Introduction
Acute ischemic stroke (AIS) remains a leading cause
of morbidity, disability and mortality worldwide (1). Despite advances in therapeutic
interventions, ~10-40% of patients with AIS experience early
neurological deterioration (END) (2). END frequently occurs in older
individuals with AIS, resulting in severe neurological impairment
and long-term disability, thereby posing a major risk to health and
survival. Considering the rapid disease progression observed in
elderly patients with AIS (3), the
identification of clinically accessible indicators, such as
hematological parameters or biomarkers, capable of predicting END
is essential to optimize therapeutic strategies and improve
prognosis in this population.
Multiple factors, including baseline stroke
severity, diabetes, hypertension, atrial fibrillation and stroke
subtype, have been recognized as predictors of END (4). Additionally, a meta-analysis has
demonstrated that elevated levels of glucose, total cholesterol,
triglycerides and white blood cells (WBC) are associated with an
increased likelihood of END (5).
Nevertheless, the underlying etiology and mechanisms of END in AIS
remain insufficiently elucidated. END has been linked to impaired
collateral circulation, thrombus extension, cerebral edema and
hemorrhagic transformation (6-8).
Furthermore, immune-mediated inflammation exerts a key influence
across these pathophysiological processes.
Inflammatory activation, coagulation disorders and
nutritional deficiency constitute essential pathophysiological
mechanisms in AIS and serve as indicators of unfavorable outcomes
(9-11).
Lymphocytes are integral to post-AIS inflammation and have been
identified as predictors of aggravated ischemic brain injury and
neurological deterioration (12).
Platelet hyperreactivity heightens the likelihood of
thromboembolism and atherosclerotic plaque formation, promoting
pathological thrombosis. Once activated, platelets participate in
thrombo-inflammatory cascades and tissue injury, enhancing
inflammatory responses (13).
Anemia and hypoalbuminemia, reflecting malnutrition, have been
recognized as risk factors for END (14). Considering the variability in stroke
progression, reliance on a single biomarker may be insufficient for
accurate END prediction. Hence, integrating multiple biomarkers can
enhance predictive precision. The hemoglobin, albumin, lymphocyte
and platelet (HALP) score, a composite biomarker that has recently
gained attention, provides an integrated measure of systemic
inflammatory and nutritional states (15). This index combines indicators of
inflammation (lymphocyte and platelet counts) with markers of
nutritional status (hemoglobin and albumin) and has demonstrated
prognostic significance in several malignancies (16-18).
Nonetheless, the association between HALP scores and END in AIS
remains uncertain. The present study was designed to determine the
predictive significance of the HALP score for END in elderly
individuals with AIS.
Materials and methods
Study population
The present retrospective study enrolled elderly
patients with AIS admitted to Nanjing Drum Tower Hospital, the
Affiliated Hospital of Nanjing University Medical School, between
January 2018 and December 2021. The inclusion criteria were as
follows: (i) age ≥60 years; (ii) diagnosis consistent with the
Guidelines for the Diagnosis and Treatment of AIS (19); (iii) availability of complete
clinical records, including National Institutes of Health Stroke
Scale (NIHSS) scores at admission and discharge as well as modified
Rankin Scale (mRS) scores; and (iv) results of routine hematologic
and albumin assessments at admission. Patients were excluded if
they had: (i) active or chronic inflammatory disorders at
admission; (ii) severe hepatic, renal, cardiac, pulmonary, or other
vital organ failure; (iii) malignancy or any surgical procedure
within the preceding three months; (iv) autoimmune or hematologic
neoplastic diseases, or a history of immunosuppressant use; (v)
received intravenous thrombolysis or endovascular intervention; or
(vi) incomplete clinical information. The study utilized anonymized
retrospective data and received approval from the Ethics Committee
of Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing
University Medical School (approval 2022-308-01; Nanjing, China).
Informed consent was waived by the aforementioned committee.
Data collection
Demographic characteristics (including sex and age),
vascular risk factors (hypertension, diabetes, coronary heart
disease, prior stroke, atrial fibrillation, smoking and alcohol
use), pre-stroke medications (statins, antiplatelet agents and
anticoagulants), baseline blood pressure and glucose, as well as
baseline laboratory parameters [routine blood counts, albumin,
creatinine, lipid profile, homocysteine (Hcy) and lipoprotein
phospholipase A2 (Lp-PLA2)] were systematically recorded. Stroke
etiology, lesion distribution (anterior or posterior circulation),
NIHSS scores at admission and on day 7, and mRS score at 90 days
were also documented. All laboratory measurements were performed on
fasting venous blood samples obtained on the morning of the second
day after admission. Data on lymphocyte count, hemoglobin, platelet
count and albumin were used to calculate the HALP score according
to the formula: Hemoglobin (g/l) x albumin (g/l) x lymphocyte count
(109/l)/platelet count (109/l). Additional
clinical variables, including onset-to-blood collection interval,
hospitalization duration, in-hospital infections and fatal
outcomes, were also recorded.
Clinical assessment
The etiology of AIS was determined following the
Trial of ORG 10172 in Acute Stroke Treatment classification,
including large artery atherosclerotic stroke, cardioembolic
stroke, small vessel occlusive stroke, ischemic stroke of other
determined etiology and ischemic stroke of undetermined etiology.
Stroke severity in elderly patients was evaluated using the NIHSS,
with scores of ≤8, 9-15, and ≥16 representing mild, moderate and
severe stroke, respectively. END was identified as an increase of
at least 2 points in the NIHSS score within 7 days after admission.
Based on the occurrence of END, participants were categorized into
END and non-END groups.
Statistical analysis
Statistical analysis was conducted using SPSS 22.0
(IBM Corp.). Categorical variables were summarized as frequencies
and percentages. Continuous variables were assessed for normality
using the Shapiro-Wilk test. Normally distributed data were
presented as the mean ± standard deviation (x̄±SD) and analyzed
using the independent-samples t-test for two groups, one-way
analysis of variance (ANOVA) for multiple groups, and the
Student-Newman-Keuls (SNK-q) test for post hoc pairwise
comparisons. Data with non-normal distribution were expressed as
medians with interquartile ranges and assessed using the
Mann-Whitney U test for two groups or the Kruskal-Wallis rank-sum
test for multiple groups. Clinical conversion at discharge was
designated as the dependent variable, and variables with P<0.05
in the univariate analysis were entered into a multivariate
logistic regression model. Receiver Operating Characteristic (ROC)
analysis was applied to determine the optimal cutoff value,
sensitivity and specificity for predicting END. Participants were
stratified into tertiles according to HALP scores: Q1 (≤28.11), Q2
(28.11<Q2<44.00) and Q3 (≥44.00). Differences in END
incidence among groups were examined using the chi-square test. A
heat map illustrated the distribution of cases with varying mRS
scores, while Pearson correlation analysis evaluated the
relationship between HALP and NIHSS scores. Statistical
significance was defined as P<0.05.
Results
Baseline characteristics
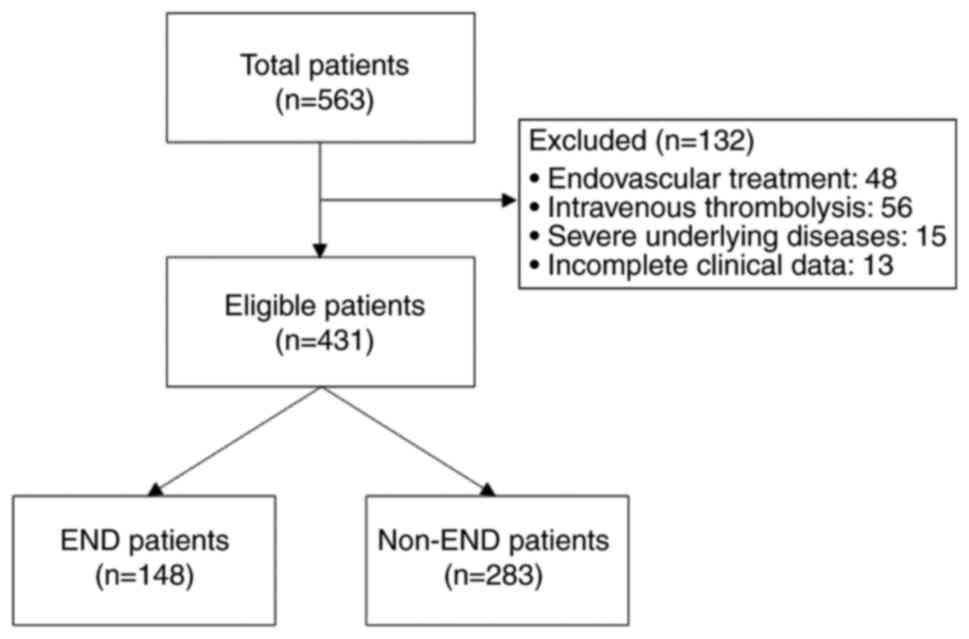
The flow diagram of patient selection and study
cohort formation is presented in Fig.
1. During the study period, 563 elderly patients with AIS were
initially included. After further excluding 48 patients who
received endovascular therapy, 56 who underwent intravenous
thrombolysis, 15 with severe comorbidities and 13 with incomplete
clinical data, 431 patients were ultimately included in the
analysis. Among them, 254 (58.93%) were men, with a median age of
72 years (62-82 years) and a median baseline NIHSS score of 5 (2-14
points). The non-END group consisted of 283 patients (65.66%), and
the END group comprised 148 (34.34%). Compared with the non-END
group, patients in the END group were older and had higher baseline
NIHSS scores. Laboratory analyses indicated significantly elevated
leukocyte count, C-reactive protein (CRP), Hcy and Lp-PLA2 levels
in the END group. In addition, this group exhibited higher
incidences of infectious complications and mortality. In contrast,
lymphocyte count, hemoglobin, triglyceride levels and HALP scores
were significantly reduced in the END group (P<0.05, Table I).
 | Table ICharacteristics of patients with acute
ischemic stroke with or without END. |
Table I
Characteristics of patients with acute
ischemic stroke with or without END.
| Variables | Total (n=431) | No-END group
(n=283) | END group
(n=148) | Statistic | P-value |
|---|
| Demographic data | | | | | |
|
Age (year,
M, IQR) | 72.00 (65.00,
82.00) | 71.00 (64.00,
81.00) | 74.50 (67.50,
84.00) | 2.566 | 0.010a |
|
Male (n,
%) | 254 (58.93) | 171 (60.42) | 83 (56.08) | 0.757 | 0.384 |
| Onset to blood
collection time (h) | 40.00 (28.00,
59.00) | 39.00 (26.00,
55.00) | 45.00 (30.00,
60.50) | 1.743 | 0.081 |
| Stroke risk factors
(n, %) | | | | | |
|
Hypertension | 286 (66.36) | 187 (66.08) | 99 (66.89) | 0.029 | 0.865 |
|
Diabetes | 121 (28.07) | 77 (27.20) | 44 (29.73) | 0.306 | 0.580 |
|
CAD | 67 (15.55) | 47 (16.61) | 20 (13.51) | 0.709 | 0.400 |
|
Prior
stroke | 102 (23.67) | 62 (21.91) | 40 (27.03) | 1.410 | 0.235 |
|
Atrial
fibrillation | 69 (16.01) | 44 (15.55) | 25 (16.89) | 0.131 | 0.718 |
|
Smoking | 112 (25.99) | 77 (27.21) | 35 (23.64) | 0.640 | 0.424 |
|
Alcohol | 77 (17.86) | 50 (17.67) | 27 (18.24) | 0.022 | 0.882 |
| Medical history, n
(%) | | | | | |
|
Antihypertensive | 263 (61.02) | 167 (59.01) | 96 (64.86) | 1.400 | 0.237 |
|
Antidiabetic | 96 (22.27) | 65 (22.97) | 31 (20.95) | 0.230 | 0.632 |
|
Statin | 73 (16.94) | 47 (16.61) | 26 (17.57) | 0.064 | 0.801 |
|
Antiplatelet | 83 (19.26) | 51 (18.02) | 32 (21.62) | 0.810 | 0.368 |
|
Anticoagulants | 32 (7.42) | 19 (6.71) | 13 (8.78) | 0.606 | 0.436 |
| Baseline blood
pressure (mmHg, x̄±S) | | | | | |
|
SBP | 141.31±21.40 | 142.21±20.81 | 139.61±22.47 | 0.054 | 0.817 |
|
DBP | 78.58±13.71 | 79.11±13.30 | 77.57±14.46 | 1.033 | 0.310 |
| Laboratory tests on
admission (IQR) | | | | | |
|
WBC
(109/l) | 7.10 (5.70,
8.90) | 6.70 (5.50,
8.35) | 8.20 (6.80,
10.40) | 5.901 |
<0.001a |
|
Lymphocyte
count (109/l) | 1.50 (1.10,
2.00) | 1.70 (1.30,
2.10) | 1.20 (0.85,
1.55) | -7.528 |
<0.001a |
|
Hemoglobin
(g/l) | 131.50 (118.00,
144.00) | 135.00 (122.00,
147.00) | 125.00 (114.00,
138.00) | -4.360 |
<0.001a |
|
Platelet
count (109/l) | 196.00 (160.00,
237.00) | 194.00 (159.50,
231.50) | 200.50 (158.50,
244.50) | 0.724 | 0.469 |
|
Albumin
(g/l) | 36.00 (33.00,
38.40) | 36.00 (33.00,
39.00) | 35.95 (33.00,
38.30) | -0.192 | 0.848 |
|
HALP
score | 36.40 (24.36,
49.76) | 40.73 (29.83,
56.35) | 25.95 (17.99,
39.26) | -7.750 |
<0.001a |
|
CRP
(mg/l) | 4.30 (2.50,
8.20) | 3.60 (2.40,
6.10) | 6.80 (3.35,
15.80) | 6.313 |
<0.001a |
|
Creatinine
(mmol/l) | 67.00 (57.00,
79.00) | 67.00 (58.00,
79.00) | 66.50 (56.00,
80.50) | 0.161 | 0.872 |
|
Triglycerides
(mmol/l) | 1.13 (0.83,
1.67) | 1.17 (0.87,
1.76) | 0.99 (0.75,
1.36) | -3.659 |
<0.001a |
|
Total
cholesterol (mmol/l) | 4.04 (3.35,
4.83) | 4.05 (3.45,
4.86) | 3.91 (3.07,
4.77) | -1.608 | 0.108 |
|
LDL-C
(mmol/l) | 2.01 (1.31,
2.90) | 2.08 (1.40,
2.85) | 1.70 (1.17,
3.08) | -1.029 | 0.303 |
|
HDL-C
(mmol/l) | 1.19 (0.92,
1.66) | 1.20 (0.94,
1.52) | 1.19 (0.84,
1.93) | -0.043 | 0.966 |
|
Hcy
(µmol/l) | 5.55 (2.60,
11.10) | 5.10 (2.50,
11.10) | 7.45 (3.05,
11.00) | 1.965 | 0.049a |
|
Lp-PLA2 | 189.00 (124.00,
324.00) | 176.00 (119.00,
322.00) | 214.50 (141.50,
360.50) | 2.022 | 0.043a |
|
Fasting
glucose (mmol/l) | 5.11 (4.56,
6.40) | 5.04 (4.54,
6.40) | 5.27 (4.72,
6.47) | 1.886 | 0.059 |
|
Glycohemoglobin
(%) | 5.90 (5.50,
6.70) | 5.90 (5.50,
6.90) | 5.80 (5.50,
6.50) | -1.150 | 0.250 |
| Stroke subtype (n,
%) | | | | 1.270 | 0.866 |
|
LAA | 168 (38.98) | 114 (40.28) | 54 (36.49) | | |
|
SAO | 143 (33.18) | 91 (32.16) | 52 (35.14) | | |
|
CE | 95 (22.04) | 63 (22.26) | 32 (21.62) | | |
|
Other | 25 (5.81) | 15 (5.30) | 10 (6.76) | | |
| Lesion location (n,
%) | | | | 0.144 | 0.704 |
|
Anterior
cerebral circulation | 250 (58.00) | 166 (58.66) | 84 (56.76) | | |
|
Posterior
cerebral circulation | 181 (42.00) | 117 (41.34) | 64 (43.24) | | |
|
Baseline
NIHSS (score, M, IQR) | 5.00 (2.00,
14.00) | 3.00 (1.00,
6.00) | 15.00 (8.00,
21.00) | 12.596 |
<0.001a |
| Baseline NIHSS
classification (n, %) | | | | 130.052 |
<0.001a |
|
Mild (0,
8) | 271 (62.88) | 231 (81.63) | 40 (27.03) | | |
|
Moderate (9,
15) | 67 (15.55) | 29 (10.25) | 38 (25.68) | | |
|
Severe
(≥16) | 93 (21.58) | 23 (8.13) | 70 (47.30) | | |
| Outcome | | | | | |
|
Hospital
infection (n, %) | 48 (11.14) | 10 (3.53) | 38 (25.68) | 48.142 |
<0.001a |
|
Death (n,
%) | 7 (1.62) | 0 (0.00) | 7 (4.73) | 13.606 |
<0.001a |
Risk factors for END
Multivariate logistic regression was performed using
END as the dependent variable and factors from Table I with P<0.05 as independent
variables. The analysis identified a lower HALP score [odds ratio
(OR): 0.965; 95% confidence interval (CI): 0.943-0.988; P=0.003),
higher baseline NIHSS score (OR: 1.169; 95% CI: 1.119-1.220;
P<0.001) and acute-phase infection (OR: 5.459; 95% CI:
2.096-14.219; P=0.001) as independent predictors of increased END
risk (Table II).
 | Table IILogistic regression analysis between
the END group (n=148) and non-END group (n=283). |
Table II
Logistic regression analysis between
the END group (n=148) and non-END group (n=283).
| | 95% CI |
|---|
| Variables | B | SE | Wald
x2 | P-value | OR | Lower | Upper |
|---|
| Age | 0.013 | 0.014 | 0.893 | 0.345 | 1.013 | 0.986 | 1.040 |
| WBC
(109/l) | 0.072 | 0.053 | 1.866 | 0.172 | 1.075 | 0.969 | 1.192 |
| Lymphocyte count
(109/l) | -0.353 | 0.309 | 1.304 | 0.254 | 0.703 | 0.383 | 1.288 |
| Hemoglobin
(g/l) | 0.002 | 0.008 | 0.071 | 0.789 | 1.002 | 0.987 | 1.017 |
| HALP score | -0.035 | 0.012 | 8.701 | 0.003a | 0.965 | 0.943 | 0.988 |
| CRP (mg/l) | 0.014 | 0.012 | 1.287 | 0.257 | 1.014 | 0.990 | 1.038 |
| Triglycerides | -0.022 | 0.154 | 0.020 | 0.889 | 0.979 | 0.723 | 1.325 |
| Hcy (µmol/l) | -0.015 | 0.022 | 0.473 | 0.491 | 0.985 | 0.944 | 1.028 |
| Lp-PLA2 | -0.001 | 0.001 | 1.027 | 0.311 | 0.999 | 0.996 | 1.001 |
| Baseline NIHSS | 0.156 | 0.022 | 49.512 |
<0.001a | 1.169 | 1.119 | 1.220 |
| Hospital
infection | 1.697 | 0.488 | 12.075 | 0.001a | 5.459 | 2.096 | 14.219 |
Predictive value of HALP score for
END
The predictive value of the HALP score, baseline
NIHSS score and their combination for END was analyzed through ROC
curve evaluation. The area under the curve (AUC) values for
predicting END were 0.727 (95% CI: 0.676-0.778), 0.868 (95% CI:
0.834-0.903) and 0.883 (95% CI: 0.850-0.916), respectively.
Sensitivity and specificity were 80.62 and 56.08%, 91.20 and
71.29%, and 82.43 and 84.10%, respectively (Table III). The optimal cut-off points
were 27.69 for the HALP score and 5.5 for the baseline NIHSS
score.
 | Table IIIClinical value of HALP and NIHSS for
predicting END in elderly patients with acute ischemic stroke. |
Table III
Clinical value of HALP and NIHSS for
predicting END in elderly patients with acute ischemic stroke.
| Variables | Threshold | Sensitivity
(%) | Specificity
(%) | AUC | 95% CI |
|---|
| HALP score | 27.69 | 80.62 | 56.08 | 0.727 | 0.676-0.778 |
| Baseline NIHSS | 5.5 | 91.20 | 71.29 | 0.868 | 0.834-0.903 |
| Both | - | 82.43 | 84.10 | 0.883 | 0.850-0.916 |
Correlation between HALP scores and
NIHSS scores
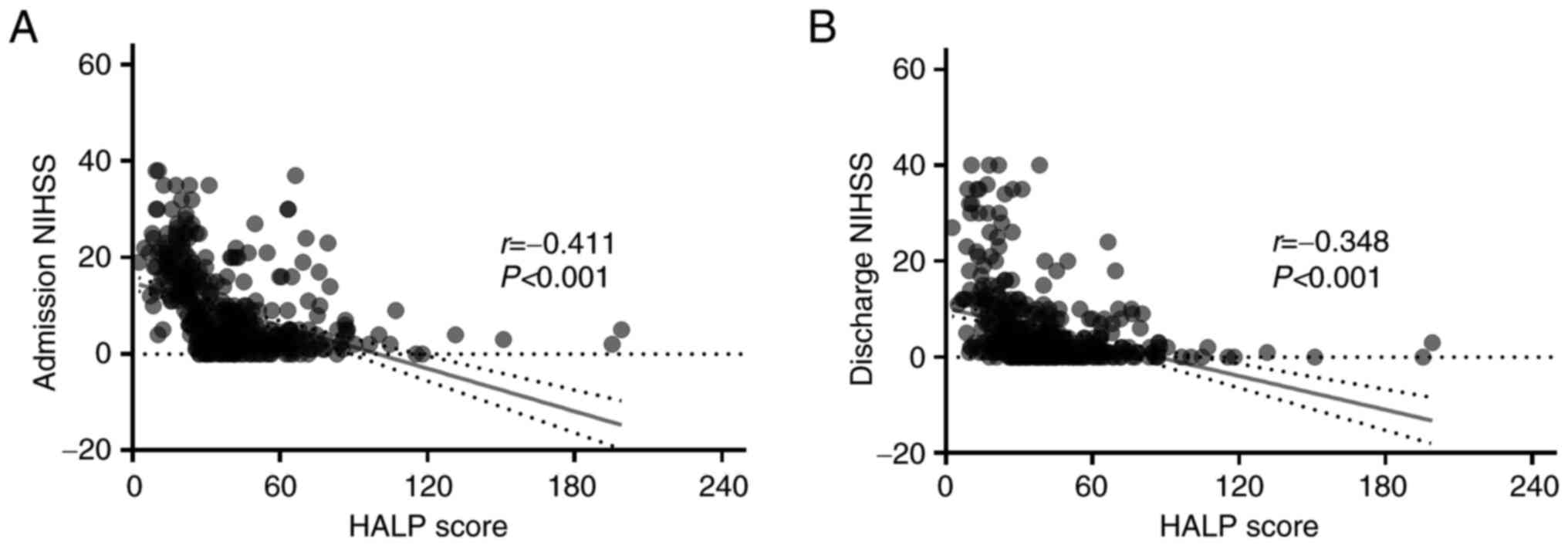
Pearson correlation analysis determined the
association between HALP and NIHSS scores at admission and
discharge in older patients with AIS. A significant inverse
relationship was observed between HALP and NIHSS scores at
admission (r=-0.411; P<0.001) and discharge (r=-0.348;
P<0.001), as shown in Fig.
2.
Association between HALP score and
clinical status in older patients with AIS
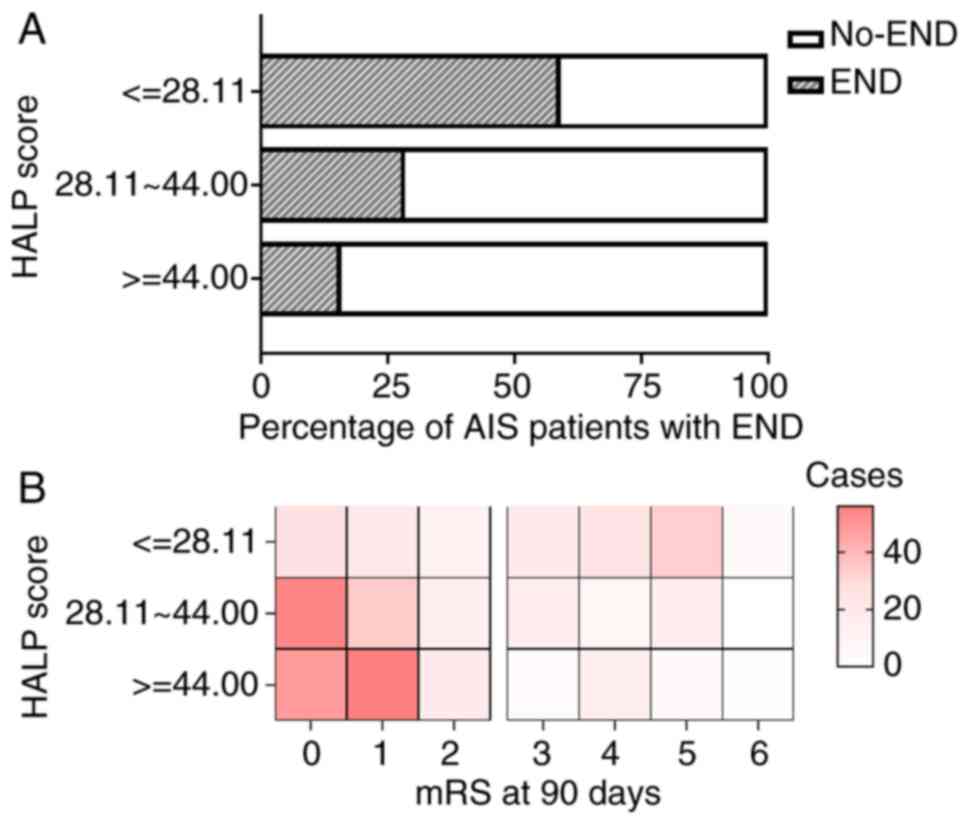
A significant variation in the incidence of END was
noted among tertiles of HALP scores (Q1: 59.15%, Q2: 28.47%, Q3:
15.86%; χ²=158.87; P<0.001) (Fig.
3A). The heat map illustrating patient distribution across HALP
tertiles revealed distinct patterns of clinical outcomes. As shown
in Fig. 3B, among 431 older
patients with AIS, 239 (55.45%) achieved 90-day mRS scores of 0-1.
The highest proportion of favorable outcomes (90-day mRS 0-1)
occurred in Q3 (104/239, 43.51%), whereas poor outcomes (90-day mRS
5-6) were most frequent in Q1 (39/60, 65.00%). The distribution
differences across HALP tertiles were statistically significant
(P<0.001).
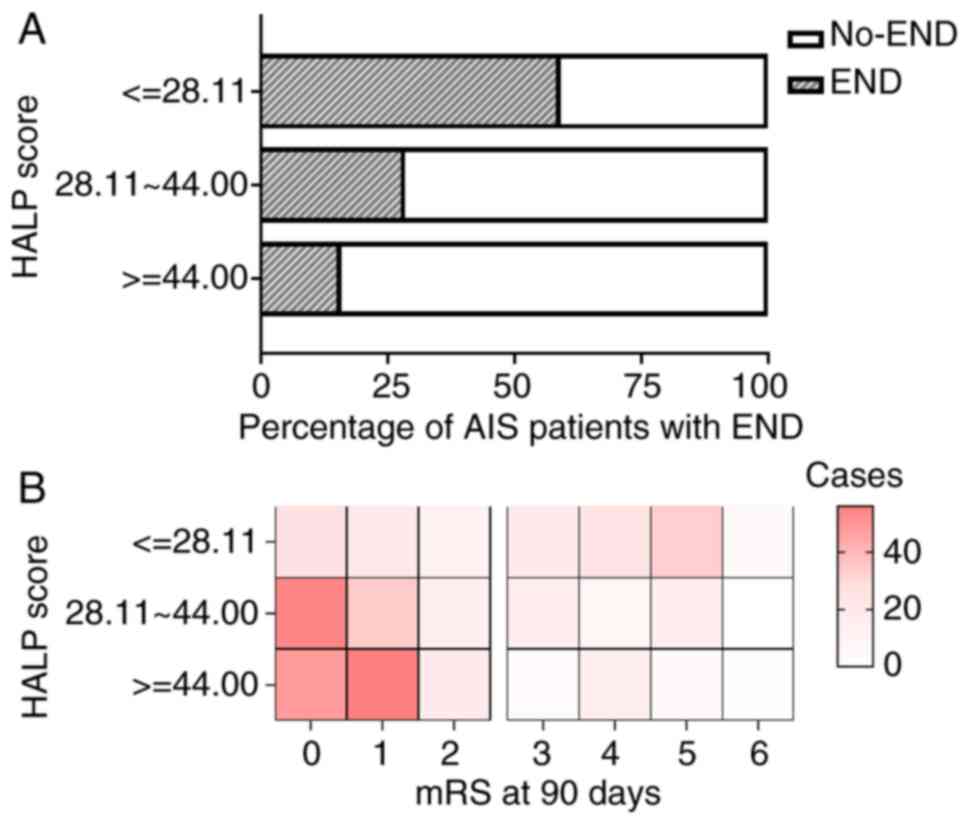 | Figure 3Correlation analysis between HALP
score tertiles and outcome of patients with AIS. Patients with AIS
(n=431) were categorized into three groups: (Q1, n=142; Q2, n=144;
Q3, n=145) based on admission HALP score tertiles. Chi-square test
assessed the difference in END incidence, and heat map illustrated
the distribution of mRS scores among the tertiles. (A) Incidence of
END among groups of patients with AIS stratified by HALP score
tertiles. END incidence varied significantly across HALP tertiles
(Q1: 59.15%, Q2: 28.47%, Q3: 15.86%; χ²=158.87; P<0.001); (B)
Clinical outcome frequency across HALP score tertiles. The
distribution of mRS scores at 90 days differed significantly among
the groups (P<0.001), with the highest proportion of favorable
outcomes (mRS 0-1) in Q3 and the highest frequency of poor outcomes
(mRS 5-6) in Q1. HALP score, hemoglobin, albumin, lymphocyte and
platelet score; mRS, modified Rankin scale; AIS, acute ischemic
stroke; END, early neurological deterioration. |
Discussion
The present study applied the HALP score as an
integrated biomarker to evaluate the risk of END in patients with
AIS and to determine its association with neurological prognosis. A
markedly lower HALP score at admission was linked to an increased
likelihood of END among older individuals with AIS. To the best of
the authors' knowledge, evidence on the connection between HALP
scores and END in this population remains limited. The present
results demonstrate the value of the HALP score in predicting
post-treatment neurological status and contribute to a more refined
understanding of factors influencing END risk factors.
The observed incidence of END (34.34%) exceeded that
reported in a recent study (20),
possibly due to the advanced age and higher comorbidity burden of
the enrolled population. Age-related declines in physical
resilience, increased bleeding tendency, and therapeutic challenges
such as revascularization delay or thrombolysis failure may
contribute to this difference. Furthermore, the adoption of a 7-day
observation window for END identification, as opposed to the more
conventional 24-72 h intervals (21), may also have influenced the observed
incidence. This extended timeframe was selected because
pathophysiological processes underlying END, including inflammatory
cascades, cerebral edema and infections, often progress beyond 72 h
(22), particularly in older
patients with more protracted courses. The 7-day window captures
these late, clinically relevant deteriorations and aligns with
established protocols for vulnerable stroke populations. This
longer observation likely contributed to the relatively high-END
incidence observed in the cohort of the present study.
Consequently, our predictors may encompass both early and subacute
deteriorations, underscoring the need for future studies to
incorporate time-trend analyses and validate the HALP score across
different diagnostic intervals.
Consistent with previous evidence, END was closely
related to unfavorable outcomes (23,24).
Both univariate and multivariate analyses identified baseline NIHSS
scores, infectious events and HALP scores as independent
determinants of END in older patients with AIS. The baseline NIHSS
score serves as an essential indicator of stroke severity,
neurological decline and eventual prognosis. Refining stroke
management protocols and shortening the time to reperfusion may
protect viable neural tissue and decrease END occurrence (25). Older patients are particularly
vulnerable to infections (26),
which can trigger severe complications that jeopardize recovery and
survival. Hence, prompt detection and prediction of infections,
together with timely interventions, may effectively lower the risk
of END. Further studies are needed to substantiate and expand upon
the current observations.
Accurate prediction of END in clinical settings
remains difficult, emphasizing the necessity for simpler and more
effective prognostic systems. Efforts have been directed toward
developing refined tools to identify individuals at high risk of
END, resulting in the formulation of multiple predictive models.
For example, Xie et al (27)
integrated variables such as NIHSS score, middle cerebral artery
stenosis and carotid stenosis into a predictive framework that
identified nearly half of patients susceptible to END. This
observation is consistent with the present study, which identifies
the NIHSS score as a key determinant in evaluating END risk.
Nonetheless, the absence of a universally accepted model in
clinical practice indicates that a multidimensional assessment
including the diverse mechanisms of AIS may yield a more accurate
and comprehensive prediction than reliance on a single
biomarker.
Infection and malnutrition substantially increase
the likelihood of END in patients with stroke (2). The HALP score, a biomarker attracting
increasing attention, provides an integrated evaluation of
inflammatory and nutritional conditions by combining inflammatory
indicators (lymphocyte and platelet counts) with nutritional
metrics (hemoglobin and albumin) (15). Within this index, platelets and
lymphocytes serve as key parameters reflecting coagulative and
inflammatory processes, respectively. A previous study emphasized
the regulatory function of platelets in modulating inflammatory
activity (28). At thrombotic
sites, platelets act as core effector cells in inflammatory
cascades, intensifying pathological progression (29). By contrast, lymphocytes participate
in modulating inflammation by coordinating tissue repair and
recovery. Some researchers have proposed composite indices, such as
the platelet-to-lymphocyte ratio (PLR), to better represent
systemic inflammation and thrombosis. Emerging evidence indicates
that elevated PLR correlates with reduced overall survival and
unfavorable prognosis in stroke populations (30,31).
Xu et al (32) further
demonstrated that increased PLR levels were associated with larger
infarct volumes and poorer clinical outcomes in patients with
AIS.
The HALP score integrates hematologic and
biochemical parameters that reflect interrelated inflammatory and
nutritional disturbances inherent to stroke pathophysiology.
Hemoglobin and albumin, key constituents of this index, exhibit
strong correlations with post-stroke outcomes. Anemia and
hypoalbuminemia have been linked to elevated risks of stroke,
cardiovascular morbidity and mortality (33,34).
Curtelin et al (35)
demonstrated that reductions in hemoglobin concentration may
aggravate neurological deficits in AIS by disrupting cerebral
perfusion and intensifying ischemic hypoxia. Albumin serves as an
indicator of inflammatory burden and overall disease severity
during acute conditions (36).
Lymphopenia reflects systemic inflammation and impaired immune
homeostasis following stroke, as lymphocytes play a regulatory role
in post-ischemic inflammatory cascades, and their depletion is
associated with poorer prognosis (12). Platelets contribute to
thrombo-inflammatory processes by enhancing thrombosis and
releasing proinflammatory mediators (13). Collectively, the HALP score captures
the interdependence between inflammatory activity and nutritional
status, parameters that together provide an integrated reflection
of stroke prognosis.
A prospective cohort study identified a low HALP
score as an independent predictor of unfavorable outcomes in
patients with AIS (37). Early
recognition of END remains essential, as the likelihood of
neurological deterioration increases with time. In the present
study, HALP scores demonstrated significant negative correlations
with NIHSS scores at admission (r=-0.411; P<0.001) and on day 7
(r=-0.348, P<0.001), indicating a moderate association. This
relationship suggests that lower HALP scores correspond to more
severe neurological impairment reflected by NIHSS values. A marked
association was also observed between reduced HALP levels and the
development of END within seven days, aligning with prior evidence
(37). This association likely
reflects the aggravation of ischemic injury induced by systemic
inflammatory activation and nutritional deficiency. Moreover, the
combined predictive performance of HALP and NIHSS scores for END
within 1 week in older patients yielded sensitivities and
specificities of 82.43 and 84.10%, respectively. Integration of
HALP and NIHSS assessments into clinical evaluation may thus enable
earlier identification of high-risk older patients and support more
targeted secondary prevention strategies.
Other unmeasured variables may also influence the
risk of END. Factors such as detailed stroke pathophysiology beyond
the TOAST framework (for example, degree of stenosis and plaque
morphology), collateral circulation integrity, in-hospital blood
pressure control protocols, and specific pharmacologic
interventions during the acute phase warrant further investigation.
These aspects represent meaningful directions for subsequent
studies expanding upon the HALP score framework. In addition, the
analysis of 90-day mRS outcomes, an established indicator of
long-term post-stroke recovery, demonstrated that a lower admission
HALP score correlated with poorer functional outcomes at three
months, suggesting its prognostic relevance may extend beyond the
acute period. The potential association of the HALP score with
long-term recovery, dependency and mortality merits validation
through future prospective studies with prolonged follow-up.
In the present study, a lower HALP score at
admission exhibited a negative correlation with the NIHSS score and
showed a strong association with END occurrence within 7 days,
aligning with previous studies. This relationship likely reflects
the aggravation of ischemic brain injury induced by systemic
inflammatory cascades and malnutrition. The combined predictive
performance of HALP and NIHSS scores for END within one week in
older patients demonstrated sensitivity and specificity of 82.43
and 84.10%, respectively. Integration of HALP with NIHSS in
clinical evaluation enables early recognition of patients at
elevated risk of deterioration, allowing for more timely and
targeted secondary prevention.
The HALP score, derived from standard admission
blood tests, provides a readily obtainable and cost-effective
biomarker. Its operational simplicity and bedside practicality
confer advantages over more complex indices. Moreover, HALP serves
as a valuable parameter for treatment decision-making and triage
during the acute phase of stroke, supporting risk stratification
that guides individualized management, including intensified
therapy and close observation. Nonetheless, large-scale prospective
studies with extended follow-up remain essential to verify the
prognostic value of HALP in predicting END among older patients
with AIS.
The present study has several limitations. First, as
a single-center retrospective investigation, potential selection
bias cannot be excluded, particularly because patients who received
thrombolysis or endovascular therapy were omitted. Although this
exclusion enhanced cohort homogeneity and allowed a focused
assessment of the HALP score's predictive value, it restricts the
applicability of the results to broader stroke populations that
include candidates for acute reperfusion therapies. Validation in
multicenter, prospective cohorts involving thrombolysis- or
thrombectomy-treated patients is required. Second, the observation
group included patients whose NIHSS scores increased by ≥2 points
within 1 week after stroke onset, without accounting for earlier
END events (within 24 or 72 h). Prospective research incorporating
temporal trend adjustments is needed to confirm the temporal
consistency of the predictive associations. Third, as a
retrospective analysis from a single institution, the study lacks
external or temporal validation across independent datasets. The
predictive model derived in the present study requires replication
in larger, multicenter, prospective studies including heterogeneous
populations to confirm its reliability and generalizability before
clinical implementation. Fourth, several potential confounding
variables that might influence END risk were not comprehensively
addressed, including detailed imaging parameters of stroke
etiology, collateral circulation status, specific blood pressure
management strategies during hospitalization and the pharmacologic
impact of in-hospital treatments. The absence of these factors
constrains the mechanistic interpretation of the findings and
should be addressed in future investigations. Finally, the sample
size was determined by the number of eligible patients admitted
during the defined study period. While the observed associations
were statistically significant, this approach remains a
methodological limitation. Accordingly, multicenter cohort studies
are warranted to further clarify the causal association between
HALP scores and END in elderly patients with AIS.
In summary, the analysis indicates that older
patients with acute stroke exhibit a higher incidence of END. A
reduced HALP score at admission likely represents malnutrition and
systemic inflammation, both strongly linked to an elevated risk of
END within 1 week. Moreover, integrating HALP with NIHSS scores
yields high sensitivity and specificity for END prediction,
providing a reliable prognostic indicator that may support
clinicians in optimizing therapeutic strategies.
Acknowledgements
The present manuscript has been released as a
preprint at Research Square (38).
Funding
Funding: The present study was supported by the National Natural
Science Foundation of China Youth Program (grant no. 82304567), the
Health Research Project of Jiangsu (grant no. LKZ2023013), the
Medical Key Science and Technology Development Project of Nanjing
(grant no. ZKX18014), the Cadre Health Care Project of Jiangsu
(grant nos. BJ18006 and BJ19001) and the Cancer Research Funding of
CSCO-Hausen (grant no. Y-HS2019-5).
Availability of data and materials
The data generated in the present study are not
publicly available due to ongoing studies using the current data
but may be requested from the corresponding author.
Authors' contributions
YJL and LLL designed the experiments, wrote the
manuscript and performed statistical analysis. XL performed the
experiments. ABG and MMH processed data. YJL and YX contributed to
the concept of the present study, design of the experiments,
analysis and interpretation of the data, and drafting the
manuscript. All authors read and approved the final version of the
manuscript. YJL and LLL confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
The study protocol was carried out according to the
principles of the Helsinki Declaration, approved by the Ethics
Committee of Nanjing Drum Tower Hospital, The Affiliated Hospital
of Nanjing University Medical School (approval no. 2022-308-01;
Nanjing, China). Informed consent was waived by the Ethics
Committee of Nanjing Drum Tower Hospital, The Affiliated Hospital
of Nanjing University Medical School. All methods were carried out
in accordance with relevant guidelines and regulations.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Meinel TR, Wilson D, Gensicke H, Scheitz
JF, Ringleb P, Goganau I, Kaesmacher J, Bae HJ, Kim DY, Kermer P,
et al: Intravenous thrombolysis in patients with ischemic stroke
and recent ingestion of direct oral anticoagulants. JAMA Neurol.
80:233–243. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Seners P, Ben Hassen W, Lapergue B,
Arquizan C, Heldner MR, Henon H, Perrin C, Strambo D, Cottier JP,
Sablot D, et al: Prediction of early neurological deterioration in
individuals with minor stroke and large vessel occlusion intended
for intravenous thrombolysis alone. JAMA Neurol. 78:321–328.
2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mannina C, Ito K, Jin Z, Yoshida Y,
Matsumoto K, Shames S, Russo C, Elkind MSV, Rundek T, Yoshita M, et
al: Association of left atrial strain with ischemic stroke risk in
older adults. JAMA Cardiol. 8:317–325. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhang M, Xing P, Tang J, Shi L, Yang P,
Zhang Y, Zhang L, Peng Y, Liu S, Zhang L, et al: Predictors and
outcome of early neurological deterioration after endovascular
thrombectomy: A secondary analysis of the DIRECT-MT trial. J
Neurointerv Surg. 15:e9–e16. 2023.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sarejloo S, Kheradjoo H, Haghi SE,
Hosseini S, Gargari MK, Azarhomayoun A, Khanzadeh S and Sadeghvand
S: Neutrophil-to-lymphocyte ratio and early neurological
deterioration in stroke patients: A systematic review and
meta-analysis. Biomed Res Int. 2022(8656864)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bourcier R, Goyal M, Muir KW, Desal H,
Dippel DWJ, Majoie CBLM, van Zwam WH, Jovin TG, Mitchell PJ,
Demchuk AM, et al: Risk factors of unexplained early neurological
deterioration after treatment for ischemic stroke due to large
vessel occlusion: a post hoc analysis of the HERMES study. J
Neurointerv Surg. 15:221–226. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yan Y, Jiang S, Yang T, Yuan Y, Wang C,
Deng Q, Wu T, Tang L, Wu S, Sun J and Wu B: Lenticulostriate artery
length and middle cerebral artery plaque as predictors of early
neurological deterioration in single subcortical infarction. Int J
Stroke. 18:95–101. 2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Liu H, Liu K, Zhang K, Zong C, Yang H, Li
Y, Li S, Wang X, Zhao J, Xia Z, et al: Early neurological
deterioration in patients with acute ischemic stroke: A prospective
multicenter cohort study. Ther Adv Neurol Disord: Jan 24, 2023
(Epub ahead of print).
|
|
9
|
He J, Fu F, Zhang W, Zhan Z and Cheng Z:
Prognostic significance of the clinical and radiological
haemorrhagic transformation subtypes in acute ischaemic stroke: A
systematic review and meta-analysis. Eur J Neurol. 29:3449–3459.
2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Freire MAM, Lima RR, Bittencourt LO,
Guimaraes JS, Falcao D and Gomes-Leal W: Astrocytosis,
inflammation, axonal damage and myelin impairment in the internal
capsule following striatal ischemic injury. Cells.
12(457)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Raposeiras Roubin S, Abu Assi E, Cespon
Fernandez M, Barreiro Pardal C, Lizancos Castro A, Parada JA, Pérez
DD, Blanco Prieto S, Rossello X, Ibanez B and Íñiguez Romo A:
Prevalence and prognostic significance of malnutrition in patients
with acute coronary syndrome. J Am Coll Cardiol. 76:828–840.
2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Malone MK, Ujas TA, Britsch DRS, Cotter
KM, Poinsatte K and Stowe AM: The immunopathology of B lymphocytes
during stroke-induced injury and repair. Semin Immunopathol.
45:315–327. 2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sharma S, Tyagi T and Antoniak S: Platelet
in thrombo-inflammation: Unraveling new therapeutic targets. Front
Immunol. 13(1039843)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bao Y, Zhang Y, Du C, Ji Y, Dai Y and
Jiang W: Malnutrition and the risk of early neurological
deterioration in elderly patients with acute ischemic stroke.
Neuropsychiatr Dis Treat. 18:1779–1787. 2022.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Xu H, Zheng X, Ai J and Yang L:
Hemoglobin, albumin, lymphocyte, and platelet (HALP) score and
cancer prognosis: A systematic review and meta-analysis of 13,110
patients. Int Immunopharmacol. 114(109496)2023.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Guc ZG, Alacacioglu A, Kalender ME,
Oflazoğlu U, Ünal S, Yıldız Y, Salman T, Küçükzeybek Y and Tarhan
MO: HALP score and GNRI: Simple and easily accessible indexes for
predicting prognosis in advanced stage NSCLC patients. The Izmir
oncology group (IZOG) study. Front Nutr. 9(905292)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Hu SJ, Zhao XK, Song X, Lei LL, Han WL, Xu
RH, Wang R, Zhou FY, Wang L and Wang LD: Preoperative maximal
voluntary ventilation, hemoglobin, albumin, lymphocytes and
platelets predict postoperative survival in esophageal squamous
cell carcinoma. World J Gastroenterol. 27:321–335. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Toshida K, Itoh S, Kayashima H, Nagao Y,
Yoshiya S, Tomino T, Fujimoto YK, Tsutsui Y, Nakayama Y, Harada N
and Yoshizumi T: The hemoglobin, albumin, lymphocyte, and platelet
score is a prognostic factor for Child-Pugh A patients undergoing
curative hepatic resection for single and small hepatocellular
carcinoma. Hepatol Res. 53:522–530. 2023.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Dawson J, Bejot Y, Christensen LM, De
Marchis GM, Dichgans M, Hagberg G, Heldner MR, Milionis H, Li L,
Pezzella FR, et al: European stroke organisation (ESO) guideline on
pharmacological interventions for long-term secondary prevention
after ischaemic stroke or transient ischaemic attack. Eur Stroke J.
7:I–II. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lattanzi S, Norata D, Broggi S, Meletti S,
Świtońska M, Słomka A and Silvestrini M: Neutrophil-to-lymphocyte
ratio predicts early neurological deterioration after endovascular
treatment in patients with ischemic stroke. Life (Basel).
12(1415)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhang X, Zhong W, Xue R, Jin H, Gong X,
Huang Y, Chen F, Chen M, Gu L, Ge Y, et al: Argatroban in patients
with acute ischemic stroke with early neurological deterioration: A
Randomized clinical trial. JAMA Neurol. 81:118–125. 2024.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Jiang X, Hu Y, Wang J, Ma M, Bao J, Fang J
and He L: Outcomes and risk factors for infection after
endovascular treatment in patients with acute ischemic stroke. CNS
Neurosci Ther. 30(e14753)2024.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Vynckier J, Maamari B, Grunder L, Goeldlin
MB, Meinel TR, Kaesmacher J, Hakim A, Arnold M, Gralla J, Seiffge
DJ and Fischer U: Early neurologic deterioration in lacunar stroke:
Clinical and imaging predictors and association with long-term
outcome. Neurology. 97:e1437–e1446. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Tan C, Zhao L, Dai C, Liang Y, Liu H,
Zhong Y, Liu G, Mo L, Den F, Liu X and Chen L: Risk factors related
to early neurological deterioration in lacunar stroke and its
influence on functional outcome. Int J Stroke. 18:681–688.
2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Bhole R, Nouer SS, Tolley EA, Turk A,
Siddiqui AH, Alexandrov AV, Arthur AS and Mocco J: COMPASS
investigators. Predictors of early neurologic deterioration (END)
following stroke thrombectomy. J Neurointerv Surg. 15:584–588.
2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
You Q, Bai D, Wu C, Wang H, Chen X, Gao J
and Hou C: Risk factors for pulmonary infection in elderly patients
with acute stroke: A meta-analysis. Heliyon.
8(e11664)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Xie X, Xiao J, Wang Y, Pan L, Ma J, Deng
L, Yang J and Ren L: Predictive model of early neurological
deterioration in patients with acute ischemic stroke: A
retrospective cohort study. J Stroke Cerebrovasc Dis.
30(105459)2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Cloutier N, Allaeys I, Marcoux G, Machlus
KR, Mailhot B, Zufferey A, Levesque T, Becker Y, Tessandier N,
Melki I, et al: Platelets release pathogenic serotonin and return
to circulation after immune complex-mediated sequestration. Proc
Natl Acad Sci USA. 115:E1550–E1559. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Smith CW, Harbi MH, Garcia-Quintanilla L,
Rookes K, Brown H, Poulter NS, Watson SP, Nicolson PLR and Thomas
MR: The Btk inhibitor AB-95-LH34 potently inhibits atherosclerotic
plaque-induced thrombus formation and platelet procoagulant
activity. J Thromb Haemost. 20:2939–2952. 2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gong P, Liu Y, Gong Y, Chen G, Zhang X,
Wang S, Zhou F, Duan R, Chen W, Huang T, et al: The association of
neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and
lymphocyte to monocyte ratio with post-thrombolysis early
neurological outcomes in patients with acute ischemic stroke. J
Neuroinflammation. 18(51)2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sun YY, Wang MQ, Wang Y, Sun X, Qu Y, Zhu
HJ, Wang SJ, Yan XL, Jin H, Zhang P, et al: Platelet-to-lymphocyte
ratio at 24h after thrombolysis is a prognostic marker in acute
ischemic stroke patients. Front Immunol. 13(1000626)2022.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Xu JH, He XW, Li Q, Liu JR, Zhuang MT,
Huang FF and Bao GS: Higher platelet-to-lymphocyte ratio is
associated with worse outcomes after intravenous thrombolysis in
acute ischaemic stroke. Front Neurol. 10(1192)2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Zhang R, Xu Q, Wang A, Jiang Y, Meng X,
Zhou M, Wang Y and Liu G: Hemoglobin concentration and clinical
outcomes after acute ischemic stroke or transient ischemic attack.
J Am Heart Assoc. 10(e022547)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mehta A, De Paola L, Pana TA, Carter B,
Soiza RL, Kafri MW, Potter JF, Mamas MA and Myint PK: The
relationship between nutritional status at the time of stroke on
adverse outcomes: A systematic review and meta-analysis of
prospective cohort studies. Nutr Rev. 80:2275–2287. 2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Curtelin D, Morales-Alamo D,
Torres-Peralta R, Rasmussen P, Martin-Rincon M, Perez-Valera M,
Siebenmann C, Pérez-Suárez I, Cherouveim E, Sheel AW, et al:
Cerebral blood flow, frontal lobe oxygenation and intra-arterial
blood pressure during sprint exercise in normoxia and severe acute
hypoxia in humans. J Cereb Blood Flow Metab. 38:136–150.
2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Di Vincenzo O, Luisi MLE, Alicante P,
Ballarin G, Biffi B, Gheri CF and Scalfi L: The assessment of the
risk of malnutrition (Undernutrition) in stroke patients.
Nutrients. 15(683)2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Tian M, Li Y, Wang X, Tian X, Pei LL, Wang
X, Zhang L, Sun W, Wu J, Sun S, et al: The hemoglobin, albumin,
lymphocyte, and platelet (HALP) score is associated with poor
outcome of acute ischemic stroke. Front Neurol.
11(610318)2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Li Ling-ling, Xie Y, Liang Xet, et al:
Clinical application of halp score to predict early neurological
deterioration in elderly acute cerebral infarction patients,
2023.
|