Introduction
Chiari malformation (CM), also known as
Arnold-Chiari malformation, is a congenital developmental
malformation characterized by a downward displacement of the
cerebellar tonsils into the spinal canal due to the reduced
capacity of the posterior cranial fossa. CM may be complicated by a
variety of other malformations, including platybasia, basilar
invagination and occipitalization, although syringomyelia (SM) is
the most commonly observed.
In 1883, Cleland first described brainstem and
cerebellar displacements and SM (1). Chiari made successive attempts to
classify these malformations into various types according to the
severity of the downward displacement of the neural axis in the
skull-vertebra transitional area and types I–IV were defined: i)
type I, displacement of the cerebellar tonsils and the medial
portions of the inferior lobes of the cerebellum which follow the
bulb inside the cervical canal; ii) type II, displacement of the
lower portions of the cerebellum, pons, medulla and part of the
elongated IV ventricle inside the cervical canal; iii) type III,
significant portions of the cerebellum and brainstem are dislocated
caudally and the orifices of the IV ventricle open into the
cervical canal, reshaping the cervical hydrocephalus through spina
bifida of the first three cervical vertebrae; and iv) type IV,
hypoplasia of the cerebellum without a caudal displacement of the
brainstem (2,3). Later, in 1894, Arnold, a German
pathologist, added further detail to the descriptions of these
malformations (4). Schwalbe and
Gredig suggested the term ‘Arnold-Chiari malformation’ to refer to
the condition in 1907 (5), whereas
Sarnat and Williams named it Chiari malformation (CM) or cerebellar
tonsil downward displacement malformation in terms of the primary
clinical manifestation of the condition (6,7).
Further studies have since been dedicated to evaluating the
occipitocervical malformations (8–10).
CM manifests as a variety of clinical symptoms,
principally including spinal canal impairment, a dissociated
sensory disorder of the limbs and body and muscular atrophy
(particularly of the upper limbs); nerve root irritation, causing
painful or burning sensations in the neck, shoulders, back or upper
limbs; posterior group cranial neural and cerebellar disorders,
causing instability of gait, nystagmus, dysphagia and hoarseness;
pyramidal tract impairment, causing hypermyotonia, tendon
hyperreflexia and loss of muscle strength; and intracranial
hypertension, causing headaches, emesis and papilledema. At
present, CM diagnosis is mainly based on a combination of clinical
manifestations and magnetic resonance imaging (MRI) of the
occipitocervical area. The radiographic criteria for diagnosing CM
include cerebellar tonsillar herniation into the spinal canal (a
downward herniation of the cerebellar tonsils >5 mm below the
foramen magnum), decreased posterior fossa capacity, cisterna magna
shrinkage or disappearance, and compression against and
malformations of the cervical cord and IV ventricle or
displacements toward the spinal canal. For patients with confirmed
CM, surgery is the only effective therapeutic measure, where
decompression of the suboccipital region is performed in order to
re-form the cisterna magnum. However, since certain patients
exhibit no neurological improvement, surgical treatment remains
controversial with regard to the size of the bone window for
decompression, whether the dura mater should be opened, how the
herniated tonsils should be treated and whether syrinx drainage is
required.
The present study was intended to resolve these
issues concerning the surgical treatment of CMI based on clinical
experience.
Patients and methods
General data
A total of 185 patients with confirmed CMI
(atlantoaxial dislocation and occipitocervical instability were
excluded) were enrolled in the present study. Of the patients, 82
were male and 103 were female. The duration of the disease ranged
between 7 days and 12 years with an average of 3.7 years. The
patients’ ages ranged between 15 and 68 years with an average of
43.5 years. CMI occurred in 21 patients <21 years old, 118
(63.8%) between 25 and 45 and 46 of >45.
The study was conducted in accordance with the
Declaration of Helsinki and approved by the Ethics Committee of the
Affiliated Hospital of Luzhou Medical College (Luzhou, China).
Written informed consent was obtained from all participants.
Clinical manifestations
Clinical manifestations were as follows: i) spinal
canal impairment symptoms: 132 patients exhibited dissociated
sensory disorders of the limbs and body and 61 exhibited muscle
atrophy in the hands or upper limbs; ii) nerve root irritation
symptoms: 74 patients had painful and burning sensations in the
neck, shoulders, back or upper limbs; iii) posterior group cranial
neural and cerebellar disorders: instability of gait, nystagmus,
and dysphagia and hoarseness were observed in 36, 24 and 16
patients, respectively; iv) pyramidal tract impairment symptoms: 68
patients were diagnosed with hypermyotonia, tendon hyperreflexia
and loss of muscle strength; and v) increased intracranial pressure
signs and symptoms: 16 patients were identified as having
headaches, emesis and papilledema.
MRI
Occipitocervical MRI revealed that the downward
herniations of the cerebellar tonsils in the patients ranged from 3
to 19 mm with an average of 9.35 mm. A total of 146 patients had a
herniation >5 mm below the lower border of the foramen magnum
and 39 had a herniation 3–5 mm below. A spinal syrinx confined to
the cervical region was observed in 46 patients, while 139 had a
cervical and thoracic syrinx. The ratio between the diameter of the
spinal syrinx and that of the spinal cord was <0.35 for 132
patients and 53 had a ratio of >0.35. All patients exhibited a
marked decrease in the size of or even the disappearance of the
cisterna magna. The complications observed were as follows: 51
patients with basilar impression, 38 with platybasia, 32 with
occipitalization, 67 with scoliosis, 16 with neuropathic
arthropathy and 17 with hydrocephalus.
Surgical procedures
All patients underwent surgery in a prone position
with the head fixed using a head rest and the neck slightly
forward, following general anesthesia with tracheal intubation.
Large-bone-window posterior fossa decompression plus
duraplasty was performed on 76 patients. A posterior median
incision was made between 1 cm below the external occipital
protuberance and the spinous process of the third cervical vertebra
(C3) and the squamous part of the occipital bone was
removed up to the posterior border of the foramen magnum. The
processes and laminae of the C1–3 were excised depending
on the severity of the cerebellar tonsil herniation. A 2.5-cm-wide
section of the posterior border of the foramen magnum and 2-cm-wide
section of the posterior arches of the C1–3 were
removed. The thickened occipital fascia was excized under a
microscope, the dura mater was Y-sheared and artificial dura mater
or muscular fascia was then used to expand and repair the dura
mater. The dura mater was suspended on the border of the bone
window and shaped afterwards.
Small-bone-window posterior fossa decompression,
cerebellar tonsillectomy and duraplasty were performed on 109
patients. The same surgical approach was adopted but with removal
of a 3x3 cm section of the occipital bone. The dura mater was then
Y-sheared and the adhesions of the arachnoid to the dura mater and
tonsils and of the tonsils to the brainstem were separated under a
microscope. Cerebellar tonsil electric coagulation was performed
under such conditions that noticeable repositioning did not occur
and the cerebellar tonsils up to 5–10 mm above the level of the
foramen magnum were excised subspially to relieve compression
against the medulla oblongata and cervical cord (attention was also
paid to the relief of the compression of the outer sides of the
cerebellar tonsils against the nerve roots). The median and lateral
apertures of the IV ventricle were detected and possible adhesions
were sufficiently released to guarantee unobstructed IV ventricular
cerebrospinal fluid (CSF) circulation. The dura mater was repaired
with artificial dura mater and then suspended on the border of the
bone window and shaped into the cisterna magna by suturing the
occipital muscle tissues. An external drainage tube was held
outside the dura mater and the incision was sewn up.
Patients turned their bodies over axially following
the surgery. The patients received neck fixation for 2–3 weeks.
Results
Short-term curative effects
The curative effects were evaluated after the
treatment as well as at the time of hospital discharge. The lengths
of the patients’ hospital stays ranged between 10 and 21 days with
an average of 14 days. Symptoms were eliminated or improved in 156
patients (84.3%) and not improved in 29 (15.7%). No symptom
deterioration or mortality occurred. Incisional hydrops were
observed in 8 patients but were healed following drainage and
dressing changes of the wound and no CSF leakage occurred. A total
of 148 patients received MRI within two weeks after operation. The
results revealed that 92 patients (62.2%) had a reconstructed
cisterna magna and 75 (50.7%) had a reduced spinal syrinx.
Long-term curative effects
A total of 147 patients were followed up for 3
months to 12 years, with an average of 3.2 years and 38 patients
(20.5%) were lost to follow-up. The symptoms were eliminated or
improved in 110 patients (74.8%), not improved in 26 (17.7%) and
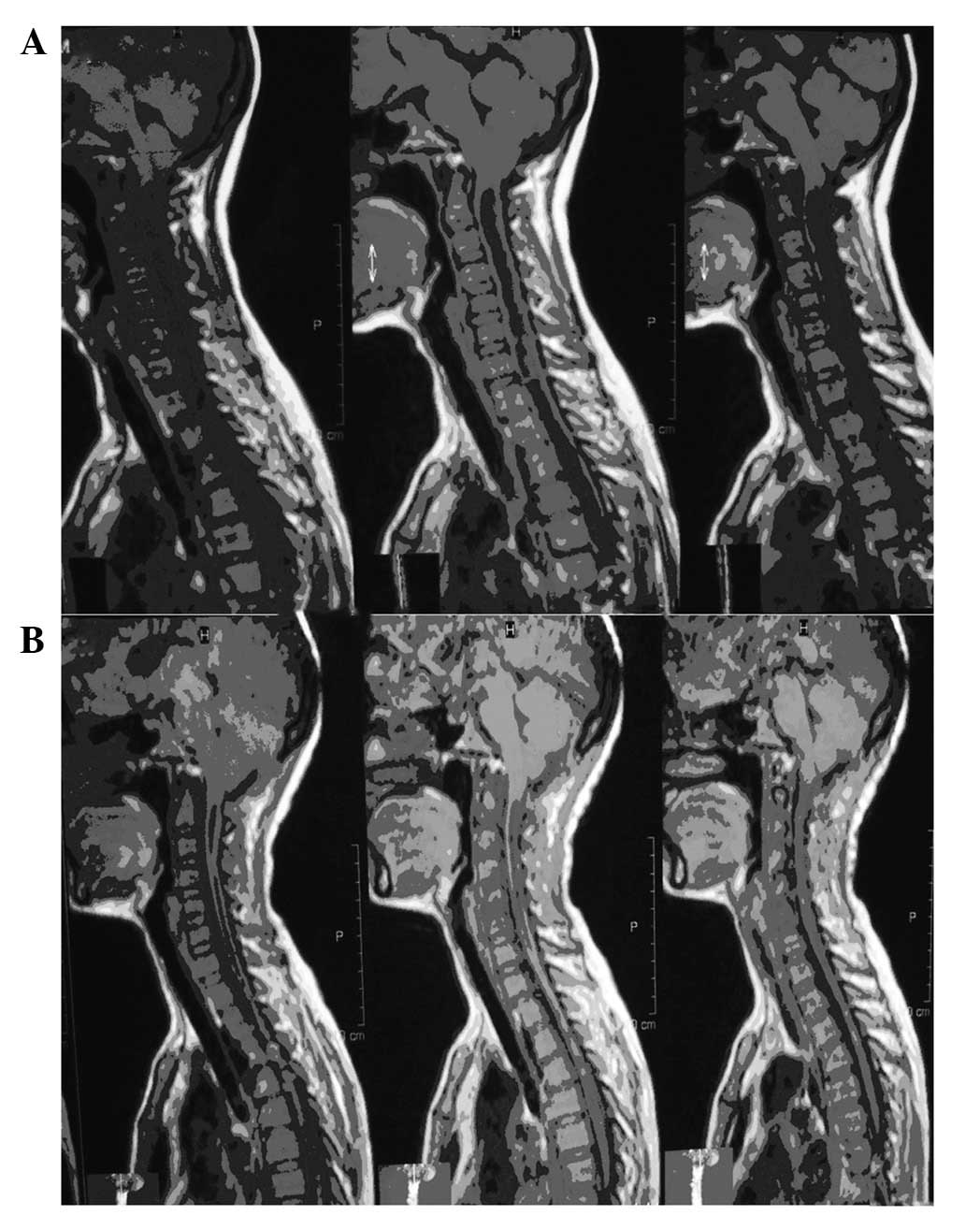
aggravated in 11 (7.5%). MRI was performed for 95 patients and
revealed that the cisterna magna was reconstructed in 87 patients
and spinal syrinx was reduced in 79 (Fig. 1). Long-term complications,
including headaches, fever (relieved after symptomatic treatment)
and CSF leakage (healed after drainage, wound suturing and enhanced
anti-inflammatory treatment) were exhibited by 8 of the patients.
The 11 patients with aggravated symptoms primarily exhibited
aggravation following symptom relief. MRI revealed that 8 of these
patients still had a noticeable spinal syrinx with a ratio between
its diameter and that of the spinal cord of >0.35. The patients
underwent syringo-subarachnoidal (SS) shunting. The remaining 3
patients received further physical and symptomatic treatment.
Symptoms were reduced somewhat in the majority of the patients.
Discussion
A popular hypothesis concerning the pathogenesis of
CMI is that the hindbrain tissues are dislocated into the spinal
canal after birth due to an overcrowded posterior cranial fossa
which is caused by the retarded development of the occipital bone
during the embryonic period (11).
However, the pathogenesis of SM remains controversial. The 3 main
theories which attempt to explain the formation of SM are Gardner’s
hydrokinetics, Williams’ intracranial and intraspinal pressure
separation and Oldfield’s CSF and spinal substance penetration,
none of which is superior to any other (12). Partial obstruction in the foramen
magnum area blocks the normal circulation of CSF which is a major
factor in the development and progression of SM (13). Morphological changes in the
subarachnoid space are important in the development and progression
of SM in that CM patients usually have increased atlanto-occipital
fascia thickness and narrowed or even obstructed cisterna magnae,
in addition to sclerotic structural abnormalities. The longer the
duration of CM and the more severe the condition, the narrower the
subarachnoid space (14). The
false membrane at the orifice of the spinal canal is one of the
causes of intraspinal canal fluid accumulation and the formation of
a syrinx (8).
A reduced posterior fossa capacity and a narrowed
occipitocervical subarachnoid space are key factors in the
development of CMI complicated with SM. CMI is congenital, whereas
SM is acquired. When the obstruction of the subarachnoid space
reaches a certain extent, SM may occur. At present, the main
treatment of CMI complicated with SM is surgery. However, surgical
treatment only stops or retards the disease’s progression rather
than curing the damage caused to the spinal cord. Therefore,
patients exhibiting symptoms should be diagnosed and treated as
early as possible. In the surgical treatment of CMI complicated
with SM, posterior fossa decompression and SS shunting are two
commonly-adopted procedures. With the establishment and development
of the Oldfield theory, numerous studies have indicated that
posterior fossa decompression is the preferred procedure. In this
procedure, the key points include expanding the capacity of the
posterior cranial fossa, reconstructing the absent cisterna magna
and allowing the obstructed CSF to circulate through in order to
make the syrinx disappear and improve the symptoms (Fig. 1) (15–17).
By contrast, since SS shunting cannot aid the return of CSF
circulation to normal and may also increase the risk of spinal cord
injury and infections, despite a certain long-term curative effect,
it is no longer recommended (15–18).
The results of the present study support this since the follow-ups
demonstrated that 79 out of 95 patients (83.2%) who did not undergo
SS shunting exhibited a reduced spinal syrinx.
Previously, posterior fossa decompression alone was
considered to be able to provide an efficient curative effect for
CMI complicated with SM. However, although posterior fossa
decompression alone expands the capacity of the posterior fossa, it
fails to correct CSF pressure separation and reinstate normal CSF
circulation. Therefore, posterior fossa decompression alone has
essentially been excluded from clinical practice for treating CMI
complicated with SM. Instead, a combination of posterior fossa
decompression and duraplasty is widely used. The combined procedure
efficiently solves the problem of a narrowed posterior fossa
capacity by removing C1–2 and reshaping the dura mater
through an occipital bone window, eliminating the compression in
the foramen magnum area and improving the associated clinical
symptoms. Numerous follow-up studies have demonstrated that
posterior fossa decompression combined with duraplasty greatly
improves the clinical symptoms of CMI with SM and reduces the
spinal syrinx (16–18). Nevertheless, the size of the bone
window for decompression is debated. An expanded bone window is
crucial for treating CMI with SM (19). A small bone window for posterior
fossa decompression is capable of achieving an effect as good as a
large one and also reduces the incidence of postoperative
complications. The present study revealed a higher incidence of
complications in the patients receiving large-bone-window
decompression and duraplasty. Early postoperative complications
were primarily manifested as fevers, headaches, CSF leakage,
pseudocyst and spinal arachnoiditis, whereas long-term
postoperative complications mainly included diplopia, tinnitus,
dizziness and limited neck activity. Expanded posterior fossa
decompression and Y-shaped shearing and expanded repair to the dura
mater possibly cause symptoms such as CSF leakage, subcutaneous
hydrops and fevers. Additionally, the wide dissection of the
occipital muscle, excessive removal of the squamous part of the
occipital bone and the resulting backward displacements of the
cerebellum, midbrain and medulla oblongata, which cannot gain
support from the expansively-repaired dura mater, cause
pseudocephalocele. This further pulls on the abducent, acoustic and
trigeminal nerves, leading to a succession of long-term
complications (20). In the
present study, 109 patients underwent small-bone-window
decompression and duraplasty. This procedure not only removes the
compression of the occipitocervical bones and thickened fascia
against the cerebellobulbaris but provides support for the
cerebellum and midbrain to reduce the incidence of neuroses caused
by their excessive drooping and dragging. Furthermore, this
procedure requires less intraoperative muscular dissection which
aids the recovery of the neck and nape (9).
In CMI, the cerebellar tonsils are the contents of
the syrinx as well as the main cause of the compression against the
medulla oblongata which further leads to SM and causes the
associated clinical symptoms. Although the necessity of opening the
arachnoid space to remove the herniated cerebellar tonsils in the
treatment of CMI is debatable (17,21),
the removal approach is preferred and is considered to achieve a
more positive curative effect. The herniated cerebellar tonsils
should be excised subpially, although attention should also be paid
to the median and lateral apertures of the IV ventricle and
adhesions should be sufficiently released to guarantee the smooth
circulation of CSF. For patients with nerve root irritation
symptoms, the compression of the cerebellar tonsils against the
nerve roots should be relieved (22). In the present study, the recovery
following surgery of the patients receiving herniated cerebellar
tonsil exsection was superior to that of the patients who did not
receive such a treatment. The patients who underwent cerebellar
tonsil excision exhibited noticeably shortened recovery times for
nerve root irritation and ataxia and superior muscle strength
recovery. This result indicates that attempts may be made to remove
the herniated cerebellar tonsils to aid patient recovery, on the
assumption of adequate microsurgical experience.
Although satisfactory surgical effects were achieved
in the majority of patients in the present study following
treatment, certain patients did not exhibit significant improvement
of symptoms, particularly spinal canal impairment. This suggests
that surgical treatment only stops or retards rather than radically
eliminates the progression of spinal impairment. Therefore,
patients with symptoms should be diagnosed and surgically treated
as early as possible (22).
In conclusion, CMI complicated with SM is a complex
condition characterized by a variety of manifestations. At present,
there is no agreement with regard to the surgical procedure for
this condition and the curative effects of various procedures
differ. With the development of studies of CMI complicated with SM,
perfection of the surgical procedures and increased knowledge
concerning the condition among medical practitioners, significant
improvements in curative effects may be achieved.
References
|
1
|
Cleland J: Contributions to the study of
spina bifida, encephalocele and anencephalus. J Anat Physyol. 17(Pt
3): 257–292. 1883.PubMed/NCBI
|
|
2
|
Chiari H: Über Veränderungen des
Kleinhirns infolge von Hydrocephalie des Grosshirns. Dtsch Med
Wochenschr. 17:1172–1175. 1891.(In German).
|
|
3
|
Chiari H: Über Veränderungen des
Kleinhirns, des Pons und Medulla Oblongata infolge Von congenitaler
Hydrocephalie des Grosshirns. Denkschr Kais Akad Wiss MathNaturw.
63:71–116. 1896.(In German).
|
|
4
|
Arnold J: Myelocyst transportation Von
Gewebskeimen und Sympodie. Beitr Path Anat Allgem Path. 37:1–28.
1994.(In German).
|
|
5
|
Schwalbe E and Gredig M: Über
Entwicklungsstörungen des Kleinhirns, Hirnstammes und Halsmarks bei
Spina bifida (Arnold’sche Missbildung). Beitr Path Anat.
40:132–194. 1907.(In German).
|
|
6
|
Sarnat HB: Embryology and dysgenesis of
the posterior fossa. Syringomyelia. Current Concepts in Diagnosis
and Treatment. Batzdorf U: Williams and Wilkins; Baltimore:
1991
|
|
7
|
Williams B: Pathogenesis of syringomyelia.
Syringomyelia. Current Concepts in Diagnosis and Treatment.
Batzdorf U: Williams and Wilkins; Baltimore: 1991
|
|
8
|
Zhang YQ, Wang ZC, Ma ZY and Li ZH: Chiari
malformation with syringomyelia: surgical treatment with
tonsillectomy plus central canal opening. Chin J Neurosurg.
20:215–217. 2004.
|
|
9
|
Zhang YZ, Zhou DB, Qiao GY and Sun ZH:
Reconstruction of the cisterna magna to treat the syringomyelia
associate Chiari type I malformation. Chin J Neurosurg. 16:274–276.
2000.(In Chinese).
|
|
10
|
Huang SQ, Xiao QH, Li GP, Cheng YZ, Liu JM
and Liu JG: Microsurgical treatments of Chiari I malformation
associated with syringomyelia: analysis of 310 cases. Chin J
Neurosurg. 21:100–102. 2005.(In Chinese).
|
|
11
|
Furtado SV, Thakre DJ, Venkatesh PK, Reddy
K and Hegde AS: Morphometric analysis of foramen magnum dimensions
and intracranial volume in pediatric Chiari I malformation. Acta
Neurochir (Wien). 152:221–217. 2010.PubMed/NCBI
|
|
12
|
Park YS, Kim DS, Shim KW, Kim JH and Choi
JU: Factors contributing improvement of syringomyelia and surgical
outcome in type I Chiari malformation. Childs Nerv Syst.
25:453–459. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pei XL, Han HB, Liu B and Wang ZY:
Cerebrospinal fluid flow dynamics study in Chiari malformation with
syrinx by using quantitiative phase-contrast MR imaging. Chin J Med
Imaging Technol. 20:985–988. 2004.(In Chinese).
|
|
14
|
Chen HR, Xu MH, Zou YW, Qiao ZC and Wang
Y: Alteration of subarachnoid space in the craniocervical junction
and its clinical significance in the pathogenesis of Chiari
malformation. Chin J Regi Anato Opera Surg. 12:205–208. 2003.(In
Chinese).
|
|
15
|
Brugières P, Idy-Peretti I, Iffenecker C,
et al: CSF flow measurement in syringomyelia. AJNR Am J
Neuroradiol. 21:1785–1792. 2000.
|
|
16
|
Depreitere B, Van Calenbergh F, van Loon
J, Goffin J and Plets C: Posterior fossa decompression in
syringomyelia associated with a Chiari malformation: a
retrospective analysis of 22 patients. Clin Neurol Neurosurg.
102:91–96. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shamji MF, Ventureyra EC, Baronia B, Nzau
M and Vassilyadi M: Classification of symptomatic Chiari I
malformation to guide surgical strategy. Can J Neurol Sci.
37:482–487. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schijman E and Steinbok P: International
survey on the management of Chiari I malformation and
syringomyelia. Childs Nerv Syst. 20:341–348. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Goel A and Desai K: Surgery for
syringomyelia: an analysis based on 163 surgical cases. Acta
Neurochir (Wien). 142:293–301. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Di Lorenze N, Palma L, Palatinsky E and
Fortuna A: ‘Conservative’ cranio-cervical decompression in the
treatment of syringomyelia-Chiari I complex. A prospective study of
20 adult cases. Spine (Phila Pa 1976). 20:2479–2483. 1995.
|
|
21
|
Erdogan E, Cansever T, Secer HI, et al:
The evaluation of surgical treatment options in the Chiari
Malformation Type I. Turk Neurosurg. 20:303–313. 2010.
|
|
22
|
Bao CS, Yang FB, Liu L, et al: Cerebellar
tonsillectomy and reconstruction of the cistern magna for treatment
of syringomyelia with Chiari malformation. J Pract Med. 10:993–995.
2011.(In Chinese).
|