Introduction
Hepatocellular carcinoma (HCC) is one of the
critical global health issues. As indicated in cancer statistics,
HCC is the sixth most common type of tumor worldwide, but due to
its poor prognosis it ranks as the third most common cause of
mortality from cancer (1,2). Despite therapeutic advances, the
overall survival of patients with HCC has not significantly
improved in the last two decades. Surgical resection,
radiofrequency ablation (RFA) and percutaneous ethanol injection
(PEI) are curative treatments; however, they are accompanied by
high recurrence rates (3–5). Transarterial chemoembolization
(TACE), the most popular non-surgical alternative, is often used as
a palliative treatment (6).
General chemotherapy and radiotherapy offer somewhat unsatisfactory
responsiveness. Thus, new therapeutic strategies are necessary to
combat HCC.
Based on observations from the beginning of the last
century, it has become well established that solid tumors may
contain oxygen-deficient hypoxic areas, and that cells in such
areas may cause tumors to become radioresistant (7,8). A
substantial amount of data have indicated the presence of hypoxia
in numerous types of human tumors, including HCC. Treating hypoxic
tumor cells could involve the specific modification of tumor
radiosensitivity by the use of chemical radiosensitizers. Targeting
various physiological characteristics of the tumor,
radiosensitizers are intended to enhance tumor cell killing by
radiation, while having much less of an effect on normal tissues
(9,10). Etanidazole, a nitroimidazole
hypoxic radiosensitizer, has the advantage of lower toxicity at
gram-level doses administered to patients in order to attain tumor
concentrations reasonable for radiosensitization (11). Paclitaxel is one of the best
anti-neoplastic drugs discovered in previous decades. A number of
studies have confirmed the radiosensitizing effect of paclitaxel
(12). Owing to the side-effects
of radiosensitizers, clinical protocols frequently combine these
drugs, which exhibit their cytotoxic action at various mechanisms.
This approach minimizes the overall toxicity while enhancing
maximal radiosensitization (13).
This strategy has been used to study the radiosensitizing effect of
the combination of etanidazole and paclitaxel in our previous
study. The results indicated that the radiosensitization produced
by etanidazole and paclitaxel was additive in vitro
(14,15).
This study was carried out to evaluate the
radiosensitizing effect of the combination of etanidazole and
paclitaxel for HCC in vivo, using a murine H22-bearing
BALB/c model.
Materials and methods
Drugs
Etanidazole was purchased from Sigma-Aldrich (St.
Louis, MO, USA). Paclitaxel (H20063662, 30 mg/5 ml) was from
Beijing Sihuan Pharmaceutical Co. Ltd (Beijing, China). Etanidazole
was dissolved in phosphate-buffered saline (PBS; pH 7.4) at a
concentration of 10 mg/ml for the actual test. A paclitaxel stock
solution of 10 μg/ml prepared in PBS medium was maintained at −20°C
and thawed for use.
Cell culture
The murine HCC H22 cells were purchased from the
Experimental Animal Center of the Fourth Military Medical
University (Xi’an, China). The cells were frozen and stored in
liquid nitrogen for further use. For experiments, the cells were
thawed and subcultured in ascites of BALB/c mice.
Animals
Male BALB/c mice (20±2 g) were supplied by the
Experimental Animal Center of the Fourth Military Medical
University. The animals were acclimatized at a temperature of
25±2°C and a relative humidity of 70±5% under natural light/ dark
conditions for 1 week prior to dosing. All animal experiments were
performed under the guidelines of an approved protocol from the
Committee on the Use of Live Animals in Teaching and Research of
the Fourth Military Medical University.
Radiation
Radiation was delivered at room temperature
utilizing a 60Co source (Department of Radiation
Medicine, Fourth Military Medical University). The dose rate
depended on the distance from the source. Radiation was delivered
at 266.82 cGy/min for a duration of 1 min 52 sec to produce a dose
of 5 Gy. Following radiation, animals were maintained under
standard breeding conditions for 6 months.
Tumor morphology
H22-bearing BALB/c mice were studied. In order to
establish the murine HCC xenografts, a cell suspension (0.2 ml)
containing 2×106 H22 cells was inoculated subcutaneously
into the back of the mice for 12 days. The mice were sacrificed by
cervical dislocation and tumors were then removed. Sections of
tumor tissue were fixed in neutral buffered formalin and the
paraffin sections were prepared for hematoxylin and eosin (H&E)
histological staining. The photomicrography was performed using a
Nikon TE2000-S microscope (Japan).
Drug content in blood and tumors
Drug content in the blood and tumors of H22-bearing
mice (n=5) was evaluated by high-performance liquid chromatography
(HPLC). Etanidazole at 200 mg/kg and/or paclitaxel at 1 mg/kg were
injected through the tail vein 12 days following inoculation. The
mice were treated with PBS as the control. Two hours following
administration, the mice were sacrificed by cervical dislocation.
Blood was then collected via decapitation and tumors were removed.
Blood was placed at room temperature for 30 min and then
centrifuged at 1,000 rpm for 5 min. Blood serum was collected.
A total of 200 mg of tumors were homogenized in 3 ml
of a mixture of acetonitrile: water [50:50, (v/v)] or
acetonitrile:water [5:95, (v/v)] and centrifuged at 3,000 rpm for 5
min. The supernatant was taken for analysis of drug content by
HPLC.
A total of 200 μl of blood serum were mixed with 1
ml of a mixture of acetonitrile:water [50:50, (v/v)] or
acetonitrile:water [5:95, (v/v)]. The solution containing the drugs
was determined using HPLC.
The HPLC assay (Agilent 1100 series) for etanidazole
and paclitaxel was performed on a reverse phase Zorbax®
C18 column. The mobile phases for etanidazole and paclitaxel were
the mixtures of acetonitrile: water 5:95 and 50:50 (v/v),
respectively. The mobile phase was delivered at a flow rate of 1.0
ml/min. Etanidazole and paclitaxel were detected at 324 and 227 nm,
respectively, with a variable wavelength detector. The calibration
curves for the quantification for etanidazole and paclitaxel were
linear over the range of a standard concentration between 50 and
100,000 ng/ml with a correlation coefficient of R2=0.99
and 1.00.
Radiosensitizing effect in vivo
Animals were randomized 12 days following
inoculation and divided into 8 mice/ group (control, radiation
only, etanidazole, paclitaxel, and combination of etanidazole and
paclitaxel). The administration of drugs and radiation were
conducted as described above. Radiation was performed 2 hours
following administration. The mice received a single dose of
whole-body γ-ray radiation using a 60Co source. Mice
were monitored daily and all surviving mice were sacrificed on day
180. Tumor volumes [(major axis) × (minor axis)2×1/2]
were measured with a caliper at defined time periods for 40 days
post-radiation. The tumor inhibition rate (%) was calculated using
the following formula: (tumor volume of control - tumor volume of
experiment)/tumor volume of control ×100%.
Immunohistochemistry
The expression of hypoxia inducible factor-1α
(HIF-1α) was determined by immunohistochemistry staining. Two days
following radiation, H22-bearing mice were sacrificed and the
tumors were removed. Paraffin-embedded tissue sections at 4 μm were
prepared. Tissue sections were deparaffinized in xylene and
rehydrated in graded alcohols and distilled water. Slides were
processed for antigen retrieval by a standard microwave heating
technique in citrate buffer (pH 6.0). Endogenous peroxidases were
inactivated by immersing the sections in 0.3% hydrogen peroxide for
10 min twice. The primary polyclonal rabbit antibody reacts
specifically with mouse HIF-1α (dilution 1:100; Wuhan Boster
Biological Technology Co. Ltd, China). The sections were incubated
with the antibody overnight at 4°C in a humidified chamber.
Immunodetection was performed using a standard avidin-biotin
peroxidase technique. The reaction was then developed using the
Liquid DAB Substrate-Chromogen System. Sections were counterstained
with Mayer’s hematoxylin. Positive staining (brown) for HIF-1α
proteins was observed predominantly in the cytoplasm of cells. More
than 1,000 cells in 5–6 various high-power fields (×400) were
analyzed for each section.
Statistical analysis
Comparisons of the drug content and tumor volume
were performed using one-way ANOVA. Survival studies were analyzed
using Kaplan-Meier plots. The Chi-square test was used to compare
the positive rate of HIF-1α. All analyses were performed using the
statistical software SPSS10.0.
Results
Tumor morphology
The morphological changes of H22 xenografts are
shown in Fig. 1. When treatments
were commenced on day 12 post-incubation, tumor size was
approximately 0.2 cm3. Macroscopic forms of the tumors
were grayish-white and soft. In microscopic appearance, the
neoplastic cells still resembled normal hepatocytes, but the nuclei
were large and more hyperchromatic. Moreover, the nuclei were more
prominent than the cytoplasm. This was consistent with the
pathological characteristics of HCC.
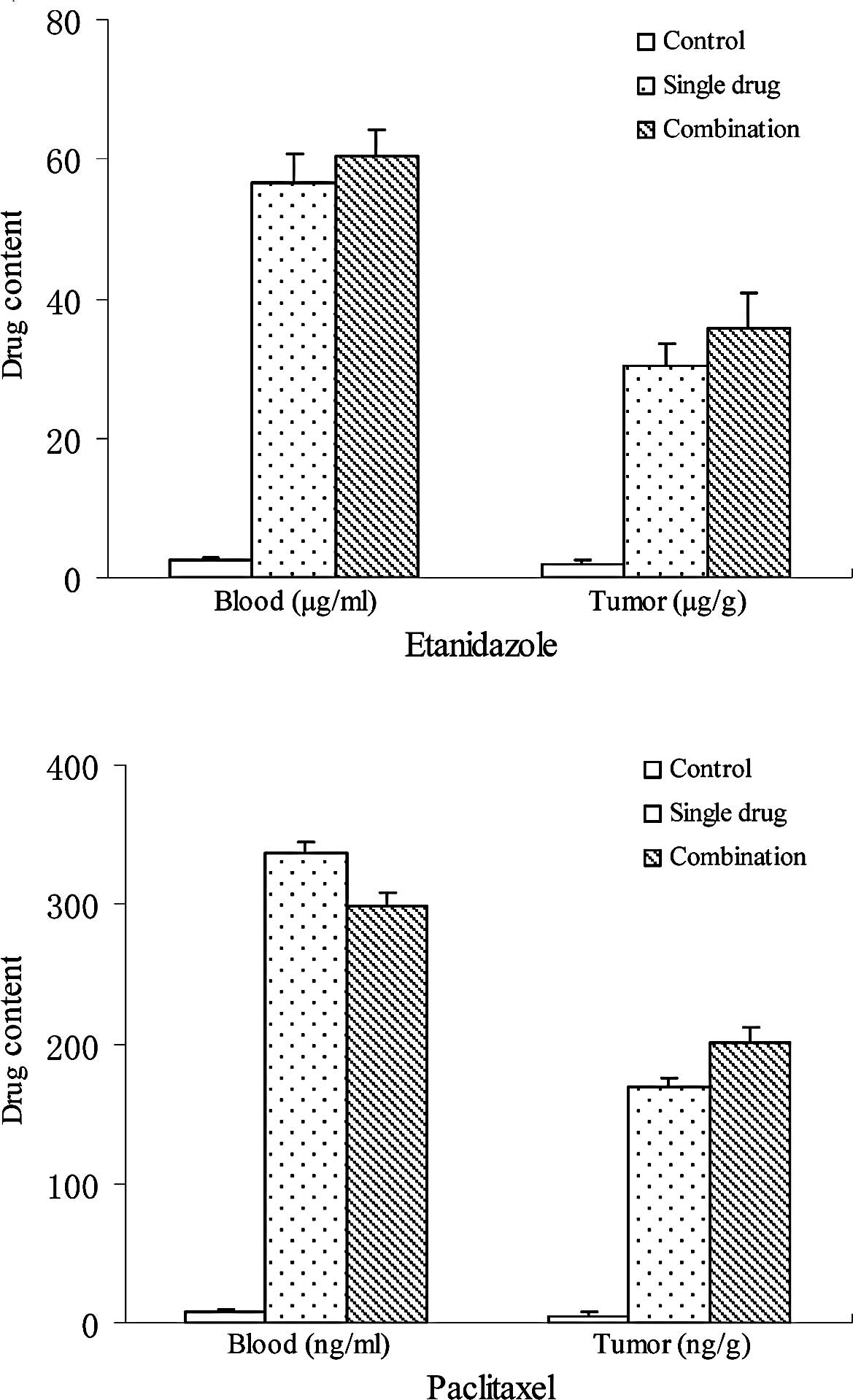
Drug content in blood and tumors
Drug content in the blood and tumors of H22-bearing
mice 2 h after intravenous administration is shown in Fig. 2. For etanidazole and paclitaxel,
there was no significant difference in drug content in the blood or
tumors between treatment with either drug alone or combination
treatment. Etanidazole content in the blood was 56.7±4.1 and
60.5±3.8 μg/ml for treatment with etanidazole alone and combination
treatment, respectively. Etanidazole content in the tumors was
30.2±3.3 μg/m and 35.6±5.1 μg/g for treatment with etanidazole
alone and combination treatment, respectively. Paclitaxel content
in the blood was 336.9±7.8 and 229.5±8.4 ng/ml for treatment with
paclitaxel alone and combination treatment, respectively.
Paclitaxel content in the tumors was 168.7±6.9 ng/m and 201.3±10.4
ng/g for treatment with paclitaxel alone and combination treatment,
respectively.
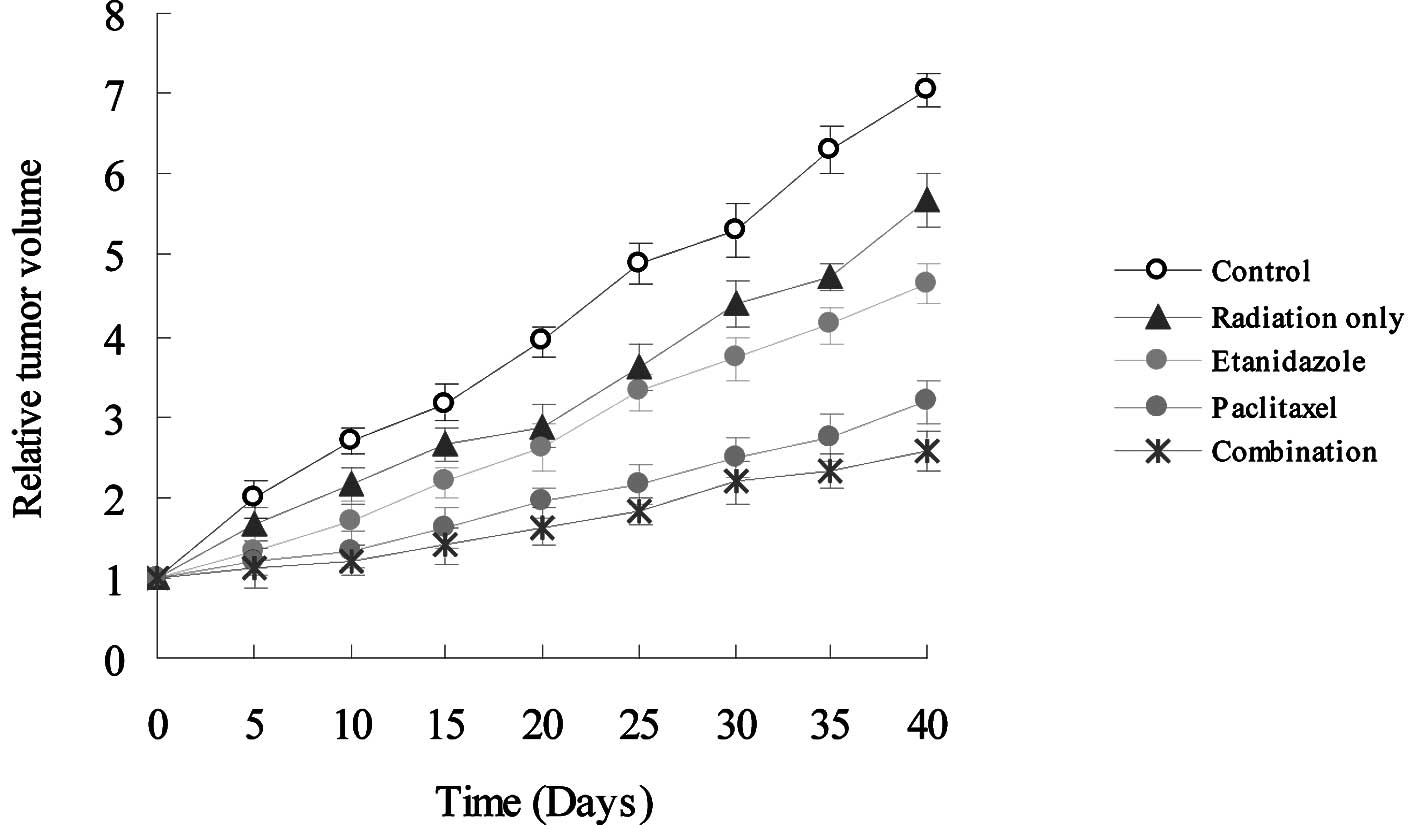
Radiosensitizing effect in vivo
To assess the radiosensitizing effect in
vivo, etanidazole and/or paclitaxel were injected through the
tail vein of H22-bearing mice at clinically relevant doses.
Following administration, the mice were exposed to radiation at 5
Gy. Tumor regression was observed in treated mice (Fig. 3). It clearly shows that the
combination of the two drugs had the greatest regressional effect
on the tumor burden in all groups. Forty days following radiation,
the tumor inhibition rates (%) were 19.2, 33.9, 54.8 and 61.6% for
radiation only, etanidazole, paclitaxel, and combination therapy,
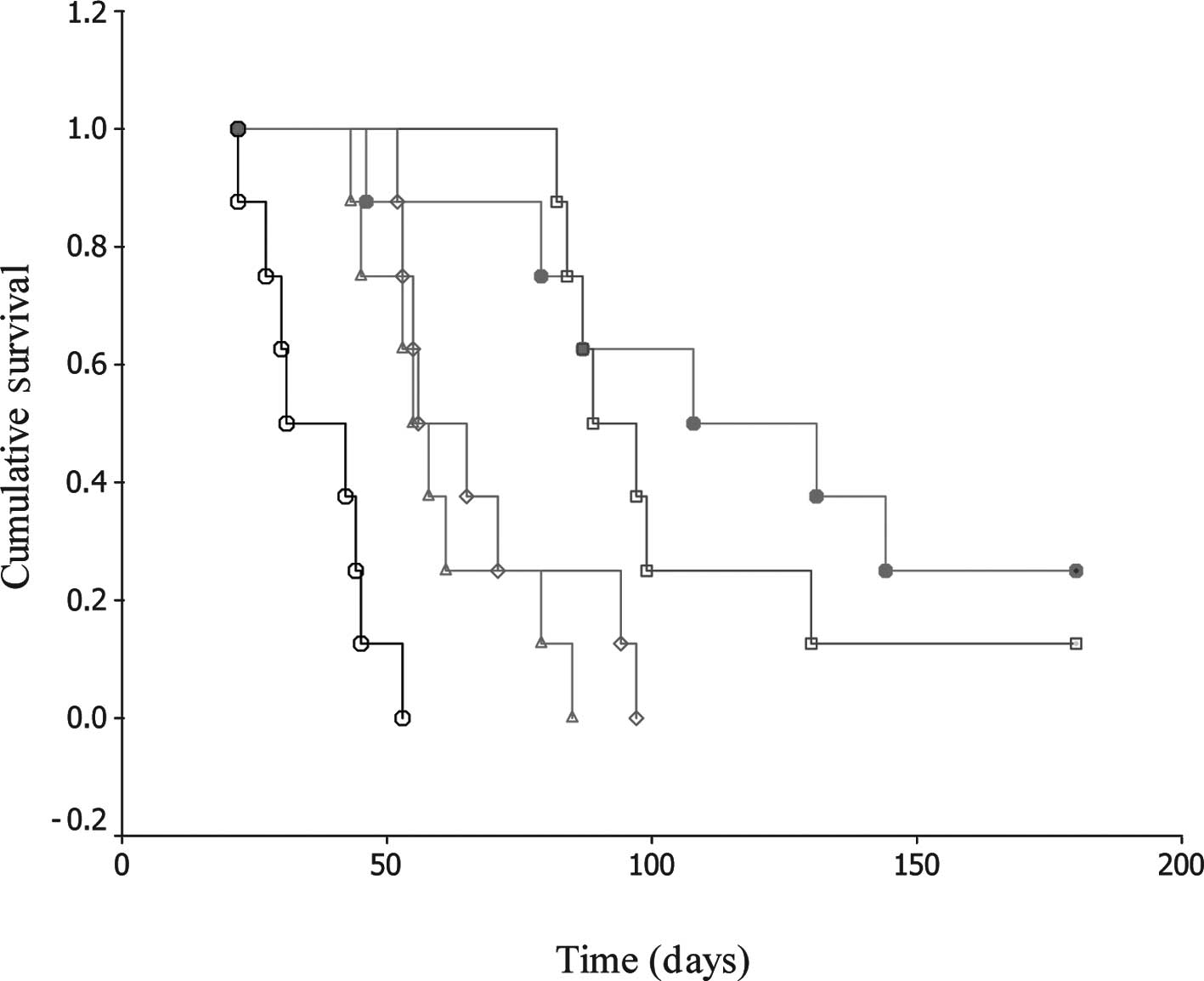
respectively. In addition, there was a significant difference in
the survival rate for these treatments. Observable even up to 180
days, the animals displayed 0, 0, 0, 12.5 and 25.0% survival rates
for control, radiation only, etanidazole, paclitaxel, and
combination therapy, respectively. The median survival times were
31.0±8.5, 55.0±3.5, 56.0±7.1, 89.0±7.1 and 108.0±31.1 days for the
control, radiation only, etanidazole, paclitaxel, and combination
therapy, respectively (Fig.
4).
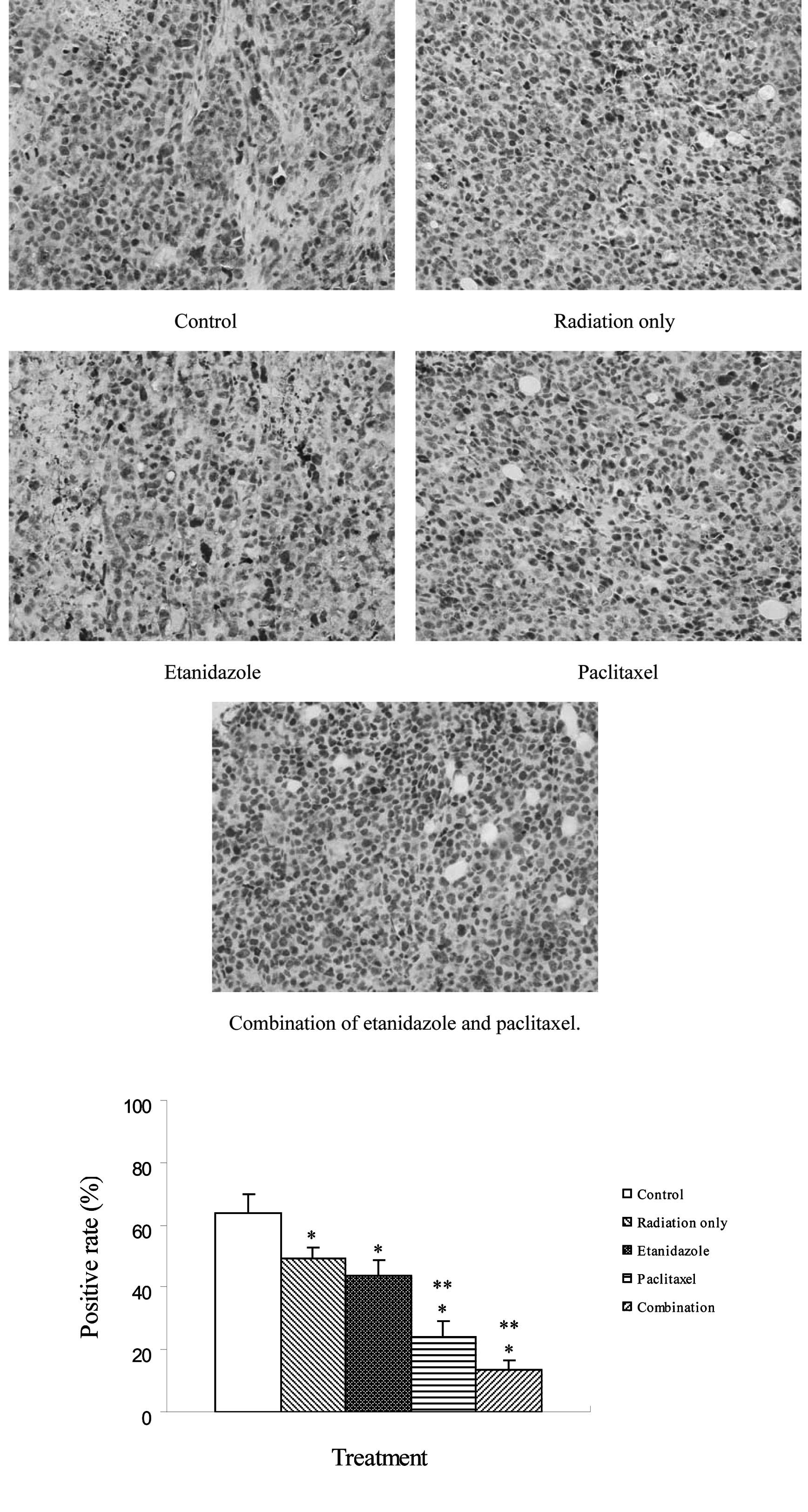
Immunohistochemistry
The expression of HIF-1α in H22 xenografts was
demonstrated immunohistochemically by positive cytoplasmic staining
(Fig. 5). Its expression was
observed in all samples and the percentages of positively stained
cells were 63.7, 49.2, 43.6, 24.3 and 13.6% for the control,
radiation only, etanidazole, paclitaxel, and combination therapy,
respectively. HIF-1α expression in the treated groups was
significantly lower than in the control group. Moreover, HIF-1α
expression in the paclitaxel and combination groups was lower than
in the radiation only and etanidazole-treated groups.
Discussion
Although the development of imaging modalities has
made the early diagnosis of HCC possible, surgically resectable
cases are relatively rare owing to a hepatic function reserve
and/or an advanced stage at presentation. Several modalities,
including RFA, PEI, TACE and microwave coagulation therapy (MCT)
reportedly aid the treatment of patients with unresectable disease.
However, unfortunately, it is effective only on limited occasions.
Therefore, intensive research efforts have been directed toward the
identification of novel treatment strategies for HCC.
Radiotherapy technology has evolved markedly over
the past decade, and radiation is capable of being precisely
delivered, thereby permitting higher doses to the tumor and reduced
doses to surrounding normal tissues. There has been increasing
interest in the merits of radiotherapy in HCC over the past few
years. Radiotherapy has been used as the definitive therapy with
curative intent in early stage tumors. It has also been used in
combination with TACE for intermediate stage tumors. In locally
advanced tumors, radiotherapy has been combined with systemic
agents, including chemotherapeutic drugs and hypoxic
radiosensitizers (16–18). Certain studies have shown promising
survival outcomes. Our previous study indicated that the
combination of etanidazole and paclitaxel had a synergetic
radiosensitizing effect on MCF-7 and HeLa cells in vitro
(14,15). Based on these findings, we
therefore investigated the efficacy of the combination of the two
drugs in vivo for overcoming HCC.
In the present study, the morphology of H22
xenografts in macroscopic and microscopic forms displayed HCC
characteristics. This demonstrates that the transplantation of
tumors was successfully carried out, and lays the foundation for
further study.
The HPLC assay was used to determine drug content in
blood and tumors of mice bearing H22 xenografts. Our results
indicated that there was no significant difference in content of
the two drugs between treatment with either drug alone or in
combination. This eliminated the effect of the difference in drug
content on therapeutic efficacy.
To understand the synergistic radiosensitizing
effect of the two drugs in vivo, a survival assay was
performed. Overall, the combination of the two drugs exhibited an
improved therapeutic profile in terms of tumor growth inhibition
and survival, compared to single drug administration in animal
models. Clearly, the treatment with etanidazole and/or paclitaxel
resulted in more significant tumor regression than radiation
therapy alone. The effect of paclitaxel was more significant than
that of etanidazole at these administered doses. These data
demonstrate that the combination of the two drugs has a synergistic
effect. These results are consistent with our previous study in
vitro. The lifespan of H22-bearing mice treated with
radiosensitizers was significantly longer than the control and mice
treated with radiation only. Animals treated with a combination of
the two drugs exhibited the longest lifespan in all the groups and
had a markedly improved survival rate. Therefore, the
co-administration of the two drugs may result in a beneficial gain
in HCC radiotherapy. However, complete tumor regression was not
observed. This suggests that the administration dose may be
modified to produce an improved radiosensitizing effect in future
studies.
HIF-1 is as a key transcriptional mediator of the
hypoxic response in tumor cells, regulating the expression of a
myriad of genes involved in oxygen transport, glucose uptake, and
glycolysis and angiogenesis. The overexpression of HIF-1 is
observed in the zones of avascularity and hypoxia of most tumors.
As a significant marker, HIF-1 expression increases with hypoxic
level in tumor location (19,20).
Therefore, it may indirectly represent the number of hypoxic cells.
This study indicated that treatment with etanidazole and/or
paclitaxel resulted in a decrease in the number of hypoxic cells
and that a combined treatment was most significant. It further
verified the results of the survival assay.
In brief, this study demonstrates the efficacy of
radiosensitization by the combination of etanidazole and paclitaxel
in vivo for HCC. The data suggest the possibility of its
clinical application. However, to date, there is no report that the
radiosensitizing effect of the combination is additive clinically.
Therefore, well-designed prospective studies are strongly
recommended to provide evidence of the true efficacy.
In conclusion, etanidazole and paclitaxel
demonstrated the ability to radiosensitize the HCC cells in
vivo. The radiosensitizing effect produced by the two drugs was
additive when they were administered together at clinically
relevant concentrations. This study may provide a new combination
of drugs for HCC radiotherapy, although further clinical studies
are required
Acknowledgements
This study was supported by grants
from the National Nature Science Foundation of China (No. 81000987)
and the China Postdoctoral Science Foundation Funded Project (No.
201003744).
References
|
1.
|
World Health OrganizationMortality
databaseWHO statistical information system. http://www.who.int/whosis/. Accessed July 2008.
|
|
2.
|
DM ParkinF BrayJ FerlayP PisaniGlobal
cancer statistics, 2002CA Cancer J
Clin5574108200510.3322/canjclin.55.2.74
|
|
3.
|
S PadmaJB MartinieDA IannittiLiver tumor
ablation: percutaneous and open approachesJ Surg
Oncol100619634200910.1002/jso.2136420017157
|
|
4.
|
T IchidaDH van ThielT HassaneinThe medical
management of hepatocellular carcinoma (HCC) in Japan: a review
with implications for HCC seen in the
westHepatogastroenterology431575158319968975968
|
|
5.
|
J BruixM ShermanPractice Guidelines
Committee, American Association for the Study of Liver
DiseasesManagement of hepatocellular
carcinomaHepatology4212081236200510.1002/hep.20933
|
|
6.
|
JM LlovetMI RealX MontanaR PlanasS CollJ
AponteArterial embolisation or chemoembolisation versus symptomatic
treatment in patients with unresectable hepatocellular carcinoma: a
randomised controlled
trialLancet35917341739200210.1016/S0140-6736(02)08649-X
|
|
7.
|
BA TeicherHypoxia and drug
resistanceCancer Metast Rev1339681994
|
|
8.
|
DM BrizelGS SibleyLR ProsnitzRL ScherMW
DewhirstTumor hypoxia adversely affects the prognosis of carcinoma
of the head and neckInt J Radiat Oncol Biol
Phys38285289199710.1016/S0360-3016(97)00101-69226314
|
|
9.
|
J OvergaardHypoxic radiosensitization:
adored and ignoredJ Clin
Oncol2540664074200710.1200/JCO.2007.12.787817827455
|
|
10.
|
P WardmanChemical radiosensitizers for use
in radiotherapyClin Oncol (R Coll
Radiol)19397417200710.1016/j.clon.2007.03.01017478086
|
|
11.
|
CN ColemanTH WassermanRC UrtasunJ HalseyVK
HirstS HancockPhase I trial of the hypoxic cell radiosensitizer
SR-2508: the results of the five to six week drug scheduleInt J
Radiat Oncol Biol
Phys1211051108198610.1016/0360-3016(86)90236-13017904
|
|
12.
|
RB TishlerPB SchiffCR GeardEJ HallTaxol: a
novel radiation sensitizerInt J Radiat Oncol Biol
Phys22613617199210.1016/0360-3016(92)90888-O1346533
|
|
13.
|
ME WattsMF DennisM WoodcockUptake and
additivity of the radiosensitizing effects of Ro 03-8799 and
SR-2508 in mammalian cells in vitroBr J
Radiol6012331235198710.1259/0007-1285-60-720-12332961396
|
|
14.
|
C JinL BaiG GuoRadiosensitization by the
combination of SR-2508 and paclitaxel in hypoxic human tumor cells
in vitroJ Radiat Res48179185200710.1269/jrr.0610517420623
|
|
15.
|
C JinL BaiH WuF TianG
GuoRadiosensitization of paclitaxel, etanidazole and
paclitaxel+etanidazole nanoparticles on hypoxic human tumor cells
in vitroBiomaterials28372437302007
|
|
16.
|
J SeongChallenge and hope in radiotherapy
of hepatocellular carcinomaYonsei Med
J50601612200910.3349/ymj.2009.50.5.60119881961
|
|
17.
|
S MaB JiaoX LiuH YiD KongL GaoApproach to
radiation therapy in hepatocellular carcinomaCancer Treat
Rev36157163201010.1016/j.ctrv.2009.11.00820031332
|
|
18.
|
SH KerrDJ KerrNovel treatments for
hepatocellular cancerCancer
Lett286114120200910.1016/j.canlet.2009.07.00119664880
|
|
19.
|
CC HudsonM LiuGG ChiangDM OtternessDC
LoomisF KaperRegulation of hypoxia-inducible factor 1alpha
expression and function by the mammalian target of rapamycinMol
Cell Biol2270047014200210.1128/MCB.22.20.7004-7014.200212242281
|
|
20.
|
JI BárdosM AshcroftNegative and positive
regulation of HIF-1: a complex networkBiochim Biophys
Acta1755107120200515994012
|