Introduction
Hypertension, defined as a systolic blood pressure
(BP) >140 mmHg and/or a diastolic BP >90 mmHg, is one of the
major risk factors for various cardiovascular morbidities,
including stroke, coronary heart disease and kidney dysfunction, as
well as for mortality (1).
Although hypertension affects up to 30% of the adult population in
the majority of countries (2),
>50% of hypertensive individuals are unaware of their condition
(3). Prehypertension, formerly
termed borderline hypertension or high-normal BP, is usually
defined as a systolic BP of 130–139 mmHg and a diastolic BP of ≤89
mmHg, or as a systolic BP of ≤139 mmHg and a diastolic BP of 85–89
mmHg (2,4). This condition is known to be a
precursor of hypertension (4,5) and
is associated with excess morbidity and mortality from
cardiovascular causes (4,6). Thus, lowering BP may be beneficial
not only for the hypertensive population but also for the
prehypertensive population. For the initial management of high BP,
relevant lifestyle modifications, including ensuring optimal
nutrition, weight reduction and regular physical activity, were
established by The Japanese Society of Hypertension (JSH) in 2004
(7). In recent years, food
supplementation, mainly using natural foods or their components,
has been considered to provide another, less strenuous
non-pharmacological option for lowering BP, particularly for
individuals with borderline to mildly high BP that does not warrant
the prescription of antihypertensive drugs.
Garlic (Allium sativum) has a long history of
use as a foodstuff and as a pungent spice in numerous countries.
Garlic has also been used in a number of cultures for various
medicinal purposes. Previous pharmacological studies concerning
garlic have revealed that it has various prophylactic and remedial
properties beneficial to good health, among which its hypotensive
activities are the most notable (8–11).
Over the last 30 years, numerous clinical studies have been carried
out to examine the effects on health of using various garlic-based
products containing dried garlic powder, garlic oil or garlic
extract as the basal component. Such varied types of garlic
preparation may contain widely varying types of sulfur-containing
phytochemicals due to the different methods of producing the
preparations. This may precipitate varying biological responses in
humans. Although several clinical trials have suggested that garlic
lowers systolic and/or diastolic BP, negative results have been
obtained in a larger number of trials, as recognized by several
systematic reviews and meta-analyses (8,12–15).
These studies may have been complicated by differences in study
design, study population, dosage, duration of treatment or type of
garlic preparation.
In Japan, a unique type of garlic preparation has
been used for centuries as a traditional health food. This is a
garlic homogenate-based supplementary diet (GH diet) that is made
by kneading and pulverizing crushed garlic together with egg yolk.
A considerable number of commercial products containing the GH diet
are currently available on the market. Tradition dictates that the
egg yolk is included to enrich the nutrient content and alleviate
the untoward effects of garlic, including gastrointestinal
complaints and breath and body odor. Using a representative GH diet
product, we have previously demonstrated that chronic oral
administration significantly lowered BP in spontaneously
hypertensive rats (16). The
promising results from this animal study tempted us to conduct a
clinical trial to evaluate the effects of short-term
supplementation with the same GH diet product on the systolic and
diastolic BPs of adult subjects with prehypertension or mild
hypertension.
Subjects and methods
Subjects and eligibility
Two populations of adult male and female Japanese
participants aged 20–70 years old were included in this study: one
population comprised prehypertensive individuals with systolic BPs
between 130 and 139 mmHg or diastolic BPs between 85 and 89 mmHg,
and the other contained mildly hypertensive (stage I hypertensive)
individuals with systolic BPs between 140 and 159 mmHg or diastolic
BPs between 90 and 99 mmHg (as defined according to the criteria of
the 2004 JSH Guidelines for the Management of Hypertension)
(7). Subjects were excluded if
they were receiving antihypertension treatment or other medications
that may have affected their BP, or if they currently suffered from
diabetes, chronic renal failure or cardiovascular dysfunction. They
were also excluded if they had a past history of such medical
conditions or routinely consumed alcohol in a daily dose of ≥60 g,
or if they had secondary hypertension, white-coat hypertension or
known allergies to garlic or any other ingredients of the GH diet
or placebo. The other exclusion criteria were participation in
another clinical study at the start time of the present study,
being a pregnant woman, nursing mother or a woman of childbearing
potential or the presence of any clinically significant medical
condition judged by the investigator to preclude the participant's
inclusion in the study. Written informed consent was obtained from
all participants prior to their enrollment in the study.
The study participants attended 2 screening visits
(clinic visits 1 and 2) at an interval of 2 weeks, each of which
included medical and life-style histories, physical examinations,
laboratory tests and measurements of BP. The study treatment began
∼2 weeks later (clinic visit 3; baseline). Participants included in
the prehypertensive and mildly hypertensive populations were those
whose systolic and diastolic BPs, measured at visits 1 and 2,
maintained levels within the ranges defined for prehypertension and
mild hypertension, respectively. All participants were further
instructed to self-measure their BP at home during the 2-week
interval between clinic visits 2 and 3, and were again confirmed to
have a systolic BP of 130–139 mmHg and/or a diastolic BP of 85–89
mmHg for prehypertensive subjects and a systolic BP of 140–159 mmHg
and/or a diastolic BP of 90–99 mmHg for mildly hypertensive
subjects.
Study design and study diet
A randomized, double-blind, placebo-controlled study
was designed to assess the efficacy and safety of the GH diet for
lowering the BP in enrolled subjects when compared with the
placebo. The study consisted of a run-in period of 4 weeks for
screening and randomization of eligible subjects, a 12-week
treatment period and a 4-week post-treatment follow-up period. The
study mainly occurred between September 2006 and May 2007 at the
Medical Corporation Keiaikai Nakamura Hospital (Beppu, Japan). The
study protocol was approved by the Institutional Review Board of
the hospital. The study was conducted in accordance with the
principles of the Declaration of Helsinki in 1995 (as revised in
Edinburgh, 2000) and the Ethical Guidelines for Epidemiological
Research (2004) enacted by the Japanese Government in 2004.
The GH diet used in this study was contained in a
500 mg capsule ‘Dentou-ninniku-ranwo™’ (Kenkoukazoku Inc.,
Kagoshima, Japan). This capsule contained 188 mg of a garlic
preparation consisting of a powdery mixture of garlic homogenate
and egg yolk (as the active ingredient). This is made by kneading
and pulverizing crushed garlic bulbs together with egg yolks at a
weight ratio of 80:20. The capsule also contained 266.5 mg rapeseed
oil (as the solvent) and 45.5 mg beeswax (as the stabilizer).
Placebo capsules contained dextrin, rapeseed oil and beeswax. The
contents were colored by saffron and caramel to make them similar
in appearance to the contents of the active capsule.
Throughout the course of the study, from the run-in
period to the post-treatment follow-up period, each participant was
required to keep a study diary of their allocated capsule intake,
any adverse events experienced, dietary composition, physical
activity assessed by a passometer and all medications or therapies
received. Participants were also instructed to maintain their body
weight and to avoid exercising, eating or drinking in excess of the
levels of their usual habits. Upon completion of the run-in period,
eligible subjects with prehypertension and those with mild
hypertension were sequentially assigned to either one of the two
masked study capsules (GH diet or placebo) according to a
predetermined computer-generated randomization schedule. The
participants were instructed to take 2 capsules (300 mg as
dehydrated GH) per day at any time of the day. Taking <85% of
the prescribed course of the allocated study capsule was considered
as non-compliance with the treatment. Such non-compliant subjects
were excluded from the efficacy assessment.
To assess efficacy and safety, medical inspections,
measurements of BP and other physical parameters and laboratory
tests were performed at baseline (clinic visit 3), at 4 weeks
(clinic visit 4), 8 weeks (clinic visit 5) and 12 weeks (clinic
visit 6) following the start of the treatment, and also after 4
weeks subsequent to the termination of the treatment (clinic visit
7; post-week 4).
BP measurement
Systolic and diastolic BPs were measured from the
left arm using an automated sphyngomanometer (HEM-7051T; Omron
Corp., Kyoto, Japan). Measurements were performed repeatedly (a
maximum of 5 times) at 2-min intervals following a 10-min or longer
rest in a sitting position, until the variance of 2 successive
measurements was ≤5 mmHg. The mean values of 2 such measurements
were then used as an estimate of BP.
Blood sampling and laboratory tests
Fasting blood samples were collected by venopuncture
at each clinic visit. The EDTA tubes were then refrigerated
immediately and centrifuged within 2 h. Plasma samples were stored
in a frozen state until analysis. All plasma samples were analyzed
for routine hematological and biochemical parameters.
Assessments of diet and physical activity
behaviors
Food intake and exercise behaviors were assessed at
every clinic visit based on the daily records from the study diary.
The exercise assessment was aided by the use of a passometer. Data
were analyzed at a group level.
Masking
Subjects and all study personnel (including the data
analyst) were blinded to the treatment assignments throughout the
study. Placebo capsules were similar in appearance and size to the
active capsules. Blinding of the subjects, effectiveness of the
blinding and the tolerance of the study capsules were assessed at
each clinic visit by analyzing the study diary. Upon completion of
the study, subjects were asked if they knew which of the two
treatments they were assigned to.
Safety assessments
Safety parameters were the incidence and severity of
treatment-related adverse events that the subjects reported that
they had experienced throughout the treatment and post-treatment
follow-up periods.
Statistical methods
Efficacy and safety were assessed on the basis of
data from the per-protocol-based (PPB) and the intention-to-treat
(ITT) populations, respectively. The PPB population consisted of
the subjects with prehypertension and those with mild hypertension
who completed all clinic visits at the prescribed times and the
full protocol and who were suitably compliant with the prescribed
regimen (GH diet or placebo), with an overall compliance rate
>85%. The ITT population included all subjects in the study
populations who were randomized and received at least 1 dose of the
assigned study capsules and for whom any follow-up evaluation
(physical parameters, laboratory tests, adverse events and
self-reported comments) were obtained. Thus, the ITT population was
to include those subjects who dropped out of the study, were
removed or lost prior to follow-up or were non-compliant with the
regimen specified in the protocol.
The baseline characteristics of the randomized
subjects with prehypertension and those with mild hypertension were
compared between the GH and placebo groups using the Student's
unpaired t-test for data expressed as mean ± standard deviation
(SD), and by the Chi-square test for category variables. The
efficacy results were expressed in terms of mean ± standard error
(SEM). The Bonferroni method was used for within-group efficacy
assessments, and the Student's unpaired t-test was used for
comparison of the treatment effects between the two groups.
P<0.05 was considered to indicate a statistically significant
difference.
Results and discussion
Characteristics of subjects
In total, 81 subjects, consisting of 34 with
prehypertension and 47 with mild hypertension, were enrolled in the
study and assigned to either the placebo (n=18 and 23,
respectively) or GH diet groups (n=16 and 24, respectively). A
total of 80 subjects completed all clinic visits resulting in a
retention rate of 99%. One male subject (mild hypertension,
placebo) dropped out for an unrelated personal reason after 4 weeks
of treatment. In addition, 8 subjects were also excluded from
efficacy analysis for the following reasons: 6 subjects delayed
taking the assigned study capsules for ≥4 days following visit 3 (1
mild hypertension, placebo; 1 prehypertension, GH; and 4 mild
hypertension, GH); 1 subject missed taking the assigned study
capsules for >4 days (prehypertension, placebo) and 1 subject
was receiving analgesic medication (mild hypertension, placebo). As
a result, 32 prehypertensive subjects (17 in the placebo group and
15 in the GH group) and 40 mildly hypertensive subjects (21 in the
placebo group and 19 in the GH group) were subjected to efficacy
analysis.
Table I shows the
baseline characteristics of the randomized subjects with
prehypertension or mild hypertension who were assigned to either
the placebo or the GH diet. In each subject population there were
no significant differences between the placebo and GH groups.
Table I also demonstrates that the
mean baseline levels of all physical and biochemical parameters,
with the exception of systolic and diastolic BPs, for the two
groups of mildly hypertensive subjects were within the normal
ranges for clinical measurements.
 | Table I.Baseline characteristics of the
randomized, grouped subjects. |
Table I.
Baseline characteristics of the
randomized, grouped subjects.
| Prehypertensive
| Mildly hypertensive
|
|---|
| Parameter | Placebo group
(n=18) | GH group (n=16) | Placebo group
(n=24) | GH group (n=23) |
|---|
| Age (years) | 47±16 | 53±12 | 53±9 | 54±8 |
| Gender
(male/female) | 11/7 | 10/6 | 13/11 | 13/11 |
| Weight (kg) | 64±13 | 68±13 | 64±10 | 62±9 |
| Body mass index
(kg/m2) | 24±4 | 25±3 | 25±3 | 23±2 |
| Systolic/diastolic BP
(mmHg) | | | | |
| Measured at clinic
visit | 134±3/82±5 | 134±4/83±6 | 142±6/92±6 | 142±6/91±6 |
| Measured at
home | 138±11/84±6 | 143±15/86±8 | 150±12/92±8 | 149±11/94±9 |
| Blood chemistry | | | | |
| LDL-cholesterol
(mg/dl) | 124±34 | 142±37 | 128±39 | 132±26 |
| HDL-cholesterol
(mg/dl) | 62±15 | 55±18 | 61±17 | 71±19 |
| Triglycerides
(mg/dl) | 100±54 | 131±63 | 124±61 | 117±48 |
| Fasting glucose
(mg/dl) | 93±9 | 92±14 | 94±9 | 94±10 |
| HbA1c (%) | 5.1±0.3 | 5.1±0.3 | 5.1±0.3 | 5.1±0.3 |
| Dietary
composition | | | | |
| Total energy
(kcal/day) | 1838±367 | 1753±239 | 1911±578 | 1845±506 |
| Total protein
(g/day) | 66±19 | 68±13 | 71±25 | 73±18 |
| Total fat
(g/day) | 59±18 | 55±17 | 67±27 | 63±29 |
| Total carbohydrate
(g/day) | 249±52 | 236±40 | 248±78 | 237±55 |
| Total mineral
(g/day) | 9.3±1.2 | 10.1±2.2 | 10.1±3.6 | 10.2±3.3 |
| Exercise-associated
energy consumption (kcal/day)a | 313±160 | 245±139 | 240±123 | 217±102 |
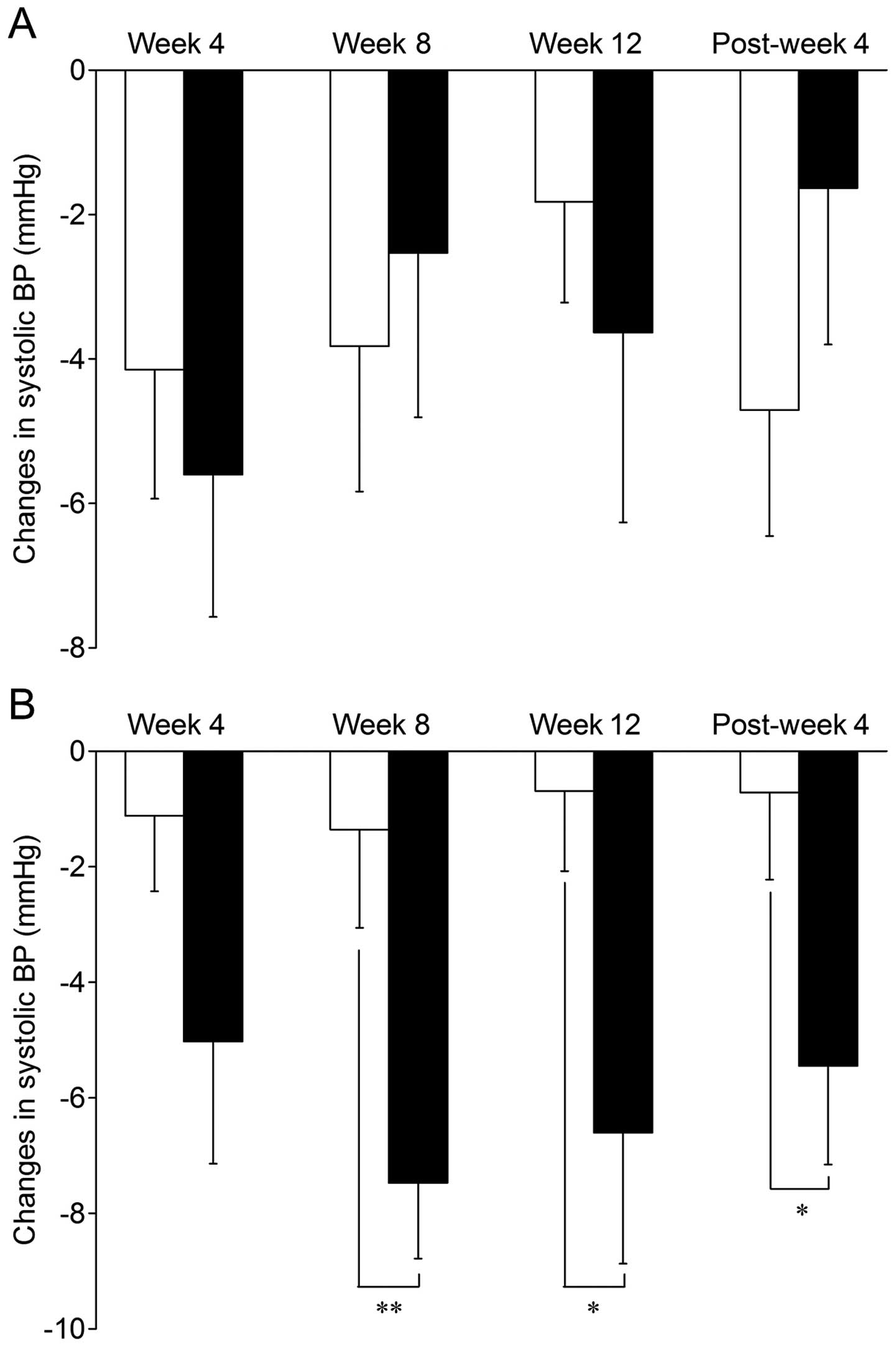
Effect on systolic and diastolic BPs
The changes in the mean value of the systolic BP
over the 12-week treatment period and the subsequent 4-week
post-treatment follow-up period are shown in Table II. In prehypertensive subjects,
systolic BP was not consistently modified by the GH diet treatment.
Although there was a significant reduction from the baseline figure
at week 4 of GH diet treatment (3.4%, P<0.05), reductions of a
similar extent (3–4%, P<0.05 each) were also observed in the
placebo group at week 4 and post-week 4. By contrast, in mildly
hypertensive subjects, the GH diet treatment significantly reduced
systolic BP at week 4 (3.5%; P<0.05), week 8 (5.3%; P<0.01)
and week 12 (4.6%; P<0.01), as well as at post-week 4 (3.9%;
P<0.05), while no such significant reduction was observed at any
time following the intake of the placebo. As shown in Fig. 1, there were significant differences
between the GH and placebo groups of mildly hypertensive subjects
at week 8 (mean change from baseline: GH, −7.5±1.3 mmHg; placebo,
−1.4±1.7 mmHg; P<0.01) and week 12 (mean change from baseline:
GH, −6.6±2.3 mmHg; placebo, −0.7±1.4 mmHg; P<0.05), as well as
at post-week 4 (mean change from baseline: GH, −5.4±1.7 mmHg;
placebo, −0.7±1.5 mmHg; P<0.05).
 | Table II.Changes in systolic BP measured over
the 12-week treatment and 4-week post-treatment follow-up periods
in prehypertensive and mildly hypertensive subjects. |
Table II.
Changes in systolic BP measured over
the 12-week treatment and 4-week post-treatment follow-up periods
in prehypertensive and mildly hypertensive subjects.
| Prehypertensive
| Mildly hypertensive
|
|---|
| Time | Placebo group
(n=17) | GH group
(n=15) | Placebo group
(n=21) | GH group
(n=19) |
|---|
| Baseline | 133.6±0.8 | 133.5±1.2 | 142.3±1.2 | 142.7±1.3 |
| Week 4 | 129.4±1.6a | 127.9±1.7a | 141.2±1.9 | 137.7±2.2a |
| Week 8 | 129.7±2.0 | 131.0±1.7 | 140.9±1.9 | 135.2±1.5b |
| Week 12 | 131.7±1.4 | 129.9±2.1 | 141.6±1.6 | 136.1±1.8b |
| Post-week 4 | 128.9±1.6a | 131.9±1.5 | 141.6±2.0 | 137.2±1.5b |
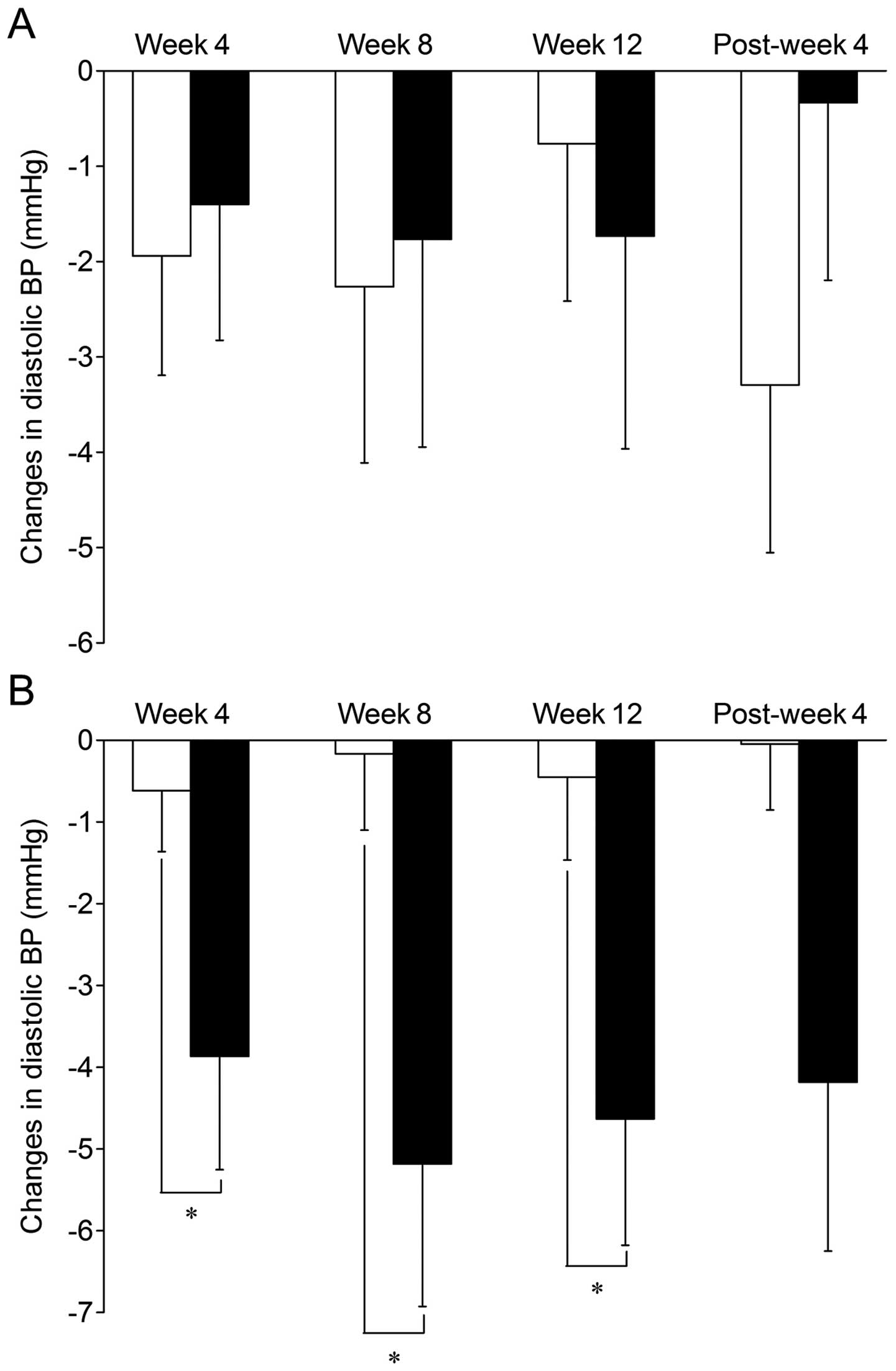
The GH diet treatment also had a hypotensive effect
on the diastolic BP in prehypertensive and mildly hypertensive
subjects. Table III shows that
while the mean diastolic BP for the prehypertensive subjects was
not significantly modified by the GH diet treatment throughout the
study period, the values for mildly hypertensive subjects were
significantly lowered when compared with the baseline at week 4
(4.3%; P<0.05), week 8 (5.8%; P<0.01) and week 12 (5.1%;
P<0.01). Fig. 2 shows that
between-group differences in the diastolic BP for mildly
hypertensive subjects reached significant levels at week 4 (mean
change from baseline: GH, −3.9±1.4 mmHg; placebo, −0.6±0.7 mmHg;
P<0.05), week 8 (mean change from baseline: GH, −5.2±1.7 mmHg;
placebo, −0.2±0.9 mmHg; P<0.05) and week 12 (mean change from
baseline: GH, −4.6±1.5 mmHg; placebo, −0.5±1.0 mmHg; P<0.05),
while no such significant between-group differences were observed
for prehypertensive subjects at any time.
 | Table III.Changes in diastolic BP measured over
the 12-week treatment and 4-week post-treatment follow-up periods
in prehypertensive and mildly hypertensive subjects. |
Table III.
Changes in diastolic BP measured over
the 12-week treatment and 4-week post-treatment follow-up periods
in prehypertensive and mildly hypertensive subjects.
| Prehypertensive
| Mildly hypertensive
|
|---|
| Time | Placebo group
(n=17) | GH group
(n=15) | Placebo group
(n=21) | GH group
(n=19) |
|---|
| Baseline | 82.0±1.1 | 82.6±1.7 | 91.2±1.3 | 90.2±1.6 |
| Week 4 | 80.1±1.3 | 81.2±1.3 | 90.6±1.3 | 86.3±1.5a |
| Week 8 | 79.7±2.0 | 80.9±1.4 | 91.0±1.6 | 85.0±1.0b |
| Week 12 | 81.2±1.6 | 80.9±1.6 | 90.8±1.6 | 85.6±1.5b |
| Post-week 4 | 78.7±1.8 | 82.3±1.7 | 91.2±1.6 | 86.0±1.6 |
Numerous clinical studies performed in the past 30
years to examine the hypotensive effect of garlic preparations have
shown controversial results, as have been summarized in 5
systematic reviews and/or meta-analyses (12–15,17).
Whereas several trials have suggested that garlic has possible
BP-lowering effects, a larger number of published studies have
reported virtually no effect. However, it is notable that all
positive studies were performed using hypertensive subjects
(baseline systolic BP, ≥140 mmHg) (18–21)
and that, by contrast, almost all negative studies used
normotensive subjects (systolic BP, <140 mmHg) as the study
population (22–26).
Consistent with these existing positive reports, the
present study, in which a new garlic-based supplementary diet, the
GH diet was used, and showed that it significantly reduced systolic
and diastolic BPs in mildly hypertensive subjects following 8- and
12-week treatments, and that, by contrast, the treatment does not
impact BP in prehypertensive subjects. This latter finding may
reflect a pharmacological phenomenon that has been reported with
certain antihypertensive medications; as the BP approaches normal
values, antihypertensives have less effect. The type of study
population (whether the subjects are normotensive or hypertensive)
is crucial in determing the BP-lowering effects of garlic and its
preparations, including the GH diet, as suggested in the two
meta-analyses (13,14). Although short-term (12-week)
treatment with the GH diet had no significant BP-reducing effects
in prehypertensive subjects, long-term trials are warranted to
examine whether this garlic preparation may be effective in
forestalling progression into a hypertensive state, as observed in
treatment with certain other antihypertensives (2,27).
The results obtained from the mildly hypertensive
subject groups in the present study appear to be in accordance with
those from earlier positive placebo-controlled studies
demonstrating the significant hypotensive effects of conventional
garlic preparations, mainly dried garlic powder products, in
individuals who had mild or moderate hypertension (18–21,28).
Several meta-analyses of placebo-controlled trials, evaluating the
efficacy of commercial, dried garlic powder products in daily doses
of 600–900 mg in the treatment of high BP, revealed reductions in
systolic BP and diastolic BP of 7–16 and 3–9 mmHg, respectively
(12–14). The results of the present study
from an 8- or 12-week intake of GH diet, in a daily dose of 300 mg
as dehydrated garlic homogenate, showed decreases of 6.6–7.5 mmHg
and 4.6–5.2 mmHg from the baseline or placebo in systolic and
diastolic BPs, respectively, in subjects with mild hypertension.
Therefore, the hypotensive effects of the GH diet do not appear to
be dissimilar to those reported for dried garlic powder products.
The findings of the present study on the hypotensive effects of the
GH diet would have beneficial implications on health at the
population level, where a reduction of 4–5 mmHg in systolic BP and
2–3 mmHg in diastolic BP has been estimated to reduce the risk of
cardiovascular morbidity and mortality by 8–20% (29).
The mechanisms behind the hypotensive action of the
GH diet and the active component(s) involved remain in need of
clarification. Our previous animal and in vitro studies
demonstrated that the GH diet and its major sulfur-containing
constituent, γ-glutamyl-S-allyl-cysteine (GSAC), are able to lower
BP in hypertensive rats (30).
They have the activities required to inhibit angiotensin
I-converting enzyme (ACE) and to induce endothelium-dependent and
-independent relaxation of the isolated rat aorta (16,31).
This leads us to consider the possibility that GSAC with its
ACE-inhibitory and vasodilating activities may play a major role in
the hypotensive effect of the GH diet in subjects with high BP.
Effect on hematology and blood
chemistry
There were no hematological or blood chemistry
parameters that demonstrated a significant change from the baseline
in subjects consuming the GH diet over the placebo throughout the
study period when analyzed with prehypertensive subjects and mildly
hypertensive subjects separately (data not shown). Of all the
laboratory parameters, the most prominent change over time was
observed for the LDL-cholesterol level in the GH group. When
compared with the baseline figures, mean values were decreased by
5.3 mg/dl (4.0%; P>0.05) at week 4, by 7.7 mg/dl (5.7%;
P>0.05) at week 8, by 13.1 mg/dl (9.8%; P<0.05) at week 12
and by 6.0 mg/dl (4.5%; P>0.05) at post-week 4.
We observed no significant effects from the 12-week
intake of the GH diet versus the placebo on any laboratory
parameters, including those correlated with metabolic diseases.
However, it remains likely that GH may have a potential for
reducing LDL-cholesterol, as the mean values for the GH group were
reduced significantly at all times during the 12-week treatment
period compared with the baseline figures. With regard to the
potential of garlic preparations, particularly the dried garlic
powder, for lowering blood levels of total cholesterol and/or
LDL-cholesterol, mixed results have been obtained from a large
number of prior randomized, double-blind placebo-controlled trials,
as observed in a systemic review by Turner et al(32) and a meta-analysis by Khoo and Aziz
(33). Larger scale, long-term
trials are likely to be required to determine whether there is a
possible beneficial effect of GH diet on blood cholesterol.
Safety and tolerability
The GH diet and the placebo were well tolerated.
When the whole study population was analyzed, the incidence and
pattern of adverse events that occurred throughout the 12-week
treatment period and the 4-week follow-up period in the GH group
were almost equivalent to those in the placebo group. Only 6 of the
34 subjects (18%) in the GH group and 7 of the 38 subjects (18%) in
the placebo group reported minor adverse events, the most common
being gastric distress (5 in the GH group and 4 in the placebo
group). Less frequent adverse events included headaches (3 each in
the GH and placebo groups) and abdominal pain with diarrhea (3
events in the GH group and 1 in the placebo group). All these
self-recorded adverse events were extremely mild in intensity,
occurred only temporarily and were judged by the investigator as
unrelated to the study treatment. It is noteworthy that none of the
subjects on the GH diet reported a garlic taste, garlic breath or
an unpleasant body odor.
A 12-week treatment with the GH diet had no
clinically significant untoward side-effects. It is generally
accepted that garlic is safe in a wide range of doses. Only a few
studies among a large number of clinical trials have reported the
occurrence of adverse events as a result of treatment with garlic
preparations. The most frequent event or complaint associated with
garlic therapy is a garlic odor on the breath and body, with the
next complaints being mild gastrointestinal adverse events,
including nausea, bloating and flatulence (34). The results of the present study
showed that no subjects treated with the GH diet reported
intolerable garlic odor or any other side-effect. Coating the
garlic homogenate core with a capsule and/or combining it with egg
yolk may contribute to the safety and tolerability of the GH
diet.
In conclusion, the results of the present study have
demonstrated that a daily 300-mg as dehydrated garlic homogenate
dose of the GH diet lowered systolic BP by 6.6–7.5 mmHg and
diastolic BP by 4.6–5.2 mmHg in subjects with mild hypertension,
but not in those with prehypertension, following an 8- or 12-week
treatment. The substantial hypotensive effects of the GH diet
appeared to continue for at least 4 weeks following the termination
of the 12-week treatment. The GH diet was well tolerated without
any clinically significant untoward effects. These results lead us
to the conclusion that GH diet may have certain benefits as a
complementary therapy for mildly hypertensive subjects.
References
|
1.
|
Kannel WB: Framingham study insights into
hypertensive risk of cardiovascular disease. Hypertens Res.
18:181–196. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Chobanian AV, Bakris GL, Black HR, Cushman
WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright
JT Jr and Roccella EJ; National Heart, Lung and Blood Institute
Joint National Committee on Prevention, Detection, Evaluation, and
Treatment of High Blood Pressure and National High Blood Pressure
Education Program Coordinating Committee: The Seventh Report of the
Joint National Committee on prevention, detection, evaluation, and
treatment of high blood pressure: the JNC 7 report. JAMA.
289:2560–2572. 2003. View Article : Google Scholar
|
|
3.
|
Chockalingam A: World hypertension day and
global awareness. Can J Cardiol. 24:441–444. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Julius S and Shork MA: Borderline
hypertension - a critical review. J Chronic Dis. 23:723–754. 1971.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Vasan RS, Larson MG, Leip EP, Kannel WB
and Levy D: Assessment of frequency of progression to hypertension
in non-hypertensive participants in the Framingham Heart Study: a
cohort study. Lancet. 358:1682–1686. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Vasan RS, Larson MG, Leip EP, Evans JC,
O'Donnell CJ, Kannel WB and Levy D: Impact of high-normal blood
pressure on the risk of cardiovascular disease. N Engl J Med.
345:1291–1297. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
The Japanese Society of Hypertension:
Japanese Society of Hypertension guidelines for the management of
hypertension 2004 (JSH 2004). Hypertens Res. 29(Suppl): S1–S105.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Banerjee SK and Maulik SK: Effect of
garlic on cardiovascular disorders: a review. Nutr J. 1:42002.
View Article : Google Scholar
|
|
9.
|
Brace LD: Cardiovascular benefits of
garlic (Allium sativum L). J Cardiovasc Nurs. 16:33–49.
2002. View Article : Google Scholar
|
|
10.
|
Yeh GY, Davis RB and Phillips RS: Use of
complementary therapies in patients with cardiovascular disease. Am
J Cardiol. 98:673–680. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Chen ZY, Peng C, Jiao R, Wong YM, Yang N
and Huang Y: Anti-hypertensive nutraceuticals and functional foods.
J Agric Food Chem. 57:4485–4499. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Ackermann RT, Mulrow CD, Ramirez G,
Gardner CD, Morbidoni L and Lawrence VA: Garlic shows promise for
improving some cardiovascular risk factors. Arch Intern Med.
161:813–824. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Reinhart KM, Coleman CI, Teevan C,
Vachhani P and White CM: Effects of garlic on blood pressure in
patients with and without systolic hypertension: a meta-analysis.
Ann Pharmacother. 42:1766–1771. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Ried K, Frank OR, Stocks NP, Fakler P and
Sullivan T: Effect of garlic on blood pressure: a systematic review
and meta-analysis. BMC Cardiovasc Disord. 8:132008. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Simons S, Wollersheim H and Thien T: A
systematic review on the influence of trial quality on the effect
of garlic on blood pressure. Neth J Med. 67:212–219.
2009.PubMed/NCBI
|
|
16.
|
Tanaka S, Watabe K and Yamaguchi H:
Studies on the mechanism of antihypertensive action of a garlic
homogenate-based diet ‘Dento Ninniku Ran-ou’ using isolated rat
aorta preparations. Oyo Yakuri (Pharmacometrics). 82:21–28.
2012.(In Japanese).
|
|
17.
|
Silagy CA and Neil HA: A meta-analysis of
the effect of garlic on blood pressure. J Hypertens. 12:463–468.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Kandziora J: The blood pressure lowering
and lipid lowering effect of a garlic preparation in combination
with a diuretic. Arztl Forsch. 3:1–8. 1988.
|
|
19.
|
Vorberg G and Schneider B: Therapy with
garlic: results of a placebo-controlled, double-blind study. Br J
Clin Pract Suppl. 69:7–11. 1990.PubMed/NCBI
|
|
20.
|
De Santos AOS and Grunwald J: Effect of
garlic powder tablets on blood lipids, blood pressure and well
being. A placebo controlled double-blind study. Br J Clin Res.
4:37–44. 1993.
|
|
21.
|
Sobenin IA, Andrianova IV, Fomchenkov IV,
Gorchakova TV and Orekhov AN: Time-released garlic powder tablets
lower systolic and diastolic blood pressure in men with mild and
moderate arterial hypertension. Hypertens Res. 32:433–437. 2009.
View Article : Google Scholar
|
|
22.
|
Jain AK, Vargas R, Gotzkowsky S and
McMahon FG: Can garlic reduce levels of serum lipids? A controlled
clinical study. Am J Med. 94:632–635. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Isaacsohn JL, Moser M, Stein EA, Dudley K,
Davey JA, Liskov E and Black HR: Garlic powder and plasma lipids
and lipoproteins: A multicenter, randomized, placebo-controlled
trial. Arch Intern Med. 158:1189–1194. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Zhang XH, Lowe D, Giles P, Fell S, Board
AR, Baughan JA, Connock MJ and Maslin DJ: A randomized trial of the
effects of garlic oil upon coronary heart disease risk factors in
trained male runners. Blood Coagul Fibrinolysis. 11:67–74. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Williams MJ, Sutherland WH, McCormick MP,
Yeoman DJ and de Jong SA: Aged garlic extract improves endothelial
function in men with coronary artery disease. Phytother Res.
19:314–319. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Macan H, Uykimpang R, Alconcel M, Takasu
J, Razon R, Amagase H and Niihara Y: Aged garlic extract may be
safe for patients on warfarin therapy. J Nutr. 136(Suppl 3):
793S–795S. 2006.PubMed/NCBI
|
|
27.
|
Julius S, Nesbitt SD, Egan BM, Weber MA,
Michelson EL, Kaciroti N, Black HR, Grimm RH Jr, Messerli FH,
Oparil S and Schork MA; Trial of Preventing Hypertension (TROPHY)
Study Investigators: Feasibility of treating prehypertension with
an angiotensin–receptor blocker. N Engl J Med. 354:1685–1697.
2006.
|
|
28.
|
Auer W, Eiber A, Hertkorn E, Hoehfeld E,
Koehrle U, Lorenz A, Mader F, Merx W, Otto G, Schmid-Otto B, et al:
Hypertension and hyperlipidaemia: garlic helps in mild cases. Br J
Clin Pract Suppl. 69:3–6. 1990.PubMed/NCBI
|
|
29.
|
McInnes GT: Lowering blood pressure for
cardiovascular risk reduction. J Hypertens Suppl. 23:S3–S8. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Tanaka S, Watabe K, Ubukata K and
Yamaguchi H: Antihypertensive effects of ‘garlic-egg’ powder and
γ-glutamyl-S-allyl-cysteine (GSAC), in spontaneously hypertensive
rats. Oyo Yakuri (Pharmacometrics). 71:73–78. 2006.(In
Japanese).
|
|
31.
|
Watabe K, Tanaka S and Yamaguchi H:
Studies on the mechanism of antihypertensive action of a
constituents of garlic, γ-glutamyl-S-allyl-cysteine (GSAC). Oyo
Yakuri (Pharmacometrics). 71:79–87. 2006.(In Japanese).
|
|
32.
|
Turner B, Mølgaard C and Marckmann P:
Effect of garlic (Allium sativum) powder tablets on serum
lipids, blood pressure and arterial stiffness in normo-lipidaemic
volunteers: a randomized, double-blind, placebo-controlled trial.
Br J Nutr. 92:701–706. 2004.
|
|
33.
|
Khoo YS and Aziz Z: Garlic supplementation
and serum cholesterol: a meta-analysis. J Clin Pharm Ther.
34:133–145. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
Borrelli F, Capasso R and Izzo AA: Garlic
(Allium sativum L): adverse effects and drug interactions in
humans. Mol Nutr Food Res. 51:1386–1397. 2007.
|