serum albumin also act as a prognostic factor in patients
with metastatic castration-resistant prostate cancer (mCRPC)
(22). Elevated CALLY index values
are inversely associated with serum LDH levels, which is a
clinically notable finding since increased LDH activity indicates
enhanced tumor glycolysis, angiogenesis and cellular proliferation,
and is an adverse prognostic biomarker across multiple
malignancies, including PCa (40).
Inflammation serves a critical role in the
development and progression of cancer, prompting investigations
into the prognostic relevance of elevated CRP levels in various
malignancies, including PCa (41).
A prospective population-based cohort study by Stikbakke et
al demonstrates that, compared with low serum CRP levels, high
serum CRP levels are associated with an increased risk of PCa and
have a reduced prognosis (23).
Furthermore, two meta-analyses confirm that CRP is a strong
predictor of adverse outcomes in PCa, including in patients with
mCRPC (42,43). Elevated CRP is also associated with
PSA levels in populations with cancer (44). As an acute-phase protein, CRP can
suppress albumin synthesis and promote prostatic epithelial cell
apoptosis through cytokine-mediated pathways (such as the IL-6 and
TNF pathways), which may reduce the secretion of PSA (45). Inflammatory markers demonstrate
strong associations with PSA levels and PCa outcomes (46). NLR, a marker of systemic
inflammation, has prognostic value in PCa (47). Elevated NLR and total PSA levels are
notably associated with increased Gleason scores (≥7) (24). Furthermore, PLR is an independent
prognostic indicator for both PFS and OS in patients with PCa
(48) and can be used to
distinguish benign prostatic hyperplasia from PCa (49). Lymphocyte-mediated mechanisms may
also influence PSA expression levels. The secretion of interferon-γ
by infiltrating lymphocytes may suppress androgen receptor
activity, which reduces the transcription of PSA (50). Although numerous studies demonstrate
the prognostic value of systemic inflammatory markers such as NLR
and PLR in PCa, it is important to acknowledge their non-specific
nature (46-50).
These ratios may be influenced by a wide range of conditions that
are not associated with malignancy, including infections (such as
pancreatitis and pulmonary infection) (51,52),
autoimmune diseases (such as systemic lupus erythematosus)
(53), trauma (such as traumatic
brain injury) (54) and metabolic
disorders (such as diabetes) (55).
This non-specificity limits their utility as standalone indicators
for PCa screening or prognosis. The findings of the present study
suggested that the CALLY index, as a composite marker, potentially
reflected these complex interactions. One potential mechanism is
that the CALLY index captures a systemic immune state that is
characterized by a Th1/Th2 balance that is skewed toward an
anti-inflammatory profile (56).
Although, to the best of our knowledge, there are not any direct
studies on the impact of the CALLY index on the Th1/Th2 balance,
the findings of the present study suggested that CRP, albumin and
lymphocyte levels individually influenced the Th1/Th2 balance. The
Th1/Th2 balance may skew toward an anti-inflammatory (Th2-dominant)
profile due to chronic infections, allergies, immunosuppressive
cytokines (such as IL-10 and TGF-β), hormonal influences, aging,
diet or environmental factors, which may suppress the
proinflammatory Th1 responses (57). This immune milieu may inhibit the
recruitment of tumor-associated macrophages (58), which reduces the passive diffusion
of PSA from the prostate stroma into the bloodstream (59). The recruitment of tumor-associated
macrophages does not directly induce passive PSA diffusion but
creates a permissive microenvironment (via inflammation, ECM
breakdown and vascular leakiness) that enhances PSA entry into
circulation. This aligns with observations that aggressive tumors
often show higher serum PSA levels (60).
However, the present study had a number of
limitations. Firstly, due to the cross-sectional design, causal
associations between the CALLY index and PSA levels cannot be
established. Therefore, prospective cohort studies should be
carried out in the future in order to validate the findings of the
present study. Secondly, PSA measurements in NHANES were carried
out using the Hybritech method, which differs systematically from
the World Health Organization (WHO)-standardized methods used in a
number of clinical laboratories (61). The Hybritech PSA assay uses
proprietary monoclonal antibodies and an in-house calibration
standard, which yields values 20-30% higher compared with the
WHO-calibrated methods. The WHO methods use polyclonal antibodies
and the WHO International Standard (code, 96/670) (62). This discrepancy may introduce
variability and limit the generalizability of the present results.
Thirdly, a number of laboratory variables, such as globulin and
testosterone levels, as well as lifestyle-associated factors
including the dietary inflammatory index and physical activity,
were not included in the present analysis due to incomplete data,
limited availability across NHANES cycles and a lack of consistent
associations with PSA or CALLY components in the population without
cancer. The omission of these variables may result in an
underestimation of the true association between the CALLY index and
PSA levels.
In conclusion, PSA, the primary biomarker for PCa
screening, is criticized for its limited diagnostic specificity,
which contributes to the ongoing clinical challenges. The present
study, to the best of our knowledge, was the first to reveal a
negative association between PSA levels and the CALLY index, a
composite marker reflecting inflammation, immunity and nutritional
status. The present findings provided an insight into the potential
biological contributors of PSA variability, which may provide
guidance to future research regarding strategies for reducing false
positives in PSA screening. However, due to the cross-sectional
design of the present study, the observed association does not
imply a causal association, nor does it support the immediate
clinical use of the CALLY index as a diagnostic adjunct.
Prospective and mechanistic studies are required to validate the
findings of the present study and investigate the implications for
PCa screening strategies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JH contributed to the conception and the design of
the present study. JH, NX and MF contributed to the acquisition,
analysis and interpretation of the data. JH, NX and MF contributed
to drafting the manuscript or revising the manuscript. JH, NX and
MF read and approved the final version of the manuscript. JH, NX
and MF confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Kratzer TB, Giaquinto AN, Sung
H and Jemal A: Cancer statistics, 2025. CA Cancer J Clin. 75:10–45.
2025.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Van Poppel H, Roobol MJ, Chapple CR, Catto
JWF, N'Dow J, Sønksen J, Stenzl A and Wirth M: Prostate-specific
antigen testing as part of a risk-adapted early detection strategy
for prostate cancer: European association of urology position and
recommendations for 2021. Eur Urol. 80:703–711. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gudmundsson J, Sigurdsson JK,
Stefansdottir L, Agnarsson BA, Isaksson HJ, Stefansson OA,
Gudjonsson SA, Gudbjartsson DF, Masson G, Frigge ML, et al:
Genome-wide associations for benign prostatic hyperplasia reveal a
genetic correlation with serum levels of PSA. Nat Commun.
9(4568)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lokant MT and Naz RK: Presence of PSA
auto-antibodies in men with prostate abnormalities (prostate
cancer/benign prostatic hyperplasia/prostatitis). Andrologia.
47:328–332. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Buddingh KT, Maatje MGF, Putter H, Kropman
RF and Pelger RCM: Do antibiotics decrease prostate-specific
antigen levels and reduce the need for prostate biopsy in type IV
prostatitis? A systematic literature review. Can Urol Assoc J.
12:E25–E30. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhao Y, Zhang Y, Wang X, Lin D and Chen Z:
Relationship between body mass index and concentrations of prostate
specific antigen: A cross-sectional study. Scand J Clin Lab Invest.
80:162–167. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tan GH, Nason G, Ajib K, Woon DTS,
Herrera-Caceres J, Alhunaidi O and Perlis N: Smarter screening for
prostate cancer. World J Urol. 37:991–999. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Misra-Hebert AD, Hu B, Klein EA,
Stephenson A, Taksler GB, Kattan MW and Rothberg MB: Prostate
cancer screening practices in a large, integrated health system:
2007-2014. BJU Int. 120:257–264. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zaffaroni M, Vincini MG, Corrao G,
Lorubbio C, Repetti I, Mastroleo F, Putzu C, Villa R, Netti S,
D'Ecclesiis O, et al: Investigating nutritional and inflammatory
status as predictive biomarkers in oligoreccurent prostate cancer-A
RADIOSA trial preliminary analysis. Nutrients.
15(4583)2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jurisic V: Multiomic analysis of cytokines
in immuno-oncology. Expert Rev Proteomics. 17:663–674.
2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tang Z, Li S, Zeng M, Zeng L and Tang Z:
The association between systemic immune-inflammation index and
prostate-specific antigen: Results from NHANES 2003-2010. PLoS One.
19(e0313080)2024.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Beer TM, Lalani AS, Lee S, Mori M, Eilers
KM, Curd JG, Henner WD, Ryan CW, Venner P, Ruether JD, et al:
C-reactive protein as a prognostic marker for men with
androgen-independent prostate cancer: results from the ASCENT
trial. Cancer. 112:2377–2383. 2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Liao DW, Hu X, Wang Y, Yang ZQ and Li X:
C-reactive protein is a predictor of prognosis of prostate cancer:
A systematic review and meta-analysis. Ann Clin Lab Sci.
50:161–171. 2020.PubMed/NCBI
|
|
14
|
Rajwa P, Schuettfort VM, D'Andrea D, Quhal
F, Mori K, Katayama S, Laukhtina E, Pradere B, Motlagh RS,
Mostafaei H, et al: Impact of systemic Immune-inflammation Index on
oncologic outcomes in patients treated with radical prostatectomy
for clinically nonmetastatic prostate cancer. Urol Oncol. 39:785
e19–785 e27. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jurisic V, Terzic T, Colic S and Jurisic
M: The concentration of TNF-alpha correlate with number of
inflammatory cells and degree of vascularization in radicular
cysts. Oral Dis. 14:600–605. 2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cui S, Cao S, Chen Q, He Q and Lang R:
Preoperative systemic inflammatory response index predicts the
prognosis of patients with hepatocellular carcinoma after liver
transplantation. Front Immunol. 14(1118053)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sawada R, Akiyoshi T, Kitagawa Y, Hiyoshi
Y, Mukai T, Nagasaki T, Yamaguchi T, Konishi T, Yamamoto N, Ueno M
and Fukunaga Y: Systemic inflammatory markers combined with
tumor-infiltrating lymphocyte density for the improved prediction
of response to neoadjuvant chemoradiotherapy in rectal cancer. Ann
Surg Oncol. 28:6189–6198. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sun Z, Ju Y, Han F, Sun X and Wang F:
Clinical implications of pretreatment inflammatory biomarkers as
independent prognostic indicators in prostate cancer. J Clin Lab
Anal. 32(e22277)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Lin HY, Zhu X, Aucoin AJ, Fu Q, Park JY
and Tseng TS: Dietary and serum antioxidants associated with
prostate-specific antigen for middle-aged and older men. Nutrients.
15(3298)2023.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Song J, Chen C, He S, Chen W, Su J, Yuan
D, Sun F and Zhu J: Is there a non-linear relationship between
dietary protein intake and prostate-specific antigen: Proof from
the national health and nutrition examination survey (2003-2010).
Lipids Health Dis. 19(82)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Xu K, Yan Y, Cheng C, Li S, Liao Y, Zeng
J, Chen Z and Zhou J: The relationship between serum albumin and
prostate-specific antigen: A analysis of the National Health and
Nutrition Examination Survey, 2003-2010. Front Public Health.
11(1078280)2023.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fan L, Chi C, Guo S, Wang Y, Cai W, Shao
X, Xu F, Pan J, Zhu Y, Shangguan X, et al: Serum pre-albumin
predicts the clinical outcome in metastatic castration-resistant
prostate cancer patients treated with abiraterone. J Cancer.
8:3448–3455. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Stikbakke E, Richardsen E, Knutsen T,
Wilsgaard T, Giovannucci EL, McTiernan A, Eggen AE, Haugnes HS and
Thune I: Inflammatory serum markers and risk and severity of
prostate cancer: The PROCA-life study. Int J Cancer. 147:84–92.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Rulando M, Siregar GP and Warli SM:
Correlation between neutrophil-to-lymphocyte ratio with Gleason
score in patients with prostate cancer at Adam Malik Hospital Medan
2013-2015. Urol Ann. 13:53–55. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Müller L, Hahn F, Mähringer-Kunz A, Stoehr
F, Gairing SJ, Michel M, Foerster F, Weinmann A, Galle PR, Mittler
J, et al: Immunonutritive scoring for patients with hepatocellular
carcinoma undergoing transarterial chemoembolization: Evaluation of
the CALLY Index. Cancers (Basel). 13(5018)2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Hashimoto I, Tanabe M, Onuma S, Morita J,
Nagasawa S, Maezawa Y, Kanematsu K, Aoyama T, Yamada T, Yukawa N,
et al: Clinical impact of the C-reactive protein-albumin-lymphocyte
index in post-gastrectomy patients with gastric cancer. In Vivo.
38:911–916. 2024.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Liu XY, Zhang X, Zhang Q, Ruan GT, Liu T,
Xie HL, Ge YZ, Song MM, Deng L and Shi HP: The value of
CRP-albumin-lymphocyte index (CALLY index) as a prognostic
biomarker in patients with non-small cell lung cancer. Support Care
Cancer. 31(533)2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Takeda Y, Sugano H, Okamoto A, Nakano T,
Shimoyama Y, Takada N, Imaizumi Y, Ohkuma M, Kosuge M and Eto K:
Prognostic usefulness of the C-reactive protein-albumin-lymphocyte
(CALLY) index as a novel biomarker in patients undergoing
colorectal cancer surgery. Asian J Surg. 47:3492–3498.
2024.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Iida H, Tani M, Komeda K, Nomi T,
Matsushima H, Tanaka S, Ueno M, Nakai T, Maehira H, Mori H, et al:
Superiority of CRP-albumin-lymphocyte index (CALLY index) as a
non-invasive prognostic biomarker after hepatectomy for
hepatocellular carcinoma. HPB (Oxford). 24:101–115. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Nazzal Z, Khatib B, Al-Quqa B, Abu-Taha L
and Jaradat A: The prevalence and risk factors of urinary
incontinence among women with type 2 diabetes in the North West
Bank: A cross-sectional study. Lancet. 398 (Suppl
1)(S42)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Laffin RJ, Chan DW, Tanasijevic MJ,
Fischer GA, Markus W, Miller J, Matarrese P, Sokoll LJ, Bruzek DJ,
Eneman J, et al: Hybritech total and free prostate-specific antigen
assays developed for the Beckman Coulter access automated
chemiluminescent immunoassay system: A multicenter evaluation of
analytical performance. Clin Chem. 47:129–132. 2001.PubMed/NCBI
|
|
32
|
Gao S, Li S, Wu B, Wang J, Ding S and Tang
Z: Relationship between albumin-globulin ratio and
prostate-specific antigen: A cross-sectional study based on NHANES
2003-2010. BMC Urol. 25(3)2025.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Wang W, Gu J, Liu Y, Liu X, Jiang L, Wu C
and Liu J: Pre-treatment CRP-albumin-lymphocyte index (CALLY Index)
as a prognostic biomarker of survival in patients with epithelial
ovarian cancer. Cancer Manag Res. 14:2803–2812. 2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Cheng H, Ma J, Zhao F, Liu Y, Wu J, Wu T,
Li H, Zhang B, Liu H, Fu J, et al: IINS Vs CALLY index: A battle of
prognostic value in NSCLC patients following surgery. J Inflamm
Res. 18:493–503. 2025.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zhang H, Shi J, Xie H, Liu X, Ruan G, Lin
S, Ge Y, Liu C, Chen Y, Zheng X, et al: Superiority of
CRP-albumin-lymphocyte index as a prognostic biomarker for patients
with gastric cancer. Nutrition. 116(112191)2023.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Ma R, Okugawa Y, Shimura T, Yamashita S,
Sato Y, Yin C, Uratani R, Kitajima T, Imaoka H, Kawamura M, et al:
Clinical implications of C-reactive protein-albumin-lymphocyte
(CALLY) index in patients with esophageal cancer. Surg Oncol.
53(102044)2024.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Zhuang J, Wang S, Wang Y, Wu Y and Hu R:
Prognostic value of CRP-Albumin-lymphocyte (CALLY) index in
patients undergoing surgery for breast cancer. Int J Gen Med.
17:997–1005. 2024.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Hirata H, Fujii N, Oka S, Nakamura K,
Shimizu K, Kobayashi K, Hiroyoshi T, Isoyama N and Shiraishi K:
C-reactive protein-albumin-lymphocyte index as a novel biomarker
for progression in patients undergoing surgery for renal cancer.
Cancer Diagn Progn. 4:748–753. 2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Zhu D, Lin YD, Yao YZ, Qi XJ, Qian K and
Lin LZ: Negative association of C-reactive
protein-albumin-lymphocyte index (CALLY index) with all-cause and
cause-specific mortality in patients with cancer: Results from
NHANES 1999-2018. BMC Cancer. 24(1499)2024.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Jurisic V, Radenkovic S and Konjevic G:
The actual role of LDH as tumor marker, biochemical and clinical
aspects. Adv Exp Med Biol. 867:115–124. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Graff JN, Beer TM, Liu B, Sonpavde G and
Taioli E: Pooled analysis of C-reactive protein levels and
mortality in prostate cancer patients. Clin Genitourin Cancer.
13:e217–e221. 2015.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Naik G, Morgan C, Rocha P, Templeton A,
Pond G and Sonpavde G: Prognostic impact of C-reactive protein
(CRP) in metastatic prostate cancer (MPC): A systematic review and
meta-analysis. J Clin Oncol. 32(43)2014.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Zhou K, Li C, Chen T, Zhang X and Ma B:
C-reactive protein levels could be a prognosis predictor of
prostate cancer: A meta-analysis. Front Endocrinol (Lausanne).
14(1111277)2023.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Santotoribio JD and Jimenez-Romero ME:
Serum biomarkers of inflammation for diagnosis of prostate cancer
in patients with nonspecific elevations of serum prostate specific
antigen levels. Transl Cancer Res. 8:273–278. 2019.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Lehrer S, Diamond EJ, Mamkine B, Droller
MJ, Stone NN and Stock RG: C-reactive protein is significantly
associated with prostate-specific antigen and metastatic disease in
prostate cancer. BJU Int. 95:961–962. 2005.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Nepal SP, Nakasato T, Fukagai T, Ogawa Y,
Nakagami Y, Shichijo T, Morita J, Maeda Y, Oshinomi K, Unoki T, et
al: Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios
alone or combined with prostate-specific antigen for the diagnosis
of prostate cancer and clinically significant prostate cancer.
Asian J Urol. 10:158–165. 2023.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Yin X, Xiao Y, Li F, Qi S, Yin Z and Gao
J: Prognostic role of neutrophil-to-lymphocyte ratio in prostate
cancer: A systematic review and meta-analysis. Medicine
(Baltimore). 95(e2544)2016.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Salciccia S, Frisenda M, Bevilacqua G,
Viscuso P, Casale P, De Berardinis E, Di Pierro GB, Cattarino S,
Giorgino G, Rosati D, et al: Prognostic role of
platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in
patients with non-metastatic and metastatic prostate cancer: A
meta-analysis and systematic review. Asian J Urol. 11:191–207.
2024.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Yuksel OH, Urkmez A, Akan S, Yldirim C and
Verit A: Predictive value of the platelet-to-lymphocyte ratio in
diagnosis of prostate cancer. Asian Pac J Cancer Prev.
16:6407–6412. 2015.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Kwon YS, Han CS, Yu JW, Kim S, Modi P,
Davis R, Park JH, Lee P, Ha YS, Kim WJ and Kim IY: Neutrophil and
lymphocyte counts as clinical markers for stratifying low-risk
prostate cancer. Clin Genitourin Cancer. 14:e1–e8. 2016.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Xu MS, Xu JL, Gao X, Mo SJ, Xing JY, Liu
JH, Tian YZ and Fu XF: Clinical study of neutrophil-to-lymphocyte
ratio and platelet-to-lymphocyte ratio in
hypertriglyceridemia-induced acute pancreatitis and acute biliary
pancreatitis with persistent organ failure. World J Gastrointest
Surg. 16:1647–1659. 2024.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Wang RH, Wen WX, Jiang ZP, Du ZP, Ma ZH,
Lu AL, Li HP, Yuan F, Wu SB, Guo JW, et al: The clinical value of
neutrophil-to-lymphocyte ratio (NLR), systemic immune-inflammation
index (SII), platelet-to-lymphocyte ratio (PLR) and systemic
inflammation response index (SIRI) for predicting the occurrence
and severity of pneumonia in patients with intracerebral
hemorrhage. Front Immunol. 14(1115031)2023.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Wu Y, Chen Y, Yang X, Chen L and Yang Y:
Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte
ratio (PLR) were associated with disease activity in patients with
systemic lupus erythematosus. Int Immunopharmacol. 36:94–99.
2016.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Wang T, Yang Z, Zhou B and Chen Y:
Relationship between NLR and PLR ratios and the occurrence and
prognosis of progressive hemorrhagic injury in patients with
traumatic brain injury. J Invest Surg. 38(2470453)2025.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Li X, Wang L, Liu M, Zhou H and Xu H:
Association between neutrophil-to-lymphocyte ratio and diabetic
kidney disease in type 2 diabetes mellitus patients: A
cross-sectional study. Front Endocrinol (Lausanne).
14(1285509)2024.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Matia-Garcia I, Vadillo E, Pelayo R,
Muñoz-Valle JF, García-Chagollán M, Loaeza-Loaeza J,
Vences-Velázquez A, Salgado-Goytia L, García-Arellano S and
Parra-Rojas I: Th1/Th2 balance in young subjects: relationship with
cytokine levels and metabolic profile. J Inflamm Res. 14:6587–6600.
2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Zhu J: T helper cell differentiation,
heterogeneity, and plasticity. Cold Spring Harb Perspect Biol.
10(a030338)2018.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Shapouri-Moghaddam A, Mohammadian S,
Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi
A, Afshari JT and Sahebkar A: Macrophage plasticity, polarization,
and function in health and disease. J Cell Physiol. 233:6425–6440.
2018.PubMed/NCBI View Article : Google Scholar
|
|
59
|
McNeel DG, Nguyen LD, Ellis WJ, Higano CS,
Lange PH and Disis ML: Naturally occurring prostate cancer
antigen-specific T cell responses of a Th1 phenotype can be
detected in patients with prostate cancer. Prostate. 47:222–229.
2001.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Guan H, Peng R, Fang F, Mao L, Chen Z,
Yang S, Dai C, Wu H, Wang C, Feng N, et al: Tumor-associated
macrophages promote prostate cancer progression via
exosome-mediated miR-95 transfer. J Cell Physiol. 235:9729–9742.
2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Garrido MM, Marta JC, Ribeiro RM, Pinheiro
LC, Holdenrieder S and Guimarães JT: Comparison of three assays for
total and free PSA using hybritech and WHO calibrations. In Vivo.
35:3431–3439. 2021.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Kort SA, Martens F, Vanpoucke H, van
Duijnhoven HL and Blankenstein MA: Comparison of 6 automated assays
for total and free prostate-specific antigen with special reference
to their reactivity toward the WHO 96/670 reference preparation.
Clin Chem. 52:1568–1574. 2006.PubMed/NCBI View Article : Google Scholar
|