Introduction
With aging of the population, degenerative lumbar
spinal stenosis (DLSS) is becoming an increasingly common spinal
disease. DLSS is often characterized by radiological findings of
multilevel disc herniation and lumbar spondylolisthesis and is
difficult to treat. Although there has been a series of
improvements in surgical technique, the traditional laminectomy
with interbody or posterolateral fusion from the posterior approach
continues to be widely used. However, multilevel fusion causes
great damage to the normal structure, prolongs recovery time and
may result in chronic lower back pain (1). In the current study, we evaluated the
combined use of microendoscopic discectomy (MED) and minimally
invasive transforaminal lumbar interbody fusion (MI-TLIF) for the
treatment of multilevel DLSS with spondylolisthesis, which had
satisfactory short-term clinical outcomes, and compared the
combined surgery with the traditional lumbar interbody fusion from
the posterior midline approach (PLIF).
Materials and methods
Patients
A total of 26 patients with multilevel DLSS and
spondylolisthesis (the minimally invasive group) who underwent
combined MED and TLIF surgery using a single-cage and pedicle
rod-screw system between July 2009 and March 2011 were involved in
the study. In this group, 14 patients were male and 12 were female
with a mean age of 63.4 (range 53–78) years; 14 patients had
stenosis of 2 segments, 12 patients had stenosis of 3 segments and
all had spondylolisthesis of 1 segment. The above cases were
compared with 27 patients (the traditional group) who underwent
traditional PLIF surgery during the same period. In the traditional
group, 15 patients were male and 12 were female; their ages ranged
from 55 to 75 years with an average of 64.9 years; 15 patients had
stenosis of 2 segments, 12 patients had stenosis of 3 segments and
all had spondylolisthesis of 1 segment. Data regarding the incision
length, surgery time, blood loss, time of bed rest and Oswestry
Disability Index (ODI) scores prior to and following surgery were
analyzed statistically. The study was approved by the ethics
committee of China-Japan Union Hospital of Jilin University
(Changchun, China).
All patients had a history of recurrent and
progressive lower back pain and leg pain with intermittent
claudication for 1–20 years, with an average duration of 4.5 years.
They had all undergone systematic conservative treatment for at
least 3 months but had experienced no improvement.
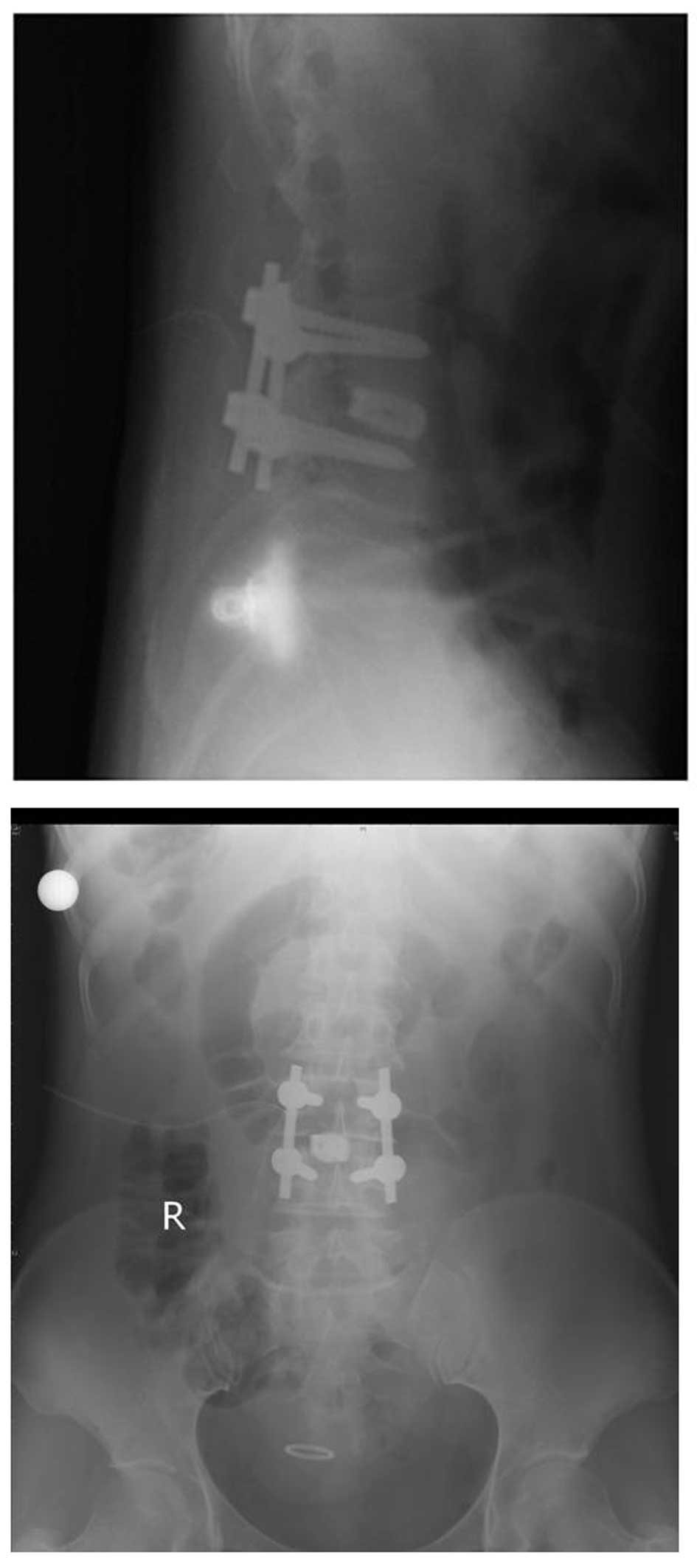
All patients were examined by X-ray imaging of the
lumbar anterior and posterior (AP) view, lateral view and lateral
view of flexion and extension, and by MRI and CT scans. The X-rays
revealed multilevel (2–3 segments) degeneration with
spondylolisthesis of a single segment. CT scans showed stenosis of
the central vertebral canal and the lumbar lateral recess, but the
degree of stenosis differed between individuals. It also
demonstrated the degree of spondylolisthesis. MRI showed the extent
of dural sac compression (Fig. 1).
The levels responsible for the symptoms were determined from the
radiological findings and a gait load test.
Surgical technique
The surgery was performed under general anesthesia.
The patients were placed in a prone position. In the traditional
group, a posterior midline incision was made to access the lamina
of the responsible segments, then laminectomy was performed to
decompress the nerve roots. Posterior segmental spinal
instrumentation was used in all cases, using a single cage and
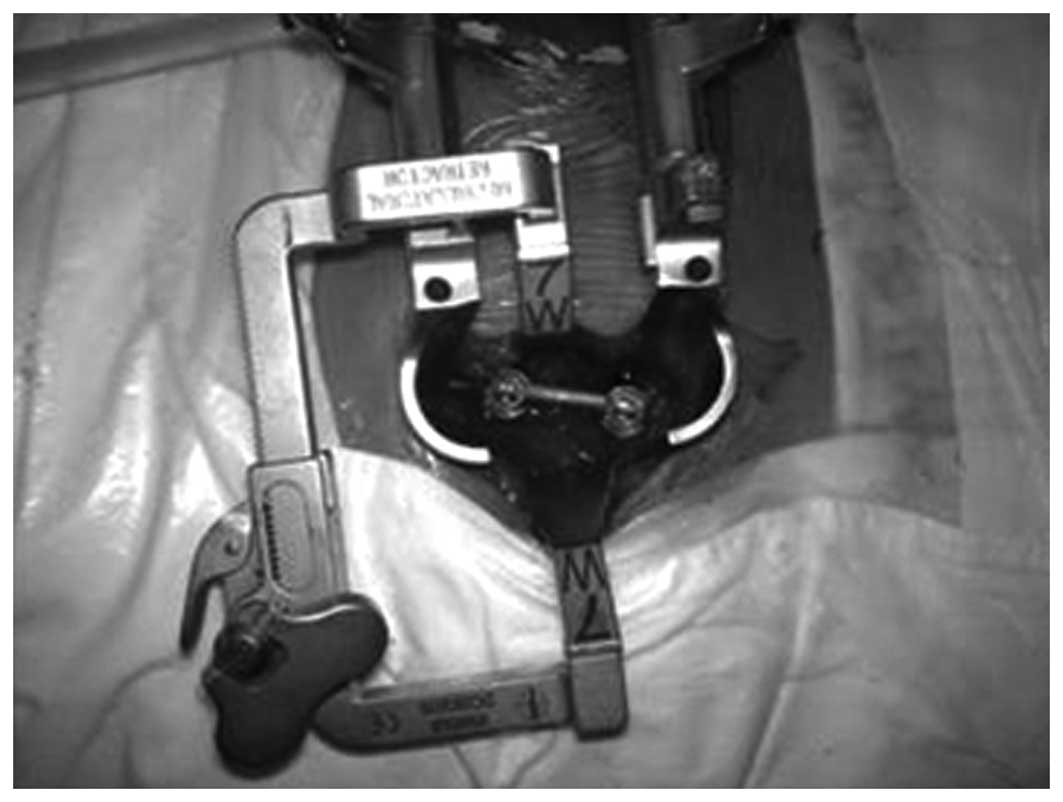
pedicle rod-screw system. In the minimally invasive group, a
standard posterior midline incision was also made and a
microendoscope was used first to decompress the stenosis and remove
the herniated disc (Fig. 2). To
treat the spondylolisthesis, a paraspinal approach was used to
perform a MI-TLIF using a single cage and pedicle rod-screw system
with the Quadrant system (an instrument with a working channel;
Fig. 3).
Postoperative care
The time of bed rest was 15–45 days in the
traditional group and 5–7 days in the minimally invasive group.
Routine antibiotics were administered for 1–2 days to prevent
infection. Care was taken of the sensory functions and movement of
the bilateral lower extremities and drainage of the incision. Back
muscle exercise began when the incision pain had alleviated.
Results
We evaluated the incision length, blood loss, time
of bed rest and ODI score prior to and following surgery of the
patients in the two groups. The data were statistically analyzed,
using SPSS 13.0 statistical software. The measurement data were
recorded, a t-test was performed to compare data from the two
groups and P<0.05 was considered to indicate a statistically
significant difference. In the minimally invasive group, the
average length of the incision was 6.9±1.1 (6–11)
cm, the surgery time was 232±28 (210–300) min, the blood loss was
361±122 (290–470) ml, the bed rest time was 6.1±0.8 (5–7) days
and the ODI score was 40.3±6.7 preoperatively and 11.5±3.8
postoperatively. In the traditional group, the average length of
the incision was 16.3±1.6 (16–22)
cm, the surgery time was 204±21 (180–240) min, the blood loss was
610±194 (410–950) ml, the bed rest time was 23.7±9.9 (15–45) days,
and the ODI scores were 39.4±7.2 and 13.6±3.1, respectively, prior
to and following surgery. There were statistically significant
differences in incision length, blood loss and bed rest time
following surgery between the two groups (P<0.05). However, the
surgery times and ODI scores of the two groups revealed no
significant differences (P>0.05; Table I).
 | Table I.Comparison between the minimal
invasive (MED+TLIF) group and the traditional PLIF group. |
Table I.
Comparison between the minimal
invasive (MED+TLIF) group and the traditional PLIF group.
| Group (n) | Incision (cm) | Surgery time
(min) | Blood loss (ml) | Bed rest time
(days) | Pre-surgery ODI | Post-surgery ODI |
|---|
| MI-TLIF (26) | 6.9±1.1a | 232±28 | 361±122a | 6.1±0.8a | 40.3±6.7 | 11.5±3.8 |
| PLIF (27) | 16.3±1.6 | 204±21 | 610±194 | 23.7±9.9 | 39.4±7.2 | 13.6±3.1 |
Discussion
From the viewpoint of pathological anatomy, lumbar
spinal stenoses are commonly multilevel, but rarely affect the
whole lumbar spine. The junctional part of two segments, that is,
the area between the upper segment and the lower one, including the
articular process, intervertebral disc, ligamentum flavum and the
connective parts of the upper and lower laminar, has the functions
of movement and stability and is most vulnerable to degeneration
(1). In the lumbar spinal canal,
stenosis rarely occurs on the vertebral body and cross-section of
the pedicle, but particularly affects the articular process,
intervertebral disc and upper part of the laminar junction
(2,3). According to anatomical pathology
studies, the areas demanding decompression are localized on the
canal near the intervertebral space, which provides the possibility
of preserving the bony canal behind the vertebral body. The
stability of the spine has been reported to be preserved due to the
good preservation of the laminar and articular processes (2,3).
These results provide theoretical evidence to support the limited
decompression of the spinal canal.
DLSS is often characterized as multilevel from the
radiologic findings, and has complicated and non-typical clinical
manifestations, which make diagnosis and treatment difficult.
According to a study by Park et al(4) of 13 spine surgery centers and 1091
patients from the USA, the patients who had spinal stenosis of more
than 3 segments were most likely to be elderly males. Single-level
stenosis is often located at the L4–L5 segment, while two-level
stenosis typically affects L3–L5 and three-level stenosis affects
L2–L5. Various surgical techniques for treating lumbar spinal
stenosis have been reported. The standard surgery for the treatment
of spinal stenosis at the early stage was extensive laminectomy for
decompression. Currently, most spinal surgeons consider that
extensive laminectomy destroys the stability of spine, and may lead
to serious complications, including lumbar spondylolisthesis and
epidural adhesions. Katz et al(5) confirmed that a quarter of the
patients studied required further surgery and one-third complained
of severe lower back pain during a 10-year follow-up. Thus,
extensive laminectomy is no longer the standard treatment for
spinal stenosis.
Since the main methods of the traditional PLIF
technique are based on laminectomy or nerve root decompression to
relieve the compression of the dural sac and nerve roots, the facet
joint has often been removed with the lamina to ensure a full
decompression, and damage to the stability of the spine is
inevitable (5). The lack of
protection for the lamina following decompression results in
adhesion between the dural sac and nerve roots, which leads to more
severe hyperostosis and re-stenosis of the spinal canal, and
effects the long-term clinical outcomes. Denervation due to
extensive stripping of the paraspinal muscle is also a major cause
of prolonged lower back pain following surgery (6).
An increasing number of groups advocate complete
decompression by limited, precise and more targeted techniques,
rather than extensive resection, to maintain the stability of the
spine by adopting less invasive techniques and to minimize the
damage to the anatomical structure by avoiding preventive
decompression at non-responsible levels (7–9). In
terms of preserving the stability of the spine, the modified
spinous-preserving laminectomy is preferable to total laminectomy,
particularly since the bilateral decompression may be conducted
using a unilateral approach, which has been reported in many
studies and has achieved satisfactory clinical outcomes (10–12).
We recommend the following operative principles for
the treatment of DLSS: locate the responsible level accurately,
decompress the spinal canal effectively, damage the normal
structure limitedly and avoid extensive resection. Limited
decompression is achieved by the precise diagnosis and location of
the responsible level according to the individual, and by
preserving the stability and integrity of the posterior column of
the spine so as to avoid the complications of iatrogenic
instability and adhesion of dural scars. The key to improving the
clinical outcomes is determining the responsible levels (13–15).
The concept of precise spinal surgery was proposed at the 5th
Chinese Orthopedic Association (COA) conference of the Chinese
Medical Association by certain experts. The combined use of
radiological examination and gait load testing for the clinical and
functional examinations is likely to aid the clarification of the
response level and range of positions that require decompression,
so as to avoid the complication of iatrogenic instability. There is
no need to carry out preventive surgery for radiologically
diagnosed stenosis without clinical symptoms (13–15).
MED from the posterior approach is a typical and
internationally recognized minimally invasive technique for the
treatment of lumbar disc herniation which has become increasingly
popular and developed in recent years and may also be used for the
minimally invasive laminectomy of lumbar spinal stenosis. It is
characterized by reduced invasion, quicker recovery and improved
clinical outcomes with clear advantages (16–18),
but may not be used for the treatment of patients with
spondylolisthesis. Compared with the traditional PLIF technique,
the TLIF technique causes less destruction of the posterior column
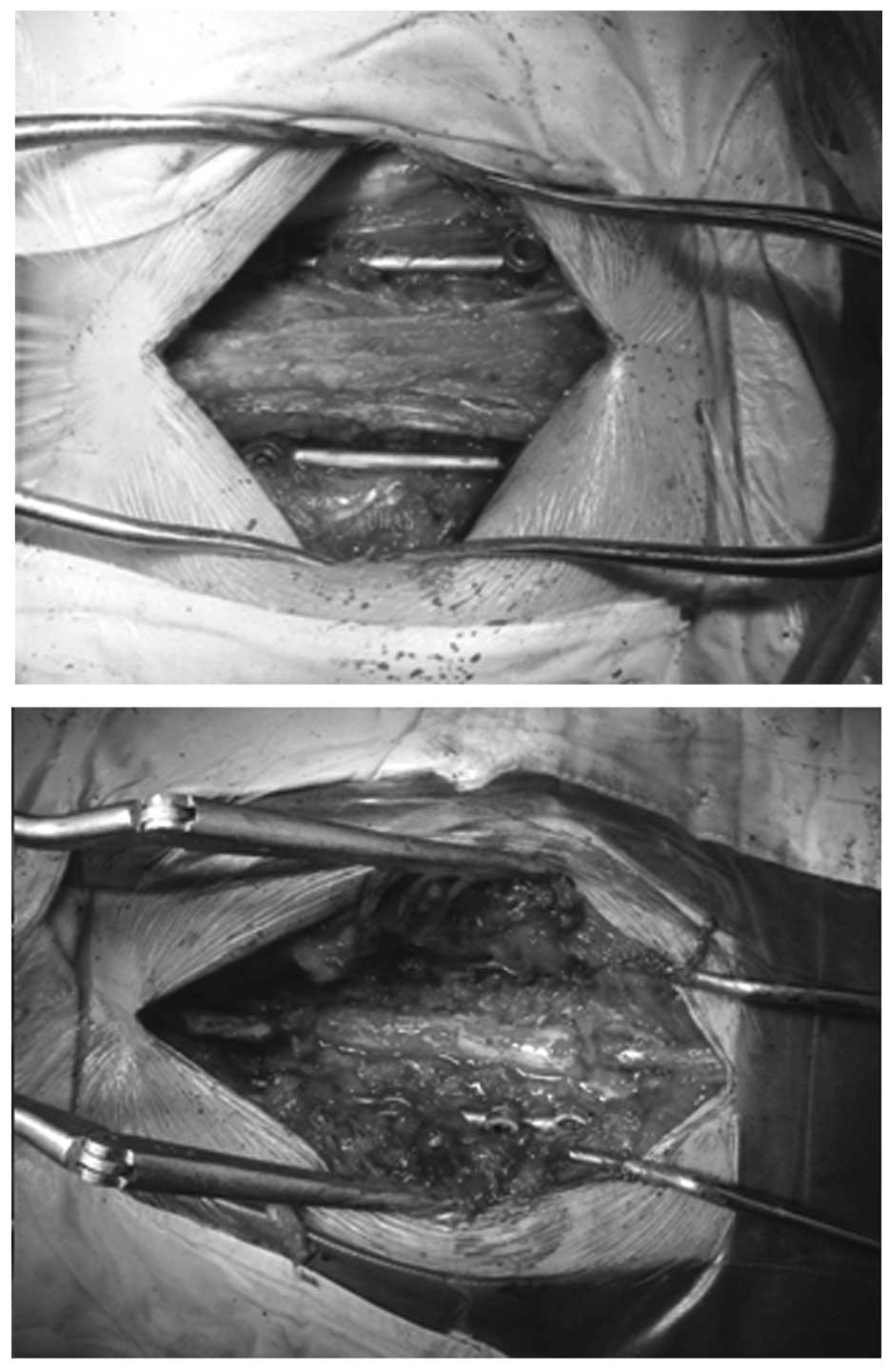
of the spine (19). In particular,
the application of MI-TLIF for the treatment of lumbar
spondylolisthesis by the paraspinal approach has the advantages of
reduced blood loss and less damage to the paraspinal soft tissue
(Figs. 4 and 5), but it also has the limitations of
long surgery times and a complicated surgical technique (20–22).
We have attempted to carry out a combination of MED and MI-TLIF
techniques for the treatment of DLSS with spondylolisthesis. MED
was used to decompress the nerve roots of the responsible level
while MI-TLIF was performed on the segments with spondylolisthesis.
Minimally invasive decompression and fusion may be carried out with
a combination of these two minimally invasive techniques, so that
the destruction of the posterior column of the spine is minimized.
All 26 patients in the minimally invasive group reached
satisfactory clinical improvements following surgery while also
having reduced blood loss, less damage to the paraspinal soft
tissue, improved outcomes and shorter recovery times than the
patients treated with the PLIF technique and similar short-term
clinical outcomes (Table I). The
combination of MED and MI-TLIF is a minimally invasive technique
for spinal surgery with clear advantages and bright prospects
worthy of further study and promotion.
References
|
1.
|
Jia LS and Yang L: The modern surgery
concept of degenerative lumbar spinal stenosis. Chin Orthop J.
29:509–512. 2002.(In Chinese).
|
|
2.
|
Spivak JM: Current concepts review -
degenerative lumbar spinal stenosis. J Bone Joint Surg Am.
80:1053–1066. 1998.
|
|
3.
|
Lee CK, Rauschning W and Glenn W: Lateral
lumbar spinal canal stenosis: classification, pathologic anatomy
and surgical decompression. Spine (Phila Pa 1976). 13:313–320.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Park DK, An HS, Lurie JD, et al: Does
multilevel lumbar stenosis lead to poorer outcomes?: a subanalysis
of the Spine Patient Outcomes Research Trial (SPORT) lumbar
stenosis study. Spine (Phila Pa 1976). 35:439–446. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Katz JN, Lipson SJ and Chang LC: Seven- to
10-year outcome of decompressive surgery for degenerative
lumbarspinal stenosis. Spine (Phila Pa 1976). 21:92–98.
1996.PubMed/NCBI
|
|
6.
|
Hackenberg L, Halm H, Bullmann V, Vieth V,
Schneider M and Liljenqvist U: Transforaminal lumbar interbody
fusion: a safe technique with satisfactory three to five year
results. Eur Spine J. 14:551–558. 2005.PubMed/NCBI
|
|
7.
|
Zouboulis P, Karageorgos A, Dimakopoulos
P, Tyllianakis M, Matzaroglou C and Lambiris E: Functional outcome
of surgical treatment for multilevel lumbar spinal stenosis. Acta
Orthop. 77:670–676. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Pons T and Shipton EA: Multilevel lumbar
fusion and postoperative physiotherapy rehabilitation in a patient
with persistent pain. Physiother Theory Pract. 27:238–45. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Zhong Y, Wei M, Xu J, et al: Clinical
short-term efficacy of selective laminectomy decompression for the
treatment of multilevel lumbar spinal stenosis. Chin Orthop Surg J.
16:1670–1672. 2008.(In Chinese).
|
|
10.
|
Sasai K, Umeda M, Maruyama T, Wakabayashi
E and Iida H: Microsurgical bilateral decompression via a
unilateral approach for lumbar spinal canal stenosis including
degenerative spondylolisthesis. J Neurosurg Spine. 9:554–559. 2008.
View Article : Google Scholar
|
|
11.
|
Vaccaro A: Unilateral approach for
microsurgical decompression. J Neurosurg Spine. 9:552–553. 2008.
View Article : Google Scholar
|
|
12.
|
Haba K, Ikeda M, Soma M and Yamashima T:
Bilateral decompression of multilevel lumbar spinal stenosis
through a unilateral approach. J Clin Neurosci. 12:169–171. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Kim YS, Park SJ, Oh IS and Kwan JY: The
clinical effect of gait load test in two level lumbar spinal
stenosis. Asia Spine J. 3:96–100. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Zhong Y, Ning Y, Li Z, et al: Correlation
analysis of surgical effect, gait load test and radiologic
examination in more than 140 patients. Chin Orthop J. 19:357–360.
2011.(In Chinese).
|
|
15.
|
Zhong Y, Ning Y and Wu Z: Research
progress in determination of the responsible level of multilevel
degenerative lumbar spinal stenosis. J Guangxi College Trad Chin
Med. 13:69–71. 2010.(In Chinese).
|
|
16.
|
Ikuta K, Tono O and Oga M: Clinical
outcome of microendoscopic posterior decompression for spinal
stenosis associated with degenerative spondylolisthesis - minimum
2-year outcome of 37 patients. Minim Invas Neurosurg. 51:267–271.
2008.
|
|
17.
|
Pao JL, Chen WC and Chen PQ: Clinical
outcomes of microendoscopic decompressive laminotomy for
degenerative lumbar spinal stenosis. Eur Spine J. 18:672–8. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Lu X, Peng H and Ling SZ: The prospective
study for the microscopic treatment of lumbar spinal stenosis. Chin
Orthop J. 17:1358–1360. 2009.(In Chinese).
|
|
19.
|
Ozgur BM, Yoo K, Rodriguez G and Taylor
WR: Minimally-invasive technique for transforaminal lumbar
interbody fusion (TLIF). Eur Spine J. 14:887–894. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Wu RH, Fraser JF and Härtl R: Minimal
access versus open transforaminal lumbar interbody fusion:
meta-analysis of fusion rates. Spine (Phila Pa 1976). 35:2273–2281.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Schizas C, Tzinieris N and Tsiridis E:
Minimally invasive versus open transforaminal lumbar interbody
fusion: evaluating initial experience. Int Orthop. 33:1683–1688.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Schizas C, Tzinieris N, Tsiridis E and
Kosmopoulos V: Minimally invasive versus open transforaminal lumbar
interbody fusion: evaluating initial experience. Int Orthop.
33:1683–1688. 2009. View Article : Google Scholar : PubMed/NCBI
|