Introduction
Numerous clinical studies have demonstrated that
postoperative chemotherapy prolongs the survival of patients with
non-small cell lung cancer (NSCLC). The 2011 guidelines from the
National Comprehensive Cancer Network (NCCN) regarding NSCLC
diagnosis and treatment state that the standard treatment for
patients with a good performance status scale (PS) was a
platinum-based double drug combination (platinum combined with
vinblastine, paclitaxel or gemcitabine). However, NSCLC with the
same pathology and stage exhibits considerable heterogeneity in its
sensitivity to chemotherapy. Currently, individual treatment of
cancer is performed, which requires distinguishing the NSCLC to
enable the treatment to be matched with the pathology and stage.
Specific tumor markers are considered a good method for identifying
changes in an individual patient and the joint detection of a
series of tumor molecular markers aids the chemotherapeutic
efficacy.
Studies have demonstrated that tubulin is a target
site for a number of antitumor drugs, among which β-tubulin has
seven species of isomers and its coding genes are located in 6p21.3
(1). According to the combined
detection with isoelectric focusing and mass spectrometry,
β-tubulin-III has been recognized as the only marker with a
resistance to a microtubule drug among the seven species of
isomers. A clinical study confirmed that β-tubulin-III expression
is associated with chemotherapeutic resistance to the
microtubule-binding protein; however, the conclusions are
inconsistent and occasionally opposing (2). Stathmin, an important microtubule
depolymerizing protein, plays a crucial role as a cell signal
transduction molecule in cell differentiation, tissue regeneration
and restoration, particularly in tumor initiation, development and
phenotype determination. Effective inhibition of stathmin
expression in malignant tumors suppresses tumor cell division and
proliferation, and also promotes cell apoptosis and collaborates
with anti-microtubule drugs to produce an antitumor effect
(3). Stathmin is likely to be a
promising therapeutic target in tumor treatment (4,5).
In the current study, a total of 73 patients with
stage II NSCLC who underwent surgery were selected and recieved
postoperative chemotherapy of Navelbine plus cisplatin (NP). The
mRNA expression levels of β-tubulin-III and stathmin were detected
in tumor tissue and the disease-free survival (DFS) and overall
survival (OS) rates of the patients were recorded. Statistical
analysis was performed to explore the correlation between gene
expression levels and DFS and OS and to investigate the correlation
between β-tubulin-III and stathmin mRNA expression with
chemotherapeutic efficacy, to provide a basis for the establishment
of personalized therapy.
Materials and methods
Clinical samples
All subjects were screened from the specimen
database of The Zhejiang Cancer Hospital. This study was conducted
in accordance with the Declaration of Helsinki and with approval
from the Ethics Committee of Zhejiang Cancer Hospital. Written
informed consent was obtained from all participants. Following
surgery, the pathology of NSCLC was classified according to the
tumor, lymph nodes and metastasis (TNM) staging system of the 2009
Union for International Cancer Control (UICC), through which we
selected 73 NSCLC patients who underwent radical surgery to remove
a tumor between September 2007 and June 2010. Two 0.5
cm3 sections of tumor tissue were collected and
processed into paraffin sections for measurement of β-tubulin-III
and stathmin mRNA expression levels. The clinical features of the
patients were as follows: age ≤60 years in 55 cases, >60 years
in 18 cases; tumor size ≤3 cm in 22 cases, >3 cm in 51 cases; no
lymphatic metastasis in 28 cases, lymphatic metastasis in 45 cases;
high-moderate differentiation in 53 cases, low differentiation in
20 cases; adenocarcinoma in 33 cases, squamous cell carcinoma in 36
cases and other pathological types in 4 cases.
Adjuvant chemotherapy
The patients underwent postoperative NP
chemotherapy; 75 mg/m2 cisplatin was administered for 3
days and 25 mg/m2 Navelbine was administered on days 1
and 8. This treatment was repeated every 3 weeks. Only one patient
recieved two cycles of chemotherapy due to bone metastasis and all
other patients finished 3–4 cycles of chemotherapy in our
hospital.
DFS and OS collection
All patients were followed-up by phone by specified
doctors and received a call every 3 months. The information was
collected from 70 patients with a follow-up rate of 95.89%; the
loss of follow-up was processed as the censored value.
mRNA detection
A QuantiGene assay was performed by Gene Technology
(Shanghai) Co., Ltd. to detect mRNA expression levels using an
Affymetrix QuantiGene Plex 2.0 assay (Panomics, Fremont, CA, USA).
The protocol was as follows: 3–5 pieces of paraffin sections were
lysed and completely digested by lysis buffer. After centrifuging
at 16,000 × g at room temperature, the supernatant was collected
and mixed with microbeads and probes, followed by incubation at
54°C at 600 rpm overnight. Then, all the substance that had not
hybridized to the microbeads was washed away in a magnetic field.
Cascade amplification was performed on the captured RNA signals by
bDNA technology. During this process, including pre-amplification
and amplification, the samples were incubated with labeled probes
for the two steps at 50°C at 600 rpm for 1 h,. The samples were
washed three times using washing buffer following each incubation.
Finally, gene expression data was recorded following streptavidin,
phycoerythrin conjugated (SAPE) labeling by Luminex 200 (Luminex
Corporation, Austin, TX, USA). Phycoerythrin is a protein that
produces a bright red-orange fluorescence. Our improved
phycoerythrin streptavidin (SA-5207) is substantially brighter than
previous conjugates. Phycoerythrin streptavidin may be used on gene
chips, in cell sorting and in tissue staining. The detailed
protocol was according to the method described by Eastham et
al(6). The hypoxanthine
phosphoribosyltransferase 1 (HPRT1) gene was set as the quality
control gene. Therefore, the copy number of the target gene
together with the HPRT1 gene was assessed in each sample. The
median value was considered as the boundary between the positive
and negative.
Statistical analysis
Univariate analysis was conducted using the COX
model. The survival curve was drawn using the Kaplan-Meier method
and checked by the Log-rank test using SPSS 17.0 software (SPSS
Inc., Chicago, IL, USA). P<0.05 was considered to indicate a
statistically significant result.
Results
β-tubulin-III mRNA expression
The mRNA expression levels of β-tubulin-III in the
patients were as follows: mean, 1.250011; median, 0.939473;
minimum, 0.2893; maximum, 4.9174; and variance, 1.018.
Stathmin mRNA expression
The mRNA expression of stathmin in the patients were
as follows: mean, 0.916739; median, 0.6318; minimum, 0.335;
maximum, 5.0746; and variance, 0.975.
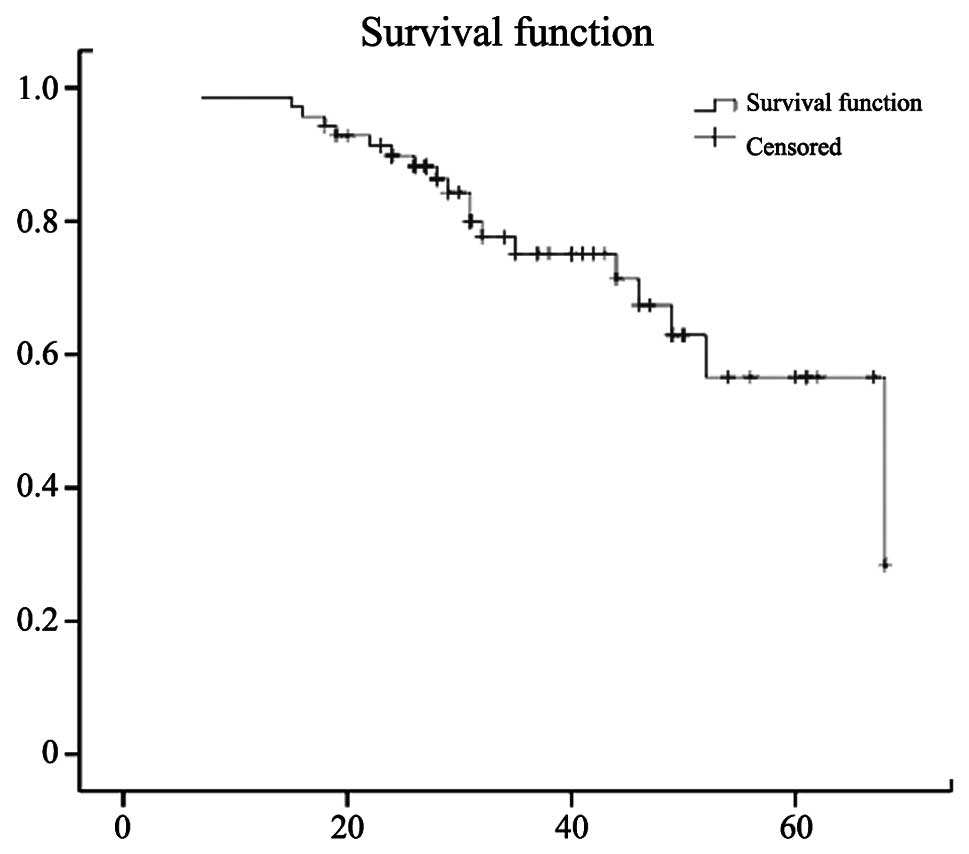
Follow-up time
The follow-up time was between January 17, 2007 and
May 31, 2012 and the median follow-up time was 48 months. In 70
cases, 23 patients relapsed and had metastasis and 19 patients
succumbed during follow-up. The 3- and 5-year survival rates were
75.1 and 56.6%, respectively. The median survival time was 68
months (95% CI, 45.21–90.79 months). The survival curve of the
patients is shown in Fig. 1.
Univariate analysis
Univariate analysis of OS and DFS was performed with
the COX model, which indicated that the OS of patients was
correlated with β-tubulin-III expression and DFS was associated
with β-tubulin-III expression and lymphatic metastasis. However,
the OS and DFS of patients were not correlated with the expression
level of stathmin, age, tumor pathological type, tumor size or
degree of differentiation (Tables
I and II).
 | Table IUnivariate COX analysis of patient
overall survival. |
Table I
Univariate COX analysis of patient
overall survival.
| | | | | | | 95% CI applied to
Exp(B)
|
|---|
| Parameter | B-value | SE | Wald | df | Sig. | Exp(B) | Lowest | Highest |
|---|
| Gender | −0.606 | 0.653 | 0.860 | 1 | 0.354 | 0.546 | 0.152 | 1.963 |
| Age | 0.564 | 0.400 | 1.991 | 1 | 0.158 | 1.758 | 0.803 | 3.847 |
| TUBB3 | 0.402 | 0.178 | 9.032 | 1 | 0.003 | 1.548 | 1.152 | 1.992 |
| STMN | −0.014 | 0.242 | 0.003 | 1 | 0.953 | 0.986 | 0.613 | 1.586 |
| Pathology | −0.049 | 0.401 | 0.015 | 1 | 0.902 | 0.952 | 0.434 | 2.090 |
| Size | 0.409 | 0.301 | 1.848 | 1 | 0.174 | 1.506 | 0.835 | 2.716 |
| Differentiation | 0.999 | 1.038 | 0.926 | 1 | 0.336 | 2.716 | 0.355 | 20.779 |
| LNM | 0.216 | 0.158 | 1.855 | 1 | 0.173 | 1.241 | 0.910 | 1.693 |
 | Table IIUnivariate COX analysis of patient
disease-free survival. |
Table II
Univariate COX analysis of patient
disease-free survival.
| | | | | | | 95% CI applied to
Exp(B)
|
|---|
| B-value | SE | Wald | df | Sig. | Exp(B) | Lowest | Highest |
|---|
| Gender | −0.032 | 0.506 | 0.004 | 1 | 0.950 | 0.969 | 0.359 | 2.614 |
| Age | 0.399 | 0.317 | 1.585 | 1 | 0.208 | 1.491 | 0.801 | 2.775 |
| TUBB3 | 0.423 | 0.140 | 9.097 | 1 | 0.003 | 1.526 | 1.160 | 2.009 |
| STMN | 0.165 | 0.188 | 0.772 | 1 | 0.380 | 1.180 | 0.816 | 1.706 |
| Pathology | 0.304 | 0.354 | 0.741 | 1 | 0.389 | 1.356 | 0.678 | 2.712 |
| Size | 0.123 | 0.218 | 0.316 | 1 | 0.574 | 1.131 | 0.737 | 1.735 |
| Differentiation | 1.038 | 0.741 | 1.962 | 1 | 0.161 | 2.823 | 0.661 | 12.062 |
| LNM | 0.345 | 0.120 | 8.191 | 1 | 0.004 | 1.412 | 1.115 | 1.788 |
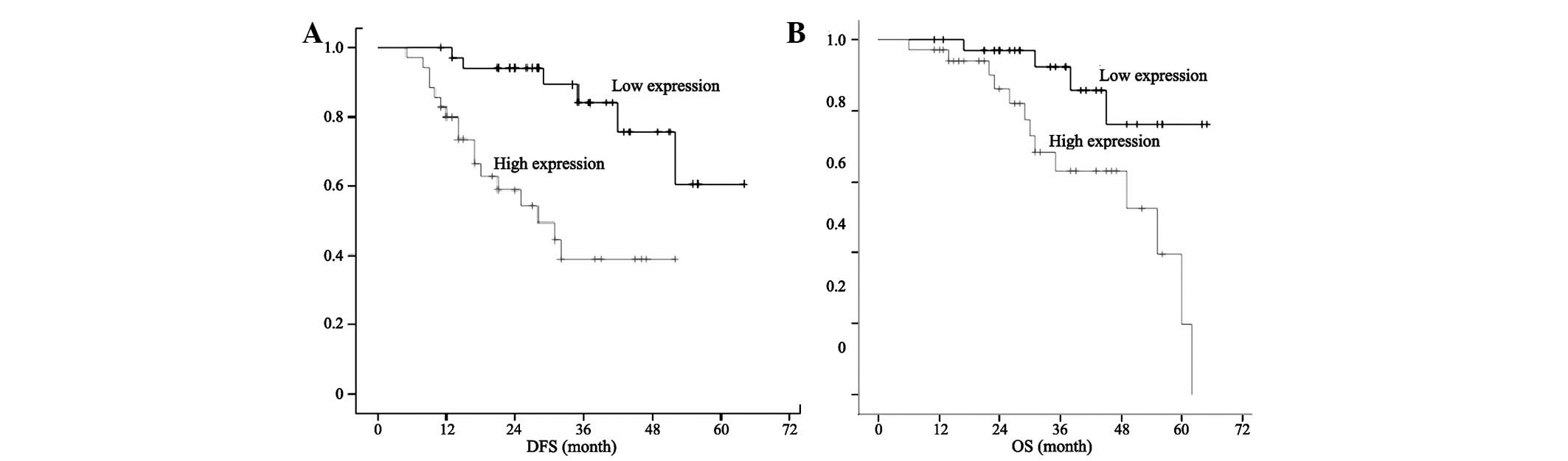
General information
Five patients with negative β-tubulin-III expression
had a relapse and metastasis and two of these patients succumbed
during follow-up. Eighteen patients with positive β-tubulin-III
expression had a relapse and metastasis and 17 of these patients
succumbed during follow-up. The Kaplan-Meier method was utilized to
produce a survival curve, which revealed that the OS and DFS were
longer in patients with low β-tubulin-III mRNA expression levels
compared with those with high β-tubulin-III mRNA expression levels
(Fig. 2).
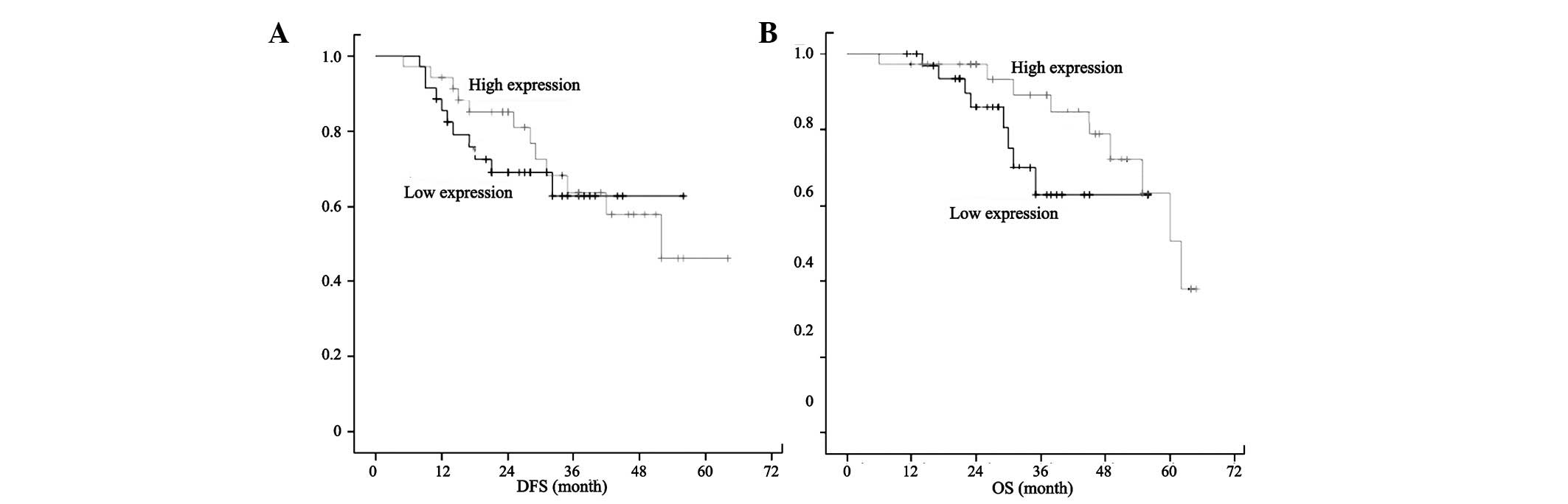
Fourteen patients with negative stathmin expression
had a relapse and metastasis and 11 of these patients succumbed
during follow-up. Nine patients with positive stathmin expression
had a relapse and metastasis and 6 of these patients succumbed
during follow-up. The Kaplan-Meier method was utilized to produce a
survival curve, which revealed no significant change in the OS and
DFS between patients with low and high stathmin mRNA expression
levels (Fig. 3).
Discussion
The theme of the 2009 American Society of Clinical
Oncology (ASCO) annual meeting was ‘personalized tumor treatment
enables the cancer patients to live longer and better’, which
should be considered when treating NSCLC patients. The aim of
personalized therapy is to treat each cancer patient according to
the biological features of the tumor and pharmacogenomics. In 2006,
a landmark article on personalized chemotherapy for lung cancer was
published in the New England Journal of Medicine, which indicated
that only patients with low expression of excision repair cross
complementation 1 (ERCC1) benefit from adjuvant chemotherapy
(7). Hereafter, personalized
chemotherapy based on pharmacogenomics, which draws great attention
among the medical community, as well as the factors for
chemosensitivity prediction and prognosis have become the focus.
The expression of several factors, including the 5′-endonuclease of
ERCC1, ribonucleotide reductase subunit M1 (RRM1) and breast cancer
susceptibility gene 1 (BRCA1), are closely correlated with
chemotherapeutic efficacy and prognosis, and have become crucial
factors for predicting the efficacy of personalized chemotherapy
(8–11).
Previous studies demonstrated that β-tubulin-III has
a close correlation with the sensitivity to chemotherapeutics,
which act on microtubules. A number of studies have confirmed that
an increased concentration of β-tubulin-III is associated with
decreased sensitivity to paclitaxel drugs (12,13).
Our study demonstrated that among patients with
stage II NSCLC who underwent NP therapy following surgery, the OS
and DFS were longer in patients with low β-tubulin-III mRNA
expression levels than in patients with high β-tubulin-III mRNA
expression levels. β-tubulin-III expression is considered an index
for predicting the chemosensitivity to NP therapy and β-tubulin-III
mRNA expression is recognized as an independent index for the
prognosis of patients. However, the results of studies worldwide
are inconsistent and occasionally opposing. Séve et al
selected stage IB-II NSCLC patients and identified that patients
with high β-tubulin-III expression levels have a shorter
progression-free survival (PFS) and OS compared with those with low
β-tubulin-III expression levels among patients who underwent
surgery. However, the situation was the opposite among patients
that underwent surgery and adjuvant NP therapy; the PFS and OS in
the patients with high β-tubulin-III expression were longer than in
those with low β-tubulin-III expression levels (14). One study performed
immunohistochemistry on stage III–IV NSCLC to detect β-tubulin-III
expression in the tumor tissue, which revealed that the expression
level of β-tubulin-III was not correlated with the response rate of
vinblastine therapy; however, it was associated with disease
progression time. The patients with high β-tubulin-III expression
had shorter PFS and OS than those with low β-tubulin-III
expression, which indicates that patients with high β-tubulin-III
expression levels have a vinblastine tolerance (15). Reiman et al investigated the
correlation between β-tubulin-III expression and prognosis of 1,149
patients in four clinical trials whose NSCLC had been resected. The
authors identified that β-tubulin-III expression level may be used
as a prognostic index but not as an index for predicting
chemotherapy efficacy (16). A
number of studies have produce inconsistent results. This may be a
result of varying predictions of β-tubulin-III expression for the
early and late stages of NSCLC. Furthermore, the prediction of
Navelbine efficacy through β-tubulin-III expression was worse than
that of paclitaxel, which required numerous prospective trials to
confirm (17).
Stathmin, an unstable microtubule protein, plays a
crucial role in modulating the dynamic equilibrium of the cell
micro-tubule system through phosphorylation and dephosphorylation
during various stages of the cell cycle. Studies on several types
of lung cancer cells have shown that microtubule polymerization has
an impact on its binding to chemotherapeutic agents. The enhanced
microtubule polymerization increases the binding of microtubules to
paclitaxel instead of vinblastine, affecting the response to
chemotherapeutics in patients with lung cancer (18,19).
The current study demonstrated that, following
surgery, stathmin expression in patients with stage II NSCLC is not
correlated with patient prognosis and should not be used as an
independent predictor for prognosis. There was no significant
change in the OS and DFS between patients with high and low mRNA
expression levels of stathmin. Pu et al reported that the
expression level of stathmin is negatively correlated with the
efficacy of NP therapy in late NSCLC, indicated by
immunohistochemistry (20), which
is inconsistent with our results. One explanation is that stathmin
expression, as well as β-tubulin-III, predicts differently for the
early and late stages of NSCLC. Stathmin, modulating the dynamic
equilibrium of the cell microtubule system through phosphorylation
and dephosphorylation during various stages of the cell cycle, has
a different function at different stages of the cell cycle. The
stathmin protein: promotes microtubule depolymerization during
mitosis interphase; it phosphorylates and the spindle apparatus
forms during the early phase of mitosis; and it dephosphorylates
and the spindle apparatus depolymerizes during the late phase of
mitosis; this process then repeats (21). The second explanation is that the
samples, methods and standards for detection are different. At
present, most studies focus on late NSCLC, utilizing a puncture or
bronchofiberscope technique to collect specimens. The qualitative
methods of PCR and immunohistochemistry are commonly applied;
however, quantitative detection is rarely performed. Moreover,
limited samples and the length of follow-up time may also result in
differences. All these factors may account for the inconsistent
results. Therefore, we are using more methods and collecting a
larger number of samples to assess the gene expression levels in
tumor tissue in order to achieve more accurate results.
Acknowledgements
This study was supported by the
2007-01314 project of the Ministry of Education, Zhejiang.
References
|
1.
|
Volz A, Weiss E, Trowsdale J and Ziegler
A: Presence of an expressed beta-tubulin gene (TUBB) in the HLA
class I region may provide the genetic basis for HLA-linked
microtubule dysfunction. Hum Genet. 93:42–6. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Séve P and Dumontet C: Class III beta
tubulin expression in non-small cell lung cancer. Rev Mal Respir.
27:383–386. 2010.(In French).
|
|
3.
|
Jeon TY, Han ME, Lee YW, et al:
Overexpression of stathmin1 in the diffuse type of gastric cancer
and its roles in proliferation and migration of gastric cancer
cells. Br J Cancer. 102:710–718. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Gan L, Guo K, Li Y, et al: Up-regulated
expression of stathmin may be associated with hepatocarcinogenesis.
Oncol Rep. 23:1037–1043. 2010.PubMed/NCBI
|
|
5.
|
Yuan SF, Chen WJ, Zhu LJ, et al: Effects
of monoclonal antibodies against human stathmin combined with
paclitaxel on proliferation of the QG-56 human lung carcinoma cell
line. Asian Pac J Cancer Prev. 13:2967–2971. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Eastham LL, Mills CN and Niles RM:
PPARalpha/gamma expression and activity in mouse and human
melanocytes and melanoma cells. Pharm Res. 25:1327–1333. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Olaussen KA, Dunant A, Fouret P, et al:
DNA repair by ER-CC1 in non-small-cell lung cancer and
cisplatin-based adjuvant chemotherapy. N Engl J Med. 355:983–991.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Bepler G, Kusmartseva I, Sharma S, et al:
RRM1-modulated in vitro and in vivo efficacy of gemcitabine and
platinum in non-small cell lung cancer. J Clin Oncol. 24:4731–4737.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Papadaki C, Tsaroucha E, Kaklamanis L, et
al: Correlation of BRCA1, TXR1 and TSP1 mRNA expression with
treatment outcome to docetaxel-based first-line chemotherapy in
patients with advanced/metastatic non-small-cell lung cancer. Br J
Cancer. 104:316–323. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Papadaki C, Sfakianaki M, Ioannidis G, et
al: ERCC1 and BRAC1 mRNA expression levels in the primary tumor
could predict the effectiveness of the second-line cisplatin-based
chemotherapy in pretreated patients with metastatic non-small cell
lung cancer. J Thorac Oncol. 7:663–671. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Reynolds C, Obasaju C, Schell MJ, et al:
Randomized phase III trial of gemcitabine-based chemotherapy with
in situ RRM1 and ERCC1 protein levels for response prediction in
non-small-cell lung cancer. J Clin Oncol. 27:5808–5815. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Mariani M, Shahabi S, Sieber S, Scambia G
and Ferlini C: Class III β-tubulin (TUBB3): more than a biomarker
in solid tumors? Curr Mol Med. 11:726–731. 2011.
|
|
13.
|
Koh Y, Jang B, Han SW, et al: Expression
of class III beta-tubulin correlates with unfavorable survival
outcome in patients with resected non-small cell lung cancer. J
Thorac Oncol. 5:320–325. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Séve P, Lai R, Reiman T, et al: Class III
beta-tubulin expression and benefit from adjuvant
cisplatin/vinorelbine chemotherapy in operable non-small-cell lung
cancer: analysis of NCIC JBR.10. Clin Cancer Res. 13:994–999.
2007.PubMed/NCBI
|
|
15.
|
Séve P, Isaac S, Trédan O, et al:
Expression of class III β-tubulin is predictive of patient outcome
in patients with non-small cell lung cancer receiving
vinorelbine-based chemotherapy. Clin Cancer Res. 11:5481–5486.
2005.
|
|
16.
|
Reiman T, Lai R, Veillard AS, et al:
Cross-validation study of class III beta-tubulin as a predictive
marker for benefit from adjuvant chemotherapy in resected
non-small-cell lung cancer: analysis of four randomized trials. Ann
Oncol. 23:86–93. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Stengel C, Newman SP, Leese MP, Potter BV,
Reed MJ and Purohit A: Class III beta-tubulin expression and in
vitro resistance to microtubule targeting agents. Br J Cancer.
102:316–324. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Hansch C and Verma RP: Understanding
tubulin/microtubule-taxane interactions: a quantitative
structure-activity relationship study. Mol Pharm. 5:151–161. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Singer S, Malz M, Herpel E, et al:
Coordinated expression of stathmin family members by far upstream
sequence element-binding protein-1 increases motility in non-small
cell lung cancer. Cancer Res. 69:2234–2243. 2009. View Article : Google Scholar
|
|
20.
|
Pu X, Wang J, Xu L, et al: Relationship
between expression of beta-tubulin-III plus stathmin in advanced
non-small cell lung cancer and its sensitivity to venorelbine
chemotherapy. Zhongguo Fei Ai Za Zhi. 12:49–53. 2009.(In
Chinese).
|
|
21.
|
Singer S, Malz M, Herpel E, et al:
Coordinated expression of stathmin family members by far upstream
sequence element binding protein-1 increases motility in non-small
cell lung cancer. J Cancer Res. 69:2234–2243. 2009. View Article : Google Scholar : PubMed/NCBI
|