Introduction
The importance of nutrition during pregnancy with
regard to pregnancy outcome has long been acknowledged. This
importance has only been further emphasized by the recent changes
in food quality and availability, lifestyle changes and a new
understanding of foetal programming’s effects on adult outcomes
(1). The Mediterranean dietary
pattern (MDP) exerts certain beneficial effects, since it appears
to be associated with a reduction in the risk of offspring affected
by spina bifida (2) and with
children presenting as less wheezy or asthmatic (3). Recently, Mariscal-Arcas et
al(4), proposed a diet quality
index for pregnancy based on MDP evaluating the diet of a group of
pregnant women by applying the Mediterranean Diet Score (MDS) and
evaluating their intake of micronutrients required in optimal
amounts during pregnancy.
Pregnancy is also associated with major
physiological and future psychosocial changes, and maternal
adaptation to these changes is crucial for normal foetal
development. Psychological stress in pregnancy predicts an earlier
birth and lower birth weight. Perceived life-event stress, as well
as depression and anxiety, predicted lower birth weight, decreased
Apgar scores and occurrence of babies small for their gestational
age (5). Therefore, it appears
that pregnancy-specific stress may be a more powerful contributor
to birth outcomes than general stress (6).
It has also been reported that women who had
unplanned pregnancies had more psychological problems throughout
their pregnancies when compared with those that planned their
pregnancy (7). These novel
findings suggest an important finding, it is estimated that
approximately 87 million pregnancies take place every year
worldwide, out of which 41 million result in labour (WHO 2005). Our
working hypothesis is that for a successful pregnancy certain
events at the nutritional, immune, psycho-emotional and genetic
level may be tightly linked. Therefore, in this study we followed a
‘holistic’ approach to investigate how maternal stress, nutrition,
pregnancy planning and exercise influence pregnancy outcome.
Subjects and methods
Subjects
The study population consisted of pregnant women
(n=113) attending the Department of Obstetrics and Gynaecology,
University Hospital, University of Crete Medical School (Crete,
Greece). The participants were in the third trimester of their
pregnancy. All participants gave informed consent to participate in
the study and ethical approval was granted by the local Ethics
Committee of the Hospital.
Construction of the questionnaire
A questionnaire was constructed comprising 59
questions, which were associated with the following specific
subject areas and variables: i) body mass index (BMI), ii) immune
problems, iii) exercise, iv) nutrition, v) stress and vi) medical
history. Specific questions were used to acquire anthropometric
data, which included gestational age, weight of the mother prior to
conception as well as the weight of the mother at the time and
self-reported height. Behavioural data that were collected,
including smoking and drinking habits, and physical activity, the
latter based on the measure of Paffenbarger et al(8). Also, multi-mineral/multi-vitamin
supplement usage before and during pregnancy was assessed. There
were specific questions associated with the stress profile, which
included: whether the pregnancy was planned or not planned and how
stressed each woman was during pregnancy, with responses ranging
from 1 to 4 (1, low; 2, medium; 3, high; 4, very high). This stress
questionnaire was adapted from a study by Wang et
al(9), where women with
dysmenorrhoea were asked to describe their stress in preceding
cycles as ‘low’, ‘medium’ or ‘high’, whereas the questions
associated with nutritional status were based on the Department of
Health Services - Women, Infants and Children Program (CA, USA;
www.sonoma-county.org/health/wic/en/applications/pregnancy.pdf).
Statistical analysis
We tested the association between continuous
predictors (e.g. age, stress levels) and infant weight using
Pearson correlations and partial correlations (when adjusting for
age and BMI). We used Student’s t-tests for dichotomous predictors
(e.g. planned pregnancy) and analysis of variance (ANOVA) for
testing the association between attitude type (initially in three
categories) and infant birth weight. For the correlation studies, a
two-tailed test using SPSS (version 18) was performed. P<0.05
was considered to indicate a statistically significant result.
Results
General profile of the participants of
the study
The data of the general profile that were collected
are presented in Table I. The
majority of the participants appeared to be of normal BMI.
Information of the weight of the mother as a newborn, as well as if
she was born at term or pre-term, was also collected, and the
majority of the participants were born in the normal for
gestational age range and after the 37th week of gestation, which
is considered to be at term. The maternal body shape was also
recorded to understand the participant adiposity type. The majority
of women reported to have a pear-shape body type. Information on
the duration of the pregnancy as well as the weight of the foetus
was also recorded. Notably, a slightly higher percentage of the
infants were born prematurely (<37 weeks).
 | Table I.Demographic details of the general
cohort. |
Table I.
Demographic details of the general
cohort.
| General profile | Percentage |
|---|
| Age (years) | |
| ≤20 | 7.7 |
| 21–30 | 56.7 |
| 31–40 | 35.6 |
| BMI | |
| Underweight
(<18.5) | 13.6 |
| Normal
(18.5–24.9) | 64.1 |
| Overweight
(25–29.9) | 12.6 |
| Obese (>30) | 9.7 |
| Weight of mother as
newborn (g) | |
| Small
(<2,500) | 5.1 |
| Normal
(2,500–3,800) | 85.6 |
| Large
(>3,800) | 9.3 |
| Born prematurely | |
| Yes | 7.1 |
| No | 92.9 |
| Body shape (BP)
mostly matches yours | |
| Apple-shape | 8.7 |
| Pear-shape | 56.3 |
|
Proportionate-shape | 35.0 |
| Duration of pregnancy
(weeks) | |
| Term (>37) | 43.2 |
| Pre-term
(<37) | 56.8 |
| Foetal weight
(g) | |
| Small
(<2,500) | 25.3 |
| Normal
(2,500–3,800) | 72.8 |
| Large
(>3,800) | 1.9 |
Immune profile of the participants
The second profile that was analysed was the immune
profile of the participants, which consisted of 7 questions in
total (Table II). A significant
inverse correlation was observed between difficulty to ‘fight’ an
infection and number of colds (r=−0.289, P=0.003) as well as number
of infections (r=−0.446, P<0.0001) during pregnancy. An inverse
correlation was also observed between pregnancy days and number of
infections during pregnancy (r=−0.212, P=0.004). Notably, the use
of antibiotics was also inversely correlated with difficulty to get
rid of a cold (r=−0.422, P<0.0001) and how prone these women
were to cystitis infections (r=−0.389, P<0.0001).
 | Table II.Details of the immune profile of the
participants in our study. |
Table II.
Details of the immune profile of the
participants in our study.
| Immune profile | Percentage |
|---|
| How many colds did
you get during pregnancy? | |
| 0 | 68.9 |
| 1 | 6.8 |
| 2 | 21.4 |
| 3 | 1.9 |
| 4 | 1.0 |
| How many infections
did you get during pregnancy? | |
| 0 | 77.9 |
| 1 | 10.6 |
| 2 | 9.6 |
| 3 | 1.9 |
| Do you find it hard
to ‘fight’ an infection (e.g. cold)? | |
| Yes | 36.5 |
| No | 63.5 |
| Are you prone to
thrush or cystitis? | |
| Yes | 16.3 |
| No | 83.7 |
| How often did you
take antibiotics in the last month? | |
| None | 71.1 |
| Once | 21.2 |
| Twice | 4.8 |
| More than 3
times | 2.9 |
| Do you have an
inflammatory disease (e.g. arthritis)? | |
| Yes | 6.8 |
| No | 93.2 |
| Do you suffer from
hay fever, allergies? | |
| Yes | 2.9 |
| No | 97.1 |
Exercise profile prior to and during
pregnancy
The majority of the women reported to have light
activity, this consisted of 2–4 flights of stairs that they climbed
on a daily basis and this is consistent before as well as during
pregnancy (Table III). As far as
their walking habits were concerned, an almost equal percentage of
women reported a light or moderate walking activity before
pregnancy, whereas this moderate activity was lower during
pregnancy and the light walking activity (equivalent of 2–4 city
blocks) was the highest category. With regard to participation in
light sports, the inactivity was increased to 60% during pregnancy.
When the participants were asked the number of h/week they would
participate in any strenuous sports, including running, cycling or
tennis, again the majority reported to be inactive both before and
during their pregnancy.
 | Table III.Details of the exercise profile of
the participants in our study. |
Table III.
Details of the exercise profile of
the participants in our study.
| Exercise
profile | BP (%) | DP (%) |
|---|
| How many flights of
stairs do you climb each day (10 steps=one flight)? | | |
| Inactive (0–1
flight of stairs) | 23.1 | 31.7 |
| Light (2–4
flights of stairs) | 47.1 | 47.1 |
| Moderate (5–7
flights of stairs) | 29.8 | 21.2 |
| Active (8+
flights of stairs) | 0.0 | 0.0 |
| How many city
blocks do you walk each day (1 block=130 m)? | | |
| Inactive (0–1
city blocks) | 12.5 | 23.1 |
| Light (2–4 city
blocks) | 34.6 | 42.3 |
| Moderate (5–7
city blocks) | 31.7 | 22.1 |
| Active (8+ city
blocks) | 21.2 | 12.5 |
| How many h/week do
you participate in any light sports (e.g. dancing, gardening,
walking)? | | |
| Inactive (0–1.5
h/week) | 41.3 | 59.6 |
| Light (1.6–2.5
h/week) | 22.1 | 28.8 |
| Moderate (2.6–3.5
h/week) | 28.8 | 8.7 |
| Active (3.6+
h/week) | 7.7 | 1.9 |
| How many h/week do
you participate in any strenuous sports (e.g. running, cycling,
swimming, tennis)? | | |
| Inactive (0–1.5
h/week) | 76.9 | 93.3 |
| Light (1.6–2.5
h/week) | 8.7 | 6.7 |
| Moderate (2.6–3.5
h/week) | 12.5 | 0.0 |
| Active (3.6+
h/week) | 1.9 | 0.0 |
Nutrition profile before and during
pregnancy
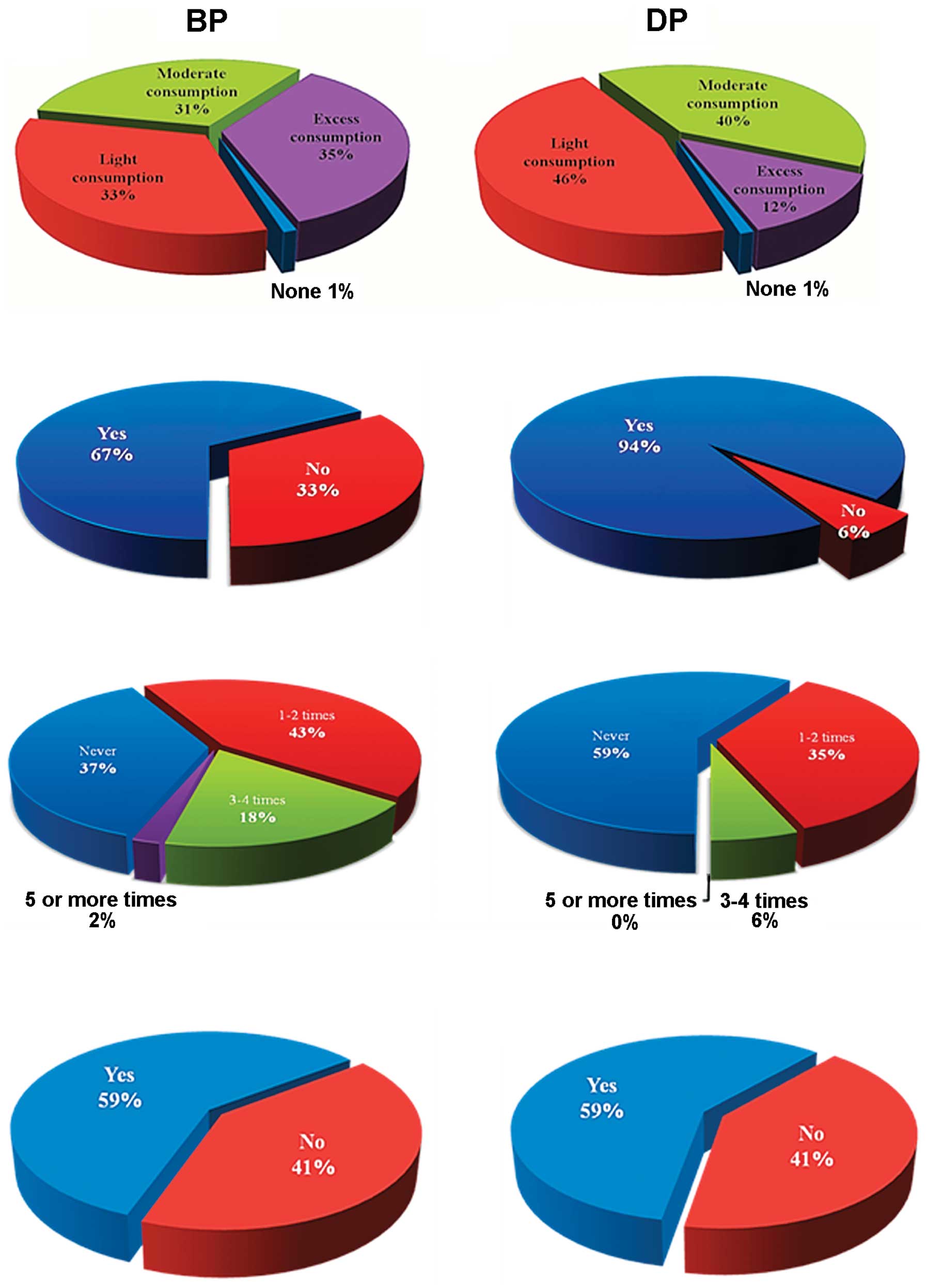
The vast majority of the participants were not
vegetarians and this percentage remained unchanged during pregnancy
(Table IV). When the participants
were asked how many of their weekly meals included foods that are
high in lipids and more specifically in saturated lipids (e.g.
pies, pastries, fried foods) the majority reported to excessively
(≥5 times/week) consume these types of foods rich in lipids before
pregnancy, whereas this percentage was lowered significantly during
pregnancy, where the majority reported light consumption of these
foods (Fig. 1A and B). A high
percentage of women reported to moderately consume vegetables on a
daily basis before pregnancy and this was maintained during
pregnancy. This was also consistent with the responses obtained
with regard to the daily consumption of fruits, before as well as
during pregnancy, where the majority reported to moderately consume
fruits in both periods.
 | Table IV.Details of the nutritional profile of
the participants in our study. |
Table IV.
Details of the nutritional profile of
the participants in our study.
| Nutrition
profile | BP (%) | DP (%) |
|---|
| Are you
vegetarian? | | |
| Yes | 7.8 | 7.8 |
| No | 92.2 | 92.2 |
| How often do you
buy full-fat dairy products? | | |
| Often | 63.1 | N/A |
| Rarely | 36.9 | N/A |
| How many meals per
week would include any of the following: pies, pastries, fried
foods? | | |
| None (0) | 1.0 | 1.0 |
| Light consumption
(1–2) | 33.0 | 46.1 |
| Moderate
consumption (3–4) | 31.1 | 40.2 |
| Excess
consumption (≥5) | 35.0 | 12.7 |
| How many servings
of vegetables/legumes do you have each day? | | |
| None (0) | 3.9 | 2.9 |
| Light consumption
(1–2) | 38.8 | 29.4 |
| Moderate
consumption (3–4) | 52.4 | 60.8 |
| Excess
consumption (≥5) | 4.9 | 6.9 |
| How many servings
of fruit do you have each day? | | |
| None (0) | 1.9 | 1.0 |
| Light consumption
(1–2) | 32.1 | 17.6 |
| Moderate
consumption (3–4) | 50.5 | 65.7 |
| Excess
consumption (≥5) | 15.5 | 15.7 |
| How many servings
of cereals do you have each day? | | |
| None (0) | 2.9 | 2.0 |
| Light consumption
(1–2) | 1.9 | 1.0 |
| Moderate
consumption (3–4) | 33.1 | 32.6 |
| Excess
consumption (≥5) | 62.1 | 64.4 |
| Do you eat
iron-rich foods (e.g. lean red meat, chicken, green leafy
vegetables) every day?a | | |
| Yes | 66.7 | 94.1 |
| No | 33.3 | 5.9 |
| Do you eat ≥2
servings of cheese, milk, yoghurt or calcium-enriched milk every
day?b | | |
| Yes | 65.0 | 85.3 |
| No | 35.0 | 14.7 |
| How much
water/sugar-free drinks do you drink each day? | | |
| <½ liter | 5.8 | 3.0 |
| ½ to 1 liter | 8.8 | 4.0 |
| >1 liter | 85.4 | 93.0 |
| How many cups of
coffee, black tea or caffeine-containing beverages do you drink
each day?a | | |
| 4–6 | 1.0 | 0.0 |
| 3–4 | 27.2 | 2.0 |
| 2–3 | 43.6 | 12.7 |
| ≤1 | 28.2 | 85.3 |
| How many soda,
sugary drinks do you normally have each day?a | | |
| >3 | 36.9 | 2.0 |
| 2–3 | 38.8 | 29.4 |
| ≤1 | 24.3 | 68.6 |
| How many alcoholic
beverages do you consume on a weekly basis?a | | |
| >5 | 0.0 | 0.0 |
| 3–4 | 14.6 | 1.0 |
| ≤2 | 23.3 | 5.2 |
| None | 62.1 | 93.8 |
| How many times a
week do you eat fast food? | | |
| Never | 36.9 | 58.8 |
| 1–2 times | 42.8 | 35.3 |
| 3–4 times | 18.4 | 5.9 |
| ≥5 times | 1.9 | 0.0 |
Also, the majority of the participants reported to
eat iron-rich foods (e.g. lean red meat, chicken, green leafy
vegetables) on a daily basis before pregnancy, but the percentage
of pregnant women consuming more iron-rich foods on a daily basis
was significantly increased compared to pre-pregnancy (Fig. 1C and D). A high percentage of women
reported to consume 2–3 cups of coffee or other caffeine-containing
beverages before pregnancy, however, during pregnancy the majority
of women reduced their daily consumption to 1 cup or less. In
addition, the percentage of women drinking 2–3 sugary drinks on a
daily basis was reduced during pregnancy to 1 or fewer. The
majority of participants reported not to consume any alcoholic
beverages before or during pregnancy. Lastly, the majority of the
participants reported to eat fast food 1–2 times/week whereas this
was reduced to none during pregnancy (Fig. 1E and F).
With regard to smoking profile, the majority (79%)
of women reported that they did not smoke immediately before their
pregnancy and this was maintained during pregnancy. However, we
emphasize that only 7% of the women reported to have stopped
smoking while pregnant, whereas the remainder of the participants
(14%) reported to have continued this habit. Notably, when asked if
anyone in the household was smoking before and if they had
continued to do so during pregnancy, a high percentage reported
that, before as well as during pregnancy, they were exposed to
passive smoking (Fig. 1G and
H).
Maternal stress and foetal birth
weight
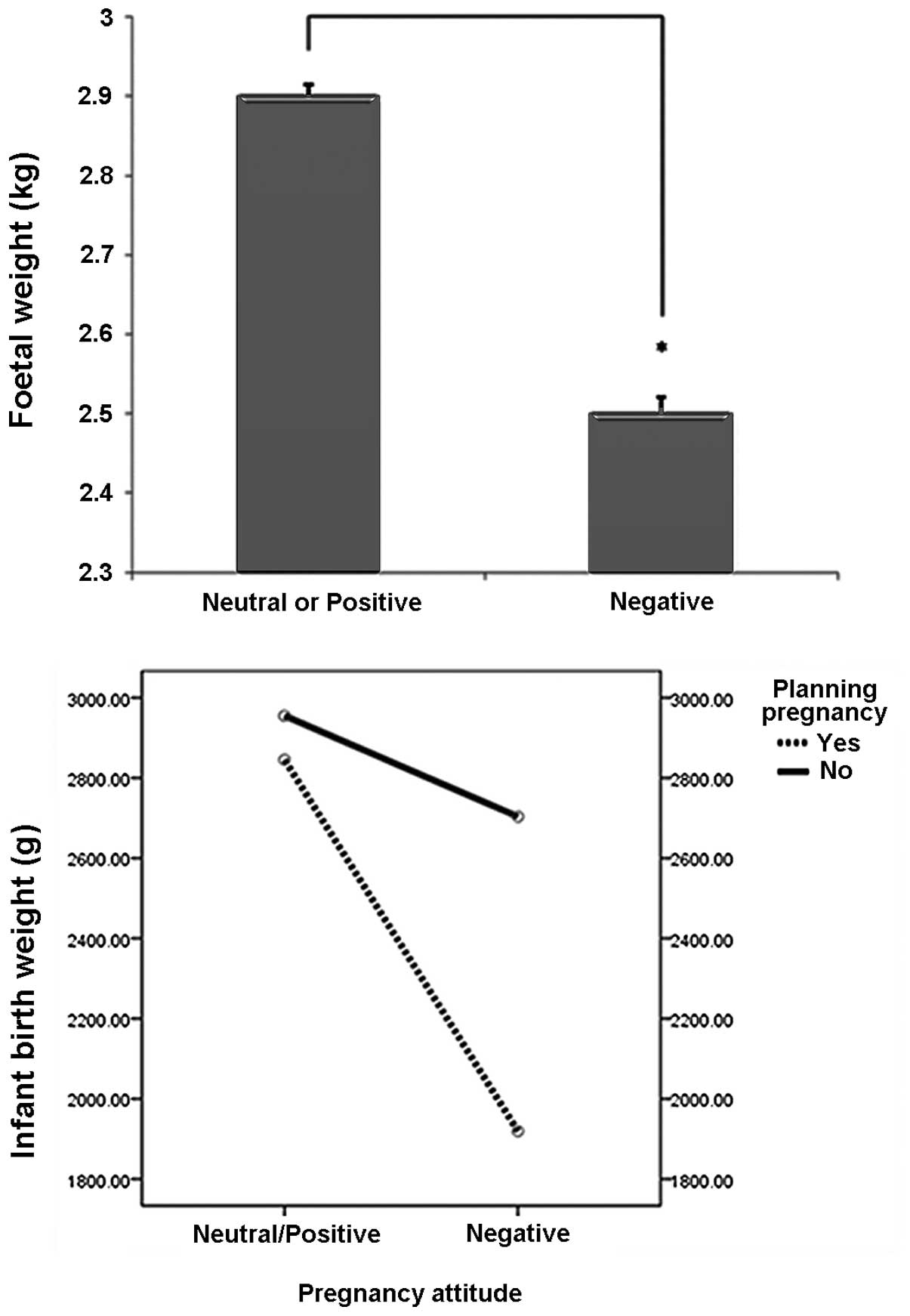
Maternal attitudes were correlated with
self-reported stress status ranging from low and medium (low stress
response) to high and very high (high stress response). The source
of the stress was not reported. The women with negative attitudes
towards their pregnancy reported significantly higher levels of
stress during pregnancy (2.8) compared to women with neutral (1.6)
or positive attitudes towards their pregnancy [1.4; t(95)=9.8,
P<0.001]. Since women with neutral and positive attitudes
towards the pregnancy did not differ on stress levels [t(95)=1.0,
P>0.05], and due to the small number of women with neutral
attitudes, both groups were merged. The women forming the first
group with the positive and neutral attitudes were compared with
those with negative attitudes. The women with negative attitudes
during pregnancy gave birth to infants with significantly lower
birth weights (2.5 kg) than those with a positive or neutral
attitude towards their pregnancy (2.9 kg; F(1,71)=4.2, P<0.05;
Fig. 2A), independent of their age
and BMI.
We then tested whether maternal background variables
predicted infant birth weight. Age, BMI, physical activity, alcohol
consumption and smoking habits during pregnancy were not associated
with infant birth weight (all P>0.05). The majority of immune
symptoms of women (i.e. difficulty overcoming an infection, number
of colds or infections during pregnancy, inflammatory diseases,
proneness to cystitis/thrush, allergies, use of antibiotics) were
also not associated with infant birth weight (all P>0.05).
Effects of maternal attitude to pregnancy
and pregnancy planning on infant birth weight
In planned pregnancies, stress predicted infant
weight, independent of age and BMI (r=−0.44, P=0.01), whereas in
unplanned pregnancies stress did not predict infant weight
(r=−0.19, P=0.23). In mothers with neutral or positive attitudes
towards pregnancy, planning the pregnancy had no effect on infant
birth weight [F(1,30)=0.091, not significant]. However, in mothers
with negative attitudes towards the pregnancy, those with an
unplanned pregnancy gave birth to infants with significantly higher
weights (2681.9 g) than those with planned pregnancies [1917.8 g;
F(1,36)=7.074, P=0.012; Fig.
2B].
Discussion
The present study extends previous findings and
provides new evidence on how psychosocial environment (i.e.
stress/pregnancy planning) affects foetal outcome. We have shown
that there was a significant reduction in the intake of alcohol,
caffeine-containing and sugary drinks, as well as sugary
refreshments during pregnancy. In our cohort 14% of women smoked
during pregnancy. This is comparable to a recent study of
Australian women that showed that 14.8% of non-indigenous women
were smoking during pregnancy (10). Maternal smoking during pregnancy is
a well-established risk factor for perinatal mortality, miscarriage
and premature births (11) and
exposure to heavy smoking in utero increases the risk of
nicotine dependence in adulthood (10). In this study, another notable
finding was identified, that parental/passive smoking was not
reduced in the household during pregnancy, staying at a high rate
of 59%. This could be detrimental, as all types of passive smoking
have been associated with a significant increase in the risk of
infants developing lower respiratory infections in the first two
years of life (12).
In this questionnaire seven questions associated
with the immune profile of this cohort were incorporated. We have
done so, as acute infections in pregnant women are often associated
with adverse effects, including miscarriage, preterm labour,
preeclampsia (PE) or even stillbirth (13–15).
Notably, a significant inverse correlation has been identified
between difficulty to ‘fight’ an infection and number of colds and
number of infections during pregnancy. Similar data have been
obtained by a recent study of Australian women, where a cold was
the most common infection reported using a similar self-reported
method (16). In the study by Lain
et al(16), only 21% of the
women that reported an infection sought medical attention. We do
not have such records for our cohort. However, our data on the
immune profile also have certain strengths as it includes the
investigation of numerous rather than a single infection and
incorporates both chronic and acute infections.
With regard to the effect of caffeine during
pregnancy, there is still some controversy in the field, as it has
been implicated as a cause of spontaneous abortion, intrauterine
growth restriction (IUGR), low birth weight and pre-term delivery
(17). However, other
investigators failed to find any association between caffeine
intake and poor pregnancy outcomes (18). Adeney et al(19) revealed that moderate caffeine
consumption during pregnancy exerts a protective effect towards
gestational diabetes mellitus (GDM) (19). These mixed results may arise due to
the problem of accurately assessing the caffeine intake. In
addition, the amount of caffeine varies greatly in different coffee
chains. In a recent study, caffeine levels varied up to 6-fold
(20). In our cohort, a
significant reduction in caffeine intake was noted, although we
were not able to quantify the precise amount ingested. Nawrot et
al(21) suggested that women
of reproductive age should consume less than 300 mg of
caffeine/day.
In this cohort, a significant decrease in the
consumption of sugar-containing drinks during pregnancy was
observed. In the USA for example, sugar-sweetened soft drinks are
the principal energy contributors in the diet (22) and they appear to play a role in the
obesity epidemic due to their high content of readily absorbed
sugars (23). In a recent study
involving 59,334 Danish pregnant women, it has been shown that
daily intake of artificially sweetened soft drinks may increase the
risk of preterm delivery (24).
Therefore, it appears that the decrease noted in this study may
protect from preterm labour. Clearly further epidemiological
studies are required to confirm these effects.
Paradoxically, a wide range of responses concerning
the consumption of fried/fast-food during pregnancy was noted. As
mentioned previously, poor nutrition may lead to a range of health
problems for mothers, including metabolic syndrome and cancer.
Pregnancy results in a state of increased energy demand of
approximately 300 kcals/day. In addition, maternal energy
metabolism is altered during pregnancy and varies greatly among
women. The same women who had increased consumption of fast food
had also increased the intake of iron-rich foods and dairy
products. However, there is no evidence to suggest that this
beneficial intake of calcium and iron counteract poor eating
habits. Our findings are comparable to an Australian study of 409
women where a high proportion of pregnant women consumed 2 meals of
snacks (fast food/take away) per week (25). This finding may also reflect that
new generations appear to give up the traditional Mediterranean
dietary pattern, adopting new dietary trends (26). In addition, dietary patterns are
influenced by various socio-demographic characteristics. Taking
these into consideration it is imperative to develop dietary
interventions to prevent undesirable health consequences during
pregnancy.
Another factor that affects pregnancy is exercise.
Regular physical activity is associated with improved
physiological, metabolic and psychological parameters, and with a
reduced risk of morbidity and mortality (27). In our study [based on the measure
of Paffenbarger et al(8)]
there was a clear shift towards a sedentary lifestyle during
pregnancy. For example, there was an increase in overall inactivity
of approximately 15% and an equal decrease in moderate exercise.
Regular physical activity during pregnancy has been proved to be
beneficial for the mother as well as the foetus. Maternal benefits
include improved cardiovascular function, minimal weight gain
during pregnancy, decreased musculoskeletal discomfort and mood
stability, reduction of GDM and gestational hypertension that may
lead to preeclampsia (PE). Benefits for the foetus include
reduction of fat mass, reduced effects of maternal stress and
advanced neurobehavioural maturation (27).
Pregnancy planning and maternal attitudes towards
pregnancy also appear to affect foetal weight. Approximately 87
million unplanned pregnancies occur every year worldwide and there
is a link between negative experiences of women with unplanned
pregnancies before and after labour. For example, two studies have
linked unplanned pregnancies with poor relationships with their
spouses, experienced financial and educational difficulties and
problems with their professional careers (28,29).
Data from our study suggest that there is no mother-foetal
coherence in the group of unplanned pregnancies, pregnancies since
maternal stress did not predict infant weight in that group.
Noteworthy findings included the effects of maternal attitude to
pregnancy and pregnancy planning on infant birth weight. A
potential interpretation would be that possessing a positive or
neutral (accepting) attitude towards the pregnancy buffers or
protects against any potential negative effect of planning/not
planning the pregnancy on foetal weight. However, women may
demonstrate negative attitudes even towards a planned pregnancy,
and therefore chronic stress may adversely affect foetal
development and weight to a greater extent when compared with
subjects with a negative attitude but in an unplanned
pregnancy.
Consequently, the future directions for healthcare
based on these data should be investigated. With regards to the
nutritional status and in view of the global epidemic of sedentary
life-style and obesity, we propose that pregnant women should
increase their physical activity as a preventative measure against
adverse pathologies for the mother as well as the foetus. Further
studies with larger sample sizes are required to provide solid
evidence of associations between increased physical activity and
positive outcomes of labour and delivery. The use of a
self-reported method for infections may be of clinical
significance, as it is likely to allow obstetricians/midwifes to
classify patients in a high or low-risk group for predisposition
towards pregnancy complications.
Finally, we have also provided evidence that there
is no mother-foetal coherence in the group of unplanned
pregnancies. Therefore, raising awareness of the impact of
unplanned or unintended pregnancy is key. This may be done by
educating the public about social and health issues associated with
unintended pregnancy. Unintended pregnancy affects individuals,
families and communities. Only by communicating this problem to the
public, increasing community and individual understanding about
prevention and improving access to necessary services, ensures more
positive outcomes for both the mother and the foetus.
References
|
1.
|
Shapira N: Prenatal nutrition: a critical
window of opportunity for mother and child. Womens Health (Lond
Engl). 4:639–656. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Vujkovic M, Steegers EA, Looman CW, Ocké
MC, van der Spek PJ and Steegers-Theunissen RP: The maternal
Mediterranean dietary pattern is associated with a reduced risk of
spina bifida in the offspring. BJOG. 116:408–415. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
de Batlle J, Garcia-Aymerich J,
Barraza-Villarreal A, Antó JM and Romieu I: Mediterranean diet is
associated with reduced asthma and rhinitis in Mexican children.
Allergy. 63:1310–1316. 2008.PubMed/NCBI
|
|
4.
|
Mariscal-Arcas M, Rivas A, Monteagudo C,
Granada A, Cerrillo I and Olea-Serrano F: Proposal of a
Mediterranean diet index for pregnant women. Br J Nutr.
102:744–749. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Marcus SM and Heringhausen JE: Depression
in childbearing women: when depression complicates pregnancy. Prim
Care. 36:151–165. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Lobel M, Cannella DL, Graham JE, DeVincent
C, Schneider J and Meyer BA: Pregnancy-specific stress, prenatal
health behaviours, and birth outcomes. Health Psychol. 27:604–615.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Karaçam Z and Ançel G: Depression, anxiety
and influencing factors in pregnancy: a study in a Turkish
population. Midwifery. 25:344–356. 2009.PubMed/NCBI
|
|
8.
|
Paffenbarger RS Jr, Wing AL and Hyde RT:
Physical activity as an index of heart attack risk in college
alumni. Am J Epidemiol. 108:161–175. 1978.PubMed/NCBI
|
|
9.
|
Wang L, Wang X, Wang W, Chen C,
Ronnennberg AG, Guang W, Huang A, Fang Z, Zang T, Wang L and Xu X:
Stress and dysmenorrhoea: a population based prospective study.
Occup Environ Med. 61:1021–1026. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Mendelsohn C: Women who smoke - a review
of the evidence. Aust Fam Physician. 40:403–407. 2010.
|
|
11.
|
Hackshaw A, Rodeck C and Boniface S:
Maternal smoking in pregnancy and birth defects: a systematic
review based on 173 687 malformed cases and 11.7 million controls.
Hum Reprod Update. 17:589–604. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Jones LL, Hashim A, McKeever T, Cook DG,
Britton J and Leonardi-Bee J: Parental and household smoking and
the increased risk of bronchitis, bronchiolitis and other lower
respiratory infections in infancy: systematic review and
meta-analysis. Respir Res. 12:52011. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Goldenberg RL, McClure EM, Saleem S and
Reddy UM: Infection-related stillbirths. Lancet. 375:1482–1490.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Goldenberg RL, Hauth JC and Andrews WW:
Intrauterine infection and preterm delivery. N Engl J Med.
342:1500–1507. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Conde-Agudelo A, Villar J and Lindheimer
M: Maternal infection and risk of preeclampsia: systematic review
and meta-analysis. Am J Obstet Gynecol. 198:7–22. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Lain SJ, Roberts CL, Warning J,
Vivian-Taylor J and Ford JB: A survey of acute self-reported
infections in pregnancy. BMJ Open. 1:e0000832011.PubMed/NCBI
|
|
17.
|
Kuczkowski KM: Caffeine in pregnancy. Arch
Gynecol Obstet. 280:695–698. 2009. View Article : Google Scholar
|
|
18.
|
Wen W, Shu XO, Jacobs DR Jr and Brown JE:
The associations of maternal caffeine consumption and nausea with
spontaneous abortion. Epidemiology. 12:38–42. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Adeney KL, Williams MA, Schiff MA, Qiu C
and Sorensen TK: Coffee consumption and the risk of gestational
diabetes mellitus. Acta Obstet Gynecol Scand. 86:161–166. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Crozier TW, Stalmach A, Lean ME and
Crozier A: Espresso coffees, caffeine and chlorogenic acid intake:
potential health implications. Food Funct. 3:30–33. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Nawrot P, Jordan S, Eastwood J, Rotstein
J, Hugenholtz A and Feeley M: Effects of caffeine on human health.
Food Addit Contam. 20:1–30. 2003. View Article : Google Scholar
|
|
22.
|
Block G: Foods contributing to energy
intake in the US: data from NHANES III and NHANES 1999–2000. J Food
Compost Anal. 17:439–447. 2004.
|
|
23.
|
Schulze MB, Liu S, Rimm EB, Manson JE,
Willett WC and Hu FB: Glycemic index, glycemic load, and dietary
fiber intake and incidence of type 2 diabetes in younger and
middle-aged women. Am J Clin Nutr. 80:348–356. 2004.PubMed/NCBI
|
|
24.
|
Halldorsson TI, Strøm M, Petersen SB and
Olsen SF: Intake of artificially sweetened soft drinks and risk of
preterm delivery: a prospective cohort study in 59,334 Danish
pregnant women. Am J Clin Nutr. 92:626–633. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Wen LM, Flood VM, Simpson JM, Rissel C and
Baur LA: Dietary behaviours during pregnancy: findings from
first-time mothers in southwest Sydney, Australia. Int J Behav Nutr
Phys Act. 7:132010. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Baldini M, Pasqui F, Bordoni A and
Maranesi M: Is the Mediterranean lifestyle still a reality?
Evaluation of food consumption and energy expenditure in Italian
and Spanish university students. Public Health Nutr. 12:148–155.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Melzer K, Schutz Y, Boulvain M and Kayser
B: Physical activity and pregnancy: cardiovascular adaptations,
recommendations and pregnancy outcomes. Sports Med. 40:493–507.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Coleman PK, Reardon DC and Cougle JR:
Substance use among pregnant women in the context of previous
reproductive loss and desire for current pregnancy. Br J Health
Psychol. 10:255–268. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Robbins AS, Chao SY, Frost LZ and Fonseca
VP: Unplanned pregnancy among active duty service women, US Air
Force, 2001. Mil Med. 170:38–43. 2005.PubMed/NCBI
|