Introduction
Gynecomastia is a benign abnormal enlargement of one
or two breasts that is estimated to affect >40% of males
(1). The treatment of gynecomastia
depends on the underlying cause. In the majority of patients with
pubertal gynecomastia, the condition resolves gradually (2,3).
Medical treatment has been shown to be effective in the
proliferative phase of gynecomastia. In a number of cases, however,
fibrotic tissue develops and medical therapy is less helpful. When
gynecomastia has been present for >2 years, medical therapy may
no longer be effective and surgery may be the only useful treatment
(3).
Traditional open surgery causes significant
scarring, seriously affecting the appearance of the breast, so a
number of patients refuse surgery for this reason. Although
traditional surgery removes the hyperplasia completely, the results
are cosmetically unsatisfactory in up to 50% of patients (4). Endoscopic subcutaneous mastectomy
leaves fewer scars and causes no sensory disturbances. Using this
technique, we treated 58 males with gynecomastia, with satisfactory
therapeutic results.
Patients and methods
Patients
A series of 58 male patients who were diagnosed with
Simon grade IIB benign gynecomastia or larger breasts, aged 17–52
years (average, 28 years), underwent endoscopic subcutaneous
mastectomy in the Second Affiliated Hospital of Soochow University
(Suzhou, China) between January 2006 and July 2010. Sixteen of the
patients underwent a unilateral procedure and 42 had a bilateral
excision; 42 breasts presented as cylindrical cones and 10
exhibited mild ptosis. The breast diameter ranged from 10 to 16 cm
and the height from 4 to 6 cm. Fifty-six breasts presented little
development of the nipple. The history of gynecomastia ranged from
13 months to 12 years. In all patients, medical therapy had failed
and surgical treatment was required since the problem was causing
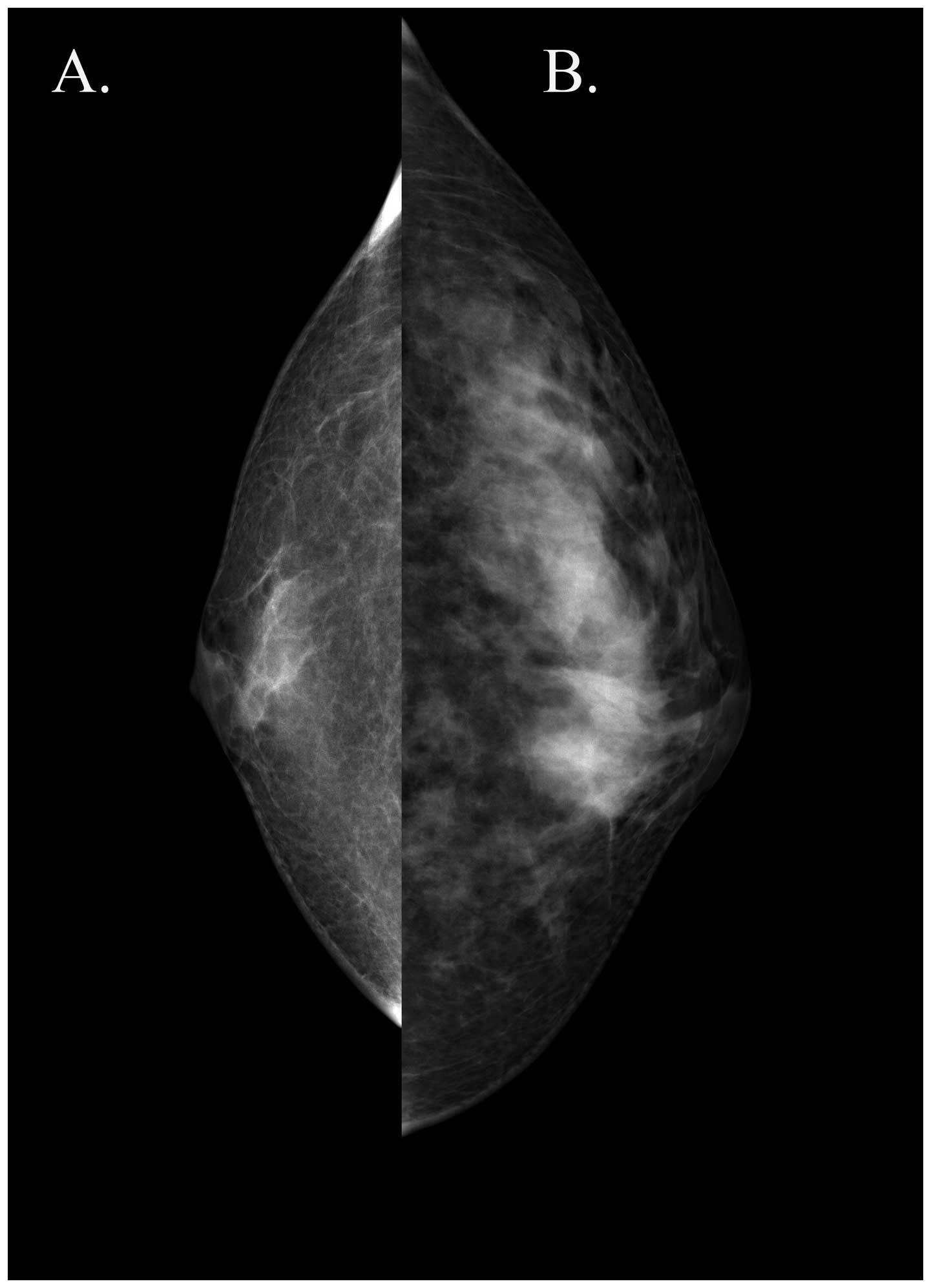
discomfort and affecting their daily lives. All patients underwent
pre-operative mammography to assist in diagnosis and breast
enlargement caused by simple obesity was excluded. This study was
conducted in accordance with the Declaration of Helsinki and with
approval from the Ethics Committee of the Second Affiliated
Hospital of Soochow University. Written informed consent was
obtained from all participants.
Surgical procedure
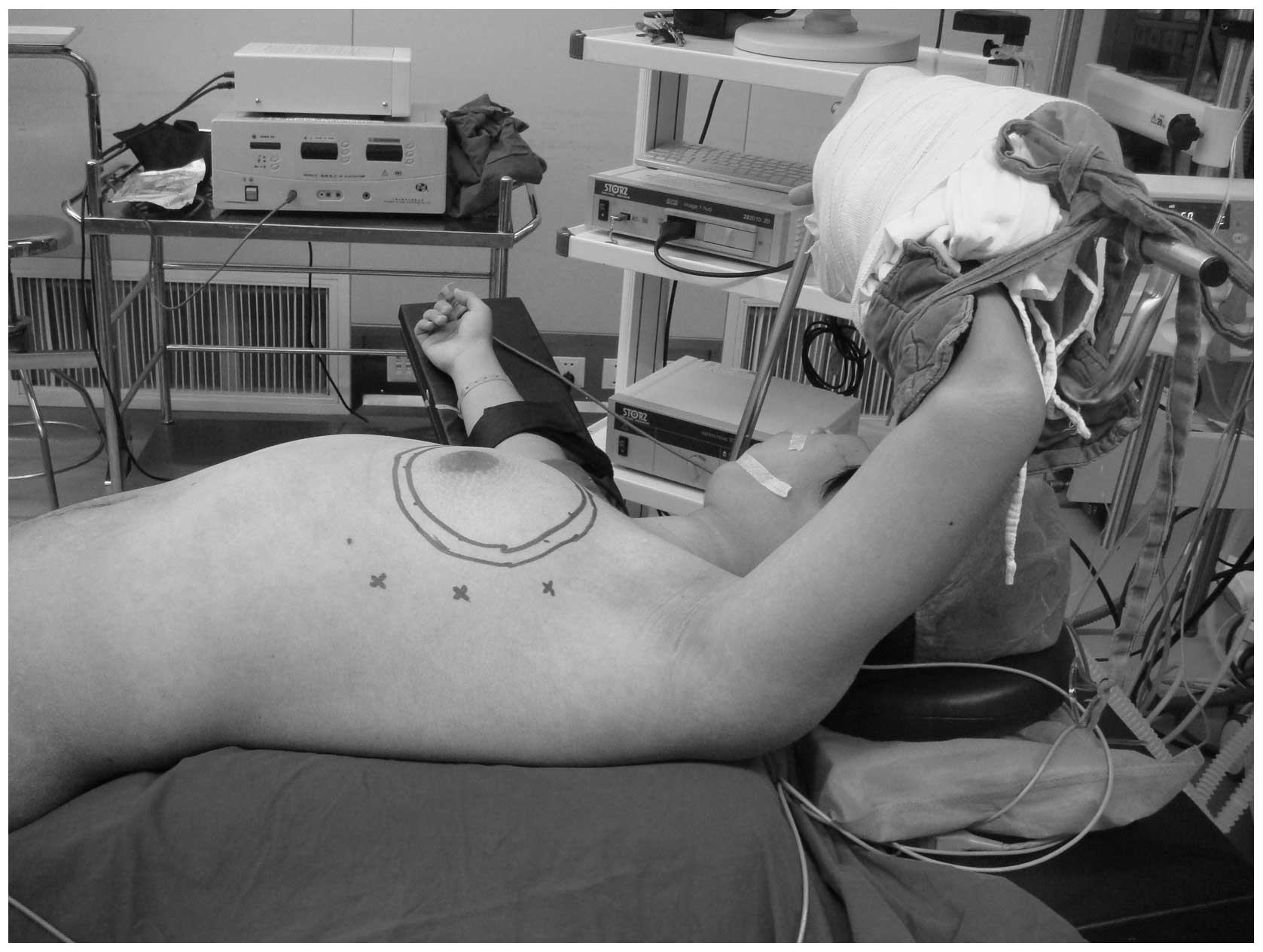
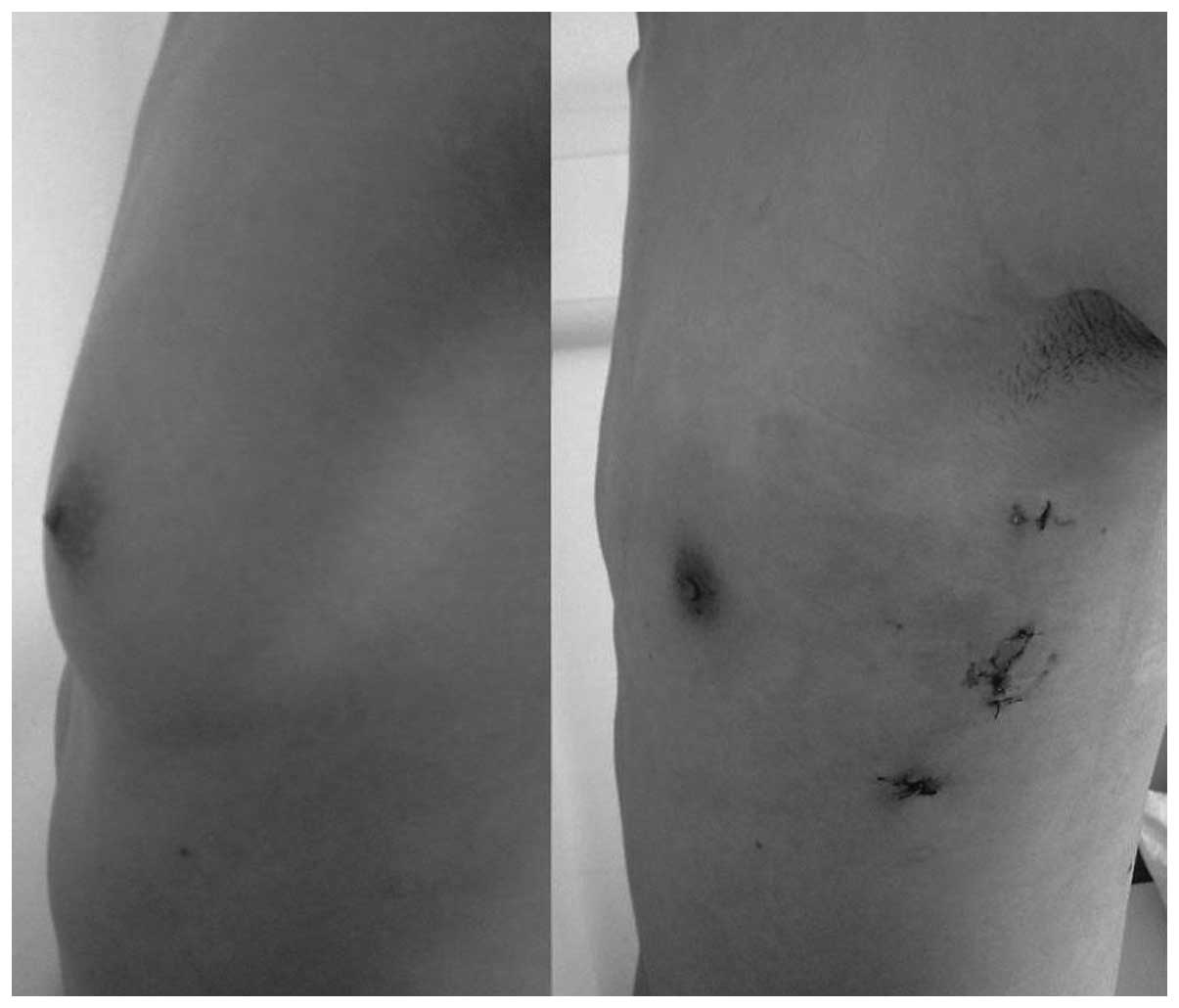
All patients underwent general anesthesia and were
placed in the supine position with the ipsilateral limb wrapped
around the head rack and a thin pillow inserted under the back on
the operative side (Fig. 1). This
position was optimal for the use of the ultrasonic scalpel and
assistant clamp. The breast enlargement was marked on the patients’
skin pre-operatively; a 1-cm mark outside the enlargement was also
marked to determine the area of resection.
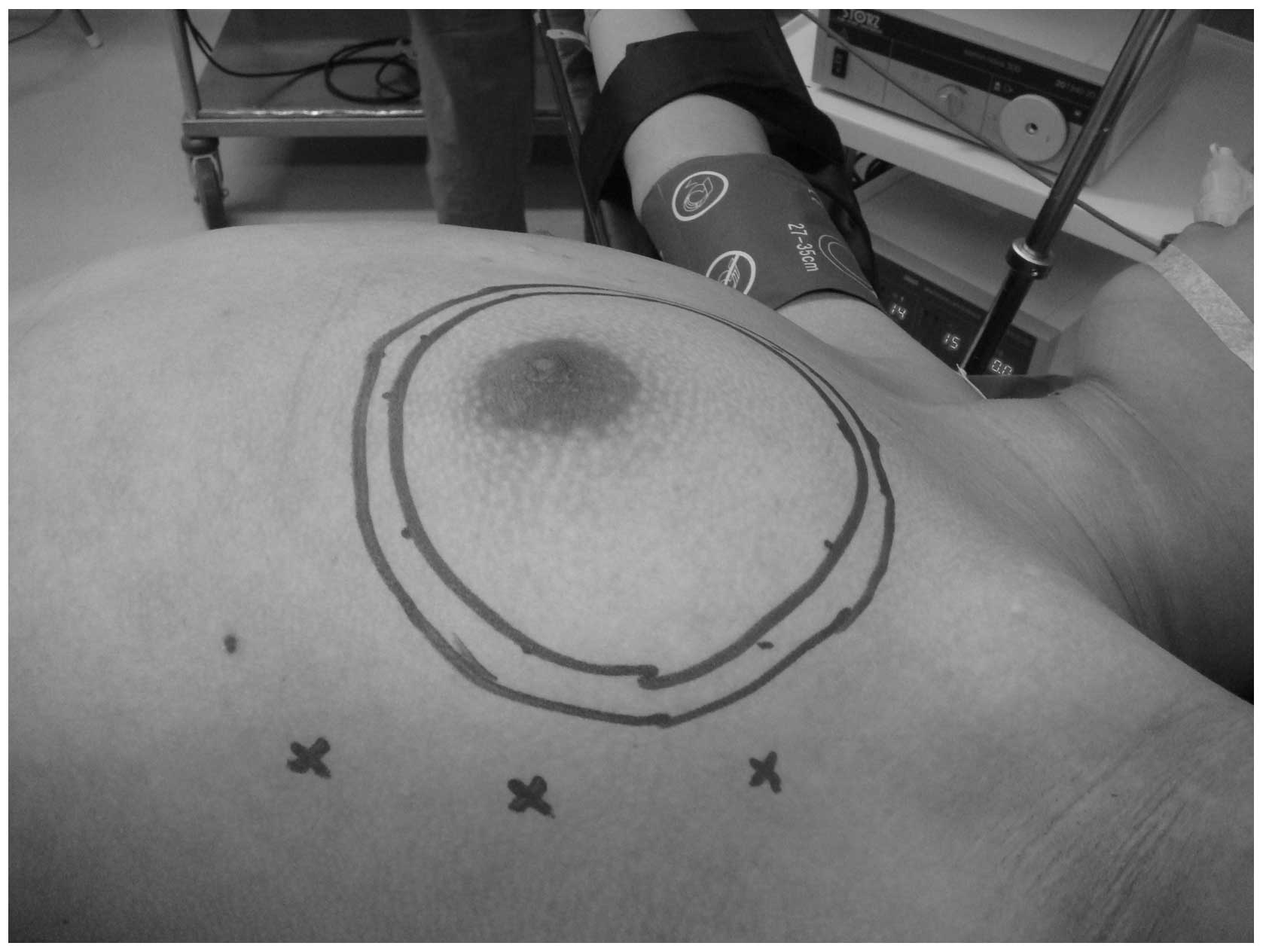
Three small skin incisions were made on the
mid-axillary line (Fig. 2). The
middle incision was 10 mm in length and the other two were 5 mm.
The 10-mm incision was made at the intersection of the mid-axillary
line and the horizontal line through the nipple; the 5-mm incisions
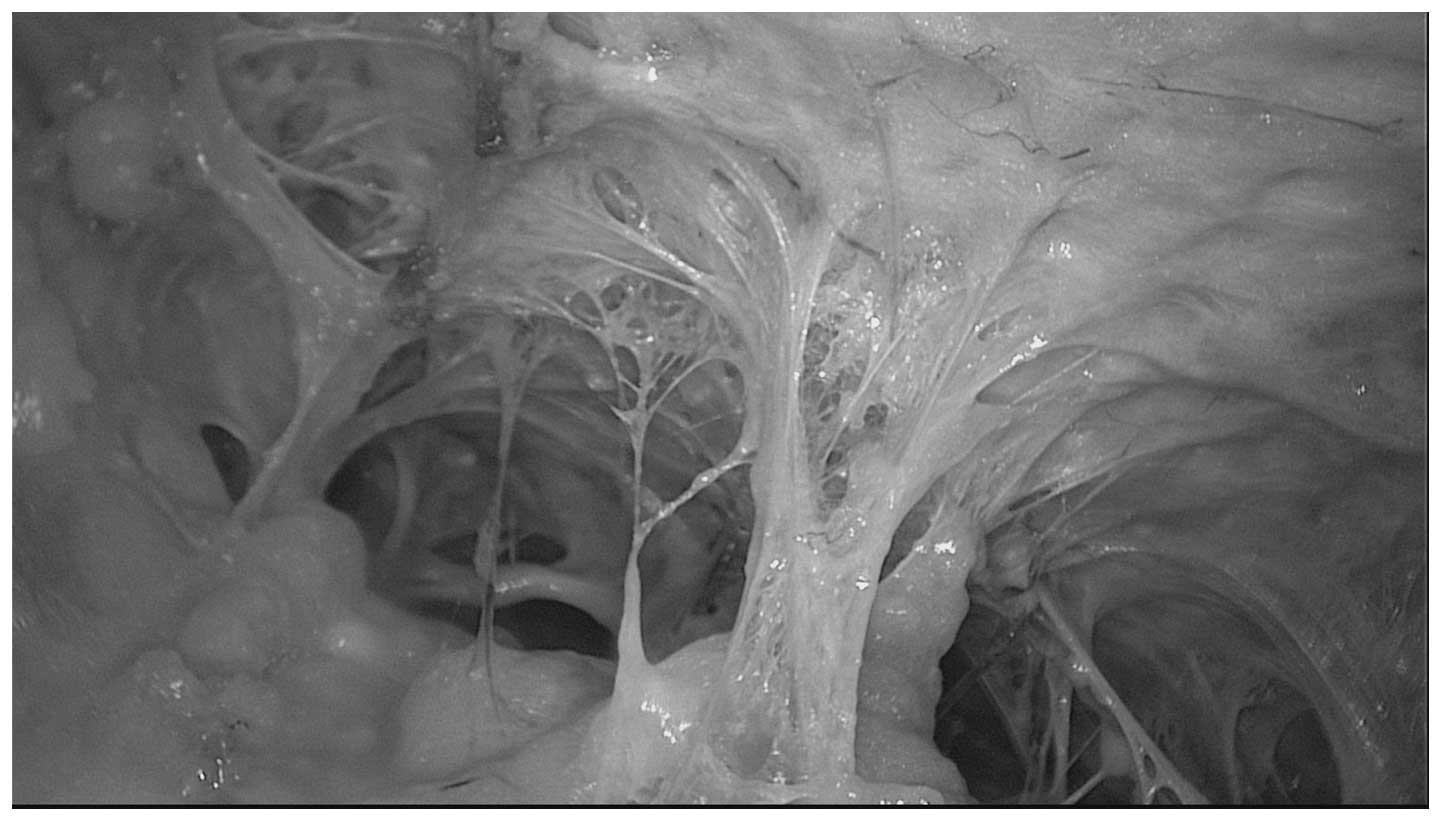
were 5 cm superior and inferior to this (Fig. 2). Warm fat dissolving solution (200
ml 0.9% saline, 200 ml distilled water, 0.5 mg epinephrine and 20
ml 2% lidocaine) was injected into the incisions and allowed to
spread evenly throughout the entire breast subcutaneous tissue and
posterior breast space. After 20 min, all dissolved subcutaneous
and posterior breast space adipose tissue, with the exception of
the fat tissue under the areola, was extracted by vacuum suction
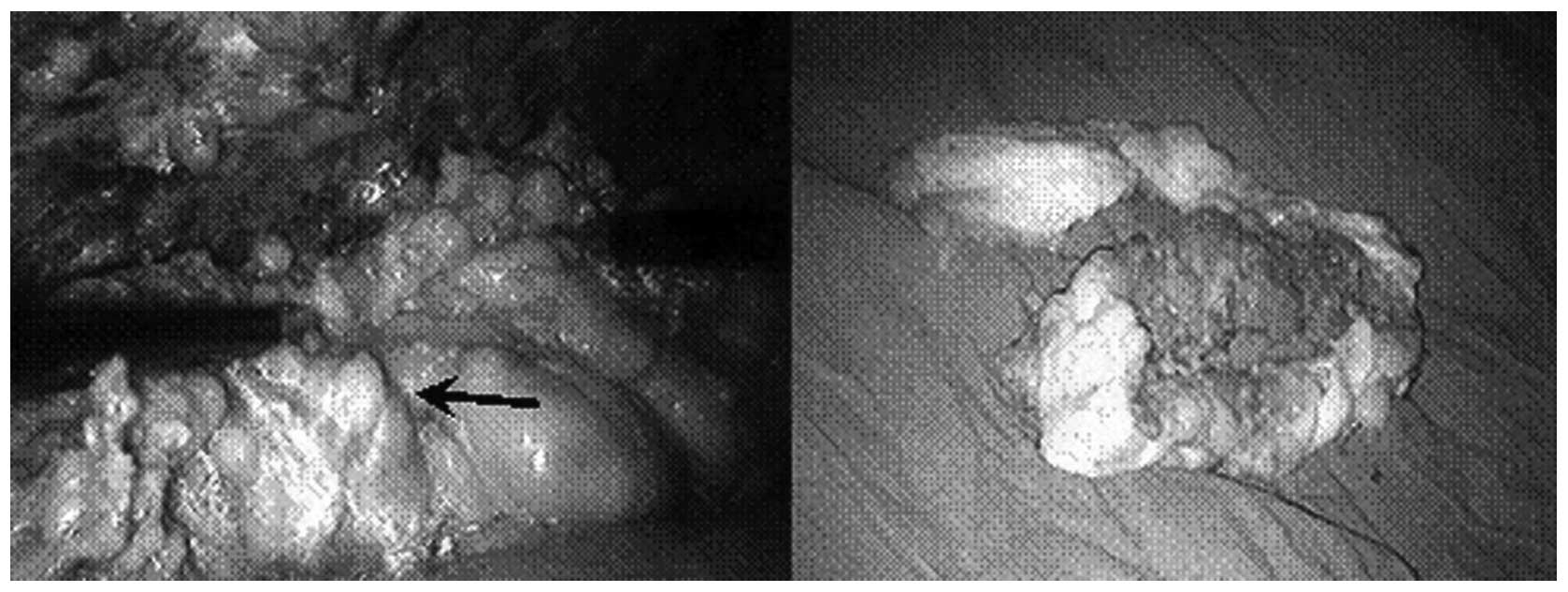
(Fig. 3). The subcutaneous fibrous
septum was detached as much as possible under direct vision; then,
using the little finger as a guide, a trocar with an inner diameter
of 10 mm was placed in the middle incision. Through this trocar, a
space was established by the insufflation of CO2 at a
pressure of 6–8 mmHg. Two 5 mm inner diameter trocars were placed
in the upper and lower incisions, respectively, and the endoscope
was placed in the middle trocar.
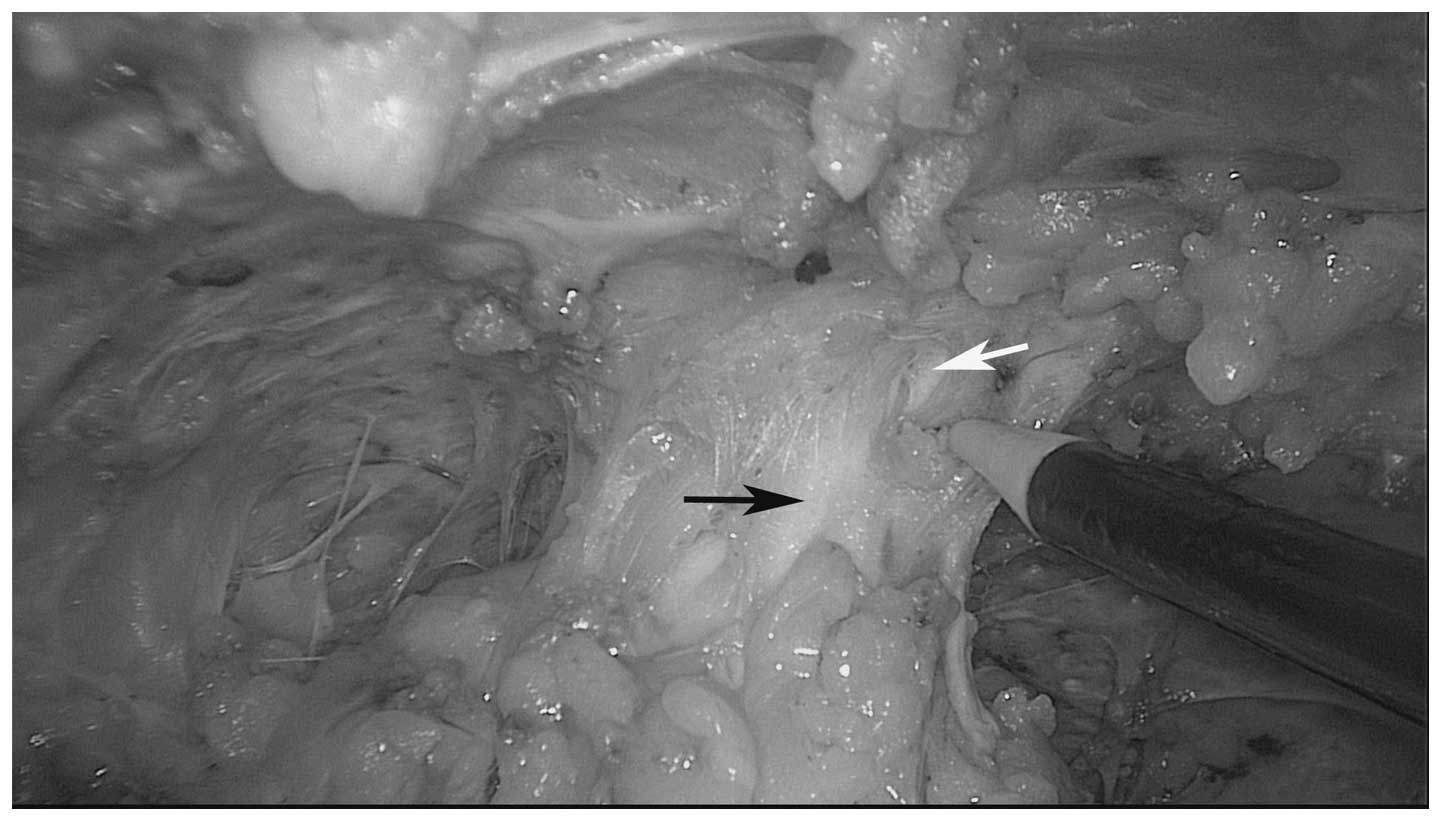
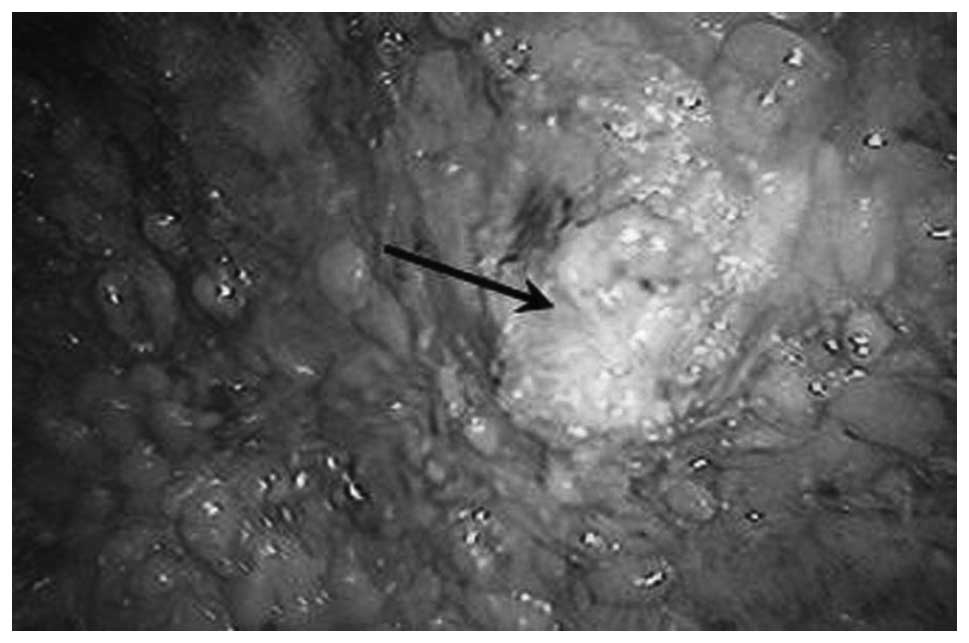
A cutting hemostasis ultrasonic scalpel and
assistant clamp were inserted into the two incisions to subdermally
dissect the fibrous septum. When operating near to the areola, the
nipple-areola complex was drawn upward and the breast tissue was
pressed downward to avoid injury (Fig.
4). The thickness of the complex was maintained at ∼1 cm;
otherwise, partial necrosis may occur postoperatively. The extent
of dissection of the skin overlying the breast was that marked
preoperatively on the breast mound.
After the breast tissue had been fully separated
from the overlying skin, a prepectoral fascia separation was
performed from the axillary side. The whole breast underwent en
bloc resection with the ultrasonic scalpel and was removed
(Fig. 5). Physiologic saline was
used to irrigate the wound and achieve thorough hemostasis
(Fig. 6). A suction drain was
brought out through the lowest incision. All the incisions were
closed with interrupted absorbable sutures (Fig. 7). An elastic compression bandage
was used to wrap the wound. The resected tissue was placed in a
500-ml measuring cup that was then filled with water. After
removing the tissue, the remaining water volume was measured to
calculate the tissue volume (tissue volume = 500 ml − remaining
water volume).
Results
All procedures were completed successfully. The
initial unilateral surgery time was 100–150 min, which has been
improved to 70–90 min with experienced surgeons and improved
cooperation. The volume of the resected specimens ranged from 150
to 300 ml, with a mean of 200 ml. There were no cases of accidental
damage or conversion to open surgery and no significant bleeding.
Postoperative drainage from one side was ∼20 ml per day and the
drainage tube was removed 2–3 days after surgery. No subcutaneous
fluid collections occurred. There were three cases of papillary
epidermal partial necrosis; however, after the dressing was removed
during the hospital stay, normal nipple sensation resumed. There
was no epidermal necrosis at the incision sites and all patients
achieved satisfactory clinical effects and ideal cosmetic results.
The duration of follow-up was 15–63 months, during which no
numbness or other postoperative complications occurred and a
satisfactory breast form was achieved (Fig. 8).
Discussion
Gynecomastia is caused by physiological and
pathological factors. In young patients, particularly adolescents,
the causes are mainly physiological at puberty and the gynecomastia
usually resolves spontaneously. In the current study, the majority
of patients that we selected had passed puberty, which meant that
the condition was unlikely to resolve spontaneously. Secondly,
prior to surgery, all patients underwent breast mammography to
ensure that the mammary gland itself was significantly enlarged. In
the present study, the mean volume of resected breast tissue was
200 ml, with a maximum of 300 ml. The indication for endoscopic
resection was breast enlargement at Simon grade IIB or above, with
glandular hyperplasia. Thirdly, the longest duration of disease in
this group was 12 years and the shortest treatment time of patients
within this group was 13 months. Therefore, all patients in this
study had been through a long-term medical consultation process and
drug therapy before they underwent endoscopic subcutaneous
mastectomy.
Gynecomastia is considered to be present in >30%
of males, with much higher rates in males aged >70 years. We
elected not to select elderly patients in this study for several
reasons. Firstly, gynecomastia in elderly male patients is often
caused by declining levels of testosterone. Treatments with
additional androgens and traditional Chinese medicine may have
therapeutic effects. Secondly, elderly patients tend not to be as
concerned with scars on the chest and are more likely to choose a
traditional surgical resection approach. Finally, elderly patients
are less likely to take on the relatively high costs of this new
technique compared with the standard surgical approach used in
China.
Obesity in males often causes increased breast size
and yet this increase is simply due to the accumulation of adipose
tissue. Thus, before the decision is made to perform surgery, we
ensured that every patient underwent breast mammography to ensure
that the breast enlargement was caused by an increased mammary
gland size rather than increased volumes of adipose tissue
(Fig. 9). If the mammary gland and
adipose volume had increased, in general we advised patients to
lose weight first and then have surgery, as the surgical outcomes
are better in patients with a lower level of adiposity.
The surgical methods for the treatment of
gynecomastia include liposuction, periareolar incision and
endoscopic surgery. Mastectomy with a periareolar incision removes
a Simon grade I or II enlarged breast; however, longer incisions
are required for breasts that are grade IIB or larger. These
incisions leave large scars on the chest, which are often
unsatisfactory to the patient (5).
Liposuction removes smaller amounts of fatty tissue; however, it
does not work well when there is a firm glandular component
(6). Liposuction plus local
resection through a periareolar or remote incision has replaced
open excision in cases of gynecomastia with severe hypertrophy
(7,8), significant skin excess and grade 3
ptosis. In the current study, we selected patients with larger
developed breasts, with a mean volume of 200 ml of resected breast
tissue. To resect large breasts, periareolar incision surgery is
likely to leave visible scars and liposuction is unable to achieve
a complete resection (Fig. 9).
Endoscopic microsurgery with a 10 mm incision at the mid-axillary
line has satisfactory esthetic results that are welcomed by the
majority of patients. In the present study, we proposed points to
achieve a good surgical effect, as follows: i) the dissolving and
suction of all fat tissue, with the exception of that under the
nipple and areolar area, provides easy access for the separation of
breast and subcutaneous tissue; ii) the subcutaneous fibrous septum
should be detached as much as possible under direct vision; using
the little finger as a guide, the trocar may then be placed
properly; iii) during subdermal breast parenchyma dissection, when
operating near the areola, the nipple-areola complex should be
drawn upward and cuts made slowly to avoid injury. Damage to the
vasculature of the complex may be avoided if some glandular tissue
remains. It is important to keep the thickness of the complex at ∼1
cm, to reduce the risk of postoperative nipple necrosis; and iv)
the sequence of the procedure is important. We detached the
subcutaneous fibrous septum to provide a satisfactory working space
for the glandular resection. The resected tissue was then pulled
out of the trocar hole with no need to lengthen the incision,
improving the esthetic results.
It should be noted that, during insufflation, too
high a pressure causes pneumoderma and too low a pressure may
induce respiratory movements that disturb the surgery. Thus, we
suggest that the pressure of insufflation of CO2 should
be 6–8 mmHg. Three cases of partial necrosis of the nipple area
were identified. These may have resulted from injury to the
subdermal vasculature or heat damage to the nipple skin from the
ultrasonic scalpel.
Liposuction plus ultrasound-guided vacuum-assisted
breast biopsy is a recently reported, potential method for esthetic
surgery (9,10). However, the endoscopic resection of
an enlarged breast achieves the complete and accurate removal of
mammary tissue under direct vision with clear advantages.
In conclusion, endoscopic subcutaneous mastectomy
for gynecomastia had satisfactory esthetic results and no
significant postoperative complications. It is an appropriate
surgical approach for gynecomastia, providing that skilled
operators and suitable endoscopic technology are available.
References