Introduction
Thoracoscopy is a useful technique for diagnosing
plural lesions, and it provides valuable information for
identifying a cancer of an unknown primary origin (CUP) (1–3). The
diagnostic procedure for the evaluation of CUP includes clinical
and laboratory investigations, namely, imaging, endoscopy,
pathology and tumor markers (4).
In particular, in the work-up of a CUP patient with exudative
pleural effusion, thoracoscopy is an established tool to aid
diagnosis (5,6).
Ovarian cancer with intrathoracic metastases is
often accompanied by abdominal-related symptoms, and ovarian cancer
cases with only thoracic lesions are rare (7–10).
It is not uncommon to initially categorize these rare cases as CUP
(4,9,10).
Here, we report 3 cases of ovarian cancer with predominantly
intrathoracic lesions, which were diagnosed by thoracoscopy. In
addition, in these cases, we observed an association between the
serum Krebs von den lungen-6 (KL-6) level and the state of the
ovarian cancer.
Case reports
Case 1
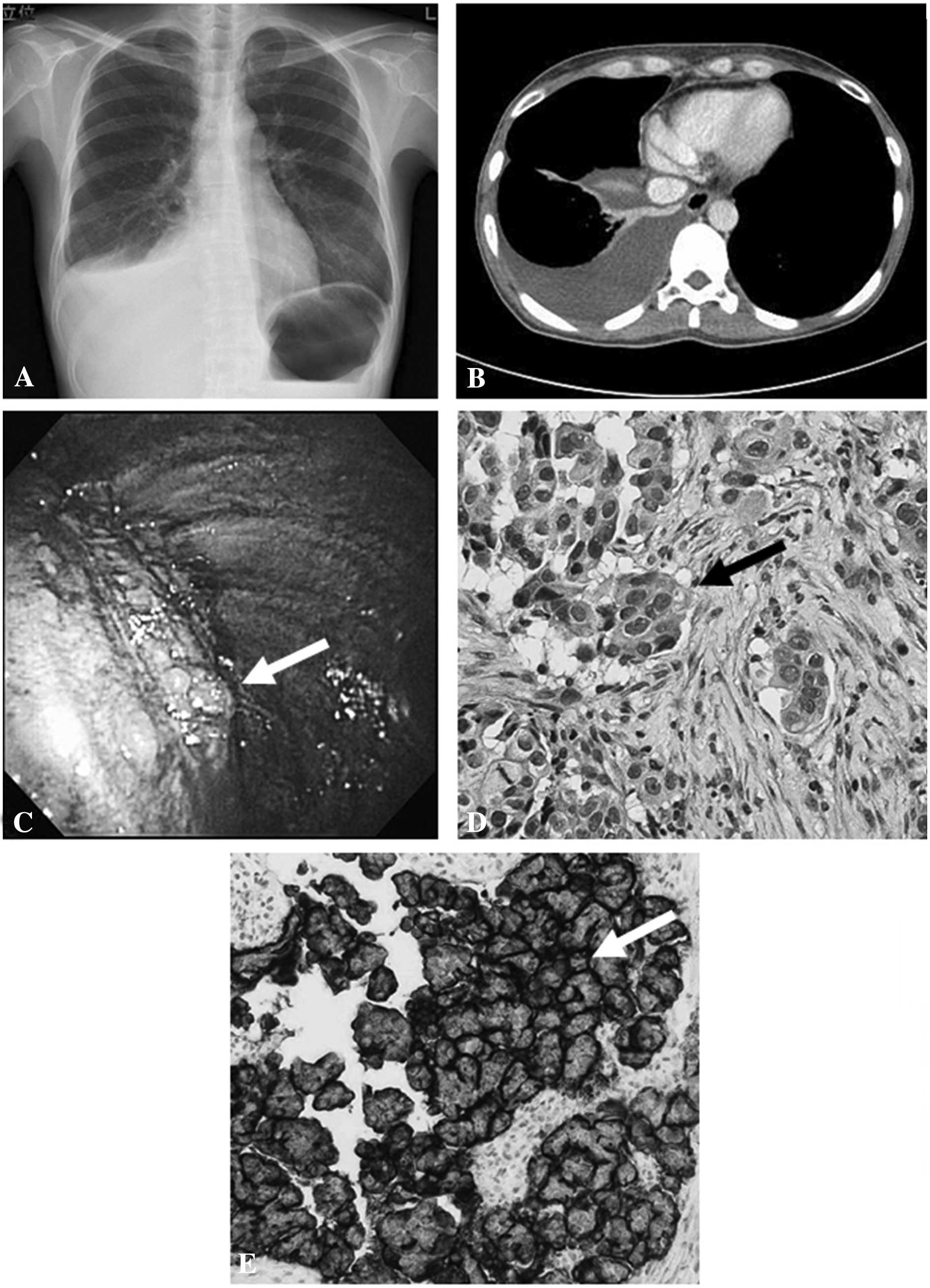
A 46-year-old woman was referred to our hospital
with right pleural effusion on chest radiograph and computed
tomography (CT) (Fig. 1A and B).
Her chief complaints were coughing and exertional dyspnea. She
underwent diagnostic thoracentesis and cytological examination of
pleural effusion showed adenocarcinoma cells. We could not detect
the origin of the adenocarcinoma on chest and abdominal CT,
gastroscopy, physical examination and gynecological examination.
Serological test revealed highly elevated levels of cancer antigen
125 (CA-125) (761.6 U/ml; normal <28) and KL-6 (6991 U/ml;
normal <500). Thoracoscopy was performed under local anesthesia,
and multiple small nodular lesions of parietal pleura were observed
(Fig. 1C). Histopathological and
immunohistochemical analyses of pleural lesions showed poorly
differentiated adenocarcinoma originating in the ovary or
endometrium; the lesion was positive for CA-125, cytokeratin (CK)
7, epithelial membrane antigen (EMA), and vimentin, and negative
for thyroid transcription factor (TTF)-1, CK20, calretinin,
carcinoembryonic antigen (CEA) and gross cystic disease fluid
protein (GCDFP)-15 (Fig. 1D and
E). Magnetic resonance imaging (MRI) suggested the possibility
of an ovarian tumor. She received chemotherapy involving paclitaxel
plus carboplatin and abdominal surgery. She achieved a good
response, and the serum levels of CA-125 and KL-6 decreased to
normal levels (7.9 and 284 U/ml, respectively). Her final diagnosis
was stage IV ovarian serous papillary carcinoma.
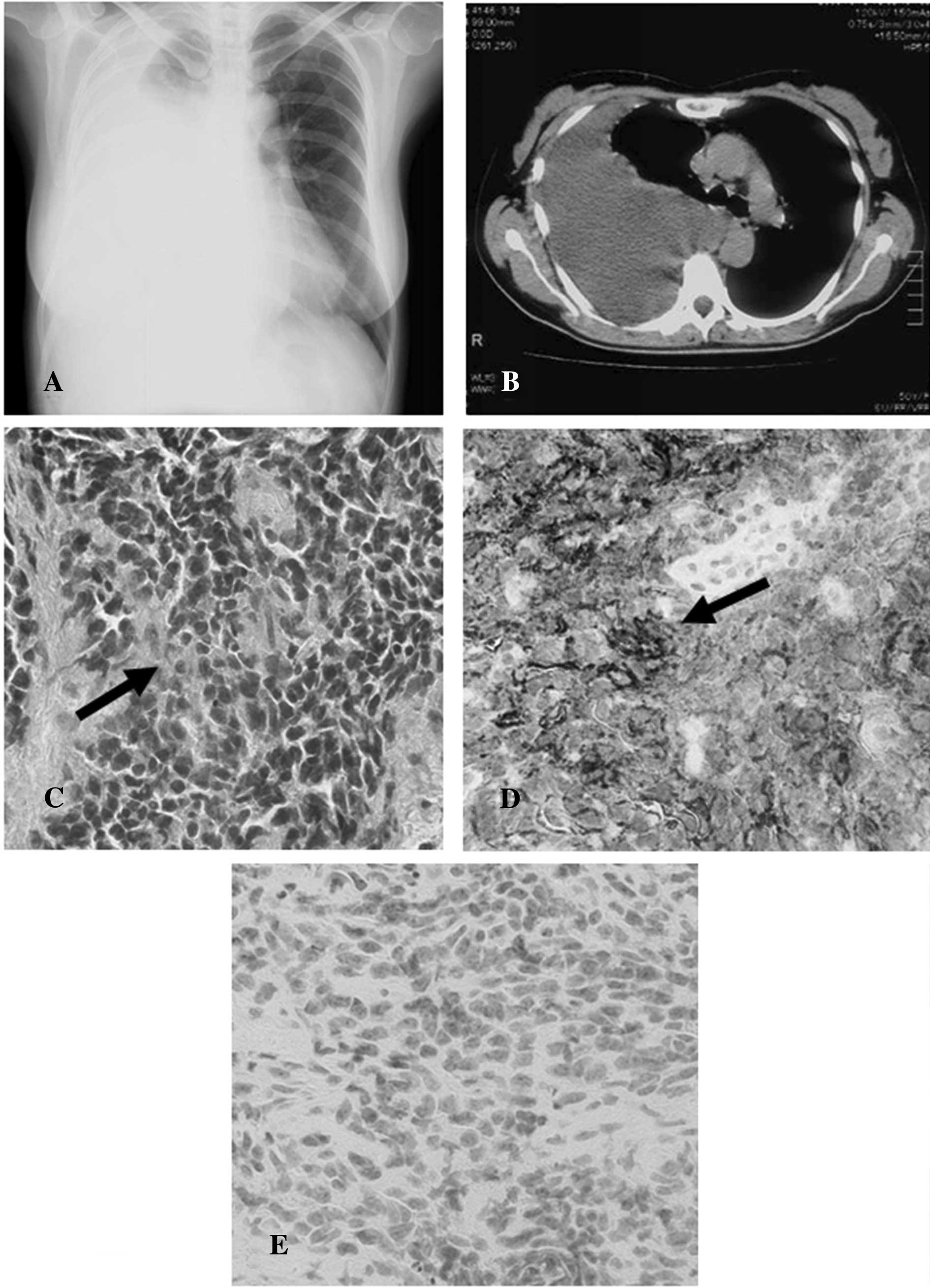
Case 2
A 50-year-old woman was admitted to our hospital
with complaints of coughing and dyspnea. Chest radiograph and CT
indicated right pleural effusion (Fig.
2A and B), and a cytological examination of the pleural
effusion suspected cancerous cells. We were unable to determine the
origin of the cancer on chest and abdominal CT, positron emission
tomography (PET)-CT, physical examination, and gynecological
examination. Serological test revealed elevated levels of CA-125
(211.1 U/ml) and KL-6 (791 U/ml). Thoracoscopy under general
anesthesia showed multiple small nodular lesions of the parietal
pleura and histopathological analyses of pleural lesions showed
adenocarcinoma (Fig. 2C). Since we
suspected lung adenocarcinoma or CUP, the patient received 4
courses of gemcitabine plus cisplatin. She achieved a good
response, and the serum levels of CA-125 and KL-6 were decreased
(13 and 490 U/ml, respectively). Approximately 2 years following
the initial examin ation, she was admitted to our hospital with a
complaint of abdominal fullness. Although chest CT showed no
thoracic lesion, abdominal CT indicated ascites and a pelvic mass
involving the left ovary. Serological test revealed re-elevated
level of CA-125 (122.1 U/ml). To identify the origin of the
previously diagnosed cancer, we re-examined the specimens of
pleural lesions. Immunohistochemical staining revealed that the
samples were positive for CA-125 and CK7, and negative for TTF-1,
CK20 and calretinin (Fig. 2D and
E). Taking into account both immunohistochemical analyses and
her clinical course, the patient was diagnosed with ovarian
adenocarcinoma.
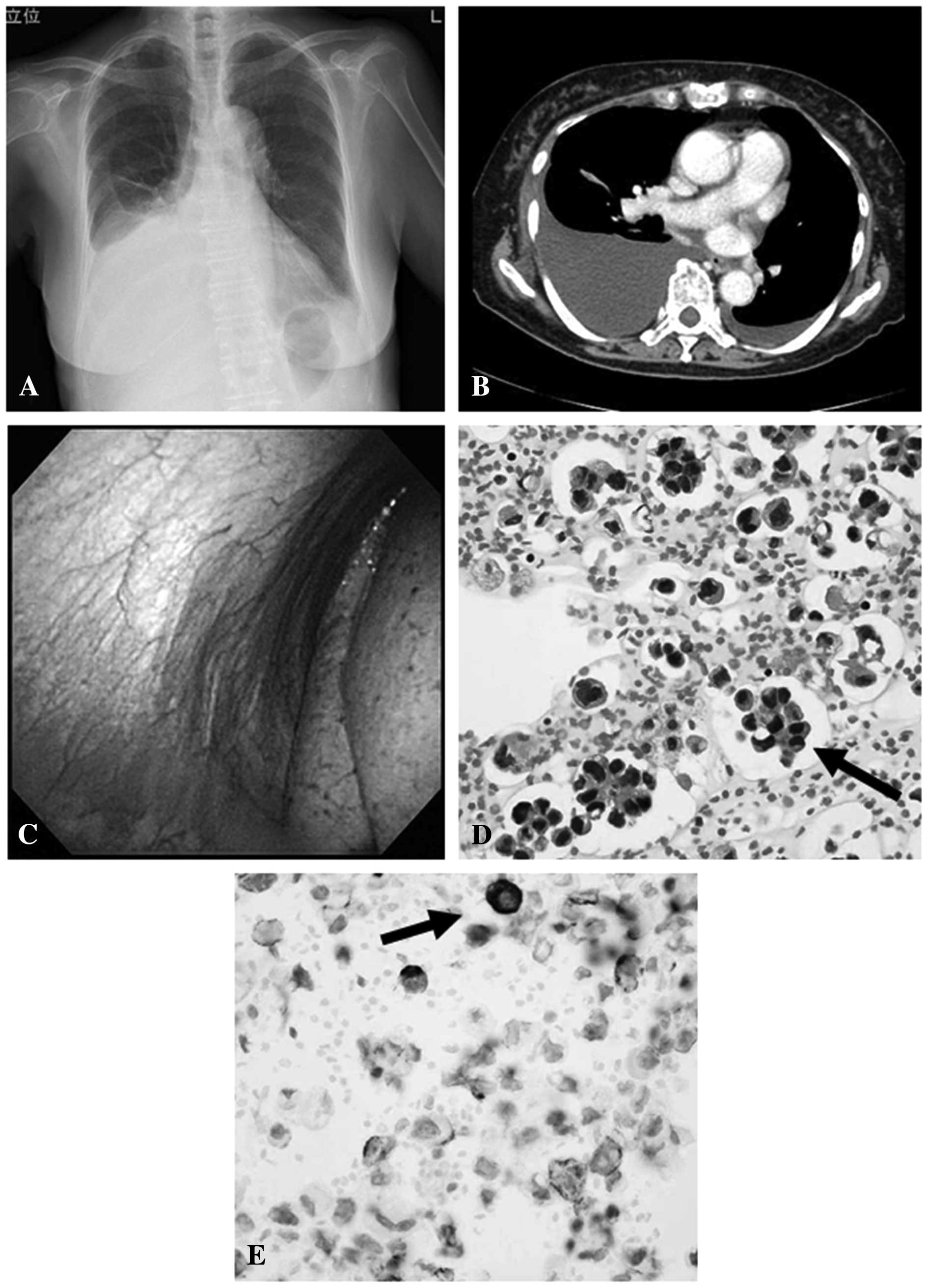
Case 3
An 81-year-old woman with a complaint of dyspnea was
referred to our hospital with pleural effusion on the chest
radiograph and CT (Fig. 3A and B).
Cytological examination of pleural effusion showed carcinoma cells.
Serological examination revealed slightly elevated CA-125 (34.5
U/ml) and normal KL-6 (129 U/ml). We were unable to detect the
origin of the carcinoma cells on chest and upper abdominal CT,
physical examination and gynecological examination at the initial
visit. Thoracoscopy under local anesthesia showed no lesion of the
parietal pleura, and biopsies of the pleura showed normal tissue
(Fig. 3C). Further analysis of the
pleural fluid obtained by thoracoscopy suggested adenocarcinoma
originating in the ovary; immunohistochemical examination of a
pleural fluid cell block showed positive results for CA-125, CK7,
CA19-9, CEA, epithelial antigen (Ber-EP4), and vimentin, and
negative results for TTF-1, CK20, calretinin, CK5/6, caudal-type
homeobox transcription factor-2 (CDX-2) and GCDFP-15 (Fig. 3D and E). PET-CT revealed a pelvic
tumor involving the left ovary and small peritoneal dissemination.
Therefore, the patient was diagnosed with stage IV ovarian
adenocarcinoma.
Discussion
We report three cases of ovarian adenocarcinomas
diagnosed by thoracoscopy. All of the patients were middle-aged and
elderly women with pleural effusion. Two of the three patients
underwent thoracoscopy under local anesthesia and one patient
underwent surgery under general anesthesia. Elevated levels of
serum CA-125 and KL-6 were observed in two patients, and these
markers indicated the state of the disease.
Diagnostic thoracoscopy under local anesthesia is a
safe and effective technique in the work-up of a patient with
pleural effusion of CUP (1–3). In
Western countries, thoracoscopy under local anesthesia is called
medical thoracoscopy, and it is an established tool used to aid
diagnosis, particularly in patients with exudative pleural effusion
of unclear origin (5,6). Diagnostic medical thoracoscopy for
pleural effusions can be used to identify pleural lesions caused by
malignancy with >90% precision, and pathological examination of
biopsy specimens provides useful information for the diagnosis of
primary lesions (2). Herein, we
describe two patients with exudative pleural effusion who were
accurately and safely diagnosed with ovarian cancer by medical
thoracoscopy. Since medical thoracoscopy is relatively easily
performed by pulmonologists, further utilization of this technique
should be promoted at Japanese clinical sites.
The most common extra-abdominal site of ovarian
cancer is the pleural space, and lung parenchymal involvement is
relatively rare (11). In numerous
ovarian cancer cases, abdominal symptoms are usually predominant
and cases with only intrathoracic lesions are rare (9,11).
Ovarian cancer cases with isolated malignant pleural effusion are
likely to be categorized as CUP at the time of initial diagnosis
(4,9). In previous reports, in approximately
10–15% of patients, who were initially diagnosed with CUP, the
cancer origin was ultimately detected; however, ovarian cancer
accounts for only 2–4% of such cases (9,12).
In our cases, adequate sampling of tumor tissues or cells using
thoracoscopy and immunohistochemical examinations were useful in
the identification of the tumor origin.
Although serum tumor markers can be helpful in
certain CUP cases, routine evaluation of commonly used epithelial
tumor markers, namely CEA, CA19-9, CA15-3 and CA-125, has no proven
diagnostic value (4). With regard
to ovarian cancer, almost 80% of cases exhibit elevated serum
CA-125 levels, but the specificity of this measurement is
insufficient for the diagnosis (11,13).
A recent report described an association between increased KL-6
levels and ovarian cancer, therefore, KL-6 is a useful tumor marker
for ovarian cancer (14).
KL-6 is a circulating high-molecular-weight
glycoprotein classified as MUC1 mucin, and is widely accepted as a
marker for interstitial lung disease (15–17).
Originally, KL-6 was introduced as a tumor marker for lung cancer,
and elevated serum KL-6 levels were observed in 30–60% patients
with lung adenocarcinoma, pancreatic cancer and breast cancer
(15). Furthermore, in ovarian
cancer cases, approximately 38% of patients exhibited increased
levels of serum KL-6 (14).
Although the mechanism of serum KL-6 elevation in cancer patients
is not clarified, serum KL-6 is suspected to be derived from cancer
cells (14,16). In a previous report, the serum
levels of KL-6 and CA-125 were correlated with each other and they
indicated the state of disease in patients with advanced and/or
relapsed phase ovarian cancer (14). These phenomena were also observed
in our cases; therefore, KL-6 is believed to be a useful tumor
marker for diagnosing advanced ovarian cancers. Further
investigations of our findings are warranted, and the biological
mechanisms should be evaluated in detail.
In summary, we describe 3 cases of ovarian cancer
with plural effusion diagnosed by thoracoscopy, including medical
thoracoscopy. Although the early diagnosis of ovarian cancer was
difficult in our cases, the measurement of serum KL-6 and CA-125
levels and immunohistochemical analyses should have been useful.
Our report may provide additional information on the clinical
significance of medical thoracoscopy and measurement of serum
KL-6.
References
|
1
|
McLean AN, Bicknell SR, McAlpine LG and
Peacock AJ: Investigation of pleural effusion: an evaluation of the
new Olympus LTF semiflexible thoracofiberscope and comparison with
Abram’s needle biopsy. Chest. 114:150–153. 1998.PubMed/NCBI
|
|
2
|
Kaburagi T, Kuroda H and Amemiya R:
Thoracoscopy under local anesthesia focusing on findings of
carcinomatous pleurisy. Kikanshigaku (J Jpn Society Bronchology).
26:326–330. 2004.
|
|
3
|
Canto A, Rivas J, Saumench J, Morera R and
Moya J: Points to consider when choosing a biopsy method in cases
of pleurisy of unknown origin. Chest. 84:176–179. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pavlidis N, Briasoulis E, Hainsworth J and
Greco FA: Diagnostic and therapeutic management of cancer of an
unknown primary. Eur J Cancer. 39:1990–2005. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Casal RF, Eapen GA, Morice RC and Jimenez
CA: Medical thoracoscopy. Curr Opin Pulm Med. 15:313–320. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Narushima M, Matsuishi J, Yamashita J and
Suzuki H: Current situations of medical thoracoscopy for pleural
deseases in Japan. Kikanshigaku (J Jpn Society Bronchology).
26:711–716. 2004.
|
|
7
|
Johnston WW: The malignant pleural
effusion. A review of cytopathologic diagnoses of 584 specimens
from 472 consecutive patients. Cancer. 56:905–909. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kobayashi Y, Terauchi F, Nishi H, Fujitou
A, Itou H and Isaka K: A case of advanced ovarian cancer upstaged
on the bases of pleural washing cytology. J Obstet Gynaecol Res.
35:588–592. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fukuoka T, Matsuoka E, Chiba S, Takayama S
and Ohono S: Ovarian cancer that was initially diagnosed as
malignant pleural effusion of unknown primary origin. J Rural Med.
4:41–44. 2009. View
Article : Google Scholar
|
|
10
|
Chernow B and Sahn SA: Carcinomatous
involvement of the pleura: an analysis of 96 patients. Am J Med.
63:695–702. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cannistra SA: Cancer of the ovary. N Engl
J Med. 351:2519–2529. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nystrom JS, Weiner JM,
Heffelfinger-Juttner J, Irwin LE, Bateman JR and Wolf RM:
Metastatic and histologic presentations in unknown primary cancer.
Semin Oncol. 4:53–58. 1977.PubMed/NCBI
|
|
13
|
Topalak O, Saygili U, Soyturk M, et al:
Serum, pleural effusion, and ascites CA-125 levels in ovarian
cancer and nonovarian benign and malignant diseases: a comparative
study. Gynecol Oncol. 85:108–113. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Matsunaga T, Hiraiwa T, Kodaira H and Imai
K: KL-6 is useful tumor marker for ovarian cancer. Nihon Fujinka
Shyuyou Gakkai Zasshi (Jpn J Gynecol Oncol). 26:387–393. 2008.
|
|
15
|
Kohno N, Akiyama M, Kyoizumi S, Hakoda M,
Kobuke K and Yamakido M: Detection of soluble tumor-associated
antigens in sera and effusions using novel monoclonal antibodies,
KL-3 and KL-6, against lung adenocarcinoma. Jpn J Clin Oncol.
18:203–216. 1988.PubMed/NCBI
|
|
16
|
Miyazaki K, Kurishima K, Kagohashi K, et
al: Serum KL-6 levels in lung cancer patients with or without
interstitial lung disease. J Clin Lab Anal. 24:295–299. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ohnishi H, Yokoyama A, Kondo K, et al:
Comparative study of KL-6, surfactant protein-A, surfactant
protein-D, and monocyte chemoattractant protein-1 as serum markers
for interstitial lung diseases. Am J Respir Crit Care Med.
165:378–381. 2002. View Article : Google Scholar : PubMed/NCBI
|