Introduction
Endoscopic mucosal resection (EMR) and endoscopic
submucosal dissection (ESD) were developed for the treatment of
benign lesions and early superficial esophageal cancers in the
gastrointestinal (GI) tract (1).
EMR is typically used for the removal of lesions smaller than 2 cm
or for the piecemeal removal of larger lesions. For the removal of
larger lesions, ESD is usually required (1). EMR has been established as a
treatment for superficial esophageal cancer due to its minimal
invasiveness and excellent survival rate (2,3) and
ESD enables the resection of widespread neoplasia, including
Barrett’s esophageal cancer (4,5).
However, esophageal strictures frequently develop in patients who
undergo EMR/ESD (6). Esophageal
stricture may seriously interfere with the oral intake of food and
fluids, and thus lead to a decline in patients’ quality of life.
More significantly, once severe esophageal stricture has developed,
it is difficult to reverse the condition.
A number of methods have been reported to prevent
esophageal stricture following EMR/ESD (7–9).
Among them, balloon dilatation (BD) has been indicated as a
frequently used technique for alleviating esophageal strictures
post EMR/ESD. A retrospective study revealed that preventive BD
reduced the incidence of esophageal stricture in patients who
underwent an extensive EMR/ESD (10). However, the efficacy of preventive
BD requires further confirmation. In the present study, we carried
out a prospective randomized trial between September 2008 and
September 2011 on 30 cases who received EMR/ESD treatment in our
hospital.
Patients and methods
Patients
Between September 2008 and September 2011, 30
patients, including 9 cases with postoperative benign tumors and 21
cases with postoperative early-stage mucosal lesions, were enrolled
in the study (Table I). Twelve
patients received preventive BD 2 weeks after EMR/ESD therapy and
18 patients who had undergone EMR/ESD treatment served as a
control. Written informed consent was obtained from all patients
prior to carrying out EMR/ESD and BD. The study was approved by the
Ethics Committees of the People’s Hospital of Lishui.
 | Table IPatients’ backgrounds. |
Table I
Patients’ backgrounds.
| Gender
| Diseases
| Therapy
|
|---|
| Group | Male | Female | Benign tumor | Early lesion | EMR | ESD |
|---|
| Control | 9 | 9 | 5 | 13 | 5 | 13 |
| Treatment | 6 | 6 | 4 | 8 | 3 | 9 |
Treatment protocol
EMR/ESD treatment was performed according to
previously described methods (11,12).
The patients in the control group underwent common endoscopic
re-examination. For patients receiving preventive BD, routine blood
tests, clotting and bleeding time tests and an electrocardiogram
(ECG) were performed prior to the treatment. Following 8 h of
fasting, 0.5 mg atropine and 10 mg diazepam were injected
intramuscularly. The local area was anesthetized with lidocaine
mortar and the lubricated balloon catheter was inserted. The
balloon was positioned at the center of the primary lesion and then
inflated carefully with air to reach a pressure of 6 psi under the
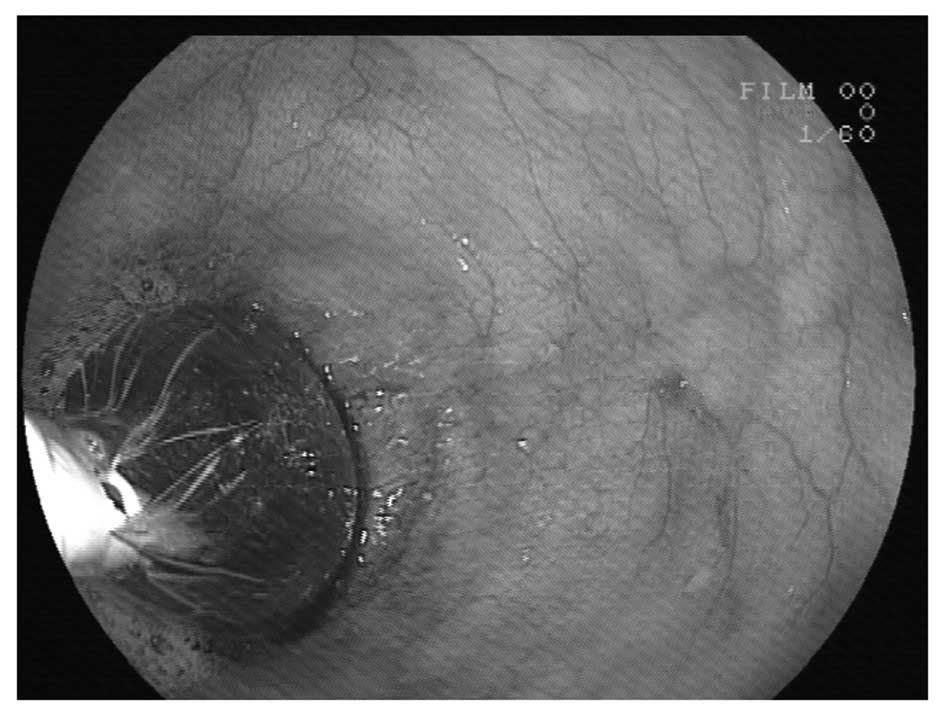
control of a pressure pump (Fig.
1). This dilatation was maintained for 1–3 min according to the
patient’s situation, and the wound was monitored for bleeding. If
bleeding occurred, it suggested that the dilatation was efficient
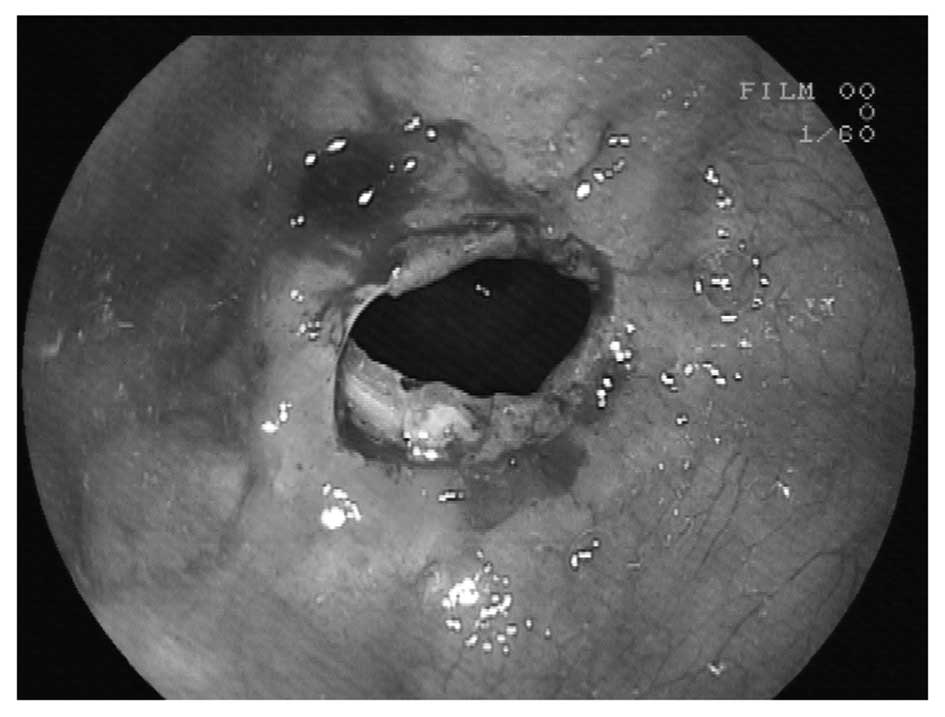
(Fig. 2). The air was then
released, the dilatation was repeated 3 min later and the balloon
was then removed. Gastroscopy was used to observe the extent of the
expansion of the stenosis and the possible complications (Fig. 3). During the procedure, the pulse,
blood pressure and oxygen saturation of the patient were closely
observed.
Results
Efficacy of preventive BD
In the treatment group, every patient was treated
with preventive BD only once and the result was observed to be
satisfactory. One year follow-up revealed that no complications,
including esophageal stenosis, dysphagia, esophageal perforation,
heavy bleeding or mortality, had occurred. However, in the control
group, seven cases experienced dysphagia, of which two were
released without clinical treatment and the other five were
released following two or three BD procedures (Table II).
 | Table IIPatients’ conditions following
EMR/ESD. |
Table II
Patients’ conditions following
EMR/ESD.
| | Dysphagia
| | |
|---|
| Group | Preventive BD | Transient | Persistent | Dilatation | Complications |
|---|
| Control | 0 | 2 | 5 | 5 | 0 |
| Treatment | 12 | 0 | 0 | 0 | 0 |
Discussion
EMR and ESD are efficient endoscopic techniques for
minimally invasive therapy. However, the occurrence rate of
cicatricial stenosis of postoperative esophageal diseases is 6–26%
(13). Stenosis of the esophagus
seriously affects the patients’ quality of life and causes certain
complications, including poor nutrition. Dilatation at an early
stage may alleviate the severity of the stenosis and, to some
extent, avoid the formation of permanent cicatricial stenosis at
later stages which may result in esophageal reconstruction due to
dysphagia. BD using endoscopic guidance has been demonstrated to be
very efficient for the treatment of esophageal stenosis (14). The balloon is able to apply
pressure uniformly all around the esophagus, leading to the
breakdown of fibrous scar tissue bundles around the stenosis and
even the breakdown of muscle fibers and the subsequent relaxation
of the esophageal lumen (1). BD
therapy has the advantages of uniform pressure, being doubly
controlled by the endoscope and the sensations of the patients.
With these advantages, it is easy to control the extent of
dilatation, avoid complications and obtain a clear field to
increase the safety and success rate. Therefore, BD has been
considered as the most favorable method for the treatment of
esophageal stenosis and as a substitute for surgery (1,15).
In the present study, no esophageal stenosis occurred in the
patients treated with preventive BD in the one year follow-up
period, whereas in the control group, five cases reported serious
dysphagia and were treated several times with BD, indicating that
preventive BD was able to prevent long-term complications in
patients undergoing EMR/ESD. The current study indicates that
patients with a wound area affecting over two-thirds of the
esophageal lumen following EMR/ESD for esophageal diseases should
receive preventive BD at an early stage to avoid esophageal
stenosis and improve the quality of life.
In conclusion, the current study indicates that
preventive BD may be considered as an effective therapy to reduce
the incidence of esophageal stenosis following EMR/ESD. Since there
is no other effective method for avoiding esophageal stenosis
following EMR/ESD at present, preventive BD should be considered
for all patients who undergo EMR/ESD. However, there are also
certain shortcomings of the present study. Firstly, the number of
patients is rather small, which limits the credibility of the
study. Secondly, the follow-up period of the patients is only one
year and certain complications may not have yet arisen. Therefore,
further studies that include more patients and are maintained for a
longer period are required to confirm the effectiveness of
preventive BD for the prevention of esophageal stenosis following
EMR/ESD in patients with early stage esophageal cancer.
Acknowledgements
This study was supported by a grant
from the Science and Technology Bureau of Lishui, Zhejiang province
(No. 20100416).
References
|
1
|
ASGE Technology Committee; Kantsevoy SV,
Adler DG, Conway JD, et al: Endoscopic mucosal resection and
endoscopic submucosal dissection. Gastrointest Endosc. 68:11–18.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Inoue H: Treatment of esophageal and
gastric tumors. Endoscopy. 33:119–125. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Inoue H, Tani M, Nagai K, et al: Treatment
of esophageal and gastric tumors. Endoscopy. 31:47–55. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Satodate H, Inoue H, Yoshida T, et al:
Circumferential EMR of carcinoma arising in Barrett’s esophagus:
case report. Gastrointest Endosc. 58:288–292. 2003.
|
|
5
|
Fujishiro M, Yahagi N, Kakushima N,
Kodashima S, Ichinose M and Omata M: En bloc resection of a large
semicircular esophageal cancer by endoscopic submucosal dissection.
Surg Laparosc Endosc Percutan Tech. 16:237–241. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim SH and Lee SO: Circumferential
intramural esophageal dissection successfully treated by endoscopic
procedure and metal stent insertion. J Gastroenterol. 40:1065–1069.
2005. View Article : Google Scholar
|
|
7
|
Yamaguchi N, Isomoto H, Shikuwa S, et al:
Effect of oral prednisolone on esophageal stricture after complete
circular endoscopic submucosal dissection for superficial
esophageal squamous cell carcinoma: a case report. Digestion.
83:291–295. 2011. View Article : Google Scholar
|
|
8
|
Alshammari J, Quesnel S, Pierrot S and
Couloigner V: Endoscopic balloon dilatation of esophageal
strictures in children. Int J Pediatr Otorhinolaryngol.
75:1376–1379. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
de Wijkerslooth LR, Vleggaar FP and
Siersema PD: Endoscopic management of difficult or recurrent
esophageal strictures. Am J Gastroenterol. 106:2080–2091. 2011.
|
|
10
|
Ezoe Y, Muto M, Horimatsu T, et al:
Efficacy of preventive endoscopic balloon dilation for esophageal
stricture after endoscopic resection. J Clin Gastroenterol.
45:222–227. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Soetikno R, Kaltenbach T, Yeh R and Gotoda
T: Endoscopic mucosal resection for early cancers of the upper
gastrointestinal tract. J Clin Oncol. 23:4490–4498. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fujishiro M, Yahagi N, Kakushima N, et al:
Endoscopic submucosal dissection of esophageal squamous cell
neoplasms. Clin Gastroenterol Hepatol. 4:688–694. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Petrin G, Ruol A, Battaglia G, et al:
Anastomotic stenoses occurring after circular stapling in
esophageal cancer surgery. Surg Endosc. 14:670–674. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lv XP, Jiang HX, Tang GD, Qin LR, Tan ZR
and Qin SY: Treatment of endoscopic probe dilation in
esophagostenosis. China J Endoscopy. 13:22–23. 262007.(In
Chinese).
|
|
15
|
Cho YK, Shin JH, Kim BS, et al:
Fluoroscopically guided balloon dilation of anastomotic strictures
after total gastrectomy: long-term results. AJR Am J Roentgenol.
188:647–651. 2007. View Article : Google Scholar : PubMed/NCBI
|