Introduction
At present, cholangiojejunostomy mostly uses
Roux-en-Y anastomosis. Broadly speaking, cholangioenterostomy in
Whipple surgery is also within this category (1). Following cholangioenterostomy,
complications, including biliary tract infection (2,3),
lithogenesis (4) and obstructive
jaundice (5) usually occur. The
generation of these complications is mostly associated with
anastomotic benign strictures (6)
or tumor recurrence congestion, duodenal-biliary reflux or
biliary-jejunal loop dyskinesis (7), as well as the increase in
non-conjugated cholic acid and bacterial content in the jejunum
following bilioenteric Roux-en-Y anastomosis (8,9).
However, bilioenteric anastomotic strictures are the main
pathological and anatomical causes generating these complications.
In view of this, certain scholars have attempted to modify the
bilioenteric Roux-en-Y anastomosis method by, for example, taking
anti-reflux measures, but the result was unsatisfactory (10). A conservative treatment is also
mostly ineffective. In conventional surgery, the trauma of
treatment is greater and operating is more difficult. Also, a
second, or even multiple, surgeries are required, which not only
increases the surgical risk and difficulty, but also makes the
bilioenteric anastomotic stoma narrower and causes further
complications. Therefore, the efficiency of surgical treatment is
unpredictable. Moreover, conventional peroral endoscopic therapy
mostly fails due to changes in anatomical relationships caused by
the post-operative gastrojejunal reconstruction. Although there are
reports of successful procedures (11), the demands on the surgeons and
equipment are higher and it is therefore difficult to encourage
further promotion and application of this procedure. Previous
studies have shown percutaneous and transhepatic balloon dilation
of bilioenteric anastomotic strictures (12–14).
Although an improved treatment efficiency is obtained, it is mostly
necessary to indwell the drainage tube in vivo
synchronously, which reduces the patient’s quality of life.
Additionally, if there is calculus of the bile duct near to the
anastomotic stoma, it is likely to take longer to complete the
endoscopic treatment via this pathway. Consequently, it is of vital
importance to seek a more effective and minimally invasive
treatment method. To solve this problem, transjejunal endoscopy for
the treatment of biliary complications following
choledochojejunostomy is adopted. Based on summaries of the
clinical experiences and observations of the treatment efficacy, a
better evaluation of the safety and efficiency of this treatment
method is required.
Patients and methods
General data
In total, 13 patients, including 6 males and 7
females, with a mean age of 59 years (range, 32–81 years) were
included in this study. The study was conducted in accordance with
the declaration of Helsinki and with approval from the Ethics
Committee of Shenyang North Hospital. Written informed consent was
obtained from all participants. Bilioenteric Roux-en-Y anastomosis
was conducted in4 cases due to bile duct cancer in the porta
hepatis, in 1 case due to congenital biliary duct cyst canceration,
in 2 cases due to congenital biliary duct cysts and in 1 further
case due to iatrogenic biliary duct injury. Palliative resection of
bile duct cancer combined with biliary-jejunal loop anastomosis was
conducted in 1 case due to cancer in the middle segment of the bile
duct. Pancreaticoduodenectomy (PD) was conducted in 3 cases due to
cancer in the lower segment of the common bile duct and in 1 other
case due to ampulla cancer. Of these 13 cases, there were 8 cases
of patients whose bilioenteric drainage tubes were indwelled at the
bilioenteric anastomotic stoma and were led out from the lateral
abdominal wall via a biliary-jejunal loop, 1 case of a patient
whose inner pipe was led out from the bile duct at the porta
hepatis and 4 cases of patients without drainage tubes. In
addition, 1 patient required surgery twice, while another required
3 surgeries in total to complete the treatment. Following
cholangioenterostomy, biliary complications occurred between 12
days and 20 years post-surgery, with a median time of 12 months.
Moreover, 5 cases presented with upper-right abdominal distension
and discomfort, 11 cases presented with recurrent chills and high
fever and 11 cases presented with icterus.
Imaging examination
Color Doppler ultrasound examination revealed that
10 cases presented with intrahepatic cholangiectasis and that 4
cases presented with calculus of the bile duct at the porta
hepatis. Of these, 3 cases presented with intrahepatic secondary
bile ducts complicated by calculus.
Surgical approach and endoscopic
technique
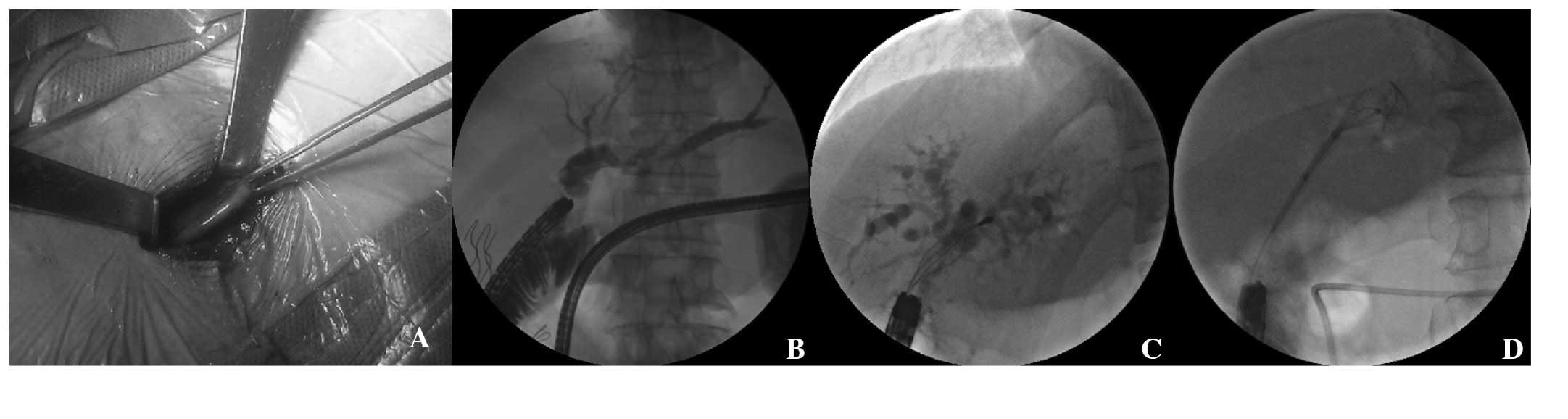
The surgical approach was to seek the
biliary-jejunal loop. Following systemic anesthesia, the skin scar
was led out from the original bilioenteric inner pipe using the
lateral abdominal wall as the midpoint, and the skin was
longitudinally cut open (3 to 5 cm) and deepened layer by layer to
find the biliary-jejunal loop in the abdomen. The biliary-jejunal
loop was mostly attached to the lateral peritoneum, its marker
being the residual line junction fixed onto the lateral peritoneum
by suturing. Subsequently, the contralateral mesentery wall of the
biliary-jejunal loop was cut open, and purse-string sutures were
performed on the seromuscular layer around the incision in order to
provide a channel for the endoscopic technique. The bilioenteric
inner pipe of 1 case was not led out from the biliary-jejunal loop.
In the cases of the 4 patients without drainage tubes, the incision
was made in the upper right abdomen via the rectus abdominis, and a
nasobiliary duct was installed in the biliary-jejunal loop as the
marker for seeking this loop (Fig.
1A).
The endoscopic technique was an exploration first
conducted with an ultrafine gastroscope to find the bilioenteric
anastomotic stoma, while under the coordination of the digital
subtraction technique (DST). Subsequently, a gastroscopy was
conducted to carry out the procedures required, including
cholangiography, basket extraction, balloon dilatation or biliary
stent installation (Fig. 1B–D). Of
these cases, the bilioenteric anastomotic stoma of 1 patient was
completely occluded by a cancer embolus due to bile duct cancer
metastasis, and so it was impossible to insert a guide wire via the
anastomotic stoma under the endoscope. Therefore, percutaneous
transhepatic biliary drainage (PTCD) was performed instead, and a
Zebra guidewire was implanted via a PTCD tube and inserted into the
biliary-jejunal loop via the anastomotic stoma. Next, an inner pipe
was installed via the guide wire by means of the gastroscope.
Finally, the internal and external dual drainage of the biliary
tract was completed.
The biliary-jejunal loop was sutured in a total of
11 cases and was fixed onto the lateral abdominal wall. A drainage
tube was implanted into the biliary-jejunal loop in 2 cases and
then led out from the incision prior to being sutured. At the early
post-operative stage, the dressing on the incision required
changing daily and anti-inflammation and liver-protection therapy
was conducted.
Results
General data
During the surgeries, metal stents were installed in
4 cases, plastic stents were installed in 5 and nasobiliary ducts
were installed in 2.
Surgical efficiency
In total, there were 9 patients that did not suffer
post-operative cholangitis attacks, 2 patients whose post-operative
cholangitis attacked at an early stage and eased at a later stage
and 2 patients whose post-operative cholangitis was recurrent and
persistent. With regard to the post-operative bilirubin levels, 10
cases showed a significant decrease, 2 cases demonstrated
fluctuations and an slight increase and 1 case demonstrated
fluctuations and a significant increase. With regard to the
cholelithiasis treatment, 3 cases were successfully treated, with
an overall stone clearance rate of 75% (3/4). Post-operative
complications included 1 case of a jejunal fistula, 1 case with
hepatapostema and 3 cases with incision infections. The incidence
rate of intra-operative biliary-jejunal anastomotic strictures was
76.9% (10/13). A total of 16 surgeries were performed on 13
patients, with an overall success rate of 100% (16/16).
Discussion
The majority of complications following
cholangioenterostomy occur in the post-operative long term
(15), with only a minority
occurring in the post-operative short term (16). In the present study, 2 cases
occurred within 2 months of surgery, 1 case after 3 months and the
remaining cases all occurred after >6 months and were possibly
associated with strictures caused by gradual scar tissue formation
at the bilioenteric anastomotic stoma. Among the cases in this
group, the incidence rate of intraoperative biliary-jejunal
anastomotic stricture was 76.9% (10/13).
The results of the present study identified that the
endoscopy treatment of biliary complications after
choledochojejunostomy via the biliary-jejunal loop stoma has a high
success rate and satisfactory short-term treatment efficiency, with
no severe post-operative complications. This not only suggests that
this method is safe and effective, but that it may also be used
repeatedly in the same patient with minimal invasion. The
successful implementation of this method further supports the
currently advocated treatment model for biliary complications
following cholangioenterostomy, namely endoscopy on the behalf of
minimally invasive treatment methods (17). Although a previous study has also
reported endoscopic stone extraction techniques via the jejunal
loop (18), the primary diseases
involved in these cases were calculi of the bile duct, while the
primary diseases in the present study are malignant tumors.
Generally, the jejunal loop in the reported cases was placed in an
uncertain location in the subcutaneous tissue and the jejunal
approaches were mostly preset, while the biliary-jejunal loop in
the present study was mostly located in the abdominal cavity.
Additionally, a fiber choledochoscope was mostly applied in the
previous studies, while only gastroscopy and ultrafine gastroscopy
were used in the cases from the present study. Also, biliary stents
and nasobiliary ducts were installed in the majority of cases in
the present study. At this time, there is no comparable research
literature to this group of cases.
The biggest difficulty of transjejunal endoscopy for
the treatment of biliary complications after choledochojejunostomy
is how to accurately select the biliary-jejunal loop. As current
complications mostly occur in the post-operative long term, the
bilioenteric inner pipe is removed and the original abdominal wall
sinus ostium is closed. In addition, the original drainage tube of
the abdominal cavity is mostly led out from the right lateral
abdominal wall. The two abdominal wall outlet scar locations are
extremely close, which often causes difficulties in selecting the
correct abdominal wall incision. Therefore, it is necessary not
only to review the original surgical records, but also to request a
detailed medical history in order to determine the outlet position
of the original bilioenteric inner pipe at the abdominal wall, and
thus correctly select an incision site. In the present study, 2
cases presented with complications in the post-operative short term
and retained the bilioenteric inner pipe. It was therefore
relatively easy to select the biliary-jejunal loop. However, the
bilioenteric inner pipe of 1 case was led out via the bile duct at
the porta hepatis, while 4 cases had no indwelling drainage pipes
at all. Therefore, the biliary-jejunal loop was not fixed onto the
abdominal wall, and it was extremely difficult to find. To avoid
searching blindly, we installed a nasobiliary duct in the
biliary-jejunal loop as a marker for finding it. After making an
incision into the peritoneum, the jejunal tube which adheres to the
lateral abdominal wall is visible, but an incision cannot be made
without careful consideration. Generally, the biliary-jejunal loop
is identified according to the residual line junction fixed onto
the lateral peritoneum by biliary-jejunal loop suturing and also
judged according to the relationship of the jejunal loop with the
first porta hepatic. Afterwards, an incision is made into the
contra-lateral mesentery wall of the biliary-jejunal loop to
conduct a endoscopic examination for the final confirmation.
Usually, an ultrafine gastroscope is used to first explore the
position of the bilioenteric anastomotic stoma and a guide wire is
indwelled. Subsequently, a common gastroscope is used to conduct
the surgery. As the jejunal tube is tortuous and adherent, the
gastroscope entry direction is usually inconsistent with the upper
and lower direction of the biliary-jejunal loop under the incision.
It is feasible to successfully find the bilioenteric anastomotic
stoma only under the guidance of DST. Certain studies (19–21)
showed that it was feasible to determine the biliary-jejunal loop
position under the guidance of ultrasound, CT or X-ray fluoroscopy,
but this relies on the jejunal loop being located in the
subcutaneous tissue or under the anadesma, and its application has
certain limitations.
Endoscope entry via the percutaneous jejunostomy
pathway usually causes an air leakage phenomenon, particularly at
the early stage of endoscope entry, which causes interference in
the endoscopic field of vision. Therefore, purse-string suture is
performed on the seromuscular layer around the endoscope. As the
endoscope enters, appropriate tightening is conducted and the
jejunal wall stoma is surrounded with gauze so that a better result
may be obtained.
In the present study, we initially injected air into
the enteric cavity to increase the field of vision in 2 cases.
Severe pneumatosis occurred in the enteric cavity during surgery
and post-operative abdominal distension of the patients was
apparent. This was not only unfavorable for abdominal closure, but
also increased the risk of intestinal fistulas or incision
infections. Even if gastrointestinal decompression is conducted, it
is difficult to relieve these symptoms. To avoid this phenomenon,
we replaced the injected air with CO2. In addition, the
gas in the enteric cavity, particularly at the distal end of
biliary-jejunal loop, was drawn out as much as possible following
the completion of surgery.
To locate the bilioenteric anastomotic stoma,
patience is required. As the bilioenteric anastomotic stoma may
suffer from an inflammatory stricure or recurring tumor congestion,
finding it becomes difficult even if the endoscope entry direction
is correct. It may be necessary to repeatedly change between
gastroscope, duodenoscope and ultrafine gastroscope. Also, multiple
attempts using radiography are required to try to insert the guide
wire in order to find the biliary tract. In the present study, the
bilioenteric anastomotic stoma was occluded in 1 patient due to
tumor recurrence, and it was impossible to insert the guide wire
from the enteric cavity into the bile duct. Therefore, PTCD was
conducted under the guidance of Color Doppler ultrasound. The guide
wire was inserted via the PTCD tube and led into the
biliary-jejunal loop through the bile duct at the porta hepatis and
the bilioenteric anastomotic stoma. Inside the enteric cavity, the
guide wire was captured with biopsy forceps. The biliary stent was
passed along the guide wire and implanted to complete the internal
and external dual drainage system. Following surgery, an efficient
reduction in Bilirubin levels provided good evidence of the
coexistence of internal and external drainage. Also, washing the
PTCD tube removed obstructions from the the biliary stent.
Therefore, due to simple PTCD external drainage, a majority of the
bile was now able to enter the intestinal tract and injury to
digestive function was avoided. The patient now maintains a good
appetite.
With the exception of 2 patients who suffered from
complications in the early post-operative stage who retained the
bilioenteric inner pipe, and for whom biliary-jejunal loop ostomy
was conducted following therapeutic endoscopy, the primary suturing
of the intestinal loop incision was conducted for the remaining
cases. The suture position was fixed onto the peritoneum under the
incision. Of these cases, only one patient sufferred from an
intestinal fistula, which was associated with poor nutritional
status or malnutrition and was not medicated in time due to
economic reasons.
To avoid post-operative incision infections, it is
necessary to use an aspirator to absorb the intraoperative outflow
of intestinal juice. Also, the incision must be thoroughly
disinfected prior to abdominal closure. Following surgery,
dressings must be changed regularly and subcutaneous effusion
monitored. If necessary, active drainage and simultaneous
physiotherapy may be carried out. The prevention of incision
infections also contributes to the prevention of intestinal
fistulas. In the present study, 3 cases presented with incision
infections of varying degrees. Following drainage and
physiotherapy, the symptoms disappeared. As a result of these
accumulated experiences, later cases did not suffer from incision
infections.
Transjejunal endoscopy for the treatment of biliary
complications after choledochojejunostomy is a further development
of endoscopic minimally invasive technology. It is an effective
minimally invasive method for the control of icterus and
cholangitis symptoms in particular, and for certain patients with
advanced tumors or for those in which repeated surgeries are
unsuitable. Although it is necessary to accumulate further cases
and constantly generate summaries and improvements, this method is
worthy of further promotion and application due to its improved
treatment efficiency and technological advantages.
References
|
1.
|
House MG, Cameron JL, Schulick RD, et al:
Incidence and outcome of biliary strictures after
pancreaticoduodenectomy. Ann Surg. 243:571–578; discussion.
576–578. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Carrel T, Matthews J, Schweizer W, Baer H,
Gertsch P and Blumgart LH: Diagnosis, etiology and treatment of
cholangitis following bilio-digestive surgery. Helv Chir Acta.
56:891–896. 1990.(In French).
|
|
3.
|
Matthews JB, Baer HU, Schweizer WP,
Gertsch P, Carrel T and Blumgart LH: Recurrent cholangitis with and
without anastomotic stricture after biliary-enteric bypass. Arch
Surg. 128:269–272. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
De Moor V, El Nakadi I, Jeanmart J, Gelin
M and Donckier V: Cholangitis caused by Roux-en-Y
hepaticojejunostomy obstruction by a biliary stone after liver
transplantation. Transplantation. 75:416–418. 2003.PubMed/NCBI
|
|
5.
|
Lasnier C, Kohneh-Shahri N and Paineau J:
Biliary-enteric anastomosis malfunction: retrospective study of 20
surgical cases. Review of literature. Ann Chir. 130:566–572.
2005.(In French).
|
|
6.
|
Frilling A, Li J, Weber F, et al: Major
bile duct injuries after laparoscopic cholecystectomy: a tertiary
center experience. J Gastrointest Surg. 8:679–685. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Johnson CP, Sarna SK, Cowles VE, et al:
Motor activity and transit in the autonomically denervated jejunum.
Am J Surg. 167:80–88. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Yamamoto T, Hamanaka Y and Suzuki T: Bile
acids and micro-organisms in the jejunal lumen after biliary
reconstruction in dogs. J Am Coll Surg. 181:525–529.
1995.PubMed/NCBI
|
|
9.
|
Chuang JH, Lee SY, Chen WJ, Hsieh CS,
Chang NK and Lo SK: Changes in bacterial concentration in the liver
correlate with that in the hepaticojejunostomy after bile duct
reconstruction: implication in the pathogenesis of postoperative
cholangitis. World J Surg. 25:1512–1518. 2001. View Article : Google Scholar
|
|
10.
|
Zorn GL III, Wright JK, Pinson CW, Debelak
JP and Chapman WC: Antiperistaltic Roux-en-Y biliary-enteric bypass
after bile duct injury: a technical error in reconstruction. Am
Surg. 65:581–585. 1999.PubMed/NCBI
|
|
11.
|
Pohl J, May A, Aschmoneit I and Ell C:
Double-balloon endoscopy for retrograde cholangiography in patients
with choledochojejunostomy and Roux-en-Y reconstruction. Z
Gastroenterol. 47:215–219. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Köcher M, Cerná M, Havlik R, Král V, Gryga
A and Duda M: Percutaneous treatment of benign bile duct
strictures. Eur J Radiol. 62:170–174. 2007.
|
|
13.
|
Lorenz JM, Denison G, Funaki B, Leef JA,
Van Ha T and Rosenblum JD: Balloon dilatation of biliary-enteric
strictures in children. AJR Am J Roentgenol. 184:151–155. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Jan YY, Chen MF and Hung CF: Balloon
dilatation of intrahepatic duct and biliary-enteric anastomosis
strictures. Long term results Int Surg. 79:103–105. 1994.PubMed/NCBI
|
|
15.
|
Tocchi A, Costa G, Lepre L, Liotta G,
Mazzoni G and Sita A: The long-term outcome of hepaticojejunostomy
in the treatment of benign bile duct strictures. Ann Surg.
224:162–167. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Zafar SN, Khan MR, Raza R, et al: Early
complications after biliary enteric anastomosis for benign
diseases: a retrospective analysis. BMC Surg. 11:192011. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Laasch HU and Martin DF: Management of
benign biliary stictures. Cardiovasc Intervent Radiol. 25:457–466.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Gott PE, Tieva MH, Barcia PJ and Laberge
JM: Biliary access procedure in the management of oriental
cholangiohepatitis. Am Surg. 62:930–934. 1996.PubMed/NCBI
|
|
19.
|
Berkmen T, Echenique A and Russell E:
Ultrasound guidance in accessing the afferent limb of a modified
Roux-en-Y choledochojejunostomy for percutaneous dilation of
biliary strictures. J Vasc Interv Radiol. 12:1219–1222. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Perry LJ, Stokes KR, Lewis WD, Jenkins RL
and Clouse ME: Biliary intervention by means of percutaneous
puncture of the antecolic jejunal loop. Radiology. 195:163–167.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Hutson DG, Russell E, Yrizarry J, et al:
Percutaneous dilatation of biliary strictures through the afferent
limb of a modified Roux-en-Y choledochojejunostomy or
hepaticojejunostomy. Am J Surg. 175:108–113. 1998. View Article : Google Scholar : PubMed/NCBI
|