Introduction
Ossifying fibroma is a rare benign tumor of the
nasal cavity and paranasal sinus, and is easily misdiagnosed. Since
the initiation of nasal endoscopies in the Department of
Otolaryngology (Gongli Hospital, Shanghai, China) we have treated
two cases of ossifying fibroma in the nasal cavity and paranasal
sinus, confirmed by pathology, over a period of 5 years
(2003–2008). Of the two, only one case has complete clinical data.
In the current study we summarize the clinical and pathological
data and follow-up results of this case. The study was approved by
the ethics committee of Gongli Hospital. Informed consent was
obtained from the patient and the patient’s family.
Case report
A 46-year-old female patient was treated due to 5
days of forehead swelling accompanied by dizziness. The patient
received a head CT in the Neurology Department, which revealed a
right frontal sinus lesion (possibly caused by inflammation due to
a fungal infection), and was subsequently transferred to the
Department of Otolaryngology, Gongli Hospital for treatment. The
patient was hospitalized on April 17, 2007. From the onset, she had
no vertigo, apparent nasal obstruction, nasal mucus, epistaxis,
hyposmia or headache. Furthermore, she denied any history of trauma
to the head or face.
At the admission examination, the systemic signs
were good and the external nasal shape was normal. Right middle
meatus mucosal edema was visible under the anterior rhinoscope but
there were no newplasm or purulent secretions in the nasal cavity.
The right part of the forehead bulged slightly, the skin was
normal, there was no local tenderness or fluctuation, the position
of the right eyeball was slightly lower than that of the left
eyeball but eye movements, visual acuity and visual field were all
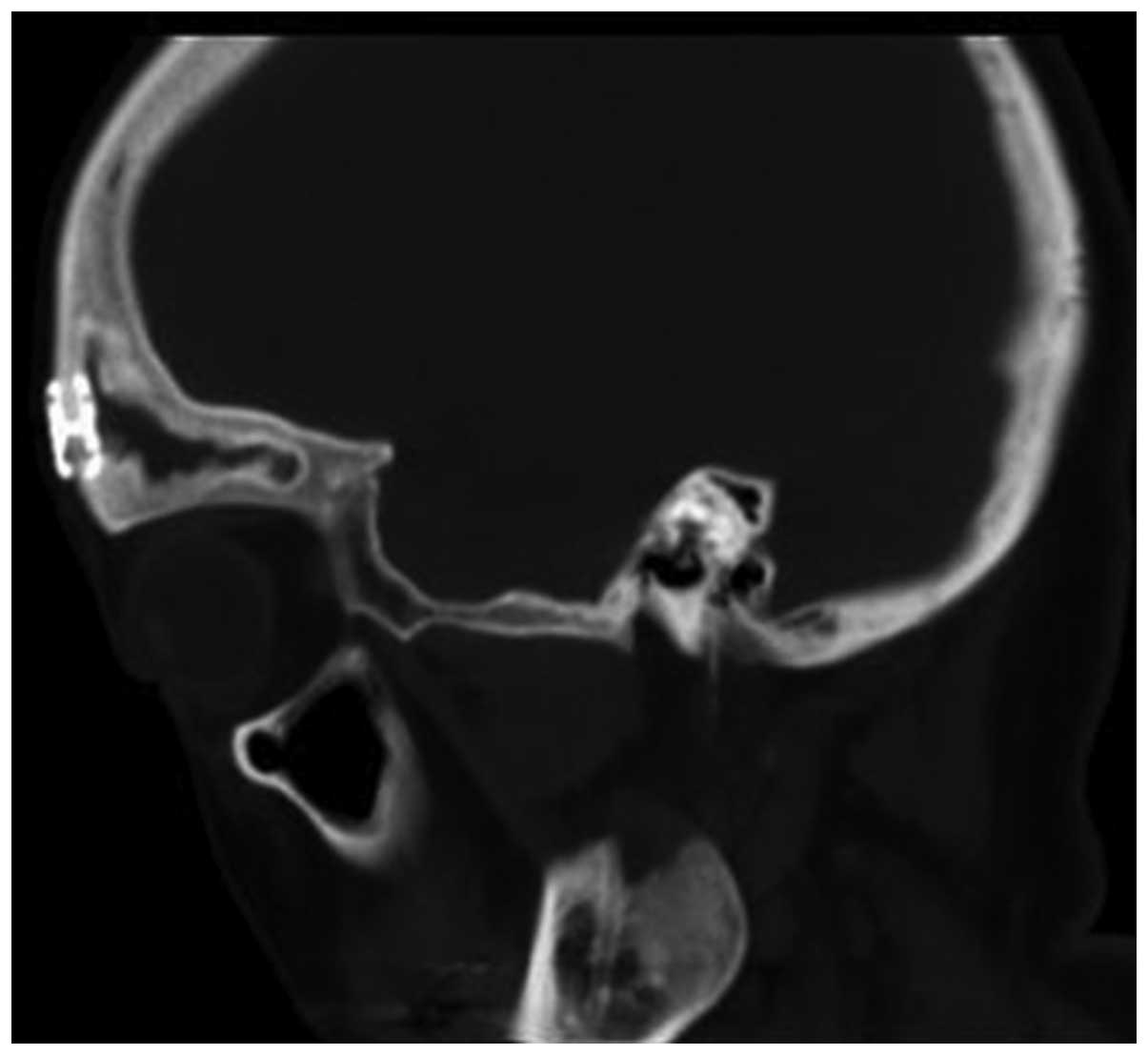
normal. CT scans revealed that the right frontal sinus had dilated,
the bone wall was integrated, dense masses were present inside the
cavity and there were multiple punctate calcification foci
internally. Furthermore, the boundary was clear, there were shadows
of bone-like density, the superior wall of the eye socket had moved
down under stress, and sclerotin was attenuated due to mild
absorption (Fig. 1).
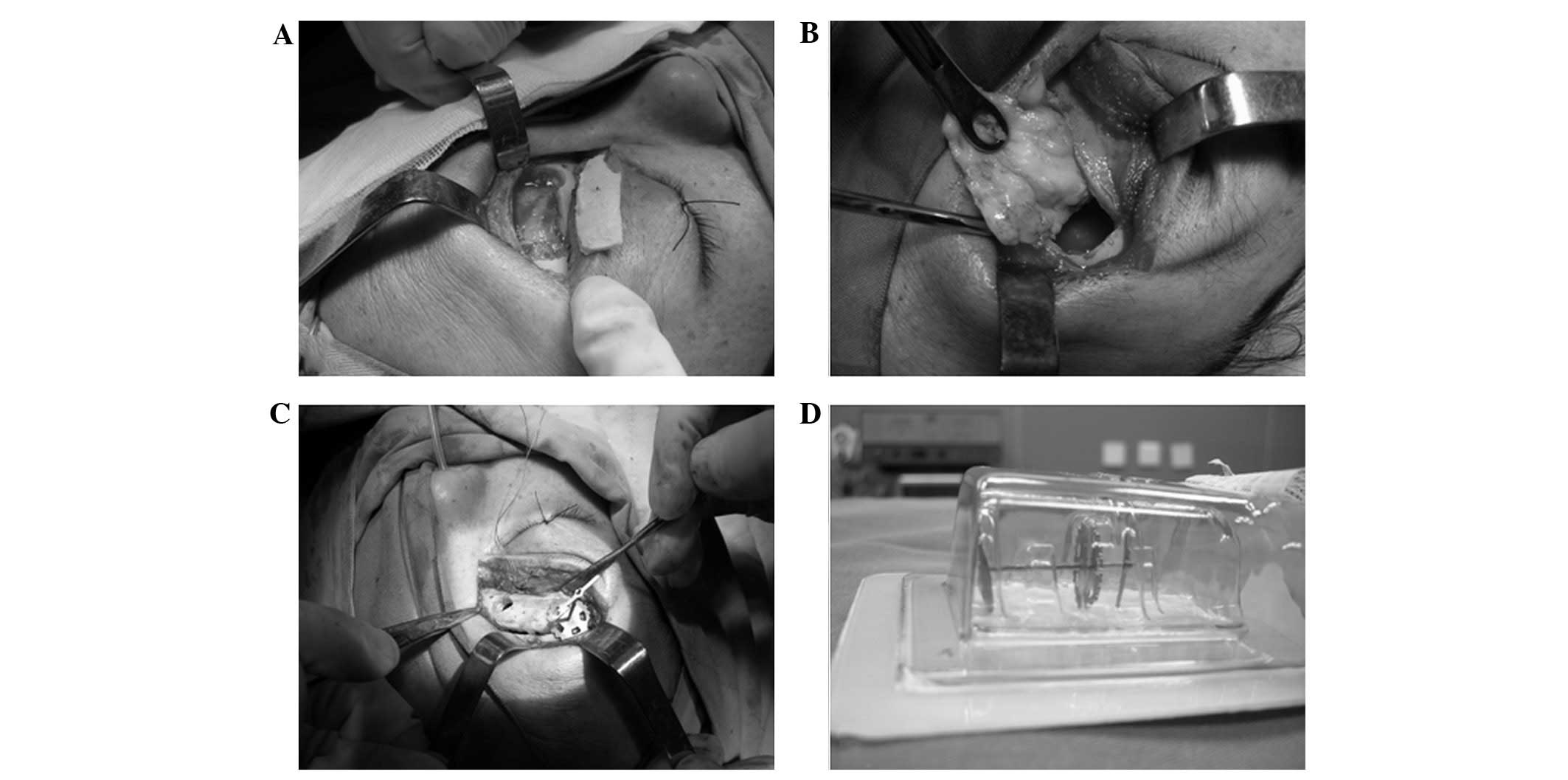
On the 4th day of hospitalization, a right frontal
sinus fenestration and tumor resection plus nasofrontal duct
reconstruction combined with nasal endoscopic frontal recess open
surgery was performed under general anesthesia. During the surgery,
a curved incision was made 0.5 cm from the right side of the inner
canthus outwards to the interior superciliary arch, and a bone
window of ∼4×2 cm was prepared at the anterior wall of the frontal
sinus in order to expose the frontal sinus cavity. It was observed
that the sinus was filled with a solid mass, ∼4.5×4×0.6 cm in size
(grey-white block mass) and sand-like tissues. The tumor had
capsule and like bone, and the boundaries were clear. Following
complete dissection, the surrounding bone wall presented
stalactite-like changes in appearance, and the surface was rough.
At the frontal sinus opening, there was a bony nodular prominence
(0.5×1 cm), the opening of the frontal sinus at the sinus cavity
surface was completely affected by bony atresia. An electric drill
was used to grind the bony prominence in the sinus cavity, and the
anterior ethmoid sinus and frontal recess were opened using a nasal
endoscope. From the bottom wall of the frontal sinus, sclerotin was
gradually ground downwards along the normal nasofrontal duct.
Subsequently, the nasofrontal duct was reconstructed. A silicone
tube was placed into the frontal sinus, led out from the anterior
naris though the nasal cavity and fixed. The frontal sinus bone
lamella was reset and fixed with a titanium bone fixation set, and
the frontal incision was sutured layer by layer. A pressure
dressing was applied and the anterior ethmoid sinus cavity was
filled with calcium alginate gauze (Fig. 2). There was little intraoperative
bleeding and no eyelid swelling or eyeball movement disorder
following the surgery. On the 3rd postoperative day, the nasal
cavity gauze was removed. On the 7th postoperative day, the suture
was removed and the frontal sinus drainage tube was retained.
Additionally, the frontal sinus was rinsed daily. The postoperative
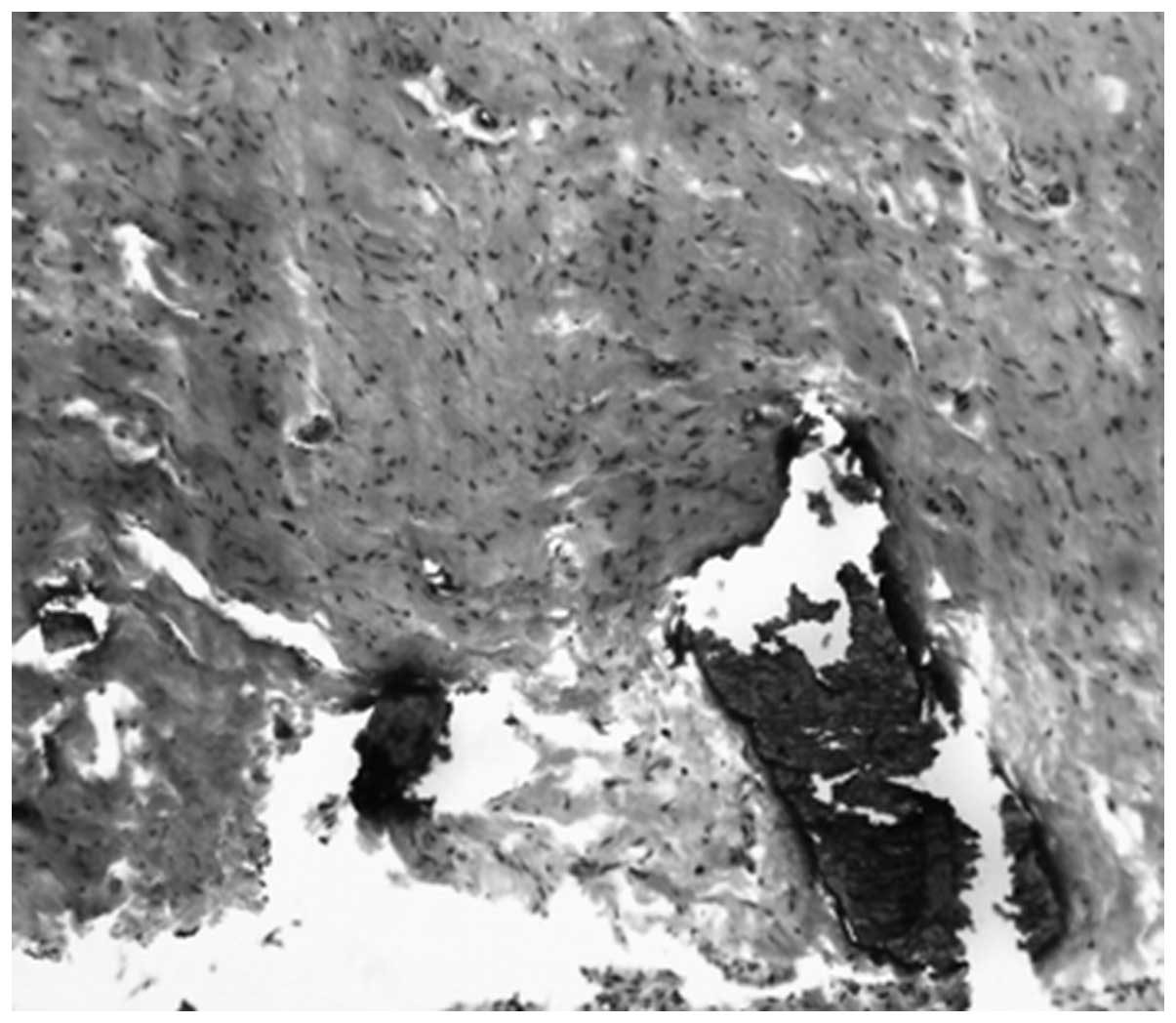
pathological diagnosis was ossifying fibroma (Fig. 3). On the 10th postoperative day,
the patient left hospital, and the forehead swelling and dizziness
had disappeared.
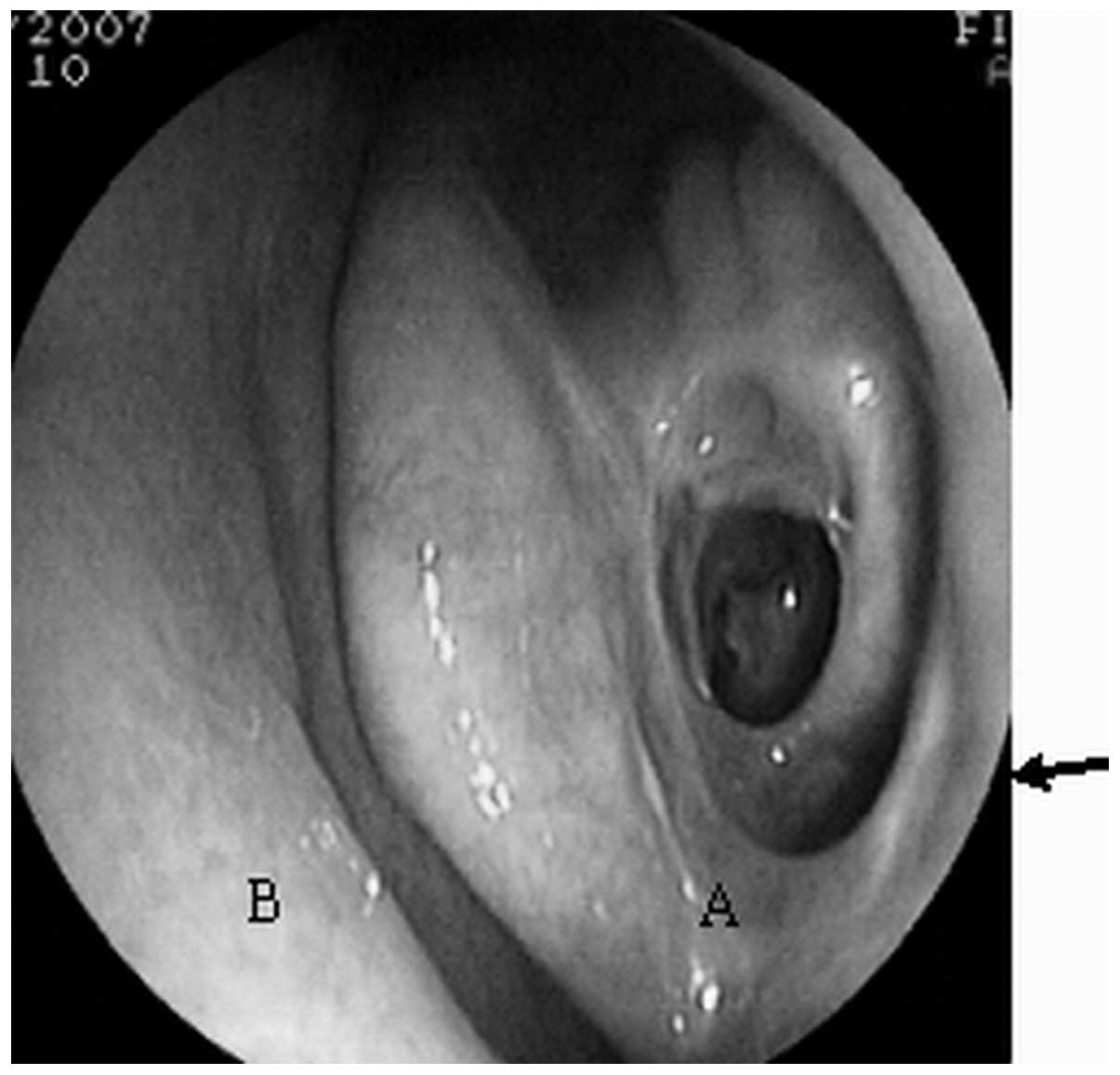
After half a month, reexamination revealed that the
frontal sinus drainage tube in the nasal cavity was unobstructed
and the frontal sinus was rinsed. After one month, the frontal
sinus drainage tube was removed, and nasal endoscopy was performed,
revealing that the nasofrontal duct opening was unobstructed. At
the 5-year postoperative follow up, there was no tumor recurrence.
Nasal endoscopy 1 year postoperatively revealed an unobstructed
nasofrontal duct opening (Fig. 4).
The 1 year postoperative paranasal sinus CT is shown in Fig. 5.
Discussion
Since the first case of ossifying fibroma was
reported in 1872, there was a period of time when ossifying fibroma
and fibrous dysplasia of bone were considered to be the same
disease (1). Following a long
period of observation and study, they are now considered to be two
different diseases. Ossifying fibroma is a bone tissue-derived
benign tumor, whereas fibrous dysplasia is a hyperplastic bone
lesion caused by bone mesenchymal dysplasia (2).
Ossifying fibroma is a rare bone tissue-derived
benign tumor occurring in the craniofacial bone. Of all cases, 70%
occur in the maxilla and mandible (particularly in the maxilla).
The frontal bone, ethmoid bone and sphenoid bone may all be
affected. Occasionally, the occipital and temporal bones have been
affected (2). Ossifying fibroma
occurs mainly in childhood and adolescence, occasionally in
patients aged 20–40 years old, and rarely in patients >40 years
old. Triantafillidou et al hypothesized that the lesions in
adult patients had developed during adolescence (3). The cause of this disease is unknown.
Currently, there are three theories: the dysplasia theory, the
trauma theory and the tumor theory. Current thinking tends towards
the tumor theory, which postulates that the disease is a bone
tissue-derived new generation product (2) and trauma is only a precipitating
factor of this disease.
The clinical symptoms of this disease have no marked
specificity, and early detection is difficult. The patient in this
study was 46 years old, and the lesion had possibly occurred
earlier. Due to the lack of clear clinical symptoms, she had not
visited a doctor. Her clinical manifestations were mainly
dizziness, local swelling and eyeball dislocation and she had no
nasal symptoms. Therefore, the diagnosis was missed by doctors in
the otorhinolaryngology department. The case was initially
diagnosed in the neurology department due to the dizziness
symptom.
The diagnosis of the case was dependent on paranasal
sinus CT and pathological examination. As a routine means of
examination, paranasal sinus CT assists diagnosis and defines the
lesion range for preparing a surgical intervention, and it should
act as a routine presurgical examination. CT scanning images of the
nasal cavity and paranasal sinus present round or oval high-density
shadows, where the density is uniform. If there is bleeding or a
cystic lesion in the tumor, partial areas present as low density
shadows, there are uneven-thickness bone shells on the surface and
the boundary is clear. Additionally, pathological examination is
critical for a definitive diagnosis. Pathological examination
reveals a clear boundary, a fibro-osseous lesion and sand-like
material distributed in the fibrous stroma. These are always the
main features of ossifying fibroma. A preoperative biopsy is
difficult to perform, as it is essential to cut open the mucus in
order to take out the central lesion of the tumor. However, this
method may easily induce the enclosed mass to bleed. It is
recommended that a biopsy is not conducted prior to surgery.
Furthermore, it is necessary to differentiate ossifying fibroma
from fibrous dysplasia of the bone. A CT of the latter generally
shows a more even mass density and the boundary is not clear,
giving an appearance more similar to that of frosted glass.
Pathological characteristics include irregular bone trabeculae,
disorganized and crisscrossed collagen fibers and a large number of
osteoclasts in the bone matrix, and no definite boundary between
the lesion and the surrounding tissues. Some investigators are of
the opinion that histochemistry and immunohistochemistry may aide
the identification of these characteristics.
Ossifying fibroma in the nasal cavity and paranasal
sinus is a benign tumor histologically, but in the clinic it has
invasive characteristics. It usually invades the eye socket, the
base of the skulland calvarium to induce symptoms in the eye and
brain, and its malignancy rate is 0.4–0.5% (4). Furthermore, it is mainly induced due
to repetitive surgery or chemotherapy. Therefore, there is only one
effective treatment method: an early surgery for complete tumor
resection. There are many approaches to the surgery, and the most
suitable approach is generally determined according to the lesion
range (5). For lesions that occur
only in the maxillary sinus, the selection of the Caldwell-Luc
approach for conducting a maxillary sinus radical operation is
appropriate. For lesions that occur in the anterior ethmoid sinus,
frontal sinus and sphenoid sinus, the selection of a lateral
rhinotomy or an extended lateral rhinotomy is appropriate. For
cases with a wide lesion range and with tumor invasion of the base
of the skulland other important sites, it is feasible to use a
combined craniofacial approach for the complete resection of the
tumor. Some investigators believe that as the tumor invasion site
is critical and the surgical risk is high, it is necessary to
conduct a partial resection of the tumor to ensure the function of
vital organs (6).
The previous literature, as well as the findings
from the current case, suggest that the prognosis of this case is
good. There was no tumor recurrence following the complete
resection of the tumor. Recurrence mostly occurs due to incomplete
surgery, and following recurrence, the only solution is to perform
a complete resection of the tumor again. Radiotherapy and
chemotherapy are invalid for this disease, as radiotherapy may
promote a malignant transformation resulting in the formation of an
osteosarcoma (6).
References
|
1.
|
Young FW and Putney FJ: Ossifying fibroma
of the sinuses. Ann Oto Rhinol Laryn. 77:425–434. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Mitrani M, Remsen K, Lawson W and Biller
HF: Giant ossifying fibroma of the paranasal sinuses. Ear Nose
Throat J. 67:186–192. 1988.PubMed/NCBI
|
|
3.
|
Triantafillidou K, Venetis G, Karakinaris
G and Iordanidis F: Ossifying fibroma of the jaws: a clinical study
of 14 cases and review of the literature. Oral Surg Oral Med Oral
Pathol Oral Radiol. 114:193–199. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Yang BT, Wang YZ, Wang XY and Wang ZC:
Imaging study of ossifying fibroma with associated aneurysmal bone
cyst in the paranasal sinus. Eur J Radiol. 81:3450–3455. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Mehta D, Clifton N, McClelland L and Jones
NS: Paediatric fibro-osseous lesions of the nose and paranasal
sinuses. Int J Pediatr Otorhinolaryngol. 70:193–199. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Mohsenifar Z, Nouhi S, Abbas FM, Farhadi S
and Abedin B: Ossifying fibroma of the ethmoid sinus: Report of a
rare case and review of literature. J Res Med Sci. 16:841–847.
2011.PubMed/NCBI
|